Abstract
Objective
To determine whether changes in preoperative osteoarthritis (OA) symptoms are associated with improvement after total knee replacement (TKR) and to identify predictors of clinically significant improvement.
Methods
Data on Osteoarthritis Initiative participants who were annually assessed and underwent TKR were included. T0 was the assessment prior to TKR while T-1 was the assessment prior to that. T+2 was the second assessment after TKR. We compiled data on the Western Ontario and McMaster Universities OA Index (WOMAC), OA-related symptoms and radiographic severity. We defined clinically significant improvement as improvement in WOMAC total score ≥ to the minimal important difference (MID) (0.5 SD of mean change) between T0 and T+2 and also considered other definitions of improvement. Logistic regression models were performed to evaluate the relationship between improvement and preoperative measures.
Results
Improved (n=211) compared to unimproved (n=58) patients had greater worsening of their WOMAC pain (p=0.002) and disability (p<0.001) from T-1 to T0. Preoperative measures as predictors of improvement included: higher WOMAC disability (OR 1.08, p<0.001), presence of chronic OA symptoms in the surgical knee (OR 5.77, p=0.033), absence of OA-related symptoms in the contralateral knee (OR 9.25, p<0.001), exposure to frequent knee-bending (OR 3.46, p=0.040), and having a Kellgren-Lawrence x-ray grade of ≥2 in the contralateral knee (OR 4.71, p=0.010).
Conclusions
More than 75% of participants had improvement after TKR. Improved patients were more likely to have escalation of OA pain and disability prior to surgery than unimproved patients. Other pre-operative measures predicted improvement after TKR.
Keywords: osteoarthritis, knee, joint replacement surgery, improvement, post-operative outcomes
INTRODUCTION
Knee osteoarthritis (OA) is a highly prevalent and disabling disease [1, 2]. When conservative (e.g. pharmacologic and non-pharmacologic) therapies no longer provide adequate relief and functional improvement, the Osteoarthritis Research Society International (OARSI) and others recommend total knee replacement (TKR) surgery [3]. There is no consensus on the criteria for the timing of TKR, and there has been a dramatic increase in the numbers of TKRs performed in the US [4].
Well-validated and patient-reported health-related quality of life (HRQL) instruments have been used to evaluate TKR outcomes and its appropriateness [5–13]. The instruments represent individual responses to the physical, mental and social effects of illness on daily living [14, 15]. Among HRQL instruments used to gauge TKR surgery outcomes, the Western Ontario and McMaster University Osteoarthritis Index (WOMAC) and the Short Form-36 (SF-36) are most frequently used [5–12]. Although there has been an attempt to define appropriateness for TKR [16], these criteria have not been widely accepted and there is wide variability in the clinical status of patients undergoing TKR [13]. Furthermore, the linkage between fulfilling these criteria and improvement after TKR is unknown.
There are different approaches to measuring patients’ responses to treatments using these HRQL instruments. The minimal important difference (MID) approach defines clinical improvement based on overall improvement of the WOMAC score [17]. The OARSI/Outcome Measures in Rheumatology (OMERACT) approach defines improvement based on absolute and relative changes in WOMAC scores [18]. The patient acceptable symptom state (PASS) is an approach based on achieving a certain WOMAC score that represents a satisfactory state of wellbeing [19]. Essentially, outcomes in TKR can be conceptualized based on change in outcome score over time or on achieving an outcome score at a specific point in time [20]. In other words, the metric of success from joint replacement can be measured based on the amount of improvement from different levels of disability or achieving a final status of a target in terms of the level of functioning, irrespective of the prior level of disability [21].
Regardless of the definition of improvement, the determinants of clinical improvement following joint replacement are largely understudied. Yet, this critical information can provide guidance for providers and patients in making informed decisions on proceeding with TKR surgery or not. Hawker et al [8] found four preoperative variables that discriminately predicted having a good outcome following joint arthroplasty based on the MID criterion. Patients with greater pain and disability, less comorbidity, OA instead of inflammatory arthritis, and fewer troublesome joints were found to be most likely to experience good outcome [8]. The trajectory of patients’ pre-surgical changes in symptoms or disability was not examined, however. Riddle et al [9] found an escalation of pain and worsening function ~2.5 years prior to surgery among patients who underwent TKR, but did not examine whether the trajectory of pre-TKR changes in OA-related symptoms and disability influenced improvement in TKR outcomes.
The Osteoarthritis Initiative (OAI) dataset provides an excellent opportunity to address the limitations of previous studies [9, 22, 23]. The OAI is a prospective longitudinal cohort study of persons with, or at high risk of developing, knee OA. Its study design allows observation of participants’ WOMAC and other HRQL measure scores years prior to and after TKR. These self-reported measures are also less susceptible to response bias, as participants’ responses do not directly determine their providers’ decision to offer TKR surgery or not. As participants were recruited from four clinical centers nationwide, data results should also have better generalizability in comparison to studies that recruit research subjects from only a single site.
The objectives of this study were to evaluate OA-related outcomes up to 2 years after TKR surgery in individuals with knee OA, and to determine whether changes in preoperative HRQL measures were associated with improvement in OA-related pain and disability after surgery. We also evaluated the specific predictors of various definitions of clinically significant improvement following TKR. We hypothesized that significant worsening in preoperative pain, disability, and other OA-related symptoms would be associated with improvement after TKR.
METHODS
Participants
Data were obtained from the publicly available OAI database (http://oai.epi-ucsf.org/datarelease/) gathered April, 2014. Subjects 45–79 years of age were recruited from four OAI Clinical Centers [University of Maryland School of Medicine and the Johns Hopkins University (Baltimore, MD), Ohio State University (Columbus, OH), University of Pittsburgh (Pitsburgh, PA) and Memorial Hospital of Rhode Island (Pawtucket, RI)] and were assessed annually. The institutional review boards at each of the sites approved the study, and all participants gave informed consent.
For this study, we examined OAI data from participants who underwent TKR surgery (verified by chart review or by x-ray) from the 12-month visit to the 72-month visit. The annual OAI visit just prior to TKR will be hereafter referred to as “T0”. The annual OAI visit after TKR was reported will be referred to as “T+1”; this may occur anytime from one day to one year after T0. “T+2” will be the participant visit one year following the T+1 visit. “T-1” is the annual OAI visit one year prior to the T0 visit. Only those with T0 and T+2 WOMAC data were included in the study. We excluded those who had partial knee replacement (i.e. unicompartmental), those who had a history of inflammatory arthritis (e.g., rheumatoid arthritis), and those who died prior to T+2. Those with a reported TKR at the 12-month visit were also excluded; they could not contribute data to the T-1 measures, as T0 was their OAI baseline visit.
