Abstract
Introduction
Although infrequently recorded in electronic health records (EHR), measures of SES are essential to describe health inequalities and account for confounding in epidemiologic research. Medical Assistance (i.e., Medicaid) is often used as a surrogate for SES, but correspondence between conventional SES and Medical Assistance has been insufficiently studied.
Methods
Geisinger Clinic EHR data from 2001 to 2014 and a 2014 questionnaire were used to create six SES measures: EHR-derived Medical Assistance and proportion of time under observation on Medical Assistance; educational attainment, income, and marital status; and area-level poverty. Analyzed in 2016–2017, associations of SES measures with obesity, hypertension, type 2 diabetes, chronic rhinosinusitus, fatigue, and migraine headache were assessed using weighted age- and sex-adjusted logistic regression.
Results
Among 5,550 participants (interquartile range, 39.6–57.5 years, 65.9% female), 83% never used Medical Assistance. All SES measures were correlated (Spearman’s p≤0.4). MA was significantly associated with all six health outcomes in adjusted models. For example, the OR for prevalent type 2 diabetes associated with Medical Assistance was 1.7 (95% CI=1.3, 2.2); the OR for high school versus college graduates was 1.7 (95% CI=1.2, 2.5). Medical Assistance was an imperfect proxy for SES: associations between conventional SES measures and health were attenuated <20% after adjustment for Medical Assistance.
Conclusions
Because systematically collected SES measures are rarely available in EHRs and are unlikely to appear soon, researchers can use EHR-based Medical Assistance to describe inequalities. As SES has many domains, researchers who use Medical Assistance to evaluate the association of SES with health should expect substantial unmeasured confounding.
INTRODUCTION
SES is associated with virtually every disease endpoint as well as many risk factors, such health-related behaviors and healthcare utilization and treatment.1–3 In epidemiologic research, accurate measures of SES are essential to describe and monitor health inequalities and to account for confounding when evaluating risk factors.2,4 Recently, a confluence of forces—technological advances, financial incentives to healthcare providers, and tightening research funding—has led to increased use of electronic health records (EHRs) for epidemiologic research.5 Because healthcare systems originally adopted EHRs for administrative purposes and to improve patient care, they do not employ systematic SES data collection.6,7
On the other hand, needs-based insurance status, because of its direct link to patient billing, is robustly and accurately recorded.8 As of 2014, Medicaid (in Pennsylvania, referred to as Medical Assistance [MA]) enrollees totaled more than 66 million Americans.9 Because MA eligibility is based on state and federal guidelines regarding poverty,10 researchers in the U.S. have considered MA an indicator of low SES (Appendix Table 1 describes common SES indicators).11–16 In Europe, Canada, and other countries with universal health care, the application of area-level social deprivation17,18 as a surrogate for individual SES is common.19–22 U.S. researchers have also used area-level measures of SES.23–25 A large literature documents independent associations between several individual and area-level SES measures and health, suggesting that SES is multidimensional.2,26,27
SES broadly refers to myriad correlated social and economic factors—education, income, occupation, and household assets or wealth (Appendix Figure 1)—that measure social standing27,28 and influence standard of living, social interactions, workplace conditions, environmental exposures, access to health care, and health status.2,3 Because of the pervasive relationship between SES and health, researchers have long understood the importance of controlling for SES in epidemiologic studies.4 Traditional measures of SES have had little perceived relevance to healthcare provision in the U.S., and thus generally are not recorded in EHR data.
Infrequent documentation of conventional SES measures and possible residual confounding by SES has emerged as a limitation of EHR-based research.29,30 In response, researchers have used MA as a surrogate, but correspondence between conventional SES measures and MA has been insufficiently studied.31–33 Such an understanding is essential to guide the use of MA in EHR-based research.
This study uses a novel dataset that included EHR-derived MA and self-reported measures of SES (i.e., income, educational attainment, and marital status) from Geisinger Clinic primary care patients in Pennsylvania. It aims to describe the relationship between MA and conventional SES and to determine the extent to which they can serve as proxies for one another.
METHODS
Study Population
The study population was drawn from the Chronic Rhinosinusitis Integrative Studies Program (CRISP) at the Geisinger Clinic.34 Geisinger Clinic, an integrated health system, provides comprehensive care from 48 outpatient clinics and eight hospitals to more than 500,000 primary care patients in Pennsylvania, who are representative of the general population of the region.13 As an open healthcare system, Geisinger serves patients with a variety of health plans, including MA. The study population included participants aged 18 to <65 years who lived in Pennsylvania.
The CRISP questionnaire was mailed to a random sample, stratified by race/ethnicity and probability of chronic rhinosinusitis diagnosis, of Geisinger primary care patients in April 2014.34 The dataset consisted of these questionnaire responses and patient EHRs from January 1, 2001 to December 31, 2014. The analysis was cross-sectional because self-reported measures from the CRISP questionnaire were collected only once. The study was reviewed and approved by the Geisinger Health System IRB.
Measures
Within the EHR, each outpatient encounter had an associated payor (e.g., MA, Blue Cross Blue Shield). An algorithm was implemented to create a binary indicator that designated participants as users versus not users of MA, beginning with each participant’s first healthcare encounter (as early as 2001) until return of the mailed survey in 2014: use at three or more encounters if patient had greater than three encounters; use at two or more encounters if patient had three encounters; use at one or more encounter if patient had two encounters; or use at one encounter if patient had one encounter. The proportion of time spent on MA (proportion MA) was calculated using payor type at each outpatient encounter (code available in Appendix). Proportion MA was skewed to the right, so categories were used in regression analyses (i.e., 0, 0.1 to 33.3%, 33.4% to 66.7%, 66.8 to 99.9%, 100%).
The study included three self-reported SES measures. The questionnaire asked about educational attainment: What is the highest grade or highest degree you have completed? Response options: no schooling, a few years, finished grammar school, some high school, high school graduate, general equivalency diploma (GED), some college, associate degree, bachelor’s degree, master’s degree, or doctoral degree. It also asked participants to report their income: About how much income did you receive last year? Response options were: $0–$9,999, $10,000–$24,999, $25,000–$49,000, $50,000–$74,999, $75,000–$99,999, $100,000–$149,999, or ≥$150,000. Although not a direct measure of SES, marital status likely correlates with financial insecurity and financial vulnerability, particularly in older women.35,36 Therefore, participants’ marital status (married, separated, divorced, widowed, never married, living with partner) was ascertained from responses to the question: what is your current marital status?
