Abstract
A limited number of studies have reported an association between erectile dysfunction (ED) and chronic periodontitis (CP). The aim of the present study is to assess the association between CP and ED through a systematic review of published literature. To address the focused question, “Is there a relationship between ED and CP?” indexed databases were searched till December 2015 using various key words “erectile dysfunction,” “periodontal disease,” “periodontitis,” “dental infection,” and “impotence.” Letters to the editor, commentaries, historic reviews, and experimental studies were excluded. The pattern of the present systematic review was customized to primarily summarize the pertinent data. Nine studies were included. Seven studies had a cross-sectional design and two studies were randomized control trials. The number of study participants ranged between 53 and 513,258 individuals with age ranging between 20 years and 85 years (median age ranging between 34.9 ± 4.9 years and 50.9 ± 16.6 years). In all studies, a positive relationship between CP and ED was reported. In four studies, odds ratio were reported, ranging between 1.53 and 3.35. From the literature reviewed, there seems to be a positive association between ED and CP; however, further well-designed controlled clinical trials are needed in this regard. It is emphasized that physicians should refer patients with ED to oral health care providers for a comprehensive oral evaluation and treatment.
Keywords: chronic periodontal disease, erectile dysfunction
Introduction
The National Institutes of Health Consensus Conference, has defined erectile dysfunction (ED) as a “consistent inability to attain or maintain a penile erection, or both, sufficient for adequate sexual relations” (“NIH Consensus Conference: Impotence: NIH Consensus Development Panel on Impotence,” 1993). It has been estimated that there are more than 18 million individuals in the United States affected by ED (Selvin, Burnett, & Platz, 2007). Ponholzer et al. (2005) reported that the prevalence of ED among Austrian men aged between 20 and 80 years old was 32.2%. It has also been projected that there will be approximately 300 million men worldwide with ED by the year 2025 (Ayta, McKinlay, & Krane, 1999). This increase has been associated with the aging of the world’s population and is expected to occur in the developing world (D. M. Lee et al., 2013).
A variety of risk factors have been associated with the etiology of ED. These include increasing age, poorly controlled diabetes mellitus (DM), hyperlipidemia, lower urinary tract symptoms, hypertension, psychological stress, and low physical activity (Ponholzer et al., 2005). A limited number of studies (Eltas, Oguz, Uslu, & Akdemir, 2013; Keller, Chung, & Lin, 2012; J. H. Lee et al., 2015; Matsumoto et al., 2014; Oguz et al., 2013; Sharma, Pradeep, & Raju, 2011; Tsao et al., 2015; Uppal, Bhandari, & Singh, 2014; Zadik, Bechor, Galor, Justo, & Heruti, 2009) have identified an association between ED and chronic periodontitis (CP), a disease of the supporting structures of teeth, namely cementum, gingiva, periodontal ligament, and alveolar bone. In the study by Matsumoto et al. (2014), an information sheet was distributed to 300 adult men with ED that received a comprehensive dental examination. These results reported a statistically significant association between scores of CP and presence of ED. In the study by Keller et al. (2012), the prevalence of CP in patients with ED was reported to be 26.9% in their study population aged less than 30 years. Similar results were reported by Eltas et al. (2013) and J. H. Lee et al. (2015).
It has been proposed that CP contributes to the etiology of ED by increasing the production of reactive oxygen species in the tissues which reduces the bioavailability of nitric oxide, which enhances endothelial dysfunction and impairs the mechanisms associated with muscular contractions (Blick, Ritchie, & Sullivan, 2016; Higashi et al., 2008). Zuo et al. (2011) in an experimental model concluded that mild systemic inflammation associated with induced periodontitis resulted in reduced expression of endothelial NO synthase (eNOS) and NOS activity in penile cavernous tissue of rats. These results suggest that CP is an important risk factor of ED. Proinflamatory cytokines (such as interleukin [IL]-1β, IL6, and tumor necrosis factor-alpha), thrombotic markers (fibrinogen), adhesion molecules (vascular cell adhesion molecule-1), and periodontal pathogens have also been associated with impaired endothelial function and muscular activity (Eaton et al., 2007; Saffi et al., 2015).
It is hypothesized that a direct and statistically significant relation exists between CP and ED. To our knowledge from indexed literature, the association between ED and CP has not been systematically reviewed. Therefore, the aim of the present study was to assess the association between CP and ED through a systematic review of indexed literature.
Method
Focused Question
The focused question was “Is there a relationship between ED and CP?”
Literature Search Protocol and Eligibility Criteria
A literature search was conducted using PubMed (National Library of Medicine, Washington, DC), Google Scholar, EMBASE, MEDLINE (OVID), and Web of Knowledge databases till December 2015 using different combinations of the following key words: (a) “erectile dysfunction + periodontitis,” (b) “erectile dysfunction + periodontal disease,” (c) “erectile dysfunction + gum disease,” (d) “erectile dysfunction + dental infection,” (e) “erectile dysfunction + gingivitis,” (f) “impotence + periodontal disease,” (g) “impotence + periodontitis.”
