Abstract
Background
Vaccine preventable diseases are making a comeback in the US. However, research is lacking on illness representations of vaccine preventable diseases and their application in improving childhood immunization.
Objective
We utilized the common sense model of self-regulation to examine illness representations of pertussis and their associations with child’s receipt of any vaccine, up-to-date vaccination status, and mothers’ intentions to follow the recommended vaccination schedule in the future.
Methods
We developed vaccine worry and vaccine hassles scales to assess mothers’ worries and hassles for child vaccination, and used an open ended question to assess mother’s illness representations of pertussis. We surveyed mothers with children <3 years old (N = 160) in the Appalachian state of West Virginia, which only allows medical vaccine exemptions.
Results
Some children (5.0%) had received no vaccination, 15.0% were not up-to-date with the recommended vaccination schedule, and 13.8% mothers reported no intention to follow the recommended schedule in future (future intention). Illness representations included identity (17.8%), timeline (61.8%), consequences (58.6%), cause (35.0%), and cure/control (56.7%). Higher vaccine worry was associated with child receiving no vaccine. Not using daycare, higher vaccine worry, and difficulty breathing (identity) were associated with child not being up-to-date. Higher vaccine worry, cough (identity), and belief that vaccines are ineffective (cure/control) were associated with no future intention.
Conclusions
Vaccination interventions need to address mothers’ worry regarding vaccine safety. ‘Common Sense’ beliefs regarding vaccines need to be reconciled with scientific data about vaccine safety and effectiveness, even among those with high socio-economic status in a strict vaccination state.
Keywords: Illness representations, Pertussis, Vaccination, Child health, Appalachia
Introduction
The United States is experiencing a large outbreak of pertussis (whooping cough) (Cherry 2012). Nearly 33,000 cases of pertussis were reported during 2014, a 15% increase from 2013, with over 500 childhood cases directly preventable through routine vaccination (CDC Provisional pertussis surveillance report 2014). A major cause of these pertussis outbreaks is the increasing rates of exemption from mandatory vaccinations (Glanz et al. 2009), with pertussis vaccination seen by parents as less important than others (Salmon et al. 2005). These mandatory vaccinations for children up to 3 years of age include hepatitis B (HepB); diphtheria, tetanus, pertussis (DTaP); Haemophilus influenzae type b (Hib); polio (IPV); measles, mumps, rubella (MMR); varicella, pneumococcal disease (PCV); hepatitis A (HepA); and rotavirus (RV) (CDC Schedules 2015). The Appalachian state of West Virginia (WV) has one of the strictest policies for mandatory vaccinations and allows medical exemptions only (Bradford and Mandich 2015). For entry into a licensed childcare center in WV, the first doses of Hep B, DTaP, Hib, IPV, and PCV are required at the age of 2–3 months and at 4–5 months (West Virginia Department of Health and Human Resources 2015). Despite strict vaccination exemption policy, the childhood immunization rates are lower in West Virginia for most vaccines as compared to the national average. For example, immunization rates for children aged 19–35 months in West Virginia (vs national average) in 2014 included MMR (≥1 dose): 86.7% (91.9%); DTaP (≥4 doses): 78.6% (84.6%); HepB at birth: 68.3% (72.4%); HepA (≥2 doses): 65.7% (59.6%); RV: 69.6% (73.2%), and series of all recommended vaccines: 64.9% (72.2%) (Hill 2016). Unfortunately, these vaccination rates may decline further due to vaccination exemptions and may further complicate efforts to eradicate these diseases (Omer et al. 2009).
Vaccination is considered one of the ten greatest achievements of public health (CDC 2011). However, public attention has recently shifted to unsubstantiated or harmless adverse events related to vaccination (Carrillo-Marquez and White 2013). Mothers who believe that vaccines are unsafe are more likely to delay or refuse vaccines (e.g., Smith et al. 2011; Yaqub et al. 2014). Parental concerns about vaccines include the risk of autism from vaccines, the harm from vaccine ingredients such as thimerosal, pain from vaccines (e.g., Kennedy et al. 2011; Luthy et al. 2009), and the number of vaccines being received by children and their combinations (Carrillo-Marquez and White 2013; Kennedy et al. 2011). However, numerous studies have found vaccines to be safe with no association to autism (Maglione et al. 2014). Other common barriers to child immunization include lack of access to healthcare provider (Dempsey et al. 2011), low household income (Gust et al. 2004; Wu et al. 2008), low perceived severity, low perceived risk of vaccine preventable diseases (Benin et al. 2006; Wu et al. 2008), and low trust in pediatricians (Benin et al. 2006).
Most studies of vaccination non-adherence have focused on specific communities which have historically had a higher rate of vaccine exemptions (e.g., Adorador et al. 2011; Vannice et al. 2011). These communities have different demographic characteristics than WV. Areas with fewer exemptions such as WV have been understudied and may portend future challenges even with the application of stricter standards. A previous study on child immunization in WV found that lack of health professionals, lack of health insurance, and limited access to immunization clinics were barriers to vaccination (Gore et al. 1999). However, this study was conducted nearly 20 years ago in a different vaccination context and is clearly a different phenomenon than that noted amongst wealthy, educated communities of the US. Thus, a more up-to-date understanding of vaccination behavior is needed in a state where vaccination is largely mandatory.
Parents’ illness representations regarding vaccine preventable diseases may be important predictors of their vaccination behavior, but they have not been investigated in a systematic way. We utilized the Common Sense Model of Self-Regulation (CSM-SR), which is a widely used theoretical framework for investigating an individual’s illness representations of a disease, to examine child vaccination (Leventhal et al. 2003). The CSM-SR posits that a health threat leads to cognitive illness representations (e.g., beliefs about pertussis) and emotional representation (e.g., worry). The cognitive illness representations depict parents’ common or ‘lay’ understanding of an illness. Parents utilize these illness representations to make sense of the symptoms of a disease (e.g., pertussis) and to guide their coping behaviors from the disease (e.g., vaccination).
