Abstract
Deposit contracting may reduce costs and increase efficacy in contingency management interventions. We evaluated two Internet-based deposit contract arrangements for smoking. In Experiment 1, nine participants deposited self-selected amounts that could be earned back for meeting goals. During treatment, participants were reimbursed for breath samples with less than or equal to 6 parts per million carbon monoxide and met the criterion for 47% of samples compared to 1% during baseline. In Experiment 2, 10 participants’ deposits were matched up to $50. No samples met the criterion during baseline but 41.5% met it during treatment. The average deposit was $82 in Experiment 1 and $49 in Experiment 2. Participants rated the intervention favorably and sample submission rates were high. These experiments suggest that Internet-based self-tailored deposits are acceptable, feasible, and can promote brief reduction and abstinence in some smokers. Future research should investigate individual and intervention factors that affect long-term cessation and uptake of deposit contracts.
Keywords: contingency management, deposit contracting, smoking, technology, incentives
There is a critical need to develop alternative and more effective smoking cessation treatments than those currently available (Schlam & Baker, 2013). One alternative, contingency management (CM), is acceptable (Raiff, Jarvis, Turturici, & Dallery, 2013) and effective in promoting short-term abstinence (Sigmon & Patrick, 2012). In CM, individuals earn monetary vouchers for providing biochemical evidence of smoking reduction or abstinence. Findings on CM for smoking are encouraging but its dissemination and use are limited by costs, especially those required for vouchers (Petry, 2010). One method to reduce voucher costs is to incorporate deposit contracts (Amass & Kamien, 2008). Deposit contracts require individuals to contribute their own money, which can be recouped for meeting reduction or abstinence goals. Just as CM promotes behavior change by supplementing positive long-term consequences of smoking abstinence with more immediate gains, deposit contracts promote abstinence by supplementing delayed negative consequences associated with smoking with more immediate losses (Halpern, Asch, & Volpp, 2012).
To date, 15 studies have evaluated the effectiveness of deposit contracting to promote smoking abstinence (Bowers, Winett, & Frederiksen, 1987; Dallery, Meredith, & Glenn, 2008; Elliot & Tighe, 1968; Gine, Karlan, & Zinman, 2010; Halpern et al., 2015; Jeffery, Pheley, Forster, Kramer, & Snell, 1988; Lando, 1976, 1977; Paxton, 1980, 1981, 1983; Singh & Leung, 1988; Spring, Sipich, Trimble, & Goeckner, 1978; White, Dow, & Rungruanghiranya, 2013; Winett, 1973), but most were published over two decades ago. Collectively, these studies suggest that deposit contracting is feasible and may increase cessation. Nevertheless, there were one or more limitations in these studies. First, several lacked appropriate controls (e.g., Elliot & Tighe). Second, approximately half made deposit repayments based on self-report only (e.g., Lando, 1977; Winett, 1973). Studies that did include biochemical verification often did so infrequently (e.g., Gine et al., 2010; White et al., 2013). Finally, many deposit contracts were delivered with other major treatment components (e.g., counseling, aversive smoking procedures; Paxton, 1980; Spring et al., 1978). These methodological limitations make it difficult to attribute treatment outcomes to the deposit contracts.
These limitations were addressed by Dallery et al. (2008) in a brief Internet-based pilot study. Eight smokers received CM with a standard voucher arrangement or CM with a deposit contract. Participants in both groups could earn roughly $80 in vouchers, but those using the deposit contract were required to contribute $50. The standard and deposit groups abstained at high and similar rates (65% and 63% of total samples were negative, respectively). Yet, the standard arrangement cost approximately $180 to deliver, whereas the deposit arrangement resulted in a surplus of over $40. These results offered preliminary evidence that deposit contracts may be as efficacious as standard systems and can be delivered with no voucher costs.
More recently, Halpern et al. (2015) evaluated incentive treatments for smoking cessation, including deposit contracting, in a large (N = 2,538) randomized 6-month intervention. Participants were offered one of four arrangements: individual reward, individual deposit, collaborative reward, and competitive deposit. Smokers in the individual reward earned up to $800 for 6 months of abstinence. Smokers in the individual deposit also earned up to $800 but completed a $150 deposit contract at the outset of the intervention. In the collaborative reward, groups of six smokers earned up to $2000 per smoker, with amounts increasing with greater group success. Finally, in the competitive deposit, smokers deposited $150 and earned up to $3800 each, with individual payouts decreasing with greater group success. Abstinence was verified at 14 days, 30 days, and 6 months after a target quit date with salivary cotinine. There were no significant differences between the group and individual arrangements on any outcome. Overall effectiveness in intent-to-treat analyses favored the reward-based programs (15.7% vs. 10.2% abstinent at all time points), perhaps owing to the much lower uptake (i.e., agreeing to enroll in assigned program) of the deposit contract compared to the reward arrangements (13.7% vs. 90%). Sustained abstinence for those who accepted the programs was 52.3% in the deposit groups compared to 17.1% in the reward groups. An analysis that corrected for group assignment bias showed that 6-month abstinence rates were 13.2% higher for the deposit arrangements among smokers who would accept either the deposit or reward arrangements. Moreover, the cost per quitter in the individual deposit group was roughly half that of individuals in the reward group. These results demonstrate that deposit contracts for smoking are highly efficacious and cost-effective but have low uptake relative to reward-based programs.
Two areas not addressed in Dallery et al. (2008) and Halpern et al. (2015) warrant further investigation. First, the deposits required in both studies were set at fixed amounts, and the $150 deposit required in Halpern et al. decreased treatment enrollment relative to the reward groups in that study. This is consistent with work showing that higher magnitude deposits decrease treatment enrollment for weight loss (Jeffery, Gerber, Rosenthal, & Lindquist, 1983). However, random assignment to higher magnitude deposits has produced better treatment outcomes in weight loss (Jeffery et al. 1983). One potential means of balancing the tradeoff between enrollment and treatment success associated with deposit magnitude is to allow participants to select their own deposit amount. Jeffery et al. (1988) first evaluated this approach in a multicomponent worksite intervention in which participants selected an amount to be withheld from their biweekly paycheck contingent on testing positive for smoking. The average amount chosen was $10.22 but ranged from $5 to $25. Similarly, smokers enrolled in a program in the Philippines made initial deposits of 50 to 410 pesos ($1 to $8.20; Gine et al., 2010) to which they were able to contribute further each week for 6 months (average deposit amount at 6 months was $11, roughly 20% of one’s monthly income). Smokers who chose to contribute higher magnitudes were more likely to quit. Despite several methodological limitations (e.g., group assignment bias, infrequent verification of smoking), these studies offered preliminary evidence that self-tailored deposits can reduce smoking. Furthermore, they highlight the fact that smokers vary in the magnitudes of deposits that they contribute.