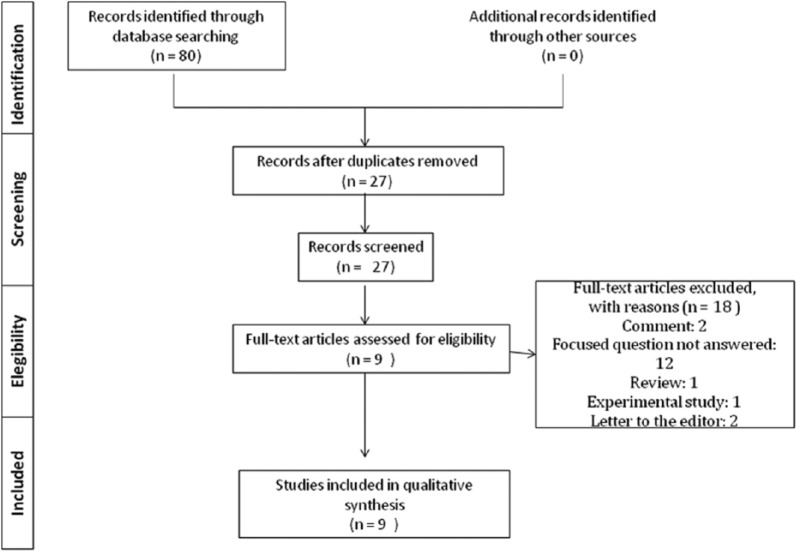
The following eligibility criteria were as follows: (a) clinical studies, (b) prospective and retrospective studies, and (c) studies assessing the relationship between CP and ED. Letters to the editor, commentaries, historic reviews, and experimental studies were excluded. Titles and abstracts of studies identified using the above-described protocol were screened by two authors (SVK and FJ) and checked for agreement. Full texts of studies judged by title and abstract to be relevant were read and independently evaluated for the stated eligibility criteria. Reference lists of potentially relevant original and review articles were hand searched to identify any studies that could have remained unidentified in the previous step. Once again, the articles were checked for disagreement via discussion among the authors (Figure 1).
Figure 1.
Article selection flow chart for the systematic review according to PRISMA guidelines.
Quality Assessment
Quality Assessment of included studies was performed using the Critical Appraisal Skills Program Cohort Study Checklist (Zeng et al., 2015). A systematic approach based on 12 specific criteria was used, which were as follows: (a) Study issue is clearly focused, (b) Cohort is recruited in an acceptable way, (c) Exposure is accurately measured, (d) Outcome is accurately measured, (e) Confounding factors are addressed, (f) Follow-up is long and complete, (g) Results are clear, (h) Results are precise, (i) Results are credible, (j) Results can be applied to the local population, (k) Results fit with available evidence, and (l) There are important clinical implications. Each criterion was given a response of either “Yes,” “No,” or “Cannot tell.” Each study could have a maximum score of 12. Critical Appraisal Skills Program scores were used to grade the methodological quality of each study assessed in the present systematic review.
Results
Study Selection and Characteristics
Through the initial search, 80 articles were identified. Fifty three publications of them were duplicates or did not answer the focused question. In the second step of evaluation, 18 more articles were excluded, which were reviews, commentaries, letters to the editor, experimental models, and/or did not answer the focused question (see the appendix). In total nine studies (Eltas et al., 2013; Keller et al., 2012; J. H. Lee et al., 2015; Matsumoto et al., 2014; Oguz et al., 2013; Sharma et al., 2011; Tsao et al., 2015; Uppal et al., 2014; Zadik et al., 2009) were included in the present systematic review and processed for data extraction.
All studies (Eltas et al., 2013; Keller et al., 2012; J. H. Lee et al., 2015; Matsumoto et al., 2014; Oguz et al., 2013; Sharma et al., 2011; Tsao et al., 2015; Uppal et al., 2014; Zadik et al., 2009) were performed on humans and under health care or university settings. These primary studies (Eltas et al., 2013; Keller et al., 2012; J. H. Lee et al., 2015; Matsumoto et al., 2014; Oguz et al., 2013; Sharma et al., 2011; Tsao et al., 2015; Uppal et al., 2014; Zadik et al., 2009) were conducted in the following countries: India, Israel, Japan, Korea, Taiwan, and Turkey. Seven studies (Keller et al., 2012; J. H. Lee et al., 2015; Matsumoto et al., 2014; Sharma et al., 2011; Tsao et al., 2015; Uppal et al., 2014; Zadik et al., 2009) had a cross-sectional design. Two studies (Eltas et al., 2013; Oguz et al., 2013) were randomized control trials (RCTs). The number of study participants ranged between 53 and 513,258 individuals with age ranging between 20 years and 85 years, and a median age ranging between 34.9 ± 4.9 years and 50.9 ± 16.6 years.
Chronic Periodontitis and Erectile Dysfunction Diagnosis
In eight studies (Eltas et al., 2013; Keller et al., 2012; J. H. Lee et al., 2015; Matsumoto et al., 2014; Oguz et al., 2013; Sharma et al., 2011; Tsao et al., 2015; Uppal et al., 2014), the assessment of CP was made by oral examination. Probing depth (PD) and clinical attachment loss (CAL) were reported in four studies (Eltas et al., 2013; Oguz et al., 2013; Sharma et al., 2011; Uppal et al., 2014) and three studies (Eltas et al., 2013; Oguz et al., 2013; Sharma et al., 2011), respectively; Eltas et al. (2013) and Oguz et al. (2013) assessed plaque index (PI), and bleeding on probing (BOP). Five studies (Keller et al., 2012; Sharma et al., 2011; Tsao et al., 2015; Uppal et al., 2014; Zadik et al., 2009) used radiographs to assess alveolar bone loss (ABL) and to diagnose CP.
The ED diagnosis was assessed in seven studies (Eltas et al., 2013; Keller et al., 2012; J. H. Lee et al., 2015; Matsumoto et al., 2014; Oguz et al., 2013; Sharma et al., 2011; Zadik et al., 2009) using the five-item version of the International Index of Erectile Function (IIEF-5) or Sexual Health Inventory for Men. Tsao et al. (2015) used data collected from the Longitudinal Health Insurance Database (LHID2000) of the Taiwan National Health Insurance program, where the International Classification of Diseases, ninth edition, Clinical modification (ICD-9-CM code 607.84) is used to establish ED diagnosis. Sharma et al. (2011) used colored penile Doppler ultrasound to assess vascularity of the penis and confirm the diagnosis of vasculogenic ED. Uppal et al. (2014) did not report the method used to diagnose ED. Severity of ED was assessed in four studies (Eltas et al., 2013; Sharma et al., 2011; Uppal et al., 2014; Zadik et al., 2009); based on the IIEF-5 scores: severe (5-7), moderate (8-11), mild to moderate (12-16), mild (17-21), and no ED (22-25; Diehm, Borm, Keo, & Wyler, 2015).