Cognitive representations include: (1) identity: perceived disease symptoms, (2) timeline: perceived duration of disease (acute/chronic)/age of disease onset, (3) Consequences: perceptions of what will happen as a result of the disease (e.g., economic burden), (4) cause: beliefs about disease etiology (e.g., bacteria, stress), and (5) cure/control: beliefs about disease cure or prevention (Leventhal et al. 2003). These illness representations prompt specific action plans to control the health threat (e.g., child immunization), which are then appraised according to their success in managing the threat (Leventhal et al. 2003). This self-regulation of health behavior occurs in the context of an individual’s self-system, which consists of socio-demographic characteristics of the individual and barriers to health behavior (Shiloh 2006).
Despite strict vaccination exemption policy, childhood immunization rates in WV are lower than national average. Further, an increasing demand for non-medical vaccine exemptions in WV on the basis of religious, moral, and personal beliefs (West Virginians for vaccination exemption) may lead to the same sorts of pertussis outbreaks in WV as seen in other regions (Atwell et al. 2013). Therefore, it is critical to examine the factors affecting immunization of children in a strict vaccination exemption community. We examined illness representations of pertussis, and worry and hassle to immunization among mothers in WV, and their associations with child’s receipt of any vaccine, up-to-date vaccination status, and mothers’ future intention for her child to follow the recommended vaccination schedule.
Methods
Participants and Procedure
The current study was part of a larger project in Health Outcomes conducted among mothers of children under 3 years of age. This study includes the findings on vaccination of children by the participants. Participants were women who could read and write in English, had at least one child under 3 years of age, and resided in WV.
Following Institutional Review Board (IRB) approval from West Virginia University (WVU), cognitive interviews were conducted with eight mothers of children under 3 years of age in West Virginia to examine the face validity of this survey. Participants were stopped at a minimum of every five questions during the interview and the questionnaire was revised according to their feedback. After cognitive interviews, we designed an online survey using the approved survey questions and advertised the survey web link on social media (e.g., Facebook parenting groups), WVU list-serves, community flyers (physicians’ offices, daycare), and a WV Extension newsletter. The survey included a consent letter and a questionnaire to assess illness representations, vaccine hassles, worry, and behavior. The final study sample size included 160 mothers with children below 3 years of age (Fig. 1). Participants excluded from the study were not significantly different in demographic characteristics of age, race, and marital status (p > .05) as compared to the final study sample.
Fig. 1.
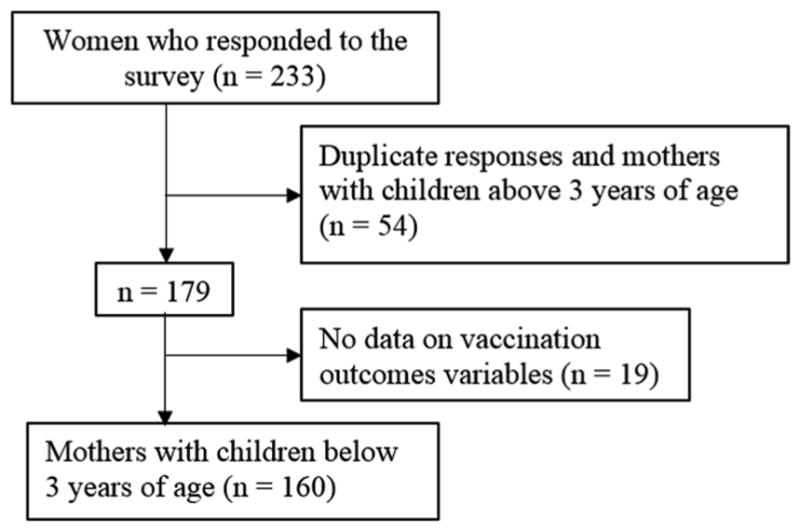
Study sample flowchart
Measures
Self-system factors included mothers’ demographic characteristics and vaccine hassles assessed by our newly-developed vaccine hassles scale (Table 1). To assess emotional representations, we developed a vaccine worry scale (Table 1). We selected separate pools of validated survey items for the vaccine worry and vaccine hassles scales from previous studies on commonly perceived parental worries about (Kennedy et al. 2011; Shui et al. 2006) and barriers to immunization (Beel et al. 2013; Niederhauser and Markowitz 2007; Topuzoglu et al. 2007). Items were selected and revised after critical discussion among the authors. We conducted separate validity and reliability tests for each scale to select final items for vaccine worry and hassles scales. We also utilized a 6-item short-form of the Profile of Mood States (POMS) scale to assess distress among mothers (Cronbach alpha = 0.89) (Lebo and Nesselroade 1978).
Table 1.
Vaccine worry and vaccine hassles scales—reliability, factor analyses, and participants’ responses
| Scales (Cronbach’s alpha, Eigen-value) | Scale items | Single factor loadings | Participants’ responses, % (N = 160) | ||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Strongly disagree | Disagree | Neither agree nor disagree | Agree | Strongly agree | |||
| Vaccine Worry (0.89, 2.67) | I am worried that vaccines could harm my child | 0.90 | 16.3 | 28.1 | 15.0 | 30.6 | 10.0 |
| I am worried that vaccines could lead to many diseases | 0.76 | 30.0 | 40.0 | 16.9 | 7.5 | 5.6 | |
| I am concerned about vaccines side effects | 0.81 | 12.5 | 20.0 | 13.1 | 43.8 | 10.6 | |
| I am concerned that vaccines could be linked to autism or other learning disabilities | 0.80 | 36.3 | 24.4 | 15.6 | 13.7 | 10.0 | |
| Vaccine hassles (0.74, 1.98) | It is difficult to take time off work for vaccination | 0.37 | 47.5 | 31.3 | 13.1 | 8.1 | 0 |
| Vaccines are costly | 0.62 | 35.0 | 38.1 | 14.4 | 11.3 | 1.2 | |
| There are too many recommended vaccines | 0.80 | 28.1 | 28.8 | 19.4 | 15.0 | 8.7 | |
| I don’t have access to vaccination facility | 0.42 | 68.8 | 27.5 | 3.7 | 0 | 0 | |
| I am against the way vaccines are made | 0.80 | 37.5 | 28.8 | 19.4 | 8.1 | 6.2 | |
To assess cognitive illness representations, we used an open-ended question: “Please tell us what you know about Whooping cough (Pertussis)?” (Weinman and Petrie 1997). We coded the participants’ responses to this question into the five domains of illness representations: identity, time-line, consequences, cause, and cure/control. We also utilized a 6-item short-form of the Profile of Mood States (POMS) scale to assess distress among mothers (Cronbach alpha = 0.89) (Lebo and Nesselroade 1978). The three main outcome health behaviors were receipt of any vaccine (Has your child received any vaccination?), up-to-date status with recommended vaccination schedule (Did your child receive all the recommended vaccinations for his/her age?), and intention to vaccinate children in the future (Are you planning to follow the recommended vaccination schedule in the future?). The second question for up-to-date status was skipped for those who responded “no” to the first question (i.e., did not receive any vaccination).