Based on previously reported socioeconomic disparities, the study included six health outcomes a priori. BMI was calculated using height and weight in the EHR for the visit closest to the date of questionnaire return and categorized BMI as obese (≥30 kg/m2) or not (<30 kg/m2). Hypertension was defined as two or more abnormal blood pressure readings (≥140 mmHg systolic/90 mmHg diastolic) or two or more diagnoses for hypertension (ICD-9 code 401.0–401.9) from encounters, problem list, or medications. Similarly, type 2 diabetes (T2DM) was identified with ICD-9 codes 250.x0 or 250.x2. Using questionnaire data, patients with chronic rhinosinusitus symptoms in the past 3 months, migraine headache symptoms in the past year, and fatigue symptoms in the past week were identified using validated questions as previously described.37
Pennsylvania neighborhoods were conceptualized as townships, boroughs, and census tracts in cities38 because they have distinct political and cultural characteristics. American Community Survey data from 2008 to 2012 was used to estimate the percent of families living in poverty within each neighborhood.38–40
Statistical Analysis
Analysis was conducted during 2016–2017 with the goal to summarize six measures of SES, evaluate correlations among them, and to compare their associations with six health outcomes. In particular, analysis sought to evaluate the extent to which conventional measures of SES remained associated with six health outcomes, after controlling for MA. Spearman’s rank correlation coefficients, sensitivity, specificity, and kappa coefficients were calculated to compare bivariate associations.
Associations among educational attainment (<high school, high school graduate or GED, some college/Associate’s degree, college graduate [reference], >college graduate), income ($0–$9,999, $10,000–$24,999, $25,000–$49,999, $50,000–$74,999 [reference], $75,000–$99,999, ≥$100,000), marital status (in aforementioned categories), area-level poverty (quartiles), and MA were evaluated using weighted, age- and sex-adjusted logistic regression models. Associations between MA and conventional SES measures and the six health outcomes were also examined. Base models were adjusted for age and sex. Next, to assess the residual association of MA and all other SES variables with each health outcome two other models were run, the first controlling for MA alone (MA-adjusted) and the second all other SES variables in the same model (fully adjusted). To account for stratified sampling and differential participation in CRISP, weights (inverse probability of inclusion in study, range, 2.8–32.3)37 and robust SEs were used. Missing self-reported SES was included with a missing indicator.
The patterns of missingness of self-reported SES were explored. Because sicker individuals may have sought out or had expanded eligibility for MA, relationships between Charlson Index41 and MA were evaluated. In another sensitivity analysis, final models were adjusted for race/ethnicity. Analyses were conducted using Stata, version 13 and R, version 3.3.2.
RESULTS
The study included 5,550 primarily non-Hispanic white participants (88.8%). Between 2001 and 2014, 17.0% of participants (n=944) used MA (Table 1). These individuals were younger and more likely to be women and racial/ethnic minorities than non-MA participants (Table 1). Non-MA participants had fewer outpatient clinic visits than MA participants (Appendix Figure 2A, Table 1). MA participants had a median of 56 outpatient encounters, but MA was the payor type at less than half of these visits (median 23 visits, interquartile range, 11–14) (Appendix Figure 2B).
Table 1.
Demographic Characteristics of Study Subjects by Receipt of Medical Assistance
| Characteristic | Used MA | |
|---|---|---|
| Demographics | Yes | No |
| N=944 (17.0) | N=4,606 (83.0) | |
| Male, N (%) | 230 (24.4) | 714 (75.6) |
| Female, N (%) | 714 (75.6) | 2943 (63.9) |
| Age, years, median (IQR) | 42.6 (30.8, 52.5) | 51.5 (41.8, 58.1) |
| Race/ethnicity, N (%) | ||
| Black | 115 (12.2) | 170 (3.7) |
| Hispanic | 104 (11.0) | 198 (4.3) |
| White | 719 (76.2) | 4,210 (91.4) |
| Other | 6 (0.6) | 22 (0.5) |
| Missing | 0 | 6 (0.1) |
| Number of outpatient encounters prior to survey, median (IQR) | 56 (33, 90) | 41 (23, 68) |
| Proportion of time on MA during follow-up, median (IQR) | 0.47 (0.22, 0.77) | 0 (0, 0) |
| Education, N (%) | ||
| Less than high school | 100 (10.6) | 117 (2.5) |
| High school graduate or GED | 399 (42.3) | 1,374 (29.8) |
| Some college/Associate’s degree | 328 (34.8) | 1,494 (32.4) |
| College graduate | 83 (8.8) | 912 (19.8) |
| More than college graduate | 21 (2.2) | 652 (14.2) |
| Missing | 13 (1.4) | 57 (1.2) |
| Income, N (%) | ||
| $0–$9,999 | 366 (38.8) | 408 (8.9) |
| $10,000–$24,999 | 312 (33.1) | 673 (14.6) |
| $25,000–$49,999 | 133 (14.1) | 1,377 (29.9) |
| $50,000–$74,999 | 47 (5.0) | 947 (20.6) |
| $75,000–$99,999 | 11 (1.2) | 403 (8.8) |
| ≥$100,000 | 10 (1.1) | 390 (8.5) |
| Missing | 65 (6.9) | 408 (8.9) |
| Marital status, N (%) | ||
| Married/living with partner | 392 (41.5) | 3,422 (74.3) |
| Never married | 268 (28.4) | 528 (11.5) |
| Divorced/separated | 240 (25.4) | 511 (11.1) |
| Widowed | 31 (3.3) | 106 (2.3) |
| Missing | 13 (1.4) | 39 (0.9) |
| Health outcomes | ||
| BMIa (kg/m2), median (IQR) | 30.3 (24.9, 36.3) | 29.2 (25.2, 34.4) |
| Hypertension,b N (%) | ||
| Yes | 449 (47.6) | 2,175 (47.2) |
| No | 495 (52.4) | 2,431 (52.8) |
| Type 2 diabetes, N (%) | ||
| Yes | 143 (15.2) | 524 (11.4) |
| No | 801 (84.9) | 4,082 (88.6) |
| CRS symptoms at baseline, N (%) | ||
| Yes | 318 (33.7) | 1,147 (24.9) |
| No | 626 (66.3) | 3,459 (75.1) |
| Migraine headache,c N (%) | ||
| Yes | 460 (48.7) | 1,151 (25.0) |
| No | 484 (51.3) | 3,455 (75.0) |
| Fatigue, severe symptoms,c N (%) | ||
| Yes | 417 (44.2) | 1,135 (24.6) |
| No | 527 (55.8) | 3,471 (75.4) |
| Charlson Index, median (IQR) | 2 (1, 3) | 2 (1, 3) |
| Area-level variablesd | ||
| Poverty (%) | ||
| Quartile 1 (<7.2%) | 143 (15.2) | 1,250 (27.1) |
| Quartile 2 (7.2 to <10.5%) | 182 (19.3) | 1,204 (26.1) |
| Quartile 3 (10.5 to <15.9%) | 260 (27.5) | 1,126 (24.5) |
| Quartile 4 (≥15.9%) | 359 (38.0) | 1,026 (22.3) |
BMI from the healthcare visit closest to the survey return date (mean=123 days).