Confounding Factors
In seven studies (Eltas et al., 2013; Keller et al., 2012; J. H. Lee et al., 2015; Oguz et al., 2013; Sharma et al., 2011; Tsao et al., 2015; Uppal et al., 2014), data were adjusted for confounding factors including systemic diseases like poorly controlled DM, high blood pressure, and cardiovascular diseases. Alcohol and tobacco consumption were adjusted in three studies (Keller et al., 2012; Sharma et al., 2011; Uppal et al., 2014) and four studies (Eltas et al., 2013; Oguz et al., 2013; Sharma et al., 2011; Uppal et al., 2014), respectively. Previous periodontal therapy within the preceding 6 months and recent systemic antibiotic exposure were assessed in four studies (Eltas et al., 2013; Oguz et al., 2013; Sharma et al., 2011; Uppal et al., 2014) and two studies (Eltas et al., 2013; Oguz et al., 2013), respectively. Sharma et al. (2011) excluded those patients undergoing pharmacological treatment for ED. In the studies by Matsumoto et al. (2014) and Zadik et al. (2009) confounding variables were not assessed (Table 1).
Table 1.
General Characteristics of the Studies Included in the Present Review.
| Authors (region of study) | Study design | Population | Age in years (range) | Study methodology | Data adjusted for | Confounding variables assessed |
|---|---|---|---|---|---|---|
| Eltas et al. (2013; Turkey) | Randomized control trial | 120: ED + NSPT = 60, ED = 60 | ED + NSPT: 38.1 ± 6.1; ED: 36.6 ± 6.9 (30 to 40) | ED: IIEF-5 Questionnaire/self-reported; CP: Oral examination AAP criteria (PI, BOP, PD, CAL) | Age; BMI; Education; ED severity income level; Marital status; Smoking | CVD; DM; HBP; Periodontal therapy; Smoking; Systemic antibiotics |
| Keller et al. (2012; Taiwan) | Cross-sectional | 197,136: Cases = 32,856, Control = 164,280 | 49.3 ± 12.5; Cases: 49.4; Controls: 49.2 | ED: IIEF-5 Questionnaire/self-reported; CP: Oral examination and radiographs; ICD-9 criteria | Age; Income level; Residence area | Alcohol abuse; CHD; DM; HBP; Hyperlipidemia; Obesity |
| J. H. Lee et al. (2015; Korea) | Cross-sectional | 513,258: Cases = 2,732, Control = 510,526 | NA | ED: IIEF-5/KCD-6 criteria; CP: Oral examination AAP and ICD-10 criteria | Age; Income level; Insurance status; Residence area | Angina pectoris; Cerebral infarction; DM; HBP; Myocardial infarction; Obesity; Osteoporosis; Rheumatoid arthritis |
| Matsumoto et al. (2014; Japan) | Cross-sectional | 88: Cases = 88, Control = NA | 50.9 ± 16.6 (20 to 85) | ED: IIEF-5 Questionnaire/self-reported; CP: Oral examination/CP self-check sheet | Age | None |
| Oguz et al. (2013; Turkey) | Randomized control trial | 162: Cases = 80, Control = 82 | Cases: 34.9 ± 4.9; Control: 35.7 ± 4.8 (30 to 40) | ED: IIEF-5 Questionnaire/self-reported; CP: Oral examination (BOP, PI, CAL, PD) | Age; BMI; CP severity; Education; Income level; Marital status | CVD; DM; HBP; Periodontal therapy smoking; Systemic antibiotics |
| Sharma et al. (2011; India) | Cross-sectional | 70: Cases = 70, Control = 0 | 35.3 ± 3.64 (25 to 40) | ED: SHIM Questionnaire/penile Doppler ultrasound; CP: Oral examination (PD, CAL) and radiographs | ED severity | Aggressive periodontitis; Alcohol; ED medication periodontal therapy; Systemic diseases; Tobacco |
| Tsao et al. (2015; Taiwan) | Cross-sectional | 15,315: Cases = 5,105, Control = 10,210 | 48.3 ± 12.5 | ED: ICD-9 criteria; CP: Oral examination and radiographs; ICD-9 criteria | Age; Comorbid factors | CVD; DM; HBP; Hyperlipidemia; IHD; Obesity |
| Uppal et al. (2014; India) | Cross-sectional | 53: Control = NA, Mild ED = 23, Moderate ED = 17, Severe ED = 13 | NA (25 to 40) | ED: NA; CP: Oral examination (PD) and bitewings radiographs | ED severity | Aggressive periodontitis; Alcohol; Periodontal therapy; Systemic diseases; Tobacco |
| Zadik et al. (2009; Israel) | Cross-sectional | 305: Control = 235, Mild ED = 51, Moderate ED = 18; Severe ED = 1 | 39.5 ± 6.7 | ED: SHIM questionnaire/self-reported; CP: Bitewings radiographs | Education; ED severity; Smoking | None |
Note. ED = erectile dysfunction; CP = chronic periodontitis; HBP = high blood pressure; DM = diabetes mellitus; CHD = coronary heart disease; IIEF-5 = International Index of Erectile Dysfunction; AAP = American Academy of Periodontology; ICD = International Statistical Classification of Diseases and Related Health Problems; CVD = cerebrovascular diseases; IHD = ischemic heart disease; KCD = Korean classification of disease; PI = plaque index; BOP = bleeding on probing; CAL = clinical attachment loss; PD = probing depth; NSPT = nonsurgical periodontal therapy; SHIM = sexual health inventory for men; BMI = body mass index.