Qualitative Analysis
We used immersion-crystallization technique with CSM-SR model to generate codes from participants’ responses and categorize them into the five domains of illness representations of pertussis (Borkan 1999). Immersion-crystallization is an iterative process of detailed textual review of data (immersion) combined with reflection, intuitive insights, and identification of common themes (crystallization) within the data (Crabtree and Miller 1999). We followed an open coding scheme to first develop codes from participants’ responses in a series of iterative steps. Two study authors independently read participants’ responses and assigned codes to recurrent beliefs or perceptions regarding pertussis. The inter-rater reliability was examined with Cohen’s Kappa value of 0.85 (McHugh 2012). The subsequent responses were analyzed using constant comparison with existing codes. The codes were reconstructed or new codes were added as new insights emerged from participants’ responses. The resulting codes were then categorized in five broader themes of cognitive illness representations from the CSM-SR—(1) identity: participants described ‘cough’, ‘difficulty breathing’, and ‘respiratory infection’ as common characteristics of pertussis; (2) Timeline: ‘Age of onset’ and ‘duration of disease’ constituted the timeline of pertussis; (3) Consequences: Participants considered pertussis to be a ‘life-threatening’ disease; (4) Cause: Most common reported causes of pertussis included ‘pathogen’, ‘non-vaccination’, ‘low herd immunity’, ‘contagion’, and ‘many bacterial strains’; (5) Cure/control: Some mothers considered vaccines to be ‘necessary’ while others described vaccines to be ‘ineffective’ in controlling pertussis. Mothers also noted the recent ‘increase in incidence’ of pertussis as lack of control (Leventhal et al. 2003). Table 3 includes the frequencies and percentages of codes and the five domains from CSM-SR.
Table 3.
Associations of Mothers’ Cognitive Illness Representations of Pertussis with Child Immunization
| Total % (N = 157) | Receipt of any vaccine, row % | Up-to-date status, row % | Future intention, row % | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||
| Yes (n = 149) | No (n = 8) | Sig | Yes (n = 133) | No (n = 24) | Sig | Yes (n = 135) | No (n = 22) | Sig | ||
| Identity (17.8%) | ||||||||||
| Cough | ** | * | ||||||||
| Yes | 14.6 | 91.3 | 8.7 | 65.2 | 34.8 | 69.6 | 30.4 | |||
| No | 85.4 | 95.5 | 4.5 | 88.1 | 11.9 | 88.8 | 11.2 | |||
| Difficulty breathing | * | † | ||||||||
| Yes | 5.7 | 88.9 | 11.1 | 55.6 | 44.4 | 66.7 | 33.3 | |||
| No | 94.3 | 95.3 | 4.7 | 86.5 | 13.5 | 87.2 | 12.8 | |||
| Respiratory infection | ||||||||||
| Yes | 3.2 | 80.0 | 20.0 | 80.0 | 20.0 | 80.0 | 20.0 | |||
| No | 96.8 | 95.4 | 4.6 | 84.9 | 15.1 | 86.2 | 13.8 | |||
| Timeline (61.8%) | ||||||||||
| Age of onset | ||||||||||
| Yes | 61.1 | 96.9 | 3.1 | 84.4 | 15.6 | 86.5 | 13.5 | |||
| No | 38.9 | 91.8 | 8.2 | 85.2 | 14.8 | 85.2 | 14.8 | |||
| Duration | ||||||||||
| Yes | 3.8 | 83.3 | 16.7 | 66.7 | 33.3 | 66.7 | 33.3 | |||
| No | 96.2 | 95.4 | 4.6 | 85.4 | 14.6 | 86.8 | 13.2 | |||
| Consequences (58.6%) | ||||||||||
| Life threatening | ||||||||||
| Yes | 58.6 | 95.7 | 4.3 | 83.7 | 16.3 | 85.9 | 14.1 | |||
| No | 41.4 | 93.8 | 6.2 | 86.2 | 13.8 | 86.2 | 13.8 | |||
| Cause (35.0%) | ||||||||||
| Contagion | ||||||||||
| Yes | 24.8 | 92.3 | 7.7 | 82.1 | 17.9 | 84.6 | 15.4 | |||
| No | 75.2 | 95.8 | 4.2 | 85.6 | 14.4 | 86.4 | 13.6 | |||
| Pathogens | † | ** | * | |||||||
| Yes | 7.6 | 83.3 | 16.7 | 58.3 | 41.7 | 66.7 | 33.3 | |||
| No | 92.4 | 95.9 | 4.1 | 86.9 | 13.1 | 87.6 | 12.4 | |||
| Non-vaccination | ||||||||||
| Yes | 4.5 | 100.0 | 0 | 100.0 | 0 | 100.0 | 0 | |||
| No | 95.5 | 94.7 | 5.3 | 84.0 | 16.0 | 85.3 | 14.7 | |||
| Many bacterial strains | † | *** | * | |||||||
| Yes | 2.5 | 75.0 | 25.0 | 25.0 | 75.0 | 50.0 | 50.0 | |||
| No | 97.5 | 95.4 | 4.6 | 86.3 | 13.7 | 86.9 | 13.1 | |||
| Cure/Control (56.7%) | ||||||||||
| Vaccines necessary | * | † | * | |||||||
| Yes | 46.5 | 98.6 | 1.4 | 90.4 | 9.6 | 93.2 | 6.8 | |||
| No | 53.5 | 91.7 | 8.3 | 79.8 | 20.2 | 79.8 | 20.2 | |||
| Increase in incidence | ||||||||||
| Yes | 17.2 | 100.0 | 0 | 88.9 | 11.1 | 92.6 | 7.4 | |||
| No | 82.8 | 93.8 | 6.2 | 83.8 | 16.2 | 84.6 | 15.4 | |||
| Vaccines ineffective | ** | *** | *** | |||||||
| Yes | 4.5 | 71.4 | 28.6 | 14.3 | 85.7 | 28.6 | 71.4 | |||
| No | 95.5 | 96.0 | 4.0 | 88.0 | 12.0 | 88.7 | 11.3 | |||
p < .001,
p < .01,
p< .05,
p < .1
Quantitative Analysis
We conducted Factor Analysis with Oblique rotation (Pro-max) to examine the construct validity of vaccine worry and the vaccine hassles scales (Table 1). Both the vaccine hassles scale and vaccine worry scale consisted of single underlying factor and indicated high internal consistency (Table 1). The codes developed from qualitative analysis of responses were quantitized to assess the frequency of report, with participants often reporting more than one code. Any code with fewer than four participants reporting was not included in further analyses, nor was it included in tables (Nardo 2003).