Study Measures
Clinical Assessment
Health-related quality of life was assessed using the Short Form Health Survey (SF-12), from which the physical and mental component scores were calculated [24]. Depressive symptoms were assessed using the validated Center for Epidemiologic Studies Depression Scale (CES-D) [25]. Comorbidity was measured using the Katz-modified Charlson Comorbidity Index Questionnaire [26].
OA-Related Measures
OA-related disease severity was determined using the 24-item WOMAC, a reliable and validated measure that consists of 3 subscales, with higher scores indicating increased pain, stiffness, and disability [27]. The total and subscale scores were normalized to the 0–100 scale.
The Knee Injury and Osteoarthritis Outcome Score (KOOS), a reliable and validated measure, is a 42-item questionnaire that encompasses: pain, other symptoms, function in sports and recreation, and knee-related quality of life [28]. Scores range from 0 to 100, with 0 representing extreme problems and 100 representing no problems.
We also determined participant-reported frequent knee-bending activities on most days during the previous 30 days. Frequent knee-bending activities included: 1) kneeling for ≥30 minutes, 2) squatting for ≥30 minutes, or getting in and out of a squatting position ≥10 times, 3) climbing ≥10 flights of stairs, and 4) lifting or moving objects weighing ≥25 pounds. Those who performed ≥1 of these activities were classified as frequent knee-benders.
Pain severity of the knee in the past 7 days was measured using a numerical rating scale (range: 0–10). The presence of pain, aching, or stiffness of the surgically replaced (i.e. index) knee, contralateral knee, and both hips was also determined by asking participants if they had had any of these symptoms in the joints for most days of the month in at least one month in the past year.
Performance Measures
Functional performance was assessed using the timed 20-meter walk and the chair stand test. The timed 20-meter walk is a standard outcome measure for OA [29]. The chair stand test measures the time required for 5 repetitions to rise from a chair and sit down.
Radiographic Measures
The radiologic severity of knee OA prior to surgery in both knees was assessed using the Kellgren-Lawrence (K-L) scoring system [30].
To deal with T0 missing data which were not assessed annually in OAI (e.g. demographics), data from previous waves were carried forward.
Definitions of Improved vs. Unimproved
For this study, we first defined improved participants as those with an overall improvement in knee WOMAC total score ≥ to the MID after TKR. MID was ½ of the standard deviation of the difference between the pre-TKR summary and post-TKR summary scores [17]. We used the WOMAC total scores gathered during T0 as the pre-surgery values and the scores obtained T+2 as the post-surgery values. The calculated MID value for the WOMAC total scores was a 9.4 point improvement. Unimproved participants were those who did not have improvement in WOMAC total score ≥ to the MID, including those whose baseline scores were already below the MID. The proportion of patients who were improved and unimproved following TKR was then determined.
The MID definition of improvement has the advantage of focusing on the general impact of TKR on knee pain, stiffness and disability [8]. As a sensitivity analysis, we also performed secondary analyses to examine the proportions of patients with improvement using alternative definitions. The OARSI/OMERACT criterion entails improvement in the WOMAC pain and disability score of ≥20% and absolute change in each of the score of ≥10 points [18]. Although, the MID and OARSI/OMERACT definitions of improvement are widely used in rheumatology research, they may also misclassify patients based on their baseline WOMAC scores [31]. The PASS criterion is defined as the value beyond which patients consider themselves satisfied with actual OA symptoms (WOMAC pain <32.4 or WOMAC disability <31.0) [19]. However, uncertainty remains on what the cut-off points should be, and patient factors may also influence what patients consider satisfactory [32].
Statistical Analysis
Analyses were performed using STATA 11.2 (StataCorp LP, College Station, TX, USA). We compared the baseline (T0) demographic, psychosocial and clinical characteristics between improved and unimproved OAI subjects. Continuous variables were compared by t-test or Wilcoxon rank sum test. Categorical variables were compared by χ2 analysis or Fisher’s exact test. Using an identical approach, we also compared the pre-surgical change of OA-related clinical measures from T-1 to T0 between improved and unimproved participants. We also evaluated the OA-related clinical characteristics of subjects included at T0, T+1 and T+2. Comparisons of mean values were done using paired t-test or Wilcoxon rank sum test.
To determine the most significant predictors of improvement after TKR, logistic regression models were used. Focusing on explanatory variables associated with or tending to associate with improvement (defined as p<0.20) based on the bivariate analyses described above, multivariable main-effects models were created. The approach started with separate models that included variables within the different categories of explanatory variables. Performance measures were excluded during this model-building stage, though, because of the large number of missing cases. Only variables that were associated with improvement with a p<0.20 when adjusted for other variables within their categories were included. Based on these models, a final multivariable model that included significant variables from all categories of explanatory variables was built.
As the time difference from TKR to T+2 (and alternately from T0 to TKR) vary and may affect the reported TKR outcome [9], we conducted sensitivity analyses to examine the impact of these time differences. The final model was adjusted for time between TKR and T+2. Interaction terms between time from TKR and T+2 and all independent variables included in final model were also added in. We then checked the impact of these terms on the quality of the model (by observing Akaike information criteria values) and the estimated main effects of the independent variables in the final model.
Identical strategies and sensitivity analyses were conducted upon determining the predictors of improvement using the other alternative definitions of improvement.
RESULTS
There were 328 OAI participants who had knee replacements after the 12 month follow-up through the 72 month follow-up visit (Appendix 1). A total of 269 participants underwent TKR surgery and had preoperative and postoperative WOMAC data available to estimate our outcome definition of improvement (Table 1). Mean age at the visit immediately prior to surgery (T0) was 67 years. The majority were female (61.0%) and white (84.4%). Many (48.3%) were considered obese or morbidly obese.
Table 1.