A second area warranting further investigation concerns supplemental vouchers. In Dallery et al. (2008) and Halpern et al. (2015), participants could earn $28.80 and between $650 and $3450, respectively, in addition to their deposits. It is not known whether the deposit contract alone, without supplemental vouchers, would be acceptable and sufficient to promote smoking cessation. Eliminating supplemental vouchers might reduce overall treatment costs and may be a more practical approach for clinics with limited budgets (Kirby, Benishek, Dugosh, & Kerwin, 2006). Alternatively, offering supplemental vouchers might be viewed as more acceptable to treatment-seeking smokers and might promote greater abstinence through increased uptake or efficacy.
The purpose of the current study was to evaluate the feasibility, acceptability, and preliminary efficacy of two novel self-tailored deposit contract arrangements to promote smoking reduction and abstinence. Experiment 1 examined self-tailored deposits alone and addressed methodological issues seen in previous studies. Experiment 2 examined self-tailored deposits in combination with clinic-matched supplemental vouchers. Both experiments used an Internet-based CM platform (Dallery, Raiff, & Grabinski, 2013), which allows for frequent and convenient monitoring of smoking, extends the reach of the intervention to any of the 74.4% of US households with home Internet access subscriptions (File & Ryan, 2014), and may reduce costs associated with in-person CM (e.g., staffing, office space). These experiments are one of the first reports of a fully-remote CM intervention for smoking. All treatment procedures were performed via computer and mobile phone, which did not require face-to-face contact with participants.
GENERAL METHOD
Recruitment
Participants were recruited locally and nationally using print (e.g., flyers) and online media (e.g., Craigslist advertisements). Study advertisements varied by format and space restrictions, but all indicated that the University of Florida Smoking Laboratory and Clinic (UFSLC) was recruiting smokers for an online quit smoking research study and provided study website and contact information.
Interested individuals were directed to a study website, which included a short study overview video, frequently asked questions with answers, and information about the clinic. To determine eligibility, individuals were directed to an online screener where they answered brief questions and gave contact information.
Eligibility
Inclusion criteria were that participants (1) were 18–60 years old, (2) expressed a desire to quit smoking, (3) smoked ≥10 cigarettes per day on average, (4) had smoked in the past 24 hr, (5) had smoked daily for ≥2 years, (6) were willing to make a one-time deposit, and (7) had computer and Internet access at home. All individuals were contacted within 48 hr to verify eligibility. Those who were ineligible were directed to online smoking cessation resources. Informed consent included a quiz to measure understanding of the study procedures and was obtained electronically from those who met the inclusion criteria. Missed questions were reviewed with participants before enrollment.
After consenting and completing the quiz, participants completed a psychosocial survey on demographics, smoking history, other tobacco use, illicit drug use, psychological and medical conditions, and prescribed medications. Nicotine dependence was assessed using the Fagerstrom Test for Nicotine Dependence (FTND; Heatherton, Kozlowski, Frecker, & Fagerstrom, 1991), a six-item measure that produces scores ranging from 0 (low dependence) to 10 (high dependence). Responses to the psychosocial survey were evaluated to determine full eligibility, based on the following exclusion criteria: (1) serious mental or medical condition that would pose an increased risk to participation (e.g., schizophrenia); (2) history of drug abuse or use of benzodiazepines, cocaine, or opiates in the previous 6 months; (3) report smoking marijuana more than 2 times per month; (4) frequent exposure to elevated carbon monoxide (CO; e.g., spouse smokes in home); (5) currently using a smoking cessation treatment (e.g., counseling, nicotine replacement); and (6) frequent use of tobacco products besides cigarettes.
Materials and Set-Up
Participants were shipped a CO meter (Bedfont piCO+ Smokelyzer, calibrated before each delivery) and web camera (Creative Live! Cam Optia). Participants signed a property contract stating that they would return the materials at the conclusion of the study. A detailed study instruction manual and an educational booklet for quitting smoking (National Cancer Institute, 2008) were also provided. Prior to beginning the study, participants scheduled a phone set-up meeting during which they were guided through the study website, received instructions, practiced video submissions until they were familiar with using the CO meter and web camera, and reviewed the study procedures. Participants chose their study start date, which was typically within 1 week of the set-up meeting. Participants also completed a behavioral contract that highlighted critical dates in the study, a pledge to quit smoking, and an acknowledgement of the deposit contract arrangement. All participants were instructed to refrain from using smoking cessation aids but to notify the UFSLC if they began using them. Using cessation aids did not affect deposit earnings.
Mōtiv8 Platform and CO Monitoring
Participants received unique logins and passwords to access the Mōtiv8 system (Dallery et al., 2013). Each participant had a customized homepage, which included a graph of their CO levels throughout the study, a summary of their earnings (updated twice daily along with feedback about their most recent sample’s earnings), and a link to submit a video. Smoking levels were monitored remotely and online using the Mōtiv8 platform. Participants provided evidence of recent smoking by submitting video samples over the Internet using the CO meter and web camera. The submissions took 1–2 min and could be sent from any computer with Internet access. Participants were required to submit two samples per day with a minimum 8-hr intersample interval. Mōtiv8 forced this time constraint by only displaying the “Post Video” button when at least 8 hr had elapsed after submitting the previous sample. To leave a CO sample, participants: (1) showed the CO meter menu screen to the web camera, (2) initiated the CO countdown screen and held breath for 15 s, (3) exhaled completely into the meter, and (4) showed the CO reading to the web camera. After recording the sample, participants manually entered the CO value and submitted the video. They then received an automated confirmation message and were returned to their homepage. Before submitting each CO sample, participants were also asked to report electronically the number of cigarettes they had smoked (0, 0–1, 1–20, or more than 20). These reports had no effect on deposit earnings, and participants were encouraged to answer honestly. All submissions were reviewed daily. Participants adhered to the sample submission procedures, and there were no discrepancies between CO readings and electronic inputs by participants. All CO meters were returned, and there was no evidence of tampering with the devices.
Deposit Contracts
Deposits were made as one lump-sum payment online using PayPal, a popular and secure e-business that manages money transfers and deposits. Participants signed a contract acknowledging that they could recoup the entire deposit, some portion, or none at all, and that the amount they could recoup depended upon their ability to reduce and quit smoking. Further, participants were told that if they dropped out of the study, only their earned portions of the deposit could be recouped. The amount of the deposit was entirely up to the participant. However, to encourage reasonable and responsible deposits, participants were asked to contribute an amount that would be sufficient to motivate them to quit smoking but not an amount that could jeopardize their personal finances.
Deposits were reimbursed on a fixed schedule, such that meeting each treatment goal resulted in the same amount of earnings. There were a total of 28 goals for each participant throughout the study. Therefore, the deposit portion for each sample was the total amount at stake divided by 28. For example, if the total amount at stake was $100, a participant could recoup $3.57 for meeting each goal. If an individual neglected to provide a sample or provided a sample that was above his or her goal, it was considered a goal failure (see below). To allow for some flexibility and uncontrollable circumstances (e.g., power outage), participants could neglect to submit up to two samples without forfeit. For data analysis purposes, all misses were considered goal failures. Monetary amounts for failing to meet treatment goals were donated to the American Lung Association. To encourage adherence to the twice daily video samples, participants could recoup 10% of their deposit if they submitted at least 90% of the required samples during the study, regardless of their smoking status. Deposit earnings were returned to participants via Pay-Pal at the end of the experiment once materials were shipped back.