Hypertension defined as ever a diagnosis of hypertension from ICD-9 codes or ≥2 visits with systolic blood pressure >140mmHg or diastolic blood pressure >90mmHg.
Migraine and fatigue reported in the 12 months prior to survey date.
Communities were defined with a mixed definition of place: minor civil division townships and boroughs and census tracts in cities using 2010 U.S. Census boundaries.
GED, general equivalency diploma; IQR, interquartile range; MA, Medical Assistance
Among MA users, an increased proportion of time on MA was associated with less education and lower income (Appendix Figure 3). There were only moderate correlations and relatively low sensitivity, specificity, and kappa coefficients among the self-reported SES variables and MA (Table 2, Appendix Table 2). The strongest correlations were between MA and annual income (p= −0.39) and annual income and educational attainment (p=0.40). Nearly 32.0% of divorced/separated participants had a history of MA, compared with 10.3% of married/cohabitating participants (Table 1).
Table 2.
Spearman Correlation Coefficients Between Medical Assistance, Income, Education, and Marital Status
| Variables | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| 1. MAa | 1 | |||||
| 2. Proportion MAa | 0.93 | 1 | ||||
| 3. Incomeb | −0.39 | −0.42 | 1 | |||
| 4. Educational levelc | −0.22 | −0.24 | 0.40 | 1 | ||
| 5. Marital statusd | 0.25 | 0.27 | −0.29 | −0.10 | 1 | |
| 6. Area-level povertye | 0.17 | 0.17 | −0.15 | −0.05 | 0.11 | 1 |
MA, a binary indicator of MA; proportion MA, the amount of time under observation spent using MA; both MA and proportion MA are defined in text.
Annual income before taxes and deductions ($0–$9,999; $10,000–$24,999; $25,000–$49,999; $50,000–$74,999; $75,000–$99,999; ≥$100,000).
Completed levels of education (<9 years to some high school; high school graduate/General Equivalency Diploma; some college or Associate’s degree; college graduate; >college graduate).
Marital status included four categories (married or living with partner; never married; divorced/separated; widowed).
Assigned at the township, borough, or census tract level based on 2008–2012 American Community Survey data; quartile 4 ≥15.9% residents living below poverty line.
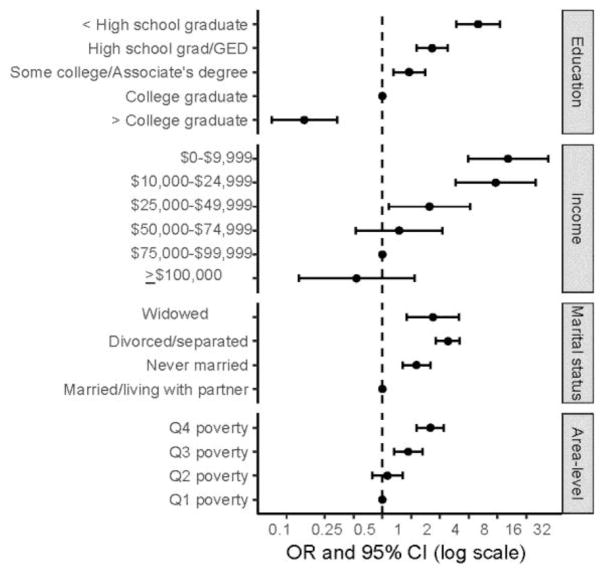
In age and sex-adjusted models, lower annual income and educational attainment were associated with higher odds of MA (Figure 1). For example, participants with less than a high school diploma had 10.0 times the odds (95% CI=5.9, 17.1) of using MA (versus college graduates). The 3,814 participants who were married/cohabitating had the lowest odds of MA; 751 divorced/separated participants had the highest odds (OR=4.2, 95% CI=3.2–5.6).
Figure 1.
ORs of MA by self-reported and area-level SES measures.
Notes: ORs and 95% CIs from weighted, age- and sex-adjusted logistic regression models with robust SEs.
GED, general equivalency diploma; MA, Medical Assistance
Study participants resided in 647 rural and suburban townships, small town boroughs, and urban census tracts (Appendix Figure 4). MA participants lived in neighborhoods with higher proportions of poverty, 38.0% of MA participants versus 22.3% of non-MA participants lived in communities in the highest quartile of poverty (Table 1). Correlations between area-level poverty and MA were not as strong as those with other individual SES measures (Table 2). Compared with the first, the fourth quartile of poverty was associated with increased odds of MA (OR=3.2, 95% CI=2.3, 4.4; Figure 1).