Baseline (T0) sociodemographic and clinical characteristics of patients who underwent TKR surgery by improvement (MID criterion) in WOMAC total score from T0 to T+2.
| Improved (n = 211) | Unimproved (n = 58) | p-value | |
|---|---|---|---|
| SOCIODEMOGRAPHIC | |||
| Age, mean ± SD | 67.56 ± 8.54 | 66.53 ± 8.24 | 0.4156 |
| Sex, # (%) female | 127 (60.19) | 37 (63.79) | 0.6513 |
| Race, #(%) | 0.8064 | ||
| White | 179 (84.83) | 48 (82.76) | |
| African-American | 22 (10.43) | 6 (10.34) | |
| Others | 10 (4.74) | 4 (6.90) | |
| Marital status, # (%) married | 153 (75.37) | 39 (69.64) | 0.3927 |
| Education, #(%) | 0.5144 | ||
| ≤High school | 38 (18.10) | 14 (24.14) | |
| Post-secondary training | 118 (56.19) | 32 (55.19) | |
| Graduate degree | 54 (25.71) | 12 (20.69) | |
| Medical insurance, # (%) with health coverage* | 203 (99.02) | 56 (98.25) | 0.5225 |
| Income, # (%) | 0.9641 | ||
| <$24,999 | 24 (12.06) | 5 (9.62) | |
| $25,000–$49,999 | 61 (30.65) | 17 (32.69) | |
| $50,000–$99,999 | 77 (38.69) | 20 (38.46) | |
| ≥$100,000 | 37 (18.59) | 10 (19.23) | |
| CLINICAL | |||
| Smoke, ever, #(%) | 0.4725 | ||
| Never | 124 (60.49) | 35 (60.34) | |
| Currently | 11 (5.37) | 1 (1.72) | |
| Former | 70 (34.15) | 22 (34.15) | |
| Alcohol use past 12 months, n(%) | 166 (81.37) | 41 (73.21) | 0.1923 |
| SF-12, Physical Health, mean ± SD | 37.95 ± 9.17 | 41.02 ± 9.77 | 0.0287 |
| SF-12, Mental Health, mean ± SD | 55.59 ± 8.36 | 57.32 ± 6.62 | 0.1028 |
| Katz Comorbidity Index, #(%) | 0.0998 | ||
| 0 | 146 (71.22) | 38 (65.52) | |
| 1 | 30 (14.63) | 15 (25.86) | |
| ≥2 | 29 (14.15) | 5 (8.62) | |
| CES-D Score, # (%) ≥16† | 25 (12.14) | 4 (7.02) | 0.3451 |
| Body mass index, n(%) | 0.0786 | ||
| Underweight/normal weight | 30 (14.78) | 12 (21.43) | |
| Overweight | 78 (38.42) | 14 (25.00) | |
| Obese | 57 (28.08) | 23 (41.07) | |
| Morbidly Obese | 38 (18.72) | 7 (12.50) | |
Coverage=private, prepaid plans (e.g. HMO), PPO, government-sponsored (Medicare, Medicaid or VA)
CES-D treshold for identifying individuals at high risk for clinical depression
CES-D=Center for Epidemiologic Studies Depression Scale; SF-12=Short Form 12
Post-Surgical Outcomes
OA-related clinical scores of participants at T0, T+1 year and T+2 years are presented in Table 2. WOMAC total, pain, disability and stiffness scores were improved at T+1 (p<0.0001, all subscales) and at T+2 (p<0.0001, all subscales) in comparison to scores at T0. KOOS scores in all four dimensions were also improved at T+1 (p<0.0001, all dimensions) and at T+2 (p<0.0001, all dimensions) compared to scores at T0. By T+2, mean 20-meter walk and chair stand paces were faster when compared to rates at T0 (p<0.05 in both).
Table 2.
Comparing knee-specific and person-specific pain, disability and functional performance measures at T0, T+1 and T+2
| T0 | T+1 year | T+2 years | |
|---|---|---|---|
| Knee-Specific | |||
| WOMAC Total, mean ± SD | 35.52 ± 17.03 | 18.50 ± 15.54† | 11.86 ± 13.04† |
| WOMAC Pain subscale, mean ± SD | 35.73 ± 19.10 | 17.35 ± 17.49† | 10.19 ± 14.42† |
| WOMAC Disability subscale, mean ± SD | 34.66 ± 17.70 | 17.61 ± 15.63† | 11.44 ± 13.27† |
| WOMAC Stiffness subscale, mean ± SD | 42.33 ± 21.70 | 29.46 ± 21.02† | 19.70 ± 19.01† |
| KOOS Pain, mean ± SD | 58.13 ± 18.38 | 77.78 ± 19.01† | 86.98 ± 14.90† |
| KOOS Symptoms, mean ± SD | 62.28 ± 19.31 | 74.64 ± 17.63† | 85.44 ± 12.47† |
| Knee Pain Severity (last 7 days), mean ± SD | 6.40 ± 2.38 | 3.10 ± 2.75† | 2.02 ± 2.29† |
| Person-Specific | |||
| KOOS Sports/Recreation, mean ± SD | 43.40 ± 25.93 | 58.21 ± 26.30† | 66.88 ± 25.52† |
| KOOS Quality of Life, mean ± SD | 40.99 ± 17.31 | 56.41 ± 20.24† | 65.15 ± 21.61† |
| Frequent Knee Bending, n(%)* | 166 (0.81) | 153 (0.79) | 136 (0.88)‡ |
| Chair Stand (reps/min), mean ± SD | 26.23 ± 6.95 | 26.34 ± 7.25 | 28.23 ± 8.67‡ |
| 20 Meter Walk (m/min), mean ± SD | 1.18 ± .21 | 1.18 ± .20 | 1.22 ± .23‡ |
Defined as at least one exposure to any of the following activities: 1) kneeling for ≥30 minutes; 2) squatting for ≥30 minutes, or getting into and out of a squatting position 10 or more times; 3) climbing ≥10 flights of stairs; 4) lifting or moving objects weighing ≥25 pounds by hand
p<0.0001, T0 to T+1 (or T+2) difference
p<0.05, T0 to T+1 (or T+2) difference
KOOS=Knee Injury and Osteoarthritis Outcome Score; WOMAC=Western Ontario and McMaster Universities OA Index (scaled from 0 to 100, higher = worse)
Improved vs. Unimproved Participants
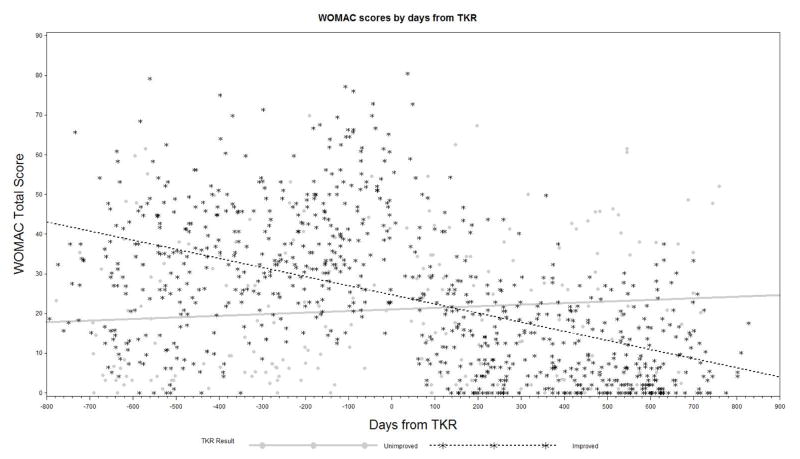
Figure 1 plots the WOMAC total scores of OAI participants included in the study prior to and after TKR. In comparison to scores prior to TKR, WOMAC total scores of improved participants were generally lower after TKR.