Abstinence and Reduction Cutoff Levels
Most previous Mōtiv8 studies used CO abstinence cutoffs of less than or equal to 4 parts per million (ppm). Because participants who submitted samples that did not meet their goals forfeited portions of their own money, we selected a more lenient CO cutoff (less than or equal to 6 ppm) to ensure that we would not incorrectly identify a recently abstinent participant as smoking. One participant (Experiment 1, RR002) suffered from chronic obstructive pulmonary disease (COPD), a condition which elevates breath CO. This participant was assigned an adjusted cutoff of 8 ppm (Sato et al., 2003). Cutoff levels for reduction goals were determined for each individual based on their smoking levels during the baseline phase (see Experimental Procedures).
Social Validity
Participants completed a 17-item brief survey that contained closed- and open-ended questions about their experience in and interaction with the program (survey available online as supplemental material). Closed-ended items were worded as statements about the intervention (e.g., “The Internet-based program was helpful in my quit attempt”) to which participants indicated their agreement on a visual analog scale (0–100) with anchors for Strongly Disagree (10), Disagree (30), Neither Agree nor Disagree (50), Agree (70), and Strongly Agree (90). Open-ended items asked what participants liked most and least, found most helpful, and suggested for future treatments.
Experimental Procedures
We used a nonconcurrent multiple baseline across participants design (Watson & Workman, 1981), which included three phases delivered in a fixed order: baseline, reducing, and abstaining.
Baseline
Each participant was assigned randomly to experience either a 4- or 5-day phase (Experiment 1) or a 3-, 4-, or 5-day phase (Experiment 2). The purpose was to collect data on natural smoking levels and to familiarize participants with Mōtiv8 and the video sample submission procedures. Deposits were made just before or during this phase. Participants submitted CO samples twice per day but there were no contingencies in place for smoking or for sample submissions.
Reducing
The reducing phase began immediately after baseline and lasted for 4 days, consistent with other CM studies using Mōtiv8 (Dallery et al., 2013). Participants continued submitting samples twice daily, but contingencies were arranged based on their smoking during the baseline phase. For each CO sample, participants were given reduction goals. These goals were computed such that the last goal during reducing was less than or equal to 6 ppm. Specifically, (1) a participant’s average CO level during baseline was calculated (e.g., 50 ppm); (2) the difference between this average and 6 ppm was determined (e.g., 50–6 ppm = 44); (3) the required amount for each reduction step was calculated (44 ppm ÷ 8 [number of samples during reducing] = 5.5); and (4) the eight goals were assigned (e.g., Goal 1 = average CO - reduction step; 50–5.5 ppm = 45 ppm, Goal 2 = 39, and so on). Participants received their goals the evening prior to beginning reducing. They were instructed to gradually and continuously reduce their smoking and that to meet their final reducing goal they should abstain for 24 hr. Deposit portions were recouped contingent on meeting each goal.
Abstaining
The abstaining phase began immediately following reducing and lasted for 10 days. The procedures were identical to reducing, but the goal for all samples was CO less than or equal to 6 ppm.
Outcomes
The primary outcome was CO level across the experimental phases. As a conservative approach and to be consistent with handling missing samples as goal failures, average baseline values were substituted for missed samples to calculate average CO levels across phases. Secondary measures were percentage of samples meeting goals, longest continuous duration of meeting the CO less than or equal to 6 ppm criterion, self-reported number of cigarettes, acceptability ratings and responses, sample submission rates, and attrition.
EXPERIMENT 1
Method
Participants (N = 9) deposited an amount they felt would motivate them to quit smoking and completed the study as described above.
Results and Discussion
Demographics for the nine participants who enrolled in the study are shown in Table 1. Most participants were between 30 and 60 years old, female, white, and had completed at least some college. Two-thirds of participants resided outside of the immediate study area in other states. All were daily smokers for at least 10 years, most smoked one-half to one pack per day, and most were moderately nicotine-dependent.
Table 1.
Participant Demographics and Deposits
| Experiment 1 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| ID | State | Sex | Age | Race | Education | Weekly income ($) | Cigs/day | Years smoked | FTND | Deposit amount ($) |
| BB001 | TX | M | 49 | White | Grad school | 501–600 | 52.5 | 34 | 7 | 170 |
| RR002 | FL | F | 56 | White | Some college | 501–600 | 20 | 38 | 6 | 50 |
| BH003 | CA | M | 28 | Biracial | Some college | 301–400 | 10 | 14 | 2 | 50 |
| DA005 | KS | F | 31 | White | Some college | >700 | 16 | 13 | 5 | 20 |
| BM007 | FL | F | 41 | White | College grad | 601–700 | 20 | 24 | 7 | 100 |
| MS008 | FL | M | 48 | White | Grad school | 601–700 | 15 | 20 | 6 | 100 |
| KC009 | TX | F | 38 | White | College grad | 100–200 | 11 | 20 | 5 | 100 |
| JR010 | WA | F | 30 | White | Some college | >700 | 17.5 | 17 | 2 | 100 |
| JJ011 | MD | F | 50 | White | Some college | 501–600 | 15 | 35 | 3 | 50 |
| Experiment 2 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| ID | State | Sex | Age | Race | Education | Weekly income ($) | Cigs/day | Years smoked | FTND | Deposit amount/match($) |
| PS001 | CA | F | 28 | White | Grad school | 501–600 | 10 | 7 | 3 | 100/50 |
| KL003 | GA | F | 26 | White | College grad | >700 | 10 | 4 | 3 | 25/25 |
| CG004 | FL | F | 50 | White | Some college | >700 | 20 | 38 | 7 | 25/25 |
| KB005 | IA | F | 59 | White | Some college | >700 | 15 | 40 | 6 | 50/50 |
| AB007 | MN | F | 29 | White | College grad | 601–700 | 10 | 15 | 4 | 50/50 |
| CH008 | VA | F | 48 | White | Grad school | 501–600 | 18 | 20 | 1 | 40/40 |
| CK009 | TN | M | 20 | White | High school | <100 | 20 | 5 | 3 | 25/25 |
| CH011 | OH | F | 58 | White | College grad | >700 | 18 | 22 | 5 | 50/50 |
| CR012 | OH | F | 49 | White | College grad | 401–500 | 12.5 | 30 | 5 | 75/50 |
| NC013 | OK | F | 32 | Biracial | College grad | 401–500 | 12.5 | 7 | 3 | 50/50 |
Note. FTND = Fagerstrom Test for Nicotine Dependence scores.