The following factors were considered in Chi square analyses (categorical) and t-tests (continuous) for the vaccination outcomes: (a) self-system factors: mothers’ age, race, Appalachian identity, education, annual household income, employment status, marital status, health insurance, child caregiver (daycare or others), and the vaccine hassles scale; (b) codes from illness representations of pertussis: cough, difficulty breathing, and respiratory infection (identity); age of onset and duration of disease (timeline); life-threatening (consequences); contagion, pathogen, non-vaccination, low herd immunity, and many bacterial strains (cause); vaccines necessary, vaccines ineffective, and increase in incidence (cure/control), and (c) emotional representation: psychological distress and the vaccine worry scale. Variables from bivariate analyses (p < .1) were entered into the logistic regression models for the three vaccination outcomes and were analyzed using backward elimination. The criterion for retaining a variable was p < .1.
Results
Participants’ Demographic Characteristics and Child’s Vaccination Status
With respect to participants’ self-system factors, the majority of mothers were white (94.4%), married (86.9%), and employed full-time (61.9%). About 46.0% identified themselves as Appalachian, 47.5% had >master’s degree, 71.7% had >$50,000 annual household income, 91.9% had health insurance, and 42.5% used daycare for their kids (Table 2). Most (95%) participants’ child had received at least one vaccination. Fewer (85.0%) reported that their child was up-to-date with recommended vaccination schedule, and 86.3% participants intended to vaccinate their children in the future (Table 2).
Table 2.
Associations of Mothers’ Characteristics with Child Immunization
| Total % (N = 160) | Receipt of any vaccine, row % | Up-to-date status, row % | Future intention, row % | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||
| Yes (n = 152) | No (n = 8) | Sig | Yes (n = 136) | No (n = 24) | Sig | Yes (n = 138) | No (n = 22) | Sig | ||
| Self-System Factors | ||||||||||
| Age, mean years (SD, Range) | 31.2 (4.7, 21.0–51.0) | 31.4 (4.6) | 29.0 (5.5) | 31.3 (4.7) | 30.7 (4.9) | 31.3 (4.7) | 30.8 (4.5) | |||
| Race | ||||||||||
| White | 94.4 | 94.7 | 5.3 | 84.1 | 15.9 | 85.4 | 14.6 | |||
| Non-Whitea | 5.6 | 100 | 0 | 100.0 | 0 | 100.0 | 0 | |||
| Self-identified as Appalachian | ||||||||||
| Yes | 40.0 | 93.8 | 6.2 | 82.8 | 17.2 | 87.5 | 12.5 | |||
| No | 60.0 | 95.8 | 4.2 | 86.3 | 13.7 | 85.3 | 14.7 | |||
| Education | ||||||||||
| <Master’s degree | 52.5 | 95.2 | 4.8 | 82.1 | 17.9 | 83.3 | 16.7 | |||
| ≥Master’s degree | 47.5 | 94.7 | 5.3 | 88.2 | 11.8 | 89.5 | 10.5 | |||
| Employment status | * | *** | ** | |||||||
| Full-time | 61.9 | 98.0 | 2.0 | 93.9 | 6.1 | 92.9 | 7.1 | |||
| Not full-timeb | 38.1 | 90.2 | 9.8 | 70.5 | 29.5 | 75.4 | 24.6 | |||
| Annual household income | ||||||||||
| ≤$50,000 | 28.1 | 91.1 | 8.9 | 84.4 | 15.6 | 86.7 | 13.3 | |||
| >$50,000 | 71.9 | 96.5 | 3.5 | 85.1 | 14.9 | 86.0 | 14.0 | |||
| Marital status | ||||||||||
| Married | 86.9 | 95.7 | 4.3 | 85.6 | 14.4 | 87.1 | 12.9 | |||
| Unmarried | 13.1 | 90.5 | 9.5 | 81.0 | 19.0 | 81.0 | 19.0 | |||
| Health Insurance | † | |||||||||
| Yes | 91.9 | 95.9 | 4.1 | 85.7 | 14.3 | 87.1 | 12.9 | |||
| No | 8.1 | 84.6 | 15.4 | 76.9 | 23.1 | 76.9 | 23.1 | |||
| Child care | * | ** | * | |||||||
| Daycare | 42.5 | 100.0 | 0.0 | 94.1 | 5.9 | 92.6 | 7.4 | |||
| Not daycarec | 57.5 | 91.3 | 8.7 | 78.3 | 21.7 | 81.5 | 18.5 | |||
| Vaccine hassles scale, mean score (SD, Range) | 2.0 (0.7, 1.0–3.8) | 1.9 (0.7) | 2.9 (0.6) | *** | 1.8 (0.7) | 2.7 (0.7) | *** | 1.9 (0.7) | 2.6 (0.7) | *** |
| Vaccine worry scale, mean score (SD, Range) | 2.7 (1.1, 1.0–5.0) | 2.6 (1.0) | 4.3 (0.8) | *** | 2.5 (1.0) | 3.8 (0.9) | *** | 2.5 (1.0) | 3.7 (1.0) | *** |
| Distress scale, mean score (SD, Range) | 1.9 (0.8, 1.0–5.0) | 1.9 (0.8) | 2.2 (1.2) | 1.9 (0.8) | 2.1 (1.0) | 1.9 (0.8) | 2.0 (1.1) | |||
p < .001,
p. < .01,
p < .05,
p < .1
African American, Asian, American Indian or Alaska Native
Part-time, self-employed, unemployed, homemaker, or student
Self, family, or babysitter
Vaccine Worry and Vaccine Hassles
The most common vaccine worries among mothers were vaccines’ side effects (54.4%), vaccine could harm child (40.6%), and vaccines could be linked to autism or other learning disabilities (23.7%) (Table 1). The most common vaccine hassles faced by mothers were too many vaccines for children (23.7%), the way vaccines are made (14.3%), and high cost of vaccines (12.5%). Mothers had a moderate vaccine worry mean score of 2.7 and low vaccine hassles mean score of 2.0 (Table 2).