Figure 1.
WOMAC total scores of OAI participants who underwent TKR surgery over time
A total of 211 OAI met our a priori MID criterion for improvement and were considered “improved” following TKR (Table 1). Improved participants had worse physical health than unimproved participants at T0 (SF-12 Physical, 38.0 vs. 41.0, p=0.0287). Improved, compared to unimproved, subjects also had higher preoperative WOMAC pain (39.3 vs. 22.7, p<0.0001), disability (39.2 vs. 18.2, p<0.0001) and stiffness (46.5 vs. 27.4, p<0.0001) subscale scores. They also had lower preoperative KOOS scores in all four dimensions (Table 3). Those who improved were also more likely to report having OA-related symptoms most days of the month in the past year (i.e., chronic, frequent OA symptoms) in the index knee joint (96.7% vs. 77.6%, p<0.0001). Mean knee pain severity prior to TKR was also higher among improved than unimproved subjects (6.9 vs. 4.7, p<0.0001).
Table 3.
Baseline OA-related characteristics of patients who underwent TKR surgery by improvement (MID criterion) in WOMAC total score from T0 to T+2.
| Improved (n = 211) | Unimproved (n = 58) | p-value | |
|---|---|---|---|
| WOMAC Total, mean ± SD | 39.81 ± 14.55 | 19.92 ± 16.37 | <0.0001 |
| WOMAC Pain subscale, mean ± SD | 39.31 ± 17.86 | 22.73 ± 17.92 | <0.0001 |
| WOMAC Disability subscale, mean ± SD | 39.17 ± 15.08 | 18.23 ± 16.86 | <0.0001 |
| WOMAC Stiffness subscale, mean ± SD | 46.45 ± 20.21 | 27.37 ± 20.47 | <0.0001 |
| KOOS Pain, mean ± SD | 53.98 ± 16.12 | 73.21 ± 18.34 | <0.0001 |
| KOOS Symptoms, mean ± SD | 59.10 ± 17.73 | 73.84 ± 20.51 | <0.0001 |
| KOOS Sports/Recreation, mean ± SD | 38.59 ± 24.01 | 55.48 ± 26.99 | 0.0013 |
| KOOS Quality of Life, mean ± SD | 38.10 ± 15.26 | 51.51 ± 20.19 | <0.0001 |
| Frequent Knee Bending, n(%)* | 131 (82.91) | 35 (72.92) | 0.1456 |
| Knee Pain Severity (last 7 days), mean ± SD | 6.85 ± 1.98 | 4.74 ± 2.95 | <0.0001 |
| OA Symptoms in Index Knee, # (%)† | 204 (96.68) | 45 (77.59) | < 0.0001 |
| OA Symptoms in Contralateral Knee, # (%)† | 106 (50.24) | 36 (62.07) | 0.1374 |
| OA Symptoms in Same Side Hip, #(%)† | 45 (21.84) | 10 (17.86) | 0.5828 |
| OA Symptoms in Contralateral Hip, #(%)† | 37 (17.87) | 4 (7.14) | 0.0606 |
| Chair Stand (reps/min), mean ± SD | 25.74 ± 6.94 | 27.76 ± 6.85 | 0.1241 |
| 20 Meter Walk (m/min), mean ± SD | 1.18 ± 0.20 | 1.18 ± 0.24 | 0.9367 |
| Index Knee, K-L Grade, n(%) | 0.1810 | ||
| 0–1 | 5 (2.63) | 3 (5.77) | |
| 2 | 26 (13.68) | 11 (21.15) | |
| 3 | 53 (27.89) | 17 (32.69) | |
| 4 | 106 (55.79) | 21 (40.38) | |
| Contralateral Knee, K-L Grade, n(%) | |||
| 0–1 | 35 (19.44) | 14 (32.56) | 0.2787 |
| 2 | 64 (35.56) | 11 (25.58) | |
| 3 | 60 (33.33) | 13 (30.23) | |
| 4 | 21 (11.67) | 5 (11.63) | |
| Time Duration Between TKR & T+2 (days), mean ± SD | 558.2 ± 107.7 | 518.5 ± 107.2 | 0.0134 |
| Days Between T0 & TKR, n (%) | |||
| 0–126 | 79 (37.44) | 11 (18.97) | 0.0046 |
| 127–220 | 71 (33.65) | 18 (31.03) | |
| ≥221 | 61 (28.91) | 29 (50.00) | |
Defined as at least one exposure to any of the following activities: 1) kneeling for ≥30 minutes; 2) squatting for ≥30 minutes; 3) climbing ≥10 flights of stairs; 4) lifting or moving objects weighing ≥25 pounds by hand
Joints with pain/aching/stiffness most days of the month in the past 12 months
K-L=Kellgren-Lawrence Grading Scale; KOOS=Knee Injury and Osteoarthritis Outcome Score; WOMAC=Western Ontario and McMaster Universities OA Index (scaled from 0 to 100, higher = worse)
Those who improved were also more likely to have had worsening of their WOMAC total, pain, disability and stiffness scores from T-1 to T0 (Table 4). Of note, changes in the functional performance measures from T-1 to T0 were not associated with improvement.
Table 4.
The relationship between change in OA-related characteristics prior to total knee replacement (from T-1 to T0) and improvement (defined by the MID criterion) in WOMAC total score from T0 to T+2.