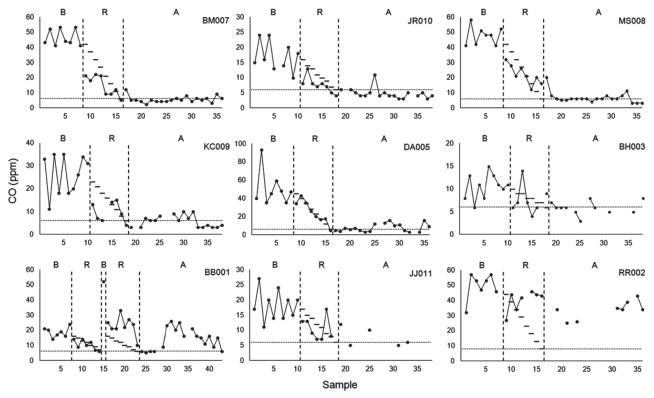
Individual CO data across phases are shown in Figure 1. Decreases in CO corresponded with the introduction of the deposit contract contingencies. During reducing, participants had lower CO levels on average and met 64% (SD = 23.6%) of their goals. Participants who met more reducing goals also tended to meet more goals during the abstaining phase (r = .78, p = .013), but CO levels during the abstaining phase varied. Five participants submitted high numbers of samples meeting the cutoff (BM007, JR010, MS008, KC009, DA005) and met it continuously for an average of 3.7 days (SD = 3.8). One participant met the cutoff briefly but lapsed (BB001). Two participants met the cutoff at low and intermittent rates (BH003, JJ011), and one participant was unable to meet it (RR002). Compared to the 1% of samples that met the CO less than or equal to 6 ppm criterion during baseline, 12% and 47% met it during reducing and abstaining, respectively (Figure 2A).
Figure 1.
Individual carbon monoxide (CO) levels in parts per million (ppm) across phases (Experiment 1). B = baseline, R = reducing, A = abstaining. Horizontal lines indicate reducing and abstaining goals. Note: BB001 experienced an equipment failure on Day 4 of reducing, creating a delay. He elected to restart the study procedures after a brief baseline probe.
Figure 2.
Percentage of carbon monoxide (CO) samples meeting the less than or equal to 6 parts per million (ppm) cutoff across experimental phases for Experiment 1 (A) and Experiment 2 (B). Each dot represents data for a different participant. Horizontal lines represent the means.
Relative to baseline, CO levels during Reducing and Abstaining represented a 45.1% and 58.4% decrease, respectively. Similar decreases occurred for self-reported number of cigarettes smoked during reducing (45.7%) and abstaining (55.4%) compared to baseline. As expected, CO and self-reported cigarettes smoked were highly related (r = .67, p < .001). However, because we chose a more lenient CO cutoff than in previous studies (Dallery et al., 2013; Meredith & Dallery, 2013), some participants were still able to smoke at low levels (33 of 90 samples that met the cutoff reported smoking). However, samples that met the CO less than or equal to 6 ppm criterion averaged just 0.84 (SD = 1.37) cigarettes smoked, a reduction of 92.5% relative to baseline. Two participants reported using additional smoking cessation aids (patch [BM007] and an electronic cigarette [DA005]). Excluding these participants from the analyses decreased the magnitude of the effect (i.e., relative to baseline, 45% vs. 38% CO decrease during reducing and 58% vs. 46% CO decrease during abstaining).
Deposit amounts are displayed in Table 1. In total, $740 was received and $460.39 was reimbursed leaving a surplus of $279.61, which was donated to the American Lung Association. The average deposit for the 14-day goal period was $82.22 (SD = $44.65). For comparison, based on participants’ self-reported number of cigarettes smoked per day and price per pack during screening, the average participant would have spent $81.85 (SD = $61.61) on cigarettes during the same 14-day period. There was a trend between deposit amount and several outcomes. Participants who deposited above the median amount ($75) had higher rates of samples meeting the 6 ppm cutoff (65% vs. 25%), longer durations of meeting the cutoff (3.8 vs. 0.8 days), and submitted more samples overall (95% vs. 72%).
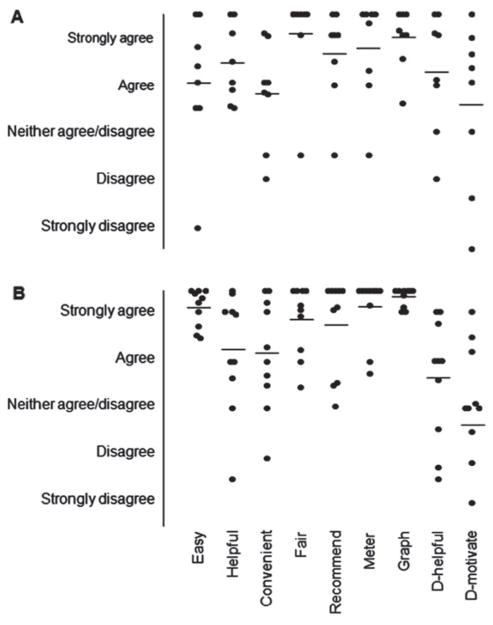
One participant (BH003) did not complete the acceptability questionnaire. Acceptability ratings are shown in Figure 3A. Overall ratings of the treatment were favorable, and on average, participants agreed or strongly agreed that the intervention was easy to use (M = 70.5, SD = 29.4), helpful in their quit attempt (M = 79.0. SD = 16.6), convenient (M = 66.0, SD = 21.8), and fair (M = 91.4, SD = 20.9), that they would recommend it others (M = 82.9, SD = 19.9), and that they liked using the CO meter (M = 85.3, SD = 21.8) and viewing the progress graph (M = 89.8, SD = 12.9). The majority agreed or strongly agreed that the deposit was helpful in their quit attempt (75%) and that the deposit amount they contributed was enough to motivate them to quit smoking (62.5%). There was variability across participants, however, and for most ratings one or two participants disagreed or strongly disagreed with the statement. Five participants referenced self-monitoring and two referenced the deposit as what they liked best. The most common weakness noted by four participants was that leaving samples was not always convenient. Three indicated that that the intervention was too short. Seven of eight participants reported that they would use the current intervention again in the future. Three of these would prefer to use the current treatment combined with nicotine replacement therapy. Recommendations were to make the goal phases longer and to make the treatment compatible with mobile devices.
Figure 3.
Treatment acceptability scores for Experiment 1(A) and Experiment 2 (B). Each dot represents data for a different participant. Horizontal lines represent the means. Responses were given on a visual analog scale ranging from 0–100 with anchors at 10, 30, 50, 70, and 90 corresponding with those on the y-axis. D = deposit.
There was no attrition during this brief study. Overall, 288 of 339 (84.9%) CO samples were submitted, with rates varying across participants. Nearly 80% of missed samples came from three participants (RR002, BH003, and JJ011). The remaining six participants had near perfect submission rates (M = 95.2%).
In sum, results from Experiment 1 suggest that Internet-based self-tailored deposit contracting is feasible, acceptable, and can promote short-term reduction and brief abstinence in some treatment-seeking smokers.
EXPERIMENT 2
Method
All methods were identical to Experiment 1. However, participants were told that the UFSLC would match their deposit amount up to a maximum of $50. Matched amounts were added to the total deposit and reimbursed on the same schedule. Practicality guided the $50 maximum, which is similar to amounts matched in deposit-matching weight loss studies (e.g., Volpp et al., 2008). Clinic-backed vouchers were delivered on a VISA prepaid debit card after the experiment and once materials had been returned for participants who met enough goals to earn their deposit in full and additional vouchers.