Cognitive Illness Representations of Pertussis
About 17.8% participants mentioned one or more domains of pertussis identity including the characteristic “deep ‘whooping’ sound is often heard” for cough (14.6%), difficulty breathing (5.7%), and respiratory infection (3.2%) (Table 3). The timeline of pertussis was mentioned by the largest number of participants (61.8%), including age of onset (61.1%, e.g., “very dangerous to babies especially under 6 months”) and duration of illness (3.8%, e.g., “the 100 day cough”). Consequences of pertussis were mentioned by 58.6% of participants in their illness representations as many mothers reported pertussis to be life-threatening (58.6%, e.g., “It’s scary and deadly for children.”). Causes of pertussis were noted by 35.0% of mothers including contagion (24.8%, e.g., “It spreads easily”) and pathogen (7.6%, e.g., “respiratory condition caused by Bordetella pertussis”). Further, some participants mentioned non-vaccination (4.5%, e.g., “I had it because I was not vaccinated as a child”), low herd immunity (1.9%, e.g., “[Pertussis] was nearly eradicated in the US prior to the anti-vax phenomenon”), and many bacterial strains (2.5%, e.g., “there are many different strains, and the vaccine does not protect against them all”) as causes.
Cure/control of pertussis was reported by 56.7% of mothers including vaccines necessary (46.5%, e.g., “really easy to prevent with a vaccination in pregnant mothers and child care workers”) and increase in incidence (17.2%). Further, some mothers perceived vaccines to be ineffective (4.5%, e.g., “most children that get this are vaccinated”). A corollary belief among some mothers was that complementary medicines (1.3%, e.g., “whole food/organic diet, increased vit[amin] C, rest, and essential oils will be adequate treatment for my healthy children if they had whooping cough”) and antibiotics (1%) are adequate treatments for pertussis. On further examination, children of participants who perceived complementary medicines and antibiotics to be adequate treatments did not receive any vaccine.
Child’s Receipt of Any Vaccine
Bivariate analyses indicated that full-time employment, using a daycare facility, and vaccines are necessary (control) were associated with child’s receipt of any vaccine while higher vaccine hassles, higher vaccine worry, and vaccines are ineffective (control) were associated with child not receiving any vaccine (Tables 2, 3). Multivariate logistic regression analysis indicated that higher vaccine worry was associated with child not receiving any vaccine (Table 4).
Table 4.
Adjusted Odds Ratios and 95% Confidence Intervals from Logistic Regression Models of Receipt of Any Vaccine, Up-to-date Status, and Future Intention
| AOR | 95% CI | Sig | |
|---|---|---|---|
| Receipt of any vaccine | |||
| Vaccine worry | 0.17 | [0.06, 0.46] | *** |
| Up-to-date status | |||
| Childcare: Daycare vs. not daycarea | 4.23 | [1.10, 16.2] | * |
| Vaccine worry | 0.38 | [0.18, 0.83] | * |
| Vaccine hassles | 0.38 | [0.13, 1.10] | † |
| Illness representations | |||
| Identity: Difficulty breathing | 0.09 | [0.01, 0.52] | ** |
| Future intention | |||
| Employment: Full-time vs. not full-timeb | 2.60 | [0.86, 7.86] | † |
| Vaccine worry | 0.32 | [0.18, 0.58] | *** |
| Illness representations | |||
| Identity: Cough | 0.27 | [0.07, 0.95] | * |
| Cure/Control: Vaccines ineffective | 0.11 | [0.01, 0.87] | * |
AOR adjusted odds ratio, CI confidence interval
p < .001,
p < .01,
p < .05,
p < .1
Self, family, or babysitter
Part-time, self-employed, unemployed, homemaker, or student
Child’s Up-to-date Vaccination Status
Bivariate analyses indicated that full-time employment and using a daycare facility were associated with child being up-to-date with recommended vaccination schedule. Higher vaccine worry, higher vaccine hassles, and illness representations of cough (identity), difficulty breathing (identity), pathogens (cause), many bacterial strains (cause), and vaccines are ineffective (control) were associated with child not being up-to-date with recommended vaccination schedule (Tables 2, 3). Multivariate logistic regression analysis indicated that using a daycare facility was associated with child being up-to-date while higher vaccine worry and difficulty breathing (identity) were associated with child not being up-to-date with recommended vaccination schedule (Table 4).