| Improved (n = 192) | Unimproved (n = 52) | p-value | |
|---|---|---|---|
| Δ WOMAC Total, mean ± SD | 9.76 ± 16.56 | 0.38 ± 12.72 | <0.0001 |
| Δ WOMAC Pain, mean ± SD | 9.65 ± 19.53 | 2.48 ± 13.19 | 0.0024 |
| Δ WOMAC Disability, mean ± SD | 9.87 ± 17.22 | −.16 ± 13.38 | <0.0001 |
| Δ WOMAC Stiffness, mean ± SD | 9.11 ± 23.23 | −.24 ± 20.34 | 0.0088 |
| Δ Knee Pain Severity (last 7 days), mean ± SD | 1.33 ± 2.62 | .63 ± 2.40 | 0.1105 |
| Δ Chair Stand (reps/min), mean ± SD | −1.18 ± 5.13 | .46 ± 4.57 | 0.1148 |
| Δ 20 Meter walk (m/min), mean ± SD | −.07 ± .14 | −.04 ± .15 | 0.2248 |
| Any worsening of Index Knee K-L Grade, n(%) | 23 (17.83) | 6 (15.00) | 0.8124 |
| Any decrease in knee bending activities, n(%) | 35 (25.55) | 17 (41.46) | 0.0768 |
K-L=Kellgren-Lawrence Grading Scale;; WOMAC=Western Ontario and McMaster Universities OA Index (scaled from 0 to 100, higher = worse)
Factors Associated with Improvement (MID Criterion)
Table 5 shows our preoperative factors associated with improvement at T+2 by MID criterion. Worse OA-related disability prior to surgery (OR 1.08, 95%CI [1.04–1.12]), presence of chronic, frequent OA symptoms in the surgical knee (OR 5.77, 95%CI [1.15–28.94]), absence of chronic, frequent OA symptoms in the contralateral knee (OR 9.25, 95%CI [3.13–27.32]), prior exposure to frequent knee bending (OR 3.46, 95%CI [1.06–11.31]), and having a K-L grade ≥2 in the contralateral knee (OR 4.71, 95%CI [1.44–15.39]) were associated with an increased likelihood of achieving improvement in TKR surgery outcome.
Table 5.
Factors associated with improvement using MID Criterion and other definitions of improvement
| Adjusted OR (95% CI) | p-value | |
|---|---|---|
| MID (n = 155) | ||
| SF-12, Mental Health | 0.93 (0.84 – 1.03) | 0.167 |
| WOMAC Disability Score at T0 | 1.08 (1.04 – 1.12) | <0.001 |
| Frequent Knee Bending* | 3.46 (1.06 – 11.31) | 0.040 |
| OA Symptoms in Index Knee Joint† | 5.77 (1.15 – 28.94) | 0.033 |
| Absence of OA Symptoms in Contralateral Knee Joint† | 9.25 (3.13 – 27.32) | < 0.001 |
| Index Knee, K-L Grade 4‡ | 2.27 (0.73 – 7.04) | 0.157 |
| Contralateral Knee, K-L Grade ≥2§ | 4.71 (1.44 – 15.39) | 0.010 |
| Δ WOMAC Stiffness from T-1 to T0 | 1.02 (1.00–1.04) | 0.104 |
| PASS-WOMAC Pain (n = 167) | ||
| WOMAC Pain Score at T0 | 0.96 (0.94–0.98) | <0.001 |
| Absence of OA Symptoms in Same Side Hip† | 3.79 (1.22–11.77) | 0.021 |
| Any worsening of Index Knee’s K-L Grade from T-1 to T0 | 0.37 (0.11–1.24) | 0.107 |
| OARSI/OMERACT (n = 237) | ||
| Marital Status, Married | 1.72 (0.77–3.87) | 0.186 |
| WOMAC Disability Score at T0 | 1.09 (1.06–1.12) | <0.001 |
| Δ WOMAC Stiffness from T-1 to T0 | 1.02 (1.00–1.04) | 0.027 |
Defined as at least one exposure to any of the following activities: 1) kneeling for ≥30 minutes; 2) squatting for ≥30 minutes; 3) climbing ≥10 flights of stairs; 4) lifting or moving objects weighing ≥25 pounds by hand
Joints with pain/aching/stiffness most days of the month in the past 12 months
K-L Grade 4 vs. 0, 1, 2 or 3
K-L Grade 2, 3 or 4 vs. 0 or 1
K-L=Kellgren-Lawrence Grading Scale; SF-12=Short Form 12; WOMAC=Western Ontario and McMaster Universities OA Index
Sensitivity Analyses: Effect of time between TKR and T+2
When time between TKR and T+2 days was added in the final model, the coefficient was found to be statistically insignificant (p=0.84). It also minimally impacted the estimated main effects of the variables in the model and did not significantly change model quality. Similarly, when the interaction terms between TKR and T+2 days and the variables included in the final model were added in, none were found to be statistically significant (p>0.20). The impact on the estimated main effects was modest, and model quality only slightly changed.
Alternative Definitions of Improvement
Table 6 shows the TKR recipients by improvement status based on different definitions of improvement. In general, there was minimal discordance on classifying participants based on the different definitions (data not shown). However, classification based on the PASS criterion appears to be different from classification based on the other criteria.
Table 6.
TKR recipients classified as improved vs. unimproved by criterion
| Improved, n (%) | Unimproved, n (%) | # Unable to Improve* | |
|---|---|---|---|
| MID | |||
| WOMAC Total | 211 (78.44) | 58 (21.56) | 23 |
| WOMAC Disability | 204 (75.56) | 66 (24.44) | 28 |
| WOMAC Pain | 204 (73.91) | 72 (26.09) | 28 |
| PASS | |||
| WOMAC Disability | 253 (90.68) | 26 (9.19) | N/A |
| WOMAC Pain | 257 (90.81) | 26 (9.19) | N/A |
| OARSI/OMERACT | |||
| WOMAC Disability + Pain | 190 (70.63) | 79 (29.37) | 33 |
Participants in the unimproved group who could not achieve important change based on pre-surgical baseline scores
Minimal Important Difference=MID, Patient Acceptable Symptom State=PASS, WOMAC=Western Ontario and McMaster Universities OA Index
The socio-demographic, clinical and specific OA-related characteristics of the TKR recipients by improvement status based on PASS-WOMAC Pain and OMERACT/OARSI criteria are shown in Appendices 2 and 3, respectively. Table 5 shows the factors associated with improvement following TKR using these alternative definitions of improvement. Less pre-surgical OA-related pain (OR 0.96, 95%CI [0.94–0.98]) and the absence of chronic, frequent OA symptoms of the hip on the same side (OR 3.79, 95%CI [1.22–11.77]) predicted being in an improved state using the PASS-WOMAC pain criterion. Worse OA-related disability prior to surgery (OR 1.09, 95%CI [1.06–1.12]) and worsening of OA-related stiffness in at least the last year prior to surgery (OR 1.02, 95%CI [1.00–1.04]) are all associated with improvement based on the OMERACT/OARSI criteria.
DISCUSSION
To our knowledge, our study is the first to find a significant association between change in preoperative HRQL measures and accepted definitions of clinical improvement following TKR. We found that worsening pain, disability and stiffness due to OA in at least the last year prior to surgery were all significantly associated with an improved outcome. Moreover, we found several other preoperative measures that are independently associated with improvement following knee arthroplasty. Significant OA-related symptoms such as disability and pain in the surgical knee, minimal chronic OA symptoms in the other knee joint, preoperative exposure to frequent knee bending, and having marked radiographic OA features in the contralateral knee significantly determined improvement following TKR. Less OA-related pain in the surgical knee and absence of chronic, frequent OA symptoms in the hip on the same side predicted achievement of an acceptable symptom state. These findings have important implications for patients and physicians in the decision-making process for elective TKR and ultimately in the development of criteria for appropriateness and timing of total knee replacement for knee OA.