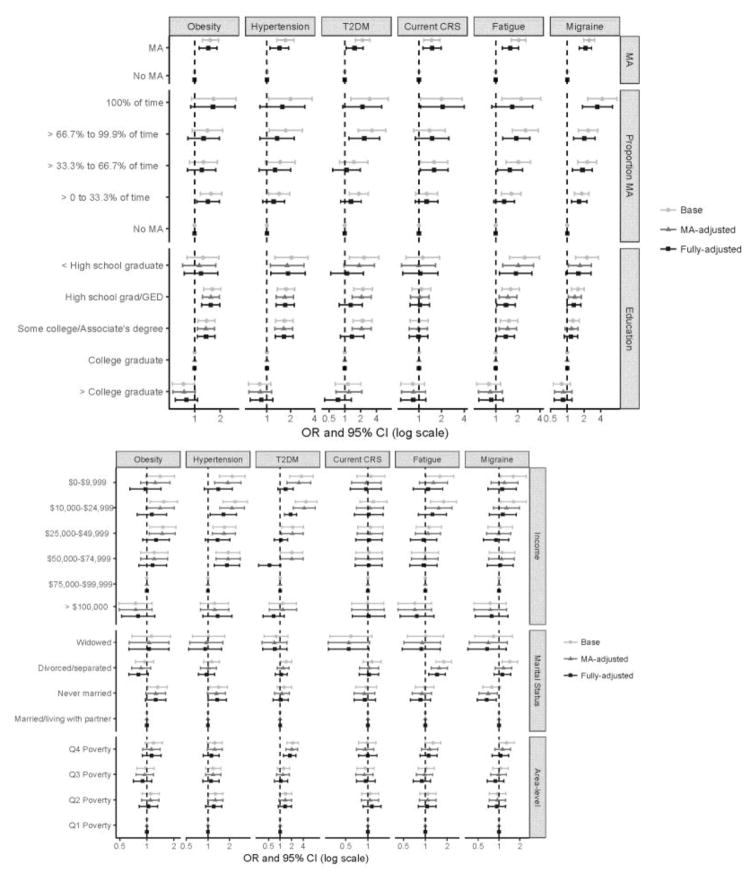
MA was associated with all six health outcomes in base and fully adjusted models (Figure 2A). As proportion MA increased, associations with adverse health outcomes generally strengthened. Conventional SES and MA were similarly associated with health outcomes. For example, in base models, the odds of hypertension were 1.7 (95% CI=1.3, 2.2) for MA versus non-MA participants, 1.7 (95% CI=1.4, 2.3) for high school versus college graduates, 1.7 (95% CI=1.2, 2.5) for those making $25,000–$49,999 compared with $75,000–$99,999 annually, and 1.4 (95% CI=1.1, 1.9) for never married versus married participants. In fully adjusted models, MA accounted for only a portion of the association between conventional SES measures and health, on average associations with health were attenuated by ≅20% with the addition of MA (Figure 2A and 2B). Area-level poverty was generally not associated with health, except for the fourth quartile of poverty and T2DM (Figure 2B). A higher Charlson score was associated with MA (for Charlson score ≥3 vs 0, OR=8.3, 95% CI=5.0, 13.6). In a second sensitivity analysis, adjustment for race/ethnicity did not substantively change inference.
Figure 2.
ORs of six health outcomes by individual and area-level SES measures.
Notes: ORs and 95% CIs from three weighted logistic regression models with robust SEs: base model, adjusted for age and sex; MA-adjusted model, adjusted age, sex, and MA; and fully-adjusted model, adjusted for age, sex, MA, educational attainment, income, marital status, and area-level poverty. (A) MA, proportion of time under observation on MA, and educational attainment; (B) income, marital status, and area-level poverty quartile.
CRS, chronic rhinosinusitus; GED, general equivalency diploma; MA, Medical Assistance; T2DM, type 2 diabetes
Regarding missing data, 0%, 0.9%, 1.3%, and 8.5% were missing MA, marital status, educational attainment, and income, respectively. No significant differences between participants who reported versus did not report educational attainment were identified. Black and Hispanic participants were slightly less likely to report marital status. By contrast, participants who did not report income (versus reporters) were, on average, older (median age 54 years vs 50 years), less likely to use MA (13.7% vs 17.3%), and healthier (lower prevalence of obesity, chronic rhinosinusitus, fatigue, and migraine).
DISCUSSION
Geisinger Clinic EHR data from 2001 to 2014 and a 2014 questionnaire were used to assess the correspondence between conventional measures of SES and Medical Assistance and their associations with obesity, hypertension, type 2 diabetes, chronic rhinosinusitus, fatigue, and migraine headache. The six measures of SES, two from EHR data, three from self-reported questionnaire, and one area-level from Census data evidenced differential associations among themselves and differential associations, as well as patterns of confounding, with six common and important health outcomes. The study found strong associations of MA with conventional SES measures—education, income, marital status, and area-level poverty—and among MA recipients, the proportion of time spent on MA exhibited an SES gradient. Health inequalities by MA mirrored those identified using conventional SES measures. MA was associated with all six health outcomes in models adjusted for conventional SES, but MA accounted for only a portion of the association between conventional SES and health.
The results presented in this paper should be understood in the context of the bidirectional relationships between EHR-based MA, SES, and health. In Pennsylvania, individuals enrolled in the Supplemental Security Income Program because of disability are automatically enrolled for MA. Poor health may result in: job loss or diagnosis of disability and subsequent MA enrollment32; increased impetus to access MA; or conversely, reduced capacity to enroll in MA.42 These circumstances may create associations between MA and health unrelated to SES.43,44 In addition, a healthcare encounter is required to measure MA. Increased diagnoses of T2DM and high cholesterol in states that expanded MA under the Affordable Care Act may indicate sicker MA populations or additional clinical testing among MA participants.45 Prior studies have also found MA more strongly associated with chronic health conditions like hypertension than conventional individual-level46,47 or area-level SES.48–50
Ideally, the use of MA to account for confounding by SES should eliminate other SES–health associations. In this analysis, estimated associations between conventional SES and health were reduced by 20%, on average, with the addition of MA suggesting that MA does not account for the majority of confounding by conventional SES. A single indicator of SES, whether MA, income, or education, likely fails to capture the range and multiple domains of SES (Appendix Figure 1). MA was an imperfect proxy for conventional SES. The substantial health inequalities by MA that mirror other social inequalities in health suggest, however, that MA may be useful to monitor the magnitude of health disparities.15,34,47,51–53
Widowed, divorced, and separated participants, those living in poorer communities, and those with lower incomes and less education tended to enroll in MA at higher rates.31–33,52,54 Each SES measure likely captures a discrete facet of SES with differing advantages and disadvantages and relevance across the life course.55 In a prior study, household income, but not insurance type, was significantly associated with obesity and overweight in children; in adolescents, the opposite was true.56 Among older adults who live on assets, income alone may not fully characterize needs and resources.57 To measure income, assets, and wealth adequately, however, requires time and considerable effort from both researchers and participants. Another large body of research suggests that area-level SES is associated with individual-level health above and beyond individual-level SES58; a finding only observed only for T2DM in the present study.