Main Outcomes
In all studies (Eltas et al., 2013; Keller et al., 2012; J. H. Lee et al., 2015; Matsumoto et al., 2014; Oguz et al., 2013; Sharma et al., 2011; Tsao et al., 2015; Uppal et al., 2014; Zadik et al., 2009), a positive relationship between CP and ED was reported. In four studies (Keller et al., 2012; J. H. Lee et al., 2015; Oguz et al., 2013; Tsao et al., 2015) odds ratio (OR) were reported, ranging between 1.53 and 3.35 (Table 2). According to J. H. Lee et al. (2015), ED presents the higher prevalence (55.6%) among the life-related comorbidities associated to CP, such as DM (46.1%), obesity (41.3%), myocardial infarction (44.8%), and hypertension (43.9%).
Table 2.
Odds Ratios and Primary Outcomes of the Studies Included.
| Authors (region of study) | Odds ratios | 95% Confidence intervals | Relationship between periodontal disease and erectile dysfunction |
|---|---|---|---|
| Eltas et al. (2013; Turkey) | NA | NA | Positive |
| Keller et al. (2012; Taiwan) | 3.35 | [3.25, 3.45] | Positive |
| J. H. Lee et al. (2015; Korea) | Univariate analysis: 2.75; multivariate analysis: 1.53 | Univariate analysis: [2.55, 2.97]; multivariate analysis: [1.41, 1.65] | Positive |
| Matsumoto et al. (2014; Japan) | NA | NA | Positive |
| Oguz et al. (2013; Turkey) | 3.29 | [1.36, 9.55] | Positive |
| Sharma et al. (2011; India) | NA | NA | Positive |
| Tsao et al. (2015; Taiwan) | 1.79 | [1.64, 1.96] | Positive |
| Uppal et al. (2014; India) | NA | NA | Positive |
| Zadik et al. (2009; Israel) | NA | NA | Positive |
Matsumoto et al. (2014) reported a statistically significant relation between CP score and ED. Keller et al. (2012) reported a higher prevalence of CP in patients with ED (26.9%) compared with healthy controls (9.4%), identifying a stronger association among the population aged less than 30 years (OR = 4.54, 95% confidence interval [CI; 3.81, 5.40]) and the group aged over than 69 years (OR = 4.84, 95% CI [4.35, 5.39]). Similar findings were reported by Tsao et al. (2015), where the association between ED and CP was stronger in the populations aged less than 30 years (OR = 2.13, 95% CI [1.23, 3.70]) and more than 59 years (OR = 2.27, 95% CI [1.99, 2.59]).
In one study (Matsumoto et al., 2014), no statistically significant difference between CP score and ED severity was reported. Sharma et al. (2011) reported that PD and CAL increased with severity of ED and the prevalence of CP is higher in severe vasculogenic ED (81.8%) compared with mild (38.8%) and moderate (76.4%) vasculogenic ED. Oguz et al. (2013) reported no significant difference in PD and CAL among patients with and without ED; however, the values for PI, BOP, and the percentage of sites with PD >4 mm and CAL >4 mm were significantly higher in ED group compared with control. Furthermore, Uppal et al. (2014) reported that the PD and ABL increased with severity of ED (mean PD = Mild ED: 3.3 ± 0.91 mm, Severe ED: 5.0 ± 1.31 mm; mean radiographic bone loss = Mild ED: 1.04 ± 1.50 mm, Severe ED: 3.31 ± 2.42 mm). In the study by Zadik et al. (2009), radiographic ABL of ≥6 mm was significantly more prevalent among patients with ED compared with healthy control.
Eltas et al. (2013) reported that nonsurgical periodontal treatment (NSPT) can improve ED severity; and according to Keller et al. (2012) gingivectomy and/or periodontal flap operation presented a lower OR (1.95, 95% CI [1.19, 1.39]) compared with untreated patients (OR = 4.33) among patients with ED and CP. Tsao et al. (2015) reported that dental extractions in patients with CP attenuated ED development (OR = 1.51, 95% CI [1.34, 1.70]).
Quality Assessment of Included Studies
Through the quality assessment was identified that all studies (Eltas et al., 2013; Keller et al., 2012; J. H. Lee et al., 2015; Matsumoto et al., 2014; Oguz et al., 2013; Sharma et al., 2011; Tsao et al., 2015; Uppal et al., 2014; Zadik et al., 2009) were conducted on humans and the total quality score ranged from 7 to 12. The most common shortcoming among all studies (Eltas et al., 2013; Keller et al., 2012; J. H. Lee et al., 2015; Matsumoto et al., 2014; Oguz et al., 2013; Sharma et al., 2011; Tsao et al., 2015; Uppal et al., 2014; Zadik et al., 2009) was the short-term, incomplete follow-up of the groups, and omission of confounding variables like smoking. Thus, on average, the quality of included studies on the relationship between ED and CP was good, limitations of short-term follow-up, and omission of confounding, limit the application of these study outcomes. Quality assessment of the individual articles is summarized in Table 3.
Table 3.