Mother’s Future Intention to Follow Vaccination Schedule
Bivariate analyses indicated that full-time employment, using a daycare facility, and vaccines are necessary (control) were associated with intention to vaccinate child in future. Higher vaccine worry, higher vaccine hassles, and illness representations of cough (identity), pathogens (cause), many bacterial strains (cause), and vaccines are ineffective (cause) were associated with no intention to vaccinate child in future (Tables 2, 3). Multivariate logistic regression analysis showed that higher vaccine worry, cough (identity), and vaccines are ineffective (control) were associated with no intention to vaccinate child in future (Table 4).
Discussion
This study offers insights into the illness representations of pertussis among mothers in WV and their associations with child’s receipt of any vaccine, child’s up-to-date vaccination status, and mothers’ future intention to follow the recommended vaccination schedule. Even though the participants reported high education and income for this region, more than one-tenth of participants’ children were not up-to-date and had no future intention to follow the recommended vaccination schedule. Also, eight children received no vaccine at all, most of whom were above 2 years of age. This finding is concerning as unvaccinated children reduce herd immunity and increase the risk of vaccine preventable diseases in community. These results highlight a lower motivation to immunize children among a significant number of mothers even in a strict vaccination exemption state.
The biggest hassle reported by mothers was that there are too many vaccines for their children, followed by the way vaccines are made, and the cost of vaccines. Although our study was conducted in the Appalachian state of WV, none of the participants reported lack of access to vaccination, which contrasts with the only previous study in this population (Gore et al. 1999). This result reinforces the salience of parental beliefs regarding the safety and effectiveness of vaccines, rather than access to vaccination in immunization behavior. We also found that using a daycare facility for child care was a significant factor for vaccinations of children. The strict vaccination exemption policies in WV are accompanied by equally strict vaccination requirements for daycare entry. However, some parents have been homeschooling their children in order to avoid vaccinating their children (Thorpe et al. 2012). Tightening vaccination exemption policies such as the recent ending of personal exemptions in California may not be effective among these parents who understand the limitations of these policies (McCarthy 2015).
Our newly-developed vaccine worry scale demonstrated solid psychometric properties and showed that a large proportion of mothers were concerned about vaccines’ side effects, such as mental disorders in their children. Mothers continue to face a dilemma about the adverse effects of vaccines (which may be chronic) versus the protection from disease that vaccines offer, such as pertussis, which is subacute and manageable in most cases. Further, vaccine worry was a strong risk factor for immunization of children. These results are consistent with (Gust et al. 2004), which found that vaccination safety concerns were associated with under-immunization children, and are extended by revealing that vaccine worry is associated with lower future intention, as well. Physicians and public health interventions need to build trusting relationship and provide mothers with knowledge regarding safety and necessity of childhood immunization. Previous research has found that tailored recommendations depending on mothers’ specific position on vaccination may be successful in improving vaccination rates (Leask et al. 2012).
The CSM-SR model helped in understanding mothers’ beliefs regarding pertussis and vaccines, which affect the vaccination of their children. Participants who were aware of the identity of pertussis (i.e., characteristic cough and breathing pattern) were less likely to have children who were up-to-date and to have future intention to follow the vaccination schedule. Similar results have been found in a previous study by Ganczak et al. which found that despite high level of Hepatitis B knowledge, the vaccine uptake was low among adults (Ganczak et al. 2015). Our study augments these results among mothers in an Appalachian, strict vaccine exemption community for the vaccination of their child. Mothers who are aware of the signs and symptoms of pertussis may be more educated and confident in identifying and treating the disease if their child contracts it. Hence, they are less motivated to prevent the disease by vaccinating their children. These findings are important in the context of framing messages, as increasing community awareness of disease symptoms by itself may not be effective in increasing the uptake of vaccines against diseases such as pertussis. For example, recent educational campaigns aim to promote pertussis vaccination by making people aware of the characteristic sound of its cough (Sounds of pertussis). Such educational efforts may be a double-edged sword, prompting some parents to rely on symptoms to seek medical care to treat the disease rather than using vaccination to prevent the disease.
Along with the identification of symptoms, the cure/control dimension of illness representations was an important factor associated with vaccination behavior. Two beliefs were important: that vaccines are ineffective and that complementary medicines and antibiotics are effective treatments for pertussis, the latter of which has been documented previously (Downey et al. 2010). Thus, the combination of beliefs that they can manage the disease, that vaccines are ineffective to prevent pertussis, and that treatments are effective may lead many mothers to ‘drag their feet’ about vaccination, unless imposed by an outside entity. These worries about and hassles to vaccines must be acknowledged in a compassionate way, while presenting well-documented evidence of the safety and effectiveness of vaccines. Continued efforts to accumulate a greater knowledge base of safety and effectiveness of vaccines and improved vaccines with higher efficacy may help to assuage these vaccine fears.
Our study results should be interpreted in light of some limitations. First, although our results are suggestive, they cannot be taken to imply causality. Due to recall bias, mothers may not have correctly recalled vaccinating their children and reported lower vaccination rates reported in our study. Also, most mothers in our study had high education with relatively high income, which limits the generalizability of findings to other communities. However, it is important to target such groups of parents with high socio-economic status as they have been found to be at higher risk of non-vaccination (Smith et al. 2011). This is the first study to assess the importance of mothers’ illness representations of a vaccine preventable disease in vaccination of their children, and we did attract our population of interest - women who were avoiding or delaying vaccination.
Conclusions
Some well-educated mothers with vaccine access in our study questioned the safety and effectiveness of vaccines and indicated high levels of vaccine worries, which were associated with lower child immunization. Consistent with the CSM-SR, awareness of the symptoms of pertussis and its treatment were associated with less than optimal childhood vaccinations. Mothers with higher symptom and treatment awareness may be more confident of managing the disease through identification and treatment, rather than preventing it through vaccination. Such anti-vaccination beliefs have been found to be resistant to change with conventional pro-vaccine messages or information on the risk of vaccine-preventable diseases (Hemerka 2014). Addressing the ‘common sense’ understandings of vaccines and vaccine preventable diseases among anti-vaccination parents is necessary to control the outbreaks of vaccine-preventable diseases.