As with other indicators of SES, what MA measures may differ by group and place. Pregnant women, parents of children younger than 18 years, and children qualify for MA at different income thresholds than other individuals.10 MA may increasingly measure disability, as Americans age. The meaning of MA will also continue to evolve over time. Between 2013 and 2015, when the Affordable Care Act went into effect and some states expanded MA to individuals with income 138% of the poverty limit, the percent of uninsured nonelderly Americans dropped from 16.6% to 10.5%, nearly a 20% reduction. Low income Americans saw even greater changes.32,45,59
Limitations
Despite being one of the first to describe relationships among EHR-based MA, SES, and health, this study has several limitations. Data came from a single state with limited racial/ethnic diversity and may not represent broader trends. Self-reported SES was measured at one time point on 5,500 individuals, this sample size resulted in uncertainty in effect estimates. EHR-based MA appeared related to both individual and community-level SES, but limited results related to area-level factors were presented. Future work should assess associations between MA, community socioeconomic deprivation, features of the built environment, and racial and economic segregation.26,38,60
Clinically, EHRs were adopted for administrative purposes and to improve patient care through enhanced access to patient histories, cost savings, and streamlined care coordination.7 However, with the pivot to financial incentives that reward population-based health management, there has been increased attention to the relevance of SES in clinical care, including a call from the National Academy of Medicine to integrate individual measures of SES into EHRs.29,61 This suite of proposed standardized measures would improve data collection and comparability across health systems. The capture of self-reported SES measures is challenged by the logistics of integrating data collection into clinical care workflows as well as patient reluctance to report personal information, as evidenced by high nonresponse rates to income-related questions (9% of participants in this study) and elsewhere.62
EHR-based measurement of social determinants of health is in its infancy.63,64 Some have argued that clinicians do not have the resources, expertise, or time to collect additional data.65 In light of particularly high burnout rates in primary care disciplines, Shanafelt et al.66 recommended streamlining and reducing documentation. Until social determinants of health data are effectively collected in EHRs, researchers should focus on using available EHR data to measure variables that are critical to research but not necessarily to clinical care. Analysis of text in clinical notes67 may hold promise for measuring social determinants of health.
CONCLUSIONS
Given the critical role SES plays for health, researchers require indicators of SES to evaluate health inequalities and control for confounding. No single measure can capture all domains of SES. MA offers some advantages—no additional clinical data collection, longer-term measure, universal availability in EHRs, and standardized meaning across health systems—as well as disadvantages owing to its correlation with disability, compared with conventional SES measures. Because systematically collected SES measures are rarely available in EHRs and are unlikely to appear soon, researchers can use EHR-based MA to describe inequalities. As SES has many domains, researchers who use MA to evaluate the association of SES with health should expect substantial unmeasured confounding.
Supplementary Material
Acknowledgments
This study was supported in part by grant U19AI106683 (Chronic Rhinosinusitis Integrative Studies Program) from the National Institute of Allergy and Infectious Diseases (Drs. Schwartz and Hirsch). Additional support was provided by the Robert Wood Johnson Foundation Health & Society Scholars program and grant K99ES027023 from the National Institute of Environmental Health Sciences (Dr. Casey) and grant K99AG053410 from the National Institute of Aging grant (Dr. Mayeda).
Drs. Casey and Schwartz had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Author contributions were as follows: Casey, Pollak, and Schwartz helped with the concept and design; acquisition, analysis, or interpretation of data was done by Casey, Pollak, Glymour, Mayeda, Hirsch, and Schwartz; Casey drafted the manuscript; critical revision of the manuscript for important intellectual content was done by Pollak, Glymour, Mayeda, Hirsch, and Schwartz; Casey did statistical analysis; Schwartz obtained funding; administrative, technical, or material support was provided by Pollak and Schwartz; and Glymour and Schwartz supervised the study.
No financial disclosures were reported by the authors of this paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kawachi I, Subramanian SV. Income Inequality. In: Kawachi I, Berkman L, Glymour MM, editors. Social Epidemiology. 2. New York, NY: Oxford University Press; 2014. https://doi.org/10.1093/med/9780195377903.003.0004. [Google Scholar]
- 2.Adler NE, Rehkopf DH. U.S. disparities in health: descriptions, causes, and mechanisms. Annu Rev Public Health. 2008;29:235–252. doi: 10.1146/annurev.publhealth.29.020907.090852. https://doi.org/10.1146/annurev.publhealth.29.020907.090852. [DOI] [PubMed] [Google Scholar]
- 3.Adler NE, Newman K. Socioeconomic disparities in health: pathways and policies. Health Aff (Millwood) 2002;21(2):60–76. doi: 10.1377/hlthaff.21.2.60. https://doi.org/10.1377/hlthaff.21.2.60. [DOI] [PubMed] [Google Scholar]
- 4.Krieger N. Epidemiology and the web of causation: has anyone seen the spider? Soc Sci Med. 1994;39(7):887–903. doi: 10.1016/0277-9536(94)90202-x. https://doi.org/10.1016/0277-9536(94)90202-X. [DOI] [PubMed] [Google Scholar]
- 5.Casey JA, Schwartz BS, Stewart WF, Adler N. Using electronic health records for population health research: a review of methods and applications. Annu Rev Public Health. 2015;37:61–81. doi: 10.1146/annurev-publhealth-032315-021353. https://doi.org/10.1146/annurev-publhealth-032315-021353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Diez Roux AV, Katz M, Crews DC, Ross D, Adler N. Social and behavioral information in electronic health records: New opportunities for medicine and public health. Am J Prev Med. 2015;49(6):980–983. doi: 10.1016/j.amepre.2015.08.027. https://doi.org/10.1016/j.amepre.2015.08.027. [DOI] [PubMed] [Google Scholar]
- 7.U.S. DHHS. [Accessed February 26, 2017];Why Adopt EHRs? www.healthit.gov/providers-professionals/why-adopt-ehrs.