Results and Discussion
Participants (N = 10) enrolled in the study and their demographics are shown in Table 1. All 10 participants resided outside of the immediate study area and 9 were out-of-state. All but one participant were female, white, and had completed at least some college education. All participants smoked between one-half and one pack per day and all but one reported low-moderate or moderate nicotine dependence. Smoking histories varied considerably with participants’ ages, from 4–40 years.
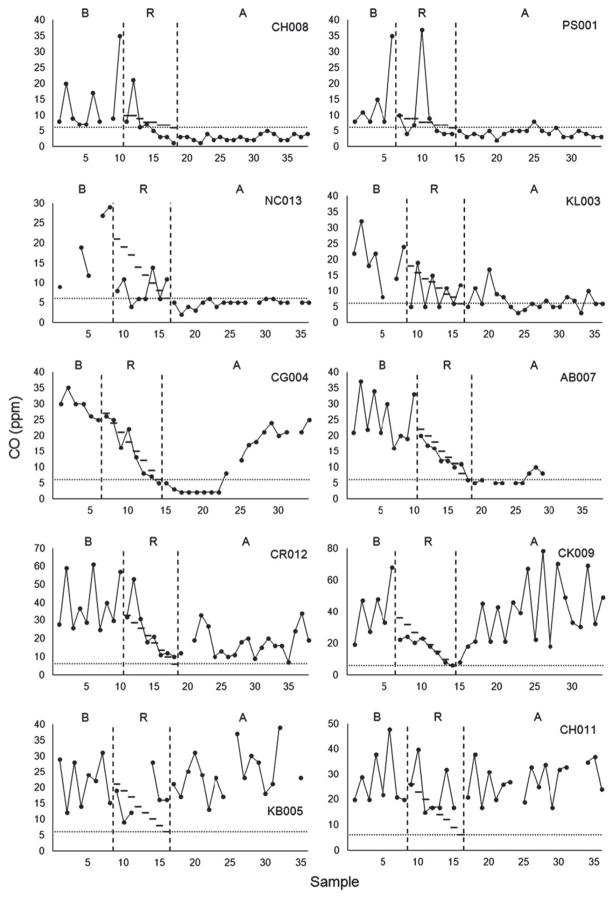
Figure 4 shows participants’ CO levels across phases. During reducing, participants decreased their CO relative to baseline and met 67.3% (SD = 21.3%) of their goals. Meeting goals during the reducing phase was positively but not significantly associated with meeting goals during abstaining (r = .45, p = .19), and CO levels during abstaining varied considerably across participants. Three participants submitted samples meeting the CO less than or equal to 6 ppm cutoff on nearly all occasions during abstaining (CH008, PS001, NC013; ≥90%) and met the cutoff continuously for an average of 8.0 days (SD = 3.5). One (KL003) frequently submitted samples below the cutoff but also submitted several samples above the cutoff. Two participants met the cutoff only briefly during abstaining (CG004, AB007). Two others showed steep decreases in CO during reducing but failed to ever meet the cutoff (CR012, CK009). Finally, two more participants showed relatively little change in CO during abstaining compared to baseline (KB005, CH011). Overall, 0% of samples were below the cutoff during baseline, but 25% and 41.5% were during reducing and abstaining, respectively (Figure 2B). Average CO levels decreased from baseline by 41.2% during reducing. Reduction during abstaining was similar (41.6%), but several participants did not maintain reductions or had CO levels similar to baseline. Reductions in self-reported cigarettes smoked were similar to CO from baseline to reducing (34.5%) and abstaining (55.6%).
Figure 4.
Individual carbon monoxide (CO) levels in parts per million (ppm) across phases (Experiment 2). B = baseline, R = reducing, A = abstaining. Horizontal lines indicate reducing and abstaining goals.
There was a statistically significant relationship between CO and self-reported cigarettes smoked (r = .85, p < .001). Similar to Experiment 1, some participants were able to meet the 6 ppm cutoff while continuing to smoke at low levels (with 41.4% of samples meeting cutoff ). However, these levels were low (M = 1.02, SD = 1.69) and still represented a 93.4% decrease relative to baseline.
Participants’ deposit amounts are displayed in Table 1. A total of $490 (M = $49.00, SD = $23.78) was received, with most participants having contributed $50 or less. For comparison, participants would have spent $57.76 (SD = $22.76) on cigarettes during the 14-day period. The average amount in clinic-backed vouchers that participants could earn was $41.50 (SD = $11.80). The total amount (deposit + match) at risk during the 14-day period for which smoking goals were present averaged $90.50 (SD = $33.54). Four participants (PS001, KL003, CH008, NC013) met enough goals to earn portions of the clinic match. One participant (CH011) declined her deposit reimbursement ($10.71) and elected to donate it instead. In total, $436.95 was reimbursed, leaving a surplus of $53.05, which was donated to the American Lung Association. In contrast to Experiment 1, deposit amounts were not related to smoking outcomes or sample submission rates.
Although there was variability across participants on acceptability (see Figure 3B), on average they agreed or strongly agreed that the intervention was easy to use (M = 92.8, SD = 8.1), helpful (M = 74.4, SD = 25.3), convenient (M = 73.5, SD = 23.6), fair (M = 87.9, SD = 14.8), that they would be likely to recommend it to others (M = 85.7, SD = 20.0), and that they liked using the CO meter (M = 92.9, SD = 13.6) and progress graph (M = 97.3, SD = 4.0). The highest degree of variability was for the two items that evaluated the deposit contract component. A small majority (60%) agreed or strongly agreed that the deposit was helpful but only 30% of participants agreed or strongly agreed that the amount they put down was sufficient to motivate them to quit. Participants liked best the ability to monitor their smoking (80%) and Mōtiv8’s ease of use (30%). Only one participant listed the deposit component as what she liked best (PS001). Nine of ten participants indicated that they would prefer to use the current treatment if they were to attempt to quit again in the future. All but two of these preferred to combine Mōtiv8 with other aids (prescription medication, nicotine replacement, and electronic cigarettes). The most common weaknesses were that the treatment was too short (40%) and that there was no counseling (20%). Suggestions for future treatments were idiosyncratic and included adding medications, updating the educational resources, using a mobile platform, and eliminating the reducing phase entirely.
One participant (AB007) withdrew from the study halfway through the abstaining phase and noted leaving because her spouse continued to smoke, which made sustained abstinence too difficult. Rates of video sample submission were high overall. Of the required 360 submissions, 329 (91.4%) were submitted.
Similar to Experiment 1, these findings demonstrate that Internet-based deposit contracting can facilitate smoking reductions and brief abstinence among some smokers desiring to quit. Including clinic-based deposit matching did not, however, produce a marked change in any measured outcomes relative to Experiment 1.