Critical Appraisal Skills Program Quality Assessment of the Reviewed Articles.
| Authors | Item 1 | Item 2 | Item 3 | Item 4 | Item 5 | Item 6 | Item 7 | Item 8 | Item 9 | Item 10 | Item 11 | Item 12 | Total quality score (0 to 12) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Eltas et al. (2013) | Yes | Yes | No | Yes | Yes | No | Yes | Yes | No | No | Yes | Yes | 8 |
| Keller et al. (2012) | Yes | Yes | No | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | 10 |
| J. H. Lee et al. (2015) | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 9 |
| Matsumoto et al. (2014) | Yes | Yes | No | No | No | No | Yes | Yes | No | Yes | Yes | Yes | 7 |
| Oguz et al. (2013) | Yes | Yes | No | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | 10 |
| Sharma et al. (2011) | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 12 |
| Tsao et al. (2015) | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 11 |
| Uppal et al. (2014) | Yes | No | No | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | 9 |
| Zadik et al. (2009) | Yes | Yes | No | No | No | No | Yes | Yes | No | Yes | Yes | Yes | 7 |
Discussion
From the literature reviewed, nine studies (Eltas et al., 2013; Keller et al., 2012; J. H. Lee et al., 2015; Matsumoto et al., 2014; Oguz et al., 2013; Sharma et al., 2011; Tsao et al., 2015; Uppal et al., 2014; Zadik et al., 2009) fulfilled the eligibility criteria and were systematically reviewed. Interestingly, results from all the studies (Eltas et al., 2013; Keller et al., 2012; J. H. Lee et al., 2015; Matsumoto et al., 2014; Oguz et al., 2013; Sharma et al., 2011; Tsao et al., 2015; Uppal et al., 2014; Zadik et al., 2009) reported a statistically significant association between CP and ED. It is therefore tempting to speculate that individuals with CP are at increased risk on developing ED as compared with individuals without CP. However, it is pertinent to mention that a variety of factors may have biased these results.
Is well known that tobacco smoking, alcohol consumption, poorly controlled DM, coronary heart disease (CHD) are significant risk factors of CP as well as ED (Al Amri et al., 2016; Chrysanthakopoulos, 2015; Javed, Bashir Ahmed, & Romanos, 2014; Kalka et al., 2015; Skeldon, Detsky, Goldenberg, & Law, 2015). It is important to mention that results from approximately 60% of the studies (Keller et al., 2012; J. H. Lee et al., 2015; Matsumoto et al., 2014; Tsao et al., 2015; Zadik et al., 2009) remained unadjusted for smoking and/or alcohol consumption, and in nearly 20% of the studies (Matsumoto et al., 2014; Zadik et al., 2009), the results were not adjusted for CHD and DM. It is therefore hypothesized that besides CP other risk factors, such as chronic hyperglycemia, raised systemic levels of proinflammatory cytokines, and cardiovascular disorders, may have significantly contributed in aggravating ED. The authors of the present study presume that habitual tobacco smokers and alcohol users with systemic diseases such as poorly controlled DM and CHD are more susceptible to ED as compared with smokers and alcohol users without systemic disorders. By no means do the authors consider smoking and/or alcohol use as less hazardous to oral health; however, the overall oxidative stress in the systemic tissues is expected to be higher in smokers and alcohol users who are immunocompromised compared with those that are not.
Vasculogenic ED diagnosis should include a comprehensive medical, sexual, and psychological examination, including underlying cardiovascular risk factors assessment and current medication, and other diagnostic tests to assess erectile function should include nocturnal penile rigidity and Doppler ultrasound (Diehm et al., 2015). However, only Sharma et al. (2011) confirm the diagnosis of vasculogenic ED using colored penile Doppler ultrasound to assess penis vascularity. In all the studies (Eltas et al., 2013; Keller et al., 2012; J. H. Lee et al., 2015; Matsumoto et al., 2014; Oguz et al., 2013; Sharma et al., 2011; Tsao et al., 2015; Uppal et al., 2014; Zadik et al., 2009) included in the present systematic review, presence or absence of ED was self-reported by the participants. Moreover, diagnosis of ED was based on a standardized questionnaire (IIEF-5 or Sexual Health Inventory for Men). According to Elnashar et al. (2012) and Chen et al. (2007), the IIEF-5 score may be unsuitable tool for the assessment of ED in susceptible populations, and cannot be used as a tool for differential diagnosis of vasculogenic ED, or to compare its specific vascular causes, nor can the scores of IIEF-5 reflect penile vascular conditions. Since the inclusion of study subjects was based in self-reported questionnaire in all the studies (Eltas et al., 2013; Keller et al., 2012; J. H. Lee et al., 2015; Matsumoto et al., 2014; Oguz et al., 2013; Sharma et al., 2011; Tsao et al., 2015; Uppal et al., 2014; Zadik et al., 2009), it is possible that they might have been patients with ED in the control group and vice versa. In this regard, the conclusions of the studies included in the present systematic review should be interpreted with caution.
Several studies (Al Amri et al., 2016; Javed, Al-Rasheed, Almas, Romanos, & Al-Hezaimi, 2012; Javed & Romanos, 2009) have reported that the severity of CP is associated with multiple factors such as daily frequency of smoking and duration of the habit, and glycemic levels in patients with DM. It is therefore possible that the severity of CP may also be associated with the exacerbation of ED. On a vigilant evaluation of all the studies (Eltas et al., 2013; Keller et al., 2012; J. H. Lee et al., 2015; Matsumoto et al., 2014; Oguz et al., 2013; Sharma et al., 2011; Tsao et al., 2015; Uppal et al., 2014; Zadik et al., 2009) included in the present systematic review, it was observed that less than 45% of the studies (Eltas et al., 2013; Sharma et al., 2011; Uppal et al., 2014; Zadik et al., 2009) evaluated the severity of ED associated to CP progression. Further well-designed RCT focusing between the association of EP and CP focusing on the severity of both diseases are needed. Furthermore, it is pertinent to mention that all the studies (Eltas et al., 2013; Keller et al., 2012; J. H. Lee et al., 2015; Matsumoto et al., 2014; Oguz et al., 2013; Sharma et al., 2011; Tsao et al., 2015; Uppal et al., 2014; Zadik et al., 2009) included were conducted in only six Asiatic countries, for a relatively short period of time and relatively small samples. It is hard to extrapolate these findings to the whole population. Hence, additional prospective studies including larger samples, for a longer period of time and including different ethnicities, habits, beliefs, and cultures are needed.