- 8.Heintzman J, Marino M, Hoopes M, et al. Supporting health insurance expansion: do electronic health records have valid insurance verification and enrollment data? J Am Med Inform Assoc. 2015;22(4):909–913. doi: 10.1093/jamia/ocv033. https://doi.org/10.1093/jamia/ocv033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Medicare & Medicaid Services. [Accessed January 18, 2017];Total Medicaid Enrollees - VIII Group Break Out Report. 2014 Mar; www.medicaid.gov/medicaid/program-information/downloads/cms-64-medicaid-enrollment-report.pdf. Published 2016.
- 10.The Henry J. Kaiser Family Foundation. [Accessed March 6, 2017];Where Are States Today? Medicaid and CHIP Eligibility Levels for Children, Pregnant Women, and Adults. http://kff.org/medicaid/fact-sheet/where-are-states-today-medicaid-and-chip/. Published 2017.
- 11.Black MH, Zhou H, Takayanagi M, Jacobsen SJ, Koebnick C. Increased asthma risk and asthma-related health care complications associated with childhood obesity. Am J Epidemiol. 2013;178(7):1120–1128. doi: 10.1093/aje/kwt093. https://doi.org/10.1093/aje/kwt093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schwartz BS, Bailey-Davis L, Bandeen-Roche K, et al. Attention deficit disorder, stimulant use, and childhood body mass index trajectory. Pediatrics. 2014;133(4):668–676. doi: 10.1542/peds.2013-3427. https://doi.org/10.1542/peds.2013-3427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Casey JA, Savitz DA, Rasmussen SG, et al. Unconventional natural gas development and birth outcomes in Pennsylvania, USA. Epidemiology. 2016;27(2):163–172. doi: 10.1097/EDE.0000000000000387. https://doi.org/10.1097/EDE.0000000000000387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bailey LC, Forrest CB, Zhang P, Richards TM, Livshits A, DeRusso PA. Association of antibiotics in infancy with early childhood obesity. JAMA Pediatr. 2014;168(11):1063–1069. doi: 10.1001/jamapediatrics.2014.1539. https://doi.org/10.1001/jamapediatrics.2014.1539. [DOI] [PubMed] [Google Scholar]
- 15.Boss EF, Benke JR, Tunkel DE, Ishman SL, Bridges JF, Kim JM. Public insurance and timing of polysomnography and surgical care for children with sleep-disordered breathing. JAMA Otolaryngol Head Neck Surg. 2015;141(2):106–111. doi: 10.1001/jamaoto.2014.3085. https://doi.org/10.1001/jamaoto.2014.3085. [DOI] [PubMed] [Google Scholar]
- 16.Rasmussen SG, Ogburn EL, McCormack M, et al. Association between unconventional natural gas development in the Marcellus Shale and asthma exacerbations. JAMA Intern Med. 2016;176(9):1334–1343. doi: 10.1001/jamainternmed.2016.2436. https://doi.org/10.1001/jamainternmed.2016.2436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Townsend P, Phillimore P, Beattie A. Health and Deprivation: Inequality and the North. London, England: Routledge; 1988. [Google Scholar]
- 18.Department for Communities and Local Government. [Accessed January 17, 2017];The English Indices of Deprivation. 2010 www.gov.uk/government/uploads/system/uploads/attachment_data/file/6320/1870718.pdf.
- 19.Court H, McLean G, Guthrie B, Mercer SW, Smith DJ. Visual impairment is associated with physical and mental comorbidities in older adults: a cross-sectional study. BMC Med. 2014;12(1):181. doi: 10.1186/s12916-014-0181-7. https://doi.org/10.1186/s12916-014-0181-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dhalwani NN, West J, Sultan AA, Ban L, Tata LJ. Women with celiac disease present with fertility problems no more often than women in the general population. Gastroenterology. 2014;147(6):1267–1274. doi: 10.1053/j.gastro.2014.08.025. https://doi.org/10.1053/j.gastro.2014.08.025. [DOI] [PubMed] [Google Scholar]
- 21.Osborn DP, Hardoon S, Omar RZ, et al. Cardiovascular risk prediction models for people with severe mental illness: results from the prediction and management of cardiovascular risk in people with severe mental illnesses (PRIMROSE) research program. JAMA Psychiatry. 2015;72(2):143–151. doi: 10.1001/jamapsychiatry.2014.2133. https://doi.org/10.1001/jamapsychiatry.2014.2133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shah AD, Langenberg C, Rapsomaniki E, et al. Type 2 diabetes and incidence of cardiovascular diseases: a cohort study in 1.9 million people. Lancet Diabetes Endocrinol. 2015;3(2):105–113. doi: 10.1016/S2213-8587(14)70219-0. https://doi.org/10.1016/S2213-8587(14)70219-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Casey JA, James P, Rudolph KE, Wu CD, Schwartz BS. Greenness and birth outcomes in a range of Pennsylvania communities. Int J Environ Res Public Health. 2016;13(3):311. doi: 10.3390/ijerph13030311. https://doi.org/10.3390/ijerph13030311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nau C, Schwartz BS, Bandeen-Roche K, et al. Community socioeconomic deprivation and obesity trajectories in children using electronic health records. Obesity (Silver Spring) 2015;23(1):207–212. doi: 10.1002/oby.20903. https://doi.org/10.1002/oby.20903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kanaya AM, Adler N, Moffet HH, et al. Heterogeneity of diabetes outcomes among Asians and Pacific Islanders in the U.S.: the Diabetes Study of Northern California (DISTANCE) Diabetes Care. 2011;34(4):930–937. doi: 10.2337/dc10-1964. https://doi.org/10.2337/dc10-1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Diez Roux AV. Neighborhoods and Health: What Do We Know? What Should We Do? Am J Public Health. 2016;106(3):430–431. doi: 10.2105/AJPH.2016.303064. https://doi.org/10.2105/AJPH.2016.303064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Braveman PA, Cubbin C, Egerter S, et al. Socioeconomic status in health research: one size does not fit all. JAMA. 2005;294(22):2879–2888. doi: 10.1001/jama.294.22.2879. https://doi.org/10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- 28.Krieger N, Williams DR, Moss NE. Measuring social class in U.S. public health research: concepts, methodologies, and guidelines. Annu Rev Public Health. 1997;18:341–378. doi: 10.1146/annurev.publhealth.18.1.341. https://doi.org/10.1146/annurev.publhealth.18.1.341. [DOI] [PubMed] [Google Scholar]