GENERAL DISCUSSION
These studies were among the first to evaluate Internet-based CM for smoking with self-tailored deposit contracts and addressed limitations from earlier deposit contracting studies for smoking. The experimental design offered support that changes in smoking were due to the deposit contingencies and not to other aspects, such as self-monitoring. Verifying smoking twice daily allowed for better resolution of smoking over time compared to trials in which smoking was assessed at longer intervals (e.g., Halpern et al., 2015; White et al., 2013). In addition, participants could contact the deposit contingency quickly for reducing and more frequently than in previous studies. Finally, the intervention did not include additional cessation aids, which helped isolate the effects of the deposit arrangement.
To our knowledge, this is one of the first reports of a fully remote technology-based CM intervention targeting smoking cessation. That is, there was no in-person contact with participants during the intervention (except equipment delivery for two local participants in Experiment 1 to avoid unnecessary costs); all procedures were conducted via computers and mobile phones. The 19 participants who enrolled in the studies resided across 13 states, which illustrates the broad reach of technology-based CM for smoking. Its extensive reach could be particularly useful to target geographical areas where Internet access is available but clinics are too distant to permit in-person CM. Technology-based CM for smoking may also be useful to address disparities in accessing smoking cessation treatment. Increases in Internet access, especially through smartphone devices, continue to bridge the digital divide previously noted across income levels, race, and educational attainment (Pew Research Center, 2015)—all areas associated with rates of cigarette smoking (Agaku, King, & Dube, 2014). Importantly, if technology-based CM is delivered remotely, it may be necessary to use deposit contracts to minimize or eliminate “sandbagging” to gain entry into an intervention that offers incentives. Deposits may deter nonsmokers from posing as smokers to gain entry to an incentive-based intervention, a common concern expressed by those who oppose incentive-based health interventions (Giles, Sniehotta, McColl, & Adams, 2015).
The results were encouraging and suggest that for some individuals seeking to quit, deposit contracting may be a useful aid to reduce and abstain briefly from smoking. Across the two deposit arrangements during abstaining, 10 of 19 participants reduced their smoking by more than 50%, as evidenced in CO level submissions. Moreover, 14 of 19 submitted at least one sample of less than or equal to 6 ppm, and 10 of 19 met the criterion for at least 2 continuous days. Both experiments, however, did not produce outcomes as robust as Dallery et al. (2008) or Halpern et al. (2015). One possibility is that the escalating magnitude with reset schedule used in Dallery et al. (2008) produced better outcomes (Roll, Higgins, & Badger, 1996). We used a fixed schedule for its simplicity in treatment delivery and because of concerns that low deposits on an escalating schedule would begin at insufficient magnitudes to encourage reduction (e.g., a $20 deposit would begin at $0.12 and increase by $0.03 per sample). However, employing escalating schedules may have promoted more sustained abstinence in several participants who lapsed frequently. Another explanation is the large voucher amounts ($650–$3650) used in Halpern et al. (2015), which were comparable to those seen in high-magnitude CM studies.
Acceptability ratings were favorable and similar to other Mōtiv8 studies (e.g., Meredith & Dallery, 2013; Raiff et al., 2013). One notable difference was ratings on convenience, which were lower in the present study than previous Mōtiv8 studies. Some participants found the twice daily submissions from a home computer burdensome. As Mōtiv8 transitions from a research tool to a clinical application, improving its flexibility and portability will be critical. Participant suggestions to extend Mōtiv8 to mobile devices represent a promising direction already underway (Hertzberg et al., 2013; Meredith et al., 2014) that may afford exciting opportunities to evaluate new features (e.g., location-based support) and could further increase submission rates.
The present arrangements completely eliminated voucher costs, even when incorporating a clinic-match. After payments to 19 participants, $332.66 was left in surplus and donated to charity. In contrast, the standard CM arrangement delivered by Dallery et al. (2008) to four participants cost nearly $180 over a similar duration. Future studies may explore other ways to use deposit surpluses, such as to offset expenses or improve uptake or efficacy. For example, forfeited funds could be used as supplemental incentives for individuals who meet certain treatment milestones (Volpp et al., 2008). This approach increases voucher magnitudes at no cost and for some may be more efficacious if giving money to someone who was able to achieve their goals is more aversive than donating to charity. Popular deposit contract sites such as http://www.stickk.com direct forfeitures to organizations inconsistent with one’s views (i.e., anti-charities; e.g., a registered Republican’s losses are donated to the Democratic National Committee), which might further improve efficacy.
Participants’ deposit amounts varied considerably from as little as $20 to as much as $170. Consistent with previous research (Gine et al., 2010), Experiment 1 showed deposit amounts may be associated with better outcomes. However, we did not observe this in Experiment 2, and participants tended to contribute less in Experiment 2. One explanation is that the clinic match reduced the amount and range of deposits, which limited our ability to see this relationship. Previous research on web-based smoking treatments has shown that incorporating other tailored intervention components can improve engagement, abstinence, and acceptability (e.g., Strecher, Shiffman, & West, 2004; Strecher et al., 2008). Although no data were collected on preference, one can assume that given a choice, individuals would prefer a customized deposit. However, whether participants are able to select sufficient amounts to help motivate them to quit smoking is less clear. Most participants reported that the deposit contract was helpful but many reported that the amount they chose was not sufficient to motivate them to quit. Future studies could explore strategies and assessments that may encourage deposits sufficient to promote abstinence (e.g., emphasizing opportunity costs; Frederick, Novemsky, Wang, Dhar, & Nowlis, 2009). A recent meta-analysis of deposit contracts for weight loss found that participant-selected deposits were associated with greater weight loss than researcher-selected deposits (Sykes-Muskett, Prestwich, Lawton, & Armitage, 2015). Future work will be necessary to determine whether a similar finding applies to quitting smoking.
Whether deposit contracts for smoking cessation will succeed as a viable treatment option depends critically on their uptake (Halpern et al., 2012). Previous studies have found uptake rates ranging from less than 2% (Jeffery et al., 1988) to between 10.5% and 13.7% (Gine et al., 2010; Halpern et al., 2015; White et al., 2013). Only one study compared uptake rates of deposit contracting with alternative incentive arrangements and found significantly lower rates of uptake when deposits were required (13.7% vs. 90.0%). In the current experiments, uptake rates could not be obtained because it is unknown how many smokers viewed recruitment materials. Future studies should evaluate the effects that self-tailoring deposits and matching have on uptake and compare them to the effects of standard CM and other commonly used smoking treatments.