NSPT has been reported to reduce the local as well systemic burden of inflammation. Studies (Al Amri et al., 2016; Ghiraldini et al., 2015; Oates, Dowell, Robinson, & McMahan, 2009) have reported that NSPT is effective in reducing glycemic levels in patients with DM. In addition, in a recent study (Javed et al., 2016), it was reported that NSPT when used with adjunct laser therapy is more effective in reducing serum proinflamatory cytokines levels in patients with systemic disorders compared with NSPT alone. It is therefore hypothesized that NSPT may also contribute in the overall treatment strategy of patients with ED by improving long-term endothelial function and decreasing levels of inflammatory mediators. To our knowledge, there is only one study (Eltas et al., 2013) that has tested this hypothesis. Eltas et al. (2013) reported improvement in the IIEF-5 scores and clinical periodontal parameters in patients with ED and CP evaluated after 3 months of NSPT. However, further studies are needed in this regard.
Within the limits of the evidence available, the relationship between these conditions remains debatable, and further longitudinal studies and RCT assessing confounders (such as, smoking and DM) and implementing accurate diagnostic tools for ED assessment are needed to establish real causation.
Conclusion
From the literature reviewed, there seems to be a positive association between ED and CP; however, further well-designed controlled clinical trials are needed in this regard. It is emphasized that physicians should refer patients with ED to oral health care providers for a comprehensive oral evaluation and treatment.
Appendix
List of Excluded Articles
- Balhara Y., Sagar R., Varghese S. T. (2007). Bleeding gums: Duloxetine may be the cause. Journal of Postgraduate Medicine, 53, 44-45. (Focused question was not answered) [DOI] [PubMed] [Google Scholar]
- Bodakçi M. N., Hatipoglu N. K., Özbey I. (2013). Chronic periodontitis and erectile dysfunction. Journal of Sexual Medicine, 10, 3154. (Letter to the editor) [DOI] [PubMed] [Google Scholar]
- Carmignani L., Gadda F., Gazzano G., Nerva F., Mancini M., Ferruti M., . . . Colpi G. M. (2003). High incidence of benign testicular neoplasms diagnosed by ultrasound. Journal of Urology, 170, 1783-1786. (Focused question was not answered) [DOI] [PubMed] [Google Scholar]
- Caskey M. F., Morgan D. J., Porto A. F., Giozza S. P., Muniz A. L., Orge G. O., . . . Glesby M. J. (2007). Clinical manifestations associated with HTLV type I infection: A cross-sectional study. AIDS Research and Human Retroviruses, 23, 365-371. (Focused question was not answered) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eastham J., Seymour R. (2015). Is oral health a risk factor for sexual health? Dental Update, 42, 160-165. (Review) [DOI] [PubMed] [Google Scholar]
- Fernández M. A., Romá E. (2003). International Normalized Ratio (INR) increase in patients taking oral anticoagulant therapy (OAT) and using sildenafil (Viagra). Haematologica, 88, ELT34. (Focused question was not answered) [PubMed] [Google Scholar]
- Garcia R. I. (2013). Periodontitis may increase likelihood of erectile dysfunction in Taiwanese men. Journal of Evidence-Based Dental Practice, 13, 35-36. (Comment) [DOI] [PubMed] [Google Scholar]
- Grant W. B., Sorenson M., Boucher B. J. (2013). Vitamin D deficiency may contribute to the explanation of the link between chronic periodontitis and erectile dysfunction. Journal of Sexual Medicine, 10, 2353-2354. (Letter to the editor) [DOI] [PubMed] [Google Scholar]
- Gulati M., Anand V., Jain N., Anand B., Bahuguna R., Govila V., Rastogi P. (2013). Essentials of periodontal medicine in preventive medicine. International Journal of Preventive Medicine, 4, 988-994. (Focused question was not answered) [PMC free article] [PubMed] [Google Scholar]
- Harte C. B., Meston C. M. (2008). Acute effects of nicotine on physiological and subjective sexual arousal in nonsmoking men: A randomized, double-blind, placebo-controlled trial. Journal of Sexual Medicine, 5, 110-121. Erratum in: Journal of Sexual Medicine, 2010, 3803. (Focused question was not answered) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Justo D., Heruti R. J. (2009). Incorporating a sexual questionnaire in screening examinations. Harefuah, 148, 646-649,655. (Focused question was not answered) [PubMed] [Google Scholar]
- Kabalin J. N., Kessler R. (1988). Infectious complications of penile prosthesis surgery. Journal of Urology, 139, 953-955. (Focused question was not answered) [DOI] [PubMed] [Google Scholar]
- Katsiki N., Athyros V. G., Karagiannis A., Wierzbicki A. S., Mikhailidis D. P. (2014). Should we expand the concept of coronary heart disease equivalents? Current Opinion in Cardiology, 29, 389-395. (Focused question was not answered) [DOI] [PubMed] [Google Scholar]
- Otomo-Corgel J., Pucher J. J., Rethman M. P., Reynolds M. A. (2012). State of the science: Chronic periodontitis and systemic health. Journal of Evidence-Based Dental Practice, 12(3 Suppl.), 20-28. (Focused question was not answered) [DOI] [PubMed] [Google Scholar]