- 29.Adler NE, Stead WW. Patients in context--EHR capture of social and behavioral determinants of health. N Engl J Med. 2015;372(8):698–701. doi: 10.1056/NEJMp1413945. https://doi.org/10.1056/NEJMp1413945. [DOI] [PubMed] [Google Scholar]
- 30.Estabrooks PA, Boyle M, Emmons KM, et al. Harmonized patient-reported data elements in the electronic health record: supporting meaningful use by primary care action on health behaviors and key psychosocial factors. J Am Med Inform Assoc. 2012;19(4):575–582. doi: 10.1136/amiajnl-2011-000576. https://doi.org/10.1136/amiajnl-2011-000576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hatch B, Tillotson C, Angier H, et al. Using the electronic health record for assessment of health insurance in community health centers. J Am Med Inform Assoc. 2016;23(5):984–990. doi: 10.1093/jamia/ocv179. https://doi.org/10.1093/jamia/ocv179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Smith J, Medalia C. Health Insurance Coverage in the United States: 2014. U.S. Government Printing Office; Washington, DC: 2015. [Google Scholar]
- 33.Thompson LM, Murray KA, Jarvis S, Scarr E. Exploring the relationship between health insurance, social connectedness, and subjective social status among residents of O’ahu. Hawaii J Med Public Health. 2016;75(11):323–331. [PMC free article] [PubMed] [Google Scholar]
- 34.Hirsch AG, Stewart WF, Sundaresan AS, et al. Nasal and sinus symptoms and chronic rhinosinusitis in a population-based sample. Allergy. 2017;72(2):274–281. doi: 10.1111/all.13042. https://doi.org/10.1111/all.13042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schneider D. Wealth and the Marital Divide. Am J Sociol. 2011;117(2):627–667. doi: 10.1086/661594. https://doi.org/10.1086/661594. [DOI] [PubMed] [Google Scholar]
- 36.DiPrete TA, McManus PA. Family change, employment transitions, and the welfare state: Household income dynamics in the United States and Germany. Am Sociol Rev. 2000;65(3):343–370. https://doi.org/10.2307/2657461. [Google Scholar]
- 37.Tustin AW, Hirsch AG, Rasmussen SG, Casey JA, Bandeen-Roche K, Schwartz BS. Associations between unconventional natural gas development and nasal and sinus, migraine headache, and fatigue symptoms in Pennsylvania. Environ Health Perspect. 2017;125(2):189–197. doi: 10.1289/EHP281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schwartz BS, Stewart WF, Godby S, et al. Body mass index and the built and social environments in children and adolescents using electronic health records. Am J Prev Med. 2011;41(4):e17–e28. doi: 10.1016/j.amepre.2011.06.038. https://doi.org/10.1016/j.amepre.2011.06.038. [DOI] [PubMed] [Google Scholar]
- 39.Minnesota Population Center. National Historical Geographic Information System: Version 11.0 [Database] Minneapolis: University of Minnesota; [Accessed December 20, 2016]. https://doi.org/10.18128/D050.V11.0. Published 2016. [Google Scholar]
- 40.Kawachi I, Berkman LF. Neighborhoods and Health. New York, NY: Oxford University Press; 2003. https://doi.org/10.1093/acprof:oso/9780195138382.001.0001. [Google Scholar]
- 41.Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47(11):1245–1251. doi: 10.1016/0895-4356(94)90129-5. https://doi.org/10.1016/0895-4356(94)90129-5. [DOI] [PubMed] [Google Scholar]
- 42.Wang T-F, Shi L, Nie X, Zhu J. Race/ethnicity, insurance, income and access to care: the influence of health status. Int J Equity Health. 2013;12(1):29. doi: 10.1186/1475-9276-12-29. https://doi.org/10.1186/1475-9276-12-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gonzales G, Golberstein E, Hill SC, Zuvekas SH. Psychological distress and enrollment in Medicaid. J Behav Health Serv Res. 2016:1–13. doi: 10.1007/s11414-016-9532-9. https://doi.org/10.1007/s11414-016-9532-9. [DOI] [PubMed]
- 44.Sommers BD, Kenney GM, Epstein AM. New evidence on the Affordable Care Act: coverage impacts of early Medicaid expansions. Health Aff (Millwood) 2014;33(1):78–87. doi: 10.1377/hlthaff.2013.1087. https://doi.org/10.1377/hlthaff.2013.1087. [DOI] [PubMed] [Google Scholar]
- 45.Wherry LR, Miller S. Early coverage, access, utilization, and health effects associated with the Affordable Care Act Medicaid expansions: a quasi-experimental study. Ann Intern Med. 2016;164(12):795–803. doi: 10.7326/M15-2234. https://doi.org/10.7326/M15-2234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Smolen JR, Thorpe RJ, Jr, Bowie JV, Gaskin DJ, LaVeist TA. Health insurance and chronic conditions in low-income urban whites. J Urban Health. 2014;91(4):637–647. doi: 10.1007/s11524-014-9875-6. https://doi.org/10.1007/s11524-014-9875-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Majidi S, Wadwa RP, Bishop FK, et al. The effect of insurance status and parental education on glycemic control and cardiovascular disease risk profile in youth with Type 1 Diabetes. J Diabetes Metab Disord. 2014;13:59. doi: 10.1186/2251-6581-13-59. https://doi.org/10.1186/2251-6581-13-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Putnam LR, Tsao K, Nguyen HT, Kellagher CM, Lally KP, Austin MT. The impact of socioeconomic status on appendiceal perforation in pediatric appendicitis. J Pediatr. 2016;170:156–160. doi: 10.1016/j.jpeds.2015.11.075. https://doi.org/10.1016/j.jpeds.2015.11.075. [DOI] [PubMed] [Google Scholar]