Using the MID or OARSI/OMERACT criterion for improvement, >70% of OAI participants who underwent TKR improved >1 year after the procedure. Using the PASS criterion, >90% had an acceptable set of OA symptoms. In contrast, Hawker et al [8] reported that only 51.9% of TKR recipients in Canada met their calculated MID for WOMAC total scores. Using attainment of a PASS score for knee pain and function as definition of having good outcome, Judge et al [33] found that 67.1% of English patients had good outcome 6 months after TKR. In a Spanish study [34], 78.8% of TKR patients were considered PASS responders and 86.3% met the OARSI/OMERACT criteria for good response one year after TKR. Differences in the proportion of patients with improvement after TKR are likely due to the varying constructs of improvement being measured, the range of follow-up period after surgery, and the differences in patient populations.
Knee OA patients typically have gradual worsening of their symptoms [22, 35]. In the only longitudinal study that quantified the trajectories of preoperative worsening of various HRQL measures in the surgical knee of patients that underwent TKR, it was found that patients experienced progression with a flat trajectory until ~2.5 years prior to surgery [9]. Around this time, there is an accelerated worsening of knee OA-related symptoms. Riddle et al [9] postulate that this preoperative worsening likely contributes to patients’ decision to undergo surgery. With a larger sample of OAI participants who underwent TKR, we found similar worsening of symptoms in at least the last year prior to surgery. In addition, our study links these pre-operative escalations of OA-related symptoms with clinical improvement at least two years following TKR. Worsening stiffness, in particular, independently predicted improvement by MID and OARSI/OMERACT criteria.
Importantly, we found that OA-related symptoms immediately prior to surgery were the most significant predictors of improvement after TKR. Specifically, the odds of having improvement by MID or OARSI/OMERACT criterion were higher for those with worse (i.e. higher) pre-TKR WOMAC disability score and those with chronic OA-related symptoms. This is consistent with Hawker et al’s prior finding that worse preoperative WOMAC summary score was associated with having good outcome following joint arthroplasty [8]. Moreover, it has been shown that low-functioning OA patients are more likely to have improvement of their WOMAC physical function score 6 months and 2 years after joint replacement [5, 6]. These findings suggest that patients with the worst preoperative HRQL measures have the most to gain from TKR, as they have a good deal of uncontrolled pain and poor function to start with [5, 6, 36]. These patients may not have better absolute outcomes than those with better preoperative HRQL scores, but they may see the biggest gain in function.
In parallel, the odds of being in an improved state by PASS criterion were higher for those with lower pre-TKR WOMAC pain score. The MID and OARSI/OMERACT criteria are based on changes in WOMAC scores [8, 18, 34]. In contrast, the PASS requires attainment of a certain absolute outcome (i.e. an absolute WOMAC pain or physical function score) [19]. Those with less OA-related symptoms are less likely to have improvement of their HRQL measures than those with more symptoms. However, they are more likely to achieve an acceptable state, with minimal symptoms, after surgery.
Having minimal OA-related symptoms in other knee or hip joints was also associated with better outcome based on both MID and PASS criteria. As OA affects many joints, studying the effect of multiple symptomatic joints on TKR recipients is relevant. High prevalence of arthritis symptoms in other joints has been associated with worse postsurgical scores for WOMAC pain and physical function following total knee or hip replacement [8, 37–39]. These studies have consistently demonstrated that the presence of arthritis symptoms in other joints tends to attenuate the beneficial effects of joint arthroplasty.
Having significant radiographic OA findings in the contralateral knee appears to be associated with improvement by MID criterion. This seems to contradict the previously described relationship between patient-reported symptoms in the contralateral knee with postoperative outcomes. As there seems to be a very weak association between radiographic OA severity and patient-reported outcomes among TKR candidates with OA [40, 41], this is not a surprising result. K-L grade severity, in particular, does not have a close association with either WOMAC function or International Knee Society score [40, 41]. More research is needed to understand this discrepancy between radiographic findings and HRQL instruments.
Previous exposure to frequent knee bending activities was also associated with MID criterion-based definition of improvement after TKR. The risk of developing knee OA is increased in those with physically demanding occupations [42, 43]. This increased risk has been attributed to prolonged exposure to occupational tasks, such as frequent knee-bending. Moreover, frequent knee bending activities have been associated with increased progression of cartilage and meniscal abnormalities [44]. These studies suggest that repetitive biomechanical loading at the knee have a detrimental effect on cartilage, leading to the development or worsening of OA. Consistent with what we have observed so far, those with worse OA are more likely to experience greater relative gains from TKR than those with minimal OA.
Recently, the use of a standard set of criteria to judge appropriateness for TKR has been proposed [13, 16]. The appropriateness criteria use by Escobar et al [16] categorizes surgeries as appropriate, inappropriate or inconclusive. Categorization is based on patient age, radiologic findings, joint mobility/stability and severity of OA-related symptoms. Surgeries classified as appropriate or inconclusive have been linked with significant improvement in pain and symptoms over two years following surgery [45]. While valuable, the criteria does not account for other factors that may also influence long term TKR outcomes. As our study demonstrates, preoperative increase in knee stiffness, absence of chronic OA symptoms in other joints and previous exposure to knee-bending activities may also determine improvement following TKR.
Our study also has some limitations. There are other potential determinants of improvement following TKR that were not assessed. This includes patient expectations of TKR surgery that has been shown to affect functional outcomes [7]. Post-operative complications and processes, such as type and duration of rehabilitation regimen, may also affect improvement from T0 to T2. Extent of preoperative focal knee abnormalities that may only be detected by magnetic resonance imaging may also determine improvement. Future studies should investigate the extent in which these other variables may contribute to improving TKR outcomes. Our study also has missing data that can bias the results. Not all patients had x-rays of both knees at T0, for example. Nevertheless, evidence of association between OA-related HRQL measures and TKR outcomes [8–10, 12, 14, 15, 36, 37, 46] seems to be more robust than evidence of relationship between radiographic findings and TKR outcomes [36, 47]. As all patients included in the study were recruited from American institutions, the generalizability of our findings to other countries may also be limited. The racial makeup of OAI participants is relatively diverse in comparison to other OA cohorts, however.