Significance.
Current studies lack illness representations of vaccine preventable diseases.
This study analyzed mothers’ illness representations of pertussis, which is on the rise in the US.
We developed vaccine worry and vaccine hassles scales to measure mothers’ worries and barriers to vaccinate their children less than 3 years of age. The illness representation of pertussis identity and higher vaccine worry were associated with lower child vaccination. It is critical to address the lay understandings of pertussis to increase child vaccination.
Acknowledgments
Funding No external funding source was involved.
Footnotes
Compliance with Ethical Standards
Conflict of interest The authors declare that they have no conflict of interest.
Ethical Approval This study was conducted in accord with prevailing ethical principles and was reviewed by West Virginia University Institutional Review Board.
References
- Adorador A, McNulty R, Hart D, Fitzpatrick JJ. Perceived barriers to immunizations as identified by Latino mothers. Journal of the American Academy of Nurse Practitioners. 2011;23(9):501–508. doi: 10.1111/j.1745-7599.2011.00632.x. [DOI] [PubMed] [Google Scholar]
- Atwell JE, Van Otterloo J, Zipprich J, Winter K, Harriman K, Salmon DA, … Omer SB. Nonmedical vaccine exemptions and pertussis in California, 2010. Pediatrics. 2013;132(4):624–630. doi: 10.1542/peds.2013-0878. [DOI] [PubMed] [Google Scholar]
- Beel ER, Rench MA, Montesinos DP, Mayes B, Healy CM. Knowledge and attitudes of postpartum women toward immunization during pregnancy and the peripartum period. Human Vaccines & Immunotherapeutics. 2013;9(9):1926–1931. doi: 10.4161/hv.25096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benin AL, Wisler-Scher DJ, Colson E, Shapiro ED, Holmboe ES. Qualitative analysis of mothers’ decision-making about vaccines for infants: The importance of trust. Pediatrics. 2006;117(5):1532–1541. doi: 10.1542/peds.2005-1728. [DOI] [PubMed] [Google Scholar]
- Borkan J. Immersion/crystallization. Doing Qualitative Research. 1999;2:179–194. [Google Scholar]
- Bradford WD, Mandich A. Some state vaccination laws contribute to greater exemption rates and disease outbreaks in the United States. Health Affairs (Project Hope) 2015;34(8):1383–1390. doi: 10.1377/hlthaff.2014.1428. [DOI] [PubMed] [Google Scholar]
- Carrillo-Marquez M, White L. Current controversies in childhood vaccination. SD Med. 2013:46–51. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. [Accessed 7 May 2016];Provisional pertussis surveillance report, September 18, 2015. 2014 http://www.cdc.gov/pertussis/downloads/pertuss-surv-report-2014.pdf.
- Centers for Disease Control and Prevention Immunization Schedules. [Accessed 7 May 2016];2015 http://www.cdc.gov/vaccines/schedules/hcp/child-adolescent.html.
- Centers for Disease Control and Prevention (CDC) Ten great public health achievements–United States, 2001–2010. MMWR Morbidity and mortality weekly report. 2011;60(19):619. [PubMed] [Google Scholar]
- Cherry JD. Epidemic pertussis in 2012—the resurgence of a vaccine-preventable disease. New England Journal of Medicine. 2012;367(9):785–787. doi: 10.1056/NEJMp1209051. [DOI] [PubMed] [Google Scholar]
- Crabtree BF, Miller WL. Doing qualitative research. Sage Publications; 1999. [Google Scholar]
- Dempsey AF, Schaffer S, Singer D, Butchart A, Davis M, Freed GL. Alternative vaccination schedule preferences among parents of young children. Pediatrics. 2011;128(5):848–856. doi: 10.1542/peds.2011-0400. [DOI] [PubMed] [Google Scholar]
- Downey L, Tyree PT, Huebner CE, Lafferty WE. Pediatric vaccination and vaccine-preventable disease acquisition: Associations with care by complementary and alternative medicine providers. Maternal and Child Health Journal. 2010;14(6):922–930. doi: 10.1007/s10995-009-0519-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganczak M, Dmytrzyk-Daniłów G, Korzeń M, Drozd-Dąbrowska M, Szych Z. Prevalence of HBV infection and knowledge of hepatitis B among patients attending primary care clinics in Poland. Journal of Community Health. 2015:1–10. doi: 10.1007/s10900-015-0139-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glanz JM, McClure DL, Magid DJ, Daley MF, France EK, Salmon DA, Hambidge SJ. Parental refusal of pertussis vaccination is associated with an increased risk of pertussis infection in children. Pediatrics. 2009;123(6):1446–1451. doi: 10.1542/peds.2008-2150. [DOI] [PubMed] [Google Scholar]
- Gore P, Madhavan S, Curry D, McClung G, Castiglia M, Rosenbluth SA, Smego RA. Predictors of childhood immunization completion in a rural population. Social Science & Medicine (1982) 1999;48(8):1011–1027. doi: 10.1016/s0277-9536(98)00410-9. [DOI] [PubMed] [Google Scholar]
- Gust DA, Strine TW, Maurice E, Smith P, Yusuf H, Wilkinson M, … Schwartz B. Underimmunization among children: Effects of vaccine safety concerns on immunization status. Pediatrics. 2004;114(1):e16–e22. doi: 10.1542/peds.114.1.e16. [DOI] [PubMed] [Google Scholar]
- Hemerka J. Effective messages in vaccine promotion: A randomized trial. Journal of Emergency Medicine. 2014;1(47):126–127. [Google Scholar]
- Hill HA. Vaccination Coverage Among Children Aged 19–35 Months—United States, 2015. MMWR Morbidity and Mortality Weekly Report. 2016:65. doi: 10.15585/mmwr.mm6539a4. [DOI] [PubMed] [Google Scholar]