- Peng S., Zhang D. X. (2009). Chronic periodontal disease may be a sign for erectile dysfunction in men. Medical Hypotheses, 73, 859-860. (Comment) [DOI] [PubMed] [Google Scholar]
- Siasos G., Tsigkou V., Kokkou E., Oikonomou E., Vavuranakis M., Vlachopoulos C., . . . Tousoulis D. (2014). Smoking and atherosclerosis: Mechanisms of disease and new therapeutic approaches. Current Medicinal Chemistry, 21, 3936-3948. (Focused question was not answered) [DOI] [PubMed] [Google Scholar]
- Trost L. W., Serefoglu E., Gokce A., Linder B. J., Sartor A. O., Hellstrom W. J. (2013). Androgen deprivation therapy impact on quality of life and cardiovascular health, monitoring therapeutic replacement. Journal of Sexual Medicine, 10(Suppl. 1), 84-101. (Focused question was not answered) [DOI] [PubMed] [Google Scholar]
- Zuo Z., Jiang J., Jiang R., Chen F., Liu J., Yang H., Cheng Y. (2011). Effect of periodontitis on erectile function and its possible mechanism. Journal of Sexual Medicine, 8, 2598-2605. (Experimental study) [DOI] [PubMed] [Google Scholar]
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- Al Amri M. D., Kellesarian S. V., Al-Kheraif A. A., Malmstrom H., Javed F., Romanos G. E. (2016). Effect of oral hygiene maintenance on HbA1c levels and peri-implant parameters around immediately-loaded dental implants placed in type-2 diabetic patients: 2 Years follow-up. Clinical Oral Implants Research. Advance online publication. doi: 10.1111/Clr.12758 [DOI] [PubMed] [Google Scholar]
- Ayta I. A., McKinlay J. B., Krane R. J. (1999). The likely worldwide increase in erectile dysfunction between 1995 and 2025 and some possible policy consequences. British Journal of Urology International, 84, 50-56. [DOI] [PubMed] [Google Scholar]
- Blick C., Ritchie R. W., Sullivan M. E. (2016). Is erectile dysfunction an example of abnormal endothelial function? Current Vascular Pharmacology, 14, 163-167. [DOI] [PubMed] [Google Scholar]
- Chen B., Lu Y. N., Han Y. F., Huang X. Y., Hu K., Wang Y. X., Huang Y. R. (2007). IIEF-5 cannot be used as a tool for diferential diagnosis of vasculogenic erectile dysfunction. Zhonghua Nan Ke Xue, 13, 118-121. [PubMed] [Google Scholar]
- Chrysanthakopoulos N. A. (2015). Risk factors for the progression of periodontal disease in a Greek adult population. Journal of Investigative and Clinical Dentistry. Advance online publication. doi: 10.1111/Jicd.12199 [DOI] [PubMed] [Google Scholar]
- Diehm N., Borm A. K., Keo H. H., Wyler S. (2015). Interdisciplinary options for diagnosis and treatment of organic erectile dysfunction. Swiss Medical Weekly, 145, W14268. doi: 10.4414/Smw.2015.14268 [DOI] [PubMed] [Google Scholar]
- Eaton C. B., Liu Y. L., Mittleman M. A., Miner M., Glasser D. B., Rimm E. B. (2007). A retrospective study of the relationship between biomarkers of atherosclerosis and erectile dysfunction in 988 men. International Journal of Impotence Research, 19, 218-225. doi: 10.1038/Sj.Ijir.3901519 [DOI] [PubMed] [Google Scholar]
- Elnashar A., Gadallah A., Abdelaal A., Soliman I., Youssef M. (2012). Can the International Index of Erectile Function (IIEF-5) be used as a diagnostic tool to the severity of vasculogenic erectile dysfunction? Middle East Fertility Society Journal, 17, 101-104. [Google Scholar]
- Eltas A., Oguz F., Uslu M. O., Akdemir E. (2013). The effect of periodontal treatment in improving erectile dysfunction: A randomized controlled trial. Journal of Clinical Periodontology, 40, 148-154. doi: 10.1111/Jcpe.12039 [DOI] [PubMed] [Google Scholar]
- Ghiraldini B., Conte A., Casarin R. C., Casati M. Z., Pimentel S. P., Cirano F. R., Ribeiro F. V. (2015). Influence of glycemic control on peri-implant bone healing: 12-Month outcomes of local release of bone-related factors and implant stabilization in type 2 diabetics. Clinical Implant Dentistry and Related Research. Advance online publication. doi: 10.1111/Cid.12339 [DOI] [PubMed] [Google Scholar]
- Higashi Y., Goto C., Jitsuiki D., Umemura T., Nishioka K., Hidaka T., . . . Taguchi A. (2008). Periodontal infection is associated with endothelial dysfunction in healthy subjects and hypertensive patients. Hypertension, 51, 446-453. doi: 10.1161/Hypertensionaha.107.101535 [DOI] [PubMed] [Google Scholar]
- Javed F., Al-Rasheed A., Almas K., Romanos G. E., Al-Hezaimi K. (2012). Effect of cigarette smoking on the clinical outcomes of periodontal surgical procedures. American Journal of the Medical Sciences, 343, 78-84. doi: 10.1097/Maj.0b013e318228283b [DOI] [PubMed] [Google Scholar]
- Javed F., Bashir Ahmed H., Romanos G. E. (2014). Association between environmental tobacco smoke and periodontal disease: A systematic review. Environmental Research, 133, 117-122. doi: 10.1016/J.Envres.2014.05.008 [DOI] [PubMed] [Google Scholar]
- Javed F., Kellesarian S. V., Al-Kheraif A. A., Ranna V., Qadri T., Yunker M., . . . Romanos G. E. (2016). Effect of Nd:Yag laser-assisted non-surgical periodontal therapy on clinical periodontal and serum biomarkers in patients with and without coronary artery disease: A short-term pilot study. Lasers in Surgery and Medicine. Advance online publication. doi: 10.1002/Lsm.22483 [DOI] [PubMed] [Google Scholar]