CONCLUSIONS
The present study identifies factors that portend a better outcome following TKR. Improved patients had more self-reported pain and disability prior to surgery and were more likely to have escalation of these symptoms than unimproved patients. Worse OA-related disability prior to surgery, presence of chronic OA symptoms in the surgical knee, absence of chronic OA symptoms in the contralateral knee, prior exposure to frequent knee bending, and having marked radiographic features of OA in the contralateral knee are most likely to increase the likelihood of achieving improvement. Less OA-related pain and absence of chronic OA symptoms in the hip on the same side are most likely to increase the likelihood of being in an acceptable symptom state. Providers may want to discuss these factors with potential TKR candidates to help decide whether they may or may not be good candidates for TKR and the amount of pain and functional improvement that may result from undergoing TKR.
Supplementary Material
Acknowledgments
We would like to thank Erin Ashbeck for performing some of the statistical analyses presented in this paper.
This manuscript has received the approval of the OAI Publications Committee based on a review of its scientific content and data interpretation.
References
- 1.Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, Deyo RA, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58:26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Michaud CM, McKenna MT, Begg S, Tomijima N, Majmudar M, Bulzacchelli MT, et al. The burden of disease and injury in the United States 1996. Popul Health Metr. 2006;4:11. doi: 10.1186/1478-7954-4-11. 1478-7954-4-11 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang W, Nuki G, Moskowitz RW, Abramson S, Altman RD, Arden NK, et al. OARSI recommendations for the management of hip and knee osteoarthritis: part III: Changes in evidence following systematic cumulative update of research published through January 2009. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society. 2010;18:476–99. doi: 10.1016/j.joca.2010.01.013. [DOI] [PubMed] [Google Scholar]
- 4.Losina E, Thornhill TS, Rome BN, Wright J, Katz JN. The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. The Journal of bone and joint surgery American volume. 2012;94:201–7. doi: 10.2106/JBJS.J.01958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fortin PR, Clarke AE, Joseph L, Liang MH, Tanzer M, Ferland D, et al. Outcomes of total hip and knee replacement: preoperative functional status predicts outcomes at six months after surgery. Arthritis and rheumatism. 1999;42:1722–8. doi: 10.1002/1529-0131(199908)42:8<1722::AID-ANR22>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 6.Fortin PR, Penrod JR, Clarke AE, St-Pierre Y, Joseph L, Belisle P, et al. Timing of total joint replacement affects clinical outcomes among patients with osteoarthritis of the hip or knee. Arthritis and rheumatism. 2002;46:3327–30. doi: 10.1002/art.10631. [DOI] [PubMed] [Google Scholar]
- 7.Mahomed NN, Liang MH, Cook EF, Daltroy LH, Fortin PR, Fossel AH, et al. The importance of patient expectations in predicting functional outcomes after total joint arthroplasty. The Journal of rheumatology. 2002;29:1273–9. [PubMed] [Google Scholar]
- 8.Hawker GA, Badley EM, Borkhoff CM, Croxford R, Davis AM, Dunn S, et al. Which patients are most likely to benefit from total joint arthroplasty? Arthritis and rheumatism. 2013;65:1243–52. doi: 10.1002/art.37901. [DOI] [PubMed] [Google Scholar]
- 9.Riddle DL, Perera RA, Stratford PW, Jiranek WA, Dumenci L. Progressing toward, and recovering from, knee replacement surgery: a five-year cohort study. Arthritis and rheumatism. 2013;65:3304–13. doi: 10.1002/art.38139. [DOI] [PubMed] [Google Scholar]
- 10.Lingard EA, Katz JN, Wright EA, Sledge CB. Predicting the outcome of total knee arthroplasty. The Journal of bone and joint surgery American volume. 2004;86-A:2179–86. doi: 10.2106/00004623-200410000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Nilsdotter AK, Toksvig-Larsen S, Roos EM. A 5 year prospective study of patient-relevant outcomes after total knee replacement. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society. 2009;17:601–6. doi: 10.1016/j.joca.2008.11.007. [DOI] [PubMed] [Google Scholar]
- 12.Kennedy DM, Hanna SE, Stratford PW, Wessel J, Gollish JD. Preoperative function and gender predict pattern of functional recovery after hip and knee arthroplasty. J Arthroplasty. 2006;21:559–66. doi: 10.1016/j.arth.2005.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Riddle DL, Jiranek WA, Hayes CW. Use of a validated algorithm to judge the appropriateness of total knee arthroplasty in the United States: a multicenter longitudinal cohort study. Arthritis Rheumatol. 2014;66:2134–43. doi: 10.1002/art.38685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ethgen O, Bruyere O, Richy F, Dardennes C, Reginster JY. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. The Journal of bone and joint surgery American volume. 2004;86-A:963–74. doi: 10.2106/00004623-200405000-00012. [DOI] [PubMed] [Google Scholar]
- 15.Guyatt GH, Feeny DH, Patrick DL. Measuring health-related quality of life. Ann Intern Med. 1993;118:622–9. doi: 10.7326/0003-4819-118-8-199304150-00009. [DOI] [PubMed] [Google Scholar]
- 16.Escobar A, Quintana JM, Arostegui I, Azkarate J, Guenaga JI, Arenaza JC, et al. Development of explicit criteria for total knee replacement. International journal of technology assessment in health care. 2003;19:57–70. doi: 10.1017/s0266462303000060. [DOI] [PubMed] [Google Scholar]
- 17.Wyrwich KW, Nienaber NA, Tierney WM, Wolinsky FD. Linking clinical relevance and statistical significance in evaluating intra-individual changes in health-related quality of life. Med Care. 1999;37:469–78. doi: 10.1097/00005650-199905000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Pham T, van der Heijde D, Altman RD, Anderson JJ, Bellamy N, Hochberg M, et al. OMERACT-OARSI initiative: Osteoarthritis Research Society International set of responder criteria for osteoarthritis clinical trials revisited. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society. 2004;12:389–99. doi: 10.1016/j.joca.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 19.Tubach F, Dougados M, Falissard B, Baron G, Logeart I, Ravaud P. Feeling good rather than feeling better matters more to patients. Arthritis and rheumatism. 2006;55:526–30. doi: 10.1002/art.22110. [DOI] [PubMed] [Google Scholar]