- Kennedy A, Basket M, Sheedy K. Vaccine attitudes, concerns, and information sources reported by parents of young children: Results from the 2009 HealthStyles survey. Pediatrics. 2011;127(1):S92–S99. doi: 10.1542/peds.2010-1722N. [DOI] [PubMed] [Google Scholar]
- Leask J, Kinnersley P, Jackson C, Cheater F, Bedford H, Rowles G. Communicating with parents about vaccination: A framework for health professionals. BMC pediatrics. 2012;12(1):154. doi: 10.1186/1471-2431-12-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebo MA, Nesselroade JR. Intraindividual differences dimensions of mood change during pregnancy identified in five P-technique factor analyses. Journal of Research in Personality. 1978;12(2):205–224. [Google Scholar]
- Leventhal H, Brissette I, Leventhal EA. The commonsense model of self-regulation of health and illness. The Self-Regulation of Health and Illness Behaviour. 2003;1:42–65. [Google Scholar]
- Luthy KE, Beckstrand RL, Peterson NE. Parental hesitation as a factor in delayed childhood immunization. Journal of Pediatric Health Care. 2009;23(6):388–393. doi: 10.1016/j.pedhc.2008.09.006. [DOI] [PubMed] [Google Scholar]
- Maglione MA, Das L, Raaen L, Smith A, Chari R, Newberry S, … Gidengil C. Safety of vaccines used for routine immunization of U.S. children: A systematic review. Pediatrics. 2014;134(2):325–337. doi: 10.1542/peds.2014-1079. [DOI] [PubMed] [Google Scholar]
- McHugh ML. Interrater reliability: the kappa statistic. Biochemia medica. 2012;22(3):276–282. [PMC free article] [PubMed] [Google Scholar]
- Nardo M. The quantification of qualitative survey data: A critical assessment. Journal of Economic Surveys. 2003;17:645–668. [Google Scholar]
- Niederhauser VP, Markowitz M. Barriers to immunizations: Multiethnic parents of under-and unimmunized children speak. Journal of the American Academy of Nurse Practitioners. 2007;19(1):15–23. doi: 10.1111/j.1745-7599.2006.00185.x. [DOI] [PubMed] [Google Scholar]
- Omer SB, Salmon DA, Orenstein WA, deHart MP, Halsey N. Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable diseases. New England Journal of Medicine. 2009;360(19):1981–1988. doi: 10.1056/NEJMsa0806477. [DOI] [PubMed] [Google Scholar]
- Salmon DA, Moulton LH, Omer SB, Patricia deHart M, Stokley S, Halsey NA. Factors associated with refusal of childhood vaccines among parents of school-aged children: A case-control study. Archives of Pediatrics & Adolescent Medicine. 2005;159(5):470–476. doi: 10.1001/archpedi.159.5.470. [DOI] [PubMed] [Google Scholar]
- Shiloh S. Illness representations, self-regulation, and genetic counseling: A theoretical review. Journal of Genetic Counseling. 2006;15(5):325–337. doi: 10.1007/s10897-006-9044-5. [DOI] [PubMed] [Google Scholar]
- Shui IM, Weintraub ES, Gust DA. Parents concerned about vaccine safety: Differences in Race/Ethnicity and attitudes. American Journal of Preventive Medicine. 2006;31(3):244–251. doi: 10.1016/j.amepre.2006.04.006. [DOI] [PubMed] [Google Scholar]
- Smith PJ, Humiston SG, Marcuse EK, Zhao Z, Dorell CG, Howes C, Hibbs B. Parental delay or refusal of vaccine doses, childhood vaccination coverage at 24 months of age, and the health belief model. Public Health Reports (Washington, DC: 1974) 2011;126(2):135–146. doi: 10.1177/00333549111260S215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorpe EL, Zimmerman RK, Steinhart JD, Lewis KN, Michaels MG. Homeschooling parents’ practices and beliefs about childhood immunizations. Vaccine. 2012;30(6):1149–1153. doi: 10.1016/j.vaccine.2011.12.019. [DOI] [PubMed] [Google Scholar]
- Topuzoglu A, Ay P, Hidiroglu S, Gurbuz Y. The barriers against childhood immunizations: A qualitative research among socio-economically disadvantaged mothers. European Journal of Public Health. 2007;17(4):348–352. doi: 10.1093/eurpub/ckl250. [DOI] [PubMed] [Google Scholar]
- Vannice KS, Salmon DA, Shui I, Omer SB, Kissner J, Edwards KM, … Gust DA. Attitudes and beliefs of parents concerned about vaccines: Impact of timing of immunization information. Pediatrics. 2011;127(1):S120–6. doi: 10.1542/peds.2010-1722R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinman JA, Petrie KJ. Perceptions of health and illness. Perceptions of health and illness. 1997:1–17. [Google Scholar]
- West Virginia Department of Health and Human Resources. Office of Epidemiology and Prevention Services. [Accessed 7 May 2016];West Virginia immunization law & entry requirements. 2015 http://www.dhhr.wv.gov/oeps/immunization/requirements/Pages/default.aspx.
- Wu AC, Wisler-Sher DJ, Griswold K, Colson E, Shapiro ED, Holmboe ES, Benin AL. Postpartum mothers’ attitudes, knowledge, and trust regarding vaccination. Maternal and Child Health Journal. 2008;12(6):766–773. doi: 10.1007/s10995-007-0302-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaqub O, Castle-Clarke S, Sevdalis N, Chataway J. Attitudes to vaccination: A critical review. Social Science & Medicine. 2014;112:1–11. doi: 10.1016/j.socscimed.2014.04.018. [DOI] [PubMed] [Google Scholar]
- Sounds of pertussis. [Accessed 7 May 2016];Pertussis (whooping cough) is a sound you won’t forget. https://www.soundsofpertussis.com/
- [Accessed 7 May 2016];West Virginians for vaccination exemption. http://www.wvve.org/
- McCarthy M. California ends vaccine exemptions on grounds of belief–will other states follow? BMJ (Clinical Research Ed) 2015 doi: 10.1136/bmj.h363516. [DOI] [PubMed] [Google Scholar]