Despite encouraging outcomes, there were limitations that future studies should address. First, the design ruled out the effects of self-monitoring, but the duration across participants’ baselines was short. The short baselines and small difference in their durations across participants minimized the time between receiving materials and starting the intervention, but future designs with longer durations would improve the ability to detect stability and experimental control. Second, because the deposit contract contained other features (e.g., a behavioral contract), these may have had an effect for some participants. Designs that include random assignment and a noncontingent deposit control group would be ideal. Third, the average treatment response was favorable, but there was considerable variability across participants. During the reducing phase, some participants showed systematic reductions that aligned closely with their goals (e.g., DA005), whereas others appeared insensitive (NC013). During Abstaining, most participants reduced their smoking, which may confer some health benefits (Pisinger & Godtfredsen, 2007) and may lead to cessation (Klemperer & Hughes, 2015), but only one participant met all treatment goals continuously without missing samples during abstaining. Further, two participants (CK009, KB005) submitted a small number of samples during this period that exceeded their baseline CO levels. Modifying parameters of the deposit contract, such as creating longer or more gradually moving reduction requirements with percentile schedules, delivering incentives immediately rather than at the end of the study, or increasing the frequency of incentive delivery early on during treatment may improve outcomes among the group of participants who never met the 6 ppm cutoff (5 of 19) or who failed to meet more stringent reducing goals (e.g., RR002, CH011). Combining these changes with other evidence-based treatments, as suggested by several participants, may also produce more robust effects. Integrating additional cessation aids could be based on individual preference but also on initial treatment response (Hughes, 2008). The ability of Mōtiv8 and developing technologies to frequently assess smoking makes it an ideal platform for testing adaptive interventions, which have shown promise for response to pharmacological treatments (e.g., Rose & Behm, 2014). Fourth, consistent with a previous Mōtiv8 study using a higher cutoff (Dallery, Glenn, & Raiff, 2007), several participants smoked at very low rates while still meeting the cutoff. Because participants could lose substantial sums of their own money for failing to meet their goals, we chose a more lenient cutoff than in previous studies. Future studies should use a more stringent cutoff to eliminate these occurrences, which has been successful in CM studies using Mōtiv8 (e.g., Dallery et al., 2008; 2013). Finally, these experiments evaluated very short-term outcomes in small homogenous samples. More work is necessary to determine if deposit contracting can be implemented for longer durations, whether effects persist at follow-up, and if subgroups are more or less likely to enroll and have success. A common finding in CM is high rates of relapse following removal of the contingencies, which cannot be in place indefinitely, due to high costs. By contrast, deposit contracts may be used at little to no cost and for extensive periods of time, which make them a great candidate as relapse prevention tools.
In summary, these experiments offer preliminary evidence that self-tailored Internet-based deposit contract arrangements may be feasible, acceptable, and promote short-term reduction and brief abstinence among some smokers. More research is needed to determine individual and intervention factors that influence their long-term effects and uptake. Given recent trends toward increased use of financial incentives to encourage healthy behaviors (Loewenstein, Asch, & Volpp, 2013), deposit contracts are a promising option that could have a significant public health impact.
Acknowledgments
This work was supported by the University of Florida Graduate School and completed in partial fulfillment of the requirements of the PhD degree by the first author.
References
- Agaku IT, King BA, Dube SR. Current cigarette smoking among adults – United States, 2005–2012. Morbidity and Mortality Weekly Report. 2014;63:29–34. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6302a2.htm. [PMC free article] [PubMed] [Google Scholar]
- Amass L, Kamien JB. Funding contingency management in community treatment clinics: Use of community donations and clinic rebates. In: Heil SH, editor. Contingency management in substance abuse treatment. New York, NY: Guilford Press; 2008. pp. 280–297. [Google Scholar]
- Bowers TG, Winett RA, Frederiksen LW. Nicotine fading, behavioral contracting, and extended treatment: Effects on smoking cessation. Addictive Behaviors. 1987;12:181–184. doi: 10.1016/0306-4603(87)90024-4. [DOI] [PubMed] [Google Scholar]
- Dallery J, Glenn IM, Raiff BR. An Internet-based abstinence reinforcement treatment for cigarette smoking. Drug and Alcohol Dependence. 2007;86:230–238. doi: 10.1016/j.drugalcdep.2006.06.013. [DOI] [PubMed] [Google Scholar]
- Dallery J, Meredith S, Glenn IM. A deposit contract method to deliver abstinence reinforcement for cigarette smoking. Journal of Applied Behavior Analysis. 2008;41:609–615. doi: 10.1901/jaba.2008.41-609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dallery J, Raiff BR, Grabinski MJ. Internet-based contingency management to promote smoking cessation: A randomized controlled study. Journal of Applied Behavior Analysis. 2013;46:750–764. doi: 10.1002/jaba.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliot R, Tighe T. Breaking the cigarette habit: Effects of a technique involving threatened loss of money. The Psychological Record. 1968;18:503–515. [Google Scholar]
- File T, Ryan C. Computer and internet use in the United States: 2013. 2014 (Report No. ACS-28). Retrieved from US Census Bureau website: https://www.census.gov/history/pdf/2013comp-internet.pdf.
- Frederick S, Novemsky N, Wang J, Dhar R, Nowlis S. Opportunity cost neglect. Journal of Consumer Research. 2009;36:553–561. doi: 10.1086/599764. [DOI] [Google Scholar]
- Giles EL, Sniehotta FF, McColl E, Adams J. Acceptability of financial incentives and penalties for encouraging uptake of healthy behaviours: Focus groups. BMC Public Health. 2015;15:58. doi: 10.1186/s12889-015-1409-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gine X, Karlan D, Zinman J. Put your money where your butt is: A commitment contract for smoking cessation. American Economic Journal: Applied Economics. 2010;2:213–235. doi: 10.1257/app.2.4.213. [DOI] [Google Scholar]
- Halpern SD, Asch DA, Volpp KG. Commitment contracts as a way to health. British Medical Journal. 2012;344:e522. doi: 10.1136/bmj.e522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halpern SD, French B, Small DS, Saulsgiver K, Harhay MO, Audrain-McGovern, … Volpp KG. Randomized trial of four financial-incentive programs for smoking cessation. New England Journal of Medicine. 2015;372:2108–2117. doi: 10.1056/NEJMoa1414293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom Test for Nicotine Dependence: A review of the Fagerstrom Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Hertzberg JS, Carpenter VL, Kirby AC, Calhoun PS, Moore SD, Dennis MF, … Beckham JC. Mobile contingency management as an adjunctive smoking cessation treatment for smokers with posttraumatic stress disorder. Nicotine & Tobacco Research. 2013;15:1934–1938. doi: 10.1093/ntr/ntt060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes J. An algorithm for choosing among smoking cessation treatments. Journal of Substance Abuse Treatment. 2008;34:426–432. doi: 10.1016/j.jsat.2007.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeffery RW, Gerber WM, Rosenthal BS, Lindquist RA. Monetary contracts in weight control: Effectiveness of group and individual contracts of varying size. Journal of Consulting and Clinical Psychology. 1983;51:242–248. doi: 10.1037/0022-006X.51.2.242. [DOI] [PubMed] [Google Scholar]
- Jeffery RW, Pheley AM, Forster JL, Kramer FM, Snell MK. Payroll contracting for smoking cessation: A worksite pilot study. American Journal of Preventive Medicine. 1988;4:83–86. [PubMed] [Google Scholar]
- Kirby KC, Benishek LA, Dugosh KL, Kerwin ME. Substance abuse treatment providers’ beliefs and objections regarding contingency management: Implications for dissemination. Drug and Alcohol Dependence. 2006;85:19–27. doi: 10.1016/j.drugalcdep.2006.03.010. [DOI] [PubMed] [Google Scholar]
- Klemperer EM, Hughes JR. Does the magnitude of reduction in cigarettes per day predict smoking cessation? A qualitative review. Nicotine & Tobacco Research. 2015;18:88–92. doi: 10.1093/ntr/ntv058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lando HA. Aversive conditioning and contingency management in the treatment of smoking. Journal of Consulting and Clinical Psychology. 1976;44:312. doi: 10.1037/0022-006X.44.2.312. [DOI] [PubMed] [Google Scholar]
- Lando HA. Successful treatment of smokers with a broad-spectrum behavioral approach. Journal of Consulting and Clinical Psychology. 1977;45:361–366. doi: 10.1037/0022-006X.45.3.361. [DOI] [PubMed] [Google Scholar]
- Loewenstein G, Asch DA, Volpp KG. Behavioral economics holds potential to deliver better results for patients, insurers, and employers. Health Affairs. 2013;32:1244–1250. doi: 10.1377/hlthaff.2012.1163. [DOI] [PubMed] [Google Scholar]
- Meredith SE, Dallery J. Investigating group contingencies to promote brief abstinence from cigarette smoking. Experimental and Clinical Psychopharmacology. 2013;21:144–154. doi: 10.1037/a0031707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meredith SE, Robinson A, Erb P, Spieler CA, Klugman N, Dutta P, … Dallery J. A mobile-phone-based breath carbon monoxide meter to detect cigarette smoking. Nicotine & Tobacco Research. 2014;16:766–773. doi: 10.1093/ntr/ntt275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Cancer Institute. Clearing the air: Quit smoking today. 2008 Retrieved from http://smokefree.gov/sites/default/files/pdf/clearing-the-air-accessible.pdf.