- 20.Losina E, Katz JN. Total knee replacement: pursuit of the paramount result. Rheumatology. 2012;51:1735–6. doi: 10.1093/rheumatology/kes199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Losina E, Katz JN. Total joint replacement outcomes in patients with concomitant comorbidities: a glass half empty or half full? Arthritis and rheumatism. 2013;65:1157–9. doi: 10.1002/art.37903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Collins JE, Katz JN, Dervan EE, Losina E. Trajectories and risk profiles of pain in persons with radiographic, symptomatic knee osteoarthritis: data from the osteoarthritis initiative. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society. 2014;22:622–30. doi: 10.1016/j.joca.2014.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Niu J, Nevitt M, McCulloch C, Torner J, Lewis CE, Katz JN, et al. Comparing the functional impact of knee replacements in two cohorts. BMC Musculoskelet Disord. 2014;15:145. doi: 10.1186/1471-2474-15-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 25.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Applied psychological measurement. 1977;1:385–401. [Google Scholar]
- 26.Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Med Care. 1996;34:73–84. doi: 10.1097/00005650-199601000-00006. [DOI] [PubMed] [Google Scholar]
- 27.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. The Journal of rheumatology. 1988;15:1833–40. [PubMed] [Google Scholar]
- 28.Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)--development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28:88–96. doi: 10.2519/jospt.1998.28.2.88. [DOI] [PubMed] [Google Scholar]
- 29.Altman R, Brandt K, Hochberg M, Moskowitz R, Bellamy N, Bloch DA, et al. Design and conduct of clinical trials in patients with osteoarthritis: recommendations from a task force of the Osteoarthritis Research Society. Results from a workshop. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society. 1996;4:217–43. doi: 10.1016/s1063-4584(05)80101-3. [DOI] [PubMed] [Google Scholar]
- 30.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Annals of the rheumatic diseases. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Davis AM, Perruccio AV, Lohmander LS. Minimally clinically important improvement: all non-responders are not really non-responders an illustration from total knee replacement. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society. 2012;20:364–7. doi: 10.1016/j.joca.2012.02.005. [DOI] [PubMed] [Google Scholar]
- 32.Kvien TK, Heiberg T, Hagen KB. Minimal clinically important improvement/difference (MCII/MCID) and patient acceptable symptom state (PASS): what do these concepts mean? Annals of the rheumatic diseases. 2007;66(Suppl 3):iii40–1. doi: 10.1136/ard.2007.079798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Judge A, Arden NK, Kiran A, Price A, Javaid MK, Beard D, et al. Interpretation of patient-reported outcomes for hip and knee replacement surgery: identification of thresholds associated with satisfaction with surgery. J Bone Joint Surg Br. 2012;94:412–8. doi: 10.1302/0301-620X.94B3.27425. [DOI] [PubMed] [Google Scholar]
- 34.Escobar A, Gonzalez M, Quintana JM, Vrotsou K, Bilbao A, Herrera-Espineira C, et al. Patient acceptable symptom state and OMERACT-OARSI set of responder criteria in joint replacement. Identification of cut-off values. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society. 2012;20:87–92. doi: 10.1016/j.joca.2011.11.007. [DOI] [PubMed] [Google Scholar]
- 35.Nguyen US, Zhang Y, Zhu Y, Niu J, Zhang B, Felson DT. Increasing prevalence of knee pain and symptomatic knee osteoarthritis: survey and cohort data. Ann Intern Med. 2011;155:725–32. doi: 10.7326/0003-4819-155-11-201112060-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kahn TL, Soheili A, Schwarzkopf R. Outcomes of total knee arthroplasty in relation to preoperative patient-reported and radiographic measures: data from the osteoarthritis initiative. Geriatr Orthop Surg Rehabil. 2013;4:117–26. doi: 10.1177/2151458514520634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Perruccio AV, Power JD, Evans HM, Mahomed SR, Gandhi R, Mahomed NN, et al. Multiple joint involvement in total knee replacement for osteoarthritis: Effects on patient-reported outcomes. Arthritis care & research. 2012;64:838–46. doi: 10.1002/acr.21629. [DOI] [PubMed] [Google Scholar]
- 38.Nilsdotter AK, Petersson IF, Roos EM, Lohmander LS. Predictors of patient relevant outcome after total hip replacement for osteoarthritis: a prospective study. Annals of the rheumatic diseases. 2003;62:923–30. doi: 10.1136/ard.62.10.923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Quintana JM, Escobar A, Aguirre U, Lafuente I, Arenaza JC. Predictors of health-related quality-of-life change after total hip arthroplasty. Clin Orthop Relat Res. 2009;467:2886–94. doi: 10.1007/s11999-009-0868-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dowsey MM, Dieppe P, Lohmander S, Castle D, Liew D, Choong PF. The association between radiographic severity and pre-operative function in patients undergoing primary knee replacement for osteoarthritis. Knee. 2012;19:860–5. doi: 10.1016/j.knee.2012.02.007. [DOI] [PubMed] [Google Scholar]
- 41.Barker K, Lamb SE, Toye F, Jackson S, Barrington S. Association between radiographic joint space narrowing, function, pain and muscle power in severe osteoarthritis of the knee. Clin Rehabil. 2004;18:793–800. doi: 10.1191/0269215504cr754oa. [DOI] [PubMed] [Google Scholar]
- 42.Anderson JJ, Felson DT. Factors associated with osteoarthritis of the knee in the first national Health and Nutrition Examination Survey (HANES I). Evidence for an association with overweight, race, and physical demands of work. Am J Epidemiol. 1988;128:179–89. doi: 10.1093/oxfordjournals.aje.a114939. [DOI] [PubMed] [Google Scholar]
- 43.Felson DT, Hannan MT, Naimark A, Berkeley J, Gordon G, Wilson PW, et al. Occupational physical demands, knee bending, and knee osteoarthritis: results from the Framingham Study. The Journal of rheumatology. 1991;18:1587–92. [PubMed] [Google Scholar]
- 44.Virayavanich W, Alizai H, Baum T, Nardo L, Nevitt MC, Lynch JA, et al. Association of frequent knee bending activity with focal knee lesions detected with 3T magnetic resonance imaging: data from the osteoarthritis initiative. Arthritis care & research. 2013;65:1441–8. doi: 10.1002/acr.22017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Riddle DL, Perera RA, Jiranek WA, Dumenci L. Using surgical appropriateness criteria to examine outcomes of total knee arthroplasty in a United States sample. Arthritis care & research. 2015;67:349–57. doi: 10.1002/acr.22428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sharma L, Sinacore J, Daugherty C, Kuesis DT, Stulberg SD, Lewis M, et al. Prognostic factors for functional outcome of total knee replacement: a prospective study. J Gerontol A Biol Sci Med Sci. 1996;51:M152–7. doi: 10.1093/gerona/51a.4.m152. [DOI] [PubMed] [Google Scholar]
- 47.Lundblad H, Kreicbergs A, Soderlund V, Ulfgren AK, Stiller CO, Jansson KA. The value of preoperative grade of radiographic and histological changes in predicting pain relief after total knee arthroplasty for osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2012;20:1815–21. doi: 10.1007/s00167-011-1821-5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.