- 49.Bergmark RW, Ishman SL, Scangas GA, Cunningham MJ, Sedaghat AR. Socioeconomic determinants of overnight and weekend emergency department use for acute rhinosinusitis. Laryngoscope. 2015;125(11):2441–2446. doi: 10.1002/lary.25390. https://doi.org/10.1002/lary.25390. [DOI] [PubMed] [Google Scholar]
- 50.Robinson MR, Daniel LC, O’Hara EA, Szabo MM, Barakat LP. Insurance status as a sociodemographic risk factor for functional outcomes and health-related quality of life among youth with sickle cell disease. J Pediatr Hematol Oncol. 2014;36(1):51–56. doi: 10.1097/MPH.0000000000000013. https://doi.org/10.1097/MPH.0000000000000013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Moorman AC, Gordon SC, Rupp LB, et al. Baseline characteristics and mortality among people in care for chronic viral hepatitis: the chronic hepatitis cohort study. Clin Infect Dis. 2013;56(1):40–50. doi: 10.1093/cid/cis815. https://doi.org/10.1093/cid/cis815. [DOI] [PubMed] [Google Scholar]
- 52.Grant SR, Walker GV, Guadagnolo BA, Koshy M, Allen PK, Mahmood U. Variation in insurance status by patient demographics and tumor site among nonelderly adult patients with cancer. Cancer. 2015;121(12):2020–2028. doi: 10.1002/cncr.29120. https://doi.org/10.1002/cncr.29120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.LaPar DJ, Stukenborg GJ, Guyer RA, et al. Primary payer status is associated with mortality and resource utilization for coronary artery bypass grafting. Circulation. 2012;126(11 Suppl 1):S132–139. doi: 10.1161/CIRCULATIONAHA.111.083782. https://doi.org/10.1161/CIRCULATIONAHA.111.083782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Peters HE, Simon K, Taber JR. Marital disruption and health insurance. Demography. 2014;51(4):1397–1421. doi: 10.1007/s13524-014-0317-6. https://doi.org/10.1007/s13524-014-0317-6. [DOI] [PubMed] [Google Scholar]
- 55.Galobardes B, Shaw M, Lawlor DA, Lynch JW, Davey Smith G. Indicators of socioeconomic position (part 1) J Epidemiol Community Health. 2006;60(1):7–12. doi: 10.1136/jech.2004.023531. https://doi.org/10.1136/jech.2004.023531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Haas JS, Lee LB, Kaplan CP, Sonneborn D, Phillips KA, Liang SY. The association of race, socioeconomic status, and health insurance status with the prevalence of overweight among children and adolescents. Am J Public Health. 2003;93(12):2105–2110. doi: 10.2105/ajph.93.12.2105. https://doi.org/10.2105/AJPH.93.12.2105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Robert S, House JS. SES differentials in health by age and alternative indicators of SES. J Aging Health. 1996;8(3):359–388. doi: 10.1177/089826439600800304. https://doi.org/10.1177/089826439600800304. [DOI] [PubMed] [Google Scholar]
- 58.Diez Roux AV, Mair C. Neighborhoods and health. Ann N Y Acad Sci. 2010;1186(1):125–145. doi: 10.1111/j.1749-6632.2009.05333.x. https://doi.org/10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- 59.The Henry J. Kaiser Family Foundation. [Accessed July 28, 2017];Key Facts about the Uninsured Population. www.kff.org/uninsured/fact-sheet/key-facts-about-the-uninsured-population/. Published 2016.
- 60.Reardon SF, Fox L, Townsend J. Neighborhood Income Composition by Household Race and Income, 1990–2009. Ann Am Acad Pol Soc Sci. 2015;660(1):78–97. https://doi.org/10.1177/0002716215576104. [Google Scholar]
- 61.National Academy of Medicine. Capturing Social and Behavioral Domains and Measures in Electronic Health Records: Phase 2. Washington, DC: 2014. [Google Scholar]
- 62.Schenker N, Raghunathan TE, Chiu P-L, Makuc DM, Zhang G, Cohen AJ. Multiple imputation of missing income data in the National Health Interview Survey. J Am Stat Assoc. 2006;101(475):924–933. https://doi.org/10.1198/016214505000001375. [Google Scholar]
- 63.Giuse NB, Koonce TY, Kusnoor SV, et al. Institute of Medicine measures of social and behavioral determinants of health: a feasibility study. Am J Prev Med. 2017;52(2):199–206. doi: 10.1016/j.amepre.2016.07.033. https://doi.org/10.1016/j.amepre.2016.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gottlieb LM, Hessler D, Long D, et al. Effects of social needs screening and in-person service navigation on child health: a randomized clinical trial. JAMA Pediatr. 2016;170(11):e162521. doi: 10.1001/jamapediatrics.2016.2521. https://doi.org/10.1001/jamapediatrics.2016.2521. [DOI] [PubMed] [Google Scholar]
- 65.Solberg LI. Theory vs practice: should primary care practice take on social determinants of health now? No. Ann Fam Med. 2016;14(2):102–103. doi: 10.1370/afm.1918. https://doi.org/10.1370/afm.1918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Shanafelt TD, Dyrbye LN, West CP. Addressing physician burnout: The way forward. JAMA. 2017;317(9):901–902. doi: 10.1001/jama.2017.0076. https://doi.org/10.1001/jama.2017.0076. [DOI] [PubMed] [Google Scholar]
- 67.Agarwal V, Podchiyska T, Banda JM, et al. Learning statistical models of phenotypes using noisy labeled training data. J Am Med Inform Assoc. 2016;23(6):1166–1173. doi: 10.1093/jamia/ocw028. https://doi.org/10.1093/jamia/ocw028. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.