- Paxton R. The effects of a deposit contract as a component in a behavioural programme for stopping smoking. Behaviour Research and Therapy. 1980;1:45–50. doi: 10.1016/0005-7967(80)90068-6. [DOI] [PubMed] [Google Scholar]
- Paxton R. Deposit contracts with smokers: Varying frequency and amount of repayments. Behaviour Research and Therapy. 1981;19:117–123. doi: 10.1016/0005-7967(81)90035-8. [DOI] [PubMed] [Google Scholar]
- Paxton R. Prolonging the effects of deposit contracts with smokers. Behaviour Research and Therapy. 1983;21:425–433. doi: 10.1016/0005-7967(83)90012-8. [DOI] [PubMed] [Google Scholar]
- Petry NM. Contingency management treatments: Controversies and challenges. Addiction. 2010;105:1507–1509. doi: 10.1111/j.1360-0443.2009.02879.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Research Center. U.S. smartphone use in 2015. 2015 Retrieved from Pew Research Center website: http://www.pewinternet.org/2015/04/01/us-smartphone-use-in-2015/
- Pisinger C, Godtfredsen NS. Is there a health benefit of reduced tobacco consumption? A systematic review. Nicotine & Tobacco Research. 2007;9:631–646. doi: 10.10801/14622200701365327. [DOI] [PubMed] [Google Scholar]
- Raiff BR, Jarvis BP, Turturici M, Dallery J. Acceptability of an Internet-based contingency management intervention for smoking cessation: Views of smokers, nonsmokers, and health-care professionals. Experimental and Clinical Psychopharmacology. 2013;21:204–213. doi: 10.1037/a0032451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roll JM, Higgins ST, Badger GJ. An experimental comparison of three different schedules of reinforcement of drug abstinence using cigarette smoking as an exemplar. Journal of Applied Behavior Analysis. 1996;29:495–505. doi: 10.1901/jaba.1996.29-495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose JE, Behm FM. Combination treatment with varenicline and bupropion in an adaptive smoking cessation program. American Journal of Psychiatry. 2014;171:1199–1205. doi: 10.1176/appi.ajp.2014.13050595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato S, Nishimura K, Koyama H, Tsukino M, Oga T, Hajiro T, … Mishima M. Optimal cutoff level of breath carbon monoxide for assessing smoking status in patients with asthma and COPD. Chest. 2003;124:1749–1754. doi: 10.1378/chest.124.5.1749. [DOI] [PubMed] [Google Scholar]
- Schlam TR, Baker TB. Interventions for tobacco smoking. Annual Review of Clinical Psychology. 2013;9:675–702. doi: 10.1146/annurev-clinpsy-050212-185602.2012.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sigmon SC, Patrick ME. The use of financial incentives in promoting smoking cessation. Preventive Medicine. 2012;55:S24–S32. doi: 10.1016/j.ypmed.2012.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh NN, Leung JP. Smoking cessation through cigarette-fading, self-recording, and contracting: Treatment, maintenance, and long-term followup. Addictive Behaviors. 1988;13:101–105. doi: 10.1016/0306-4603(88)90033-0. [DOI] [PubMed] [Google Scholar]
- Spring FL, Sipich JF, Trimble RW, Goeckner DJ. Effects of contingency and noncontingency contracts in the context of a self-control-oriented smoking modification program. Behavior Therapy. 1978;9:967–968. doi: 10.1016/S0005-7894(78)80038-0. [DOI] [Google Scholar]
- Strecher VJ, McClure JB, Alexander GL, Chakraborty B, Nair VN, Konkel JM, … Pomerleau OF. Web-based smoking-cessation programs: Results of a randomized trial. American Journal of Preventive Medicine. 2008;34:373–381. doi: 10.1016/j.amepre.2007.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strecher VJ, Shiffman S, West R. Randomized controlled trial of a web-based computer-tailored smoking cessation program as a supplement to nicotine patch therapy. Addiction. 2004;100:682–688. doi: 10.1111/j.1360-0443.2005.01093.x. [DOI] [PubMed] [Google Scholar]
- Sykes-Muskett BJ, Prestwich A, Lawton RJ, Armitage CJ. The utility of monetary contingency contracts for weight loss: A systematic review and meta-analysis. Health Psychology Review. 2015;9:434–451. doi: 10.1080/17437199.2015.1030685. [DOI] [PubMed] [Google Scholar]
- Volpp KG, John LK, Troxel AB, Norton L, Fassbender J, Loewenstein G. Financial incentive-based approaches for weight loss: A randomized trial. Journal of the American Medical Association. 2008;300:2631–2637. doi: 10.1001/jama.2008.804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson PJ, Workman EA. The non-concurrent multiple baseline across-individuals design: An extension of the traditional multiple baseline design. Journal of Behavior Therapy and Experimental Psychiatry. 1981;3:257–259. doi: 10.1016/0005-7916(81)90055-0. [DOI] [PubMed] [Google Scholar]
- White JS, Dow WH, Rungruanghiranya S. Commitment contracts and team incentives: A randomized controlled trial for smoking cessation in Thailand. American Journal of Preventive Medicine. 2013;45:533–542. doi: 10.1016/j.amepre.2013.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winett RA. Parameters of deposit contracts in the modification of smoking. The Psychological Record. 1973;23:49–60. [Google Scholar]