- Javed F., Romanos G. E. (2009). Impact of diabetes mellitus and glycemic control on the osseointegration of dental implants: A systematic literature review. Journal of Periodontology, 80, 1719-1730. doi: 10.1902/Jop.2009.090283 [DOI] [PubMed] [Google Scholar]
- Kalka D., Domagala Z., Rakowska A., Womperski K., Franke R., Sylwina-Krauz E., . . . Pilecki W. (2015). Modifiable risk factors for erectile dysfunction: An assessment of the awareness of such factors in patients suffering from ischaemic heart disease. International Journal of Impotence Research, 28, 14-19. doi: 10.1038/Ijir.2015.26 [DOI] [PubMed] [Google Scholar]
- Keller J. J., Chung S. D., Lin H. C. (2012). A nationwide population-based study on the association between chronic periodontitis and erectile dysfunction. Journal of Clinical Periodontology, 39, 507-512. doi: 10.1111/J.1600-051x.2012.01879.X [DOI] [PubMed] [Google Scholar]
- Lee D. M., Tajar A., Ravindrarajah R., Pye S. R., O’Connor D. B., Corona G., . . . O’Neill T. W. (2013). Frailty and sexual health in older European men. Journals of Gerontology. Series A: Biological Sciences & Medical Sciences, 68, 837-844. doi: 10.1093/Gerona/Gls217 [DOI] [PubMed] [Google Scholar]
- Lee J. H., Lee J. S., Park J. Y., Choi J. K., Kim D. W., Kim Y. T., Choi S. H. (2015). Association of lifestyle-related comorbidities with periodontitis: A nationwide cohort study in Korea. Medicine (Baltimore), 94, e1567. doi: 10.1097/Md.0000000000001567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsumoto S., Matsuda M., Takekawa M., Okada M., Hashizume K., Wada N., . . . Kakizaki H. (2014). Association of ED with chronic periodontal disease. International Journal of Impotence Research, 26, 13-15. doi: 10.1038/Ijir.2013.30 [DOI] [PubMed] [Google Scholar]
- NIH Consensus Conference: Impotence: NIH Consensus Development Panel on Impotence. (1993). Journal of American Medical Association, 270, 83-90. doi: 10.1001/jama.1993.03510010089036 [DOI] [PubMed] [Google Scholar]
- Oates T. W., Dowell S., Robinson M., McMahan C. A. (2009). Glycemic control and implant stabilization in type 2 diabetes mellitus. Journal of Dental Research, 88, 367-371. doi: 10.1177/0022034509334203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oguz F., Eltas A., Beytur A., Akdemir E., Uslu M. O., Gunes A. (2013). Is there a relationship between chronic periodontitis and erectile dysfunction? Journal of Sexual Medicine, 10, 838-843. doi: 10.1111/J.1743-6109.2012.02974.X [DOI] [PubMed] [Google Scholar]
- Ponholzer A., Temml C., Mock K., Marszalek M., Obermayr R., Madersbacher S. (2005). Prevalence and risk factors for erectile dysfunction in 2869 men using a validated questionnaire. European Urology, 47, 80-86. doi: 10.1016/J.Eururo.2004.08.017 [DOI] [PubMed] [Google Scholar]
- Saffi M. A., Furtado M. V., Polanczyk C. A., Montenegro M. M., Ribeiro I. W., Kampits C., . . . Rabelo-Silva E. R. (2015). Relationship between vascular endothelium and periodontal disease in atherosclerotic lesions: Review article. World Journal of Cardiology, 7, 26-30. doi: 10.4330/Wjc.V7.I1.26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selvin E., Burnett A. L., Platz E. A. (2007). Prevalence and risk factors for erectile dysfunction in the US. American Journal of Medicine, 120, 151-157. doi: 10.1016/J.Amjmed.2006.06.010 [DOI] [PubMed] [Google Scholar]
- Sharma A., Pradeep A. R., Raju P. A. (2011). Association between chronic periodontitis and vasculogenic erectile dysfunction. Journal of Periodontology, 82, 1665-1669. doi: 10.1902/Jop.2011.110049 [DOI] [PubMed] [Google Scholar]
- Skeldon S. C., Detsky A. S., Goldenberg S. L., Law M. R. (2015). Erectile dysfunction and undiagnosed diabetes, hypertension, and hypercholesterolemia. Annals of Family Medicine, 13, 331-335. doi: 10.1370/Afm.1816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsao C. W., Liu C. Y., Cha T. L., Wu S. T., Chen S. C., Hsu C. Y. (2015). Exploration of the association between chronic periodontal disease and erectile dysfunction from a population-based view point. Andrologia, 47, 513-518. doi: 10.1111/And.12294 [DOI] [PubMed] [Google Scholar]
- Uppal R. S., Bhandari R., Singh K. (2014). Association between erectile dysfunction and chronic periodontitis: A clinical study. Indian Journal of Dental Research, 25, 430-433. doi: 10.4103/0970-9290.142516 [DOI] [PubMed] [Google Scholar]
- Zadik Y., Bechor R., Galor S., Justo D., Heruti R. J. (2009). Erectile dysfunction might be associated with chronic periodontal disease: Two ends of the cardiovascular spectrum. Journal of Sexual Medicine, 6, 1111-1116. doi: 10.1111/J.1743-6109.2008.01141.X [DOI] [PubMed] [Google Scholar]
- Zeng X., Zhang Y., Kwong J. S., Zhang C., Li S., Sun F., . . . Du L. (2015). The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: A systematic review. Journal of Evidence-Based Medicine, 8, 2-10. doi: 10.1111/Jebm.12141 [DOI] [PubMed] [Google Scholar]