Abstract
Introduction
Women from lower-income backgrounds have the highest rates of obesity. Thus, effective programs for this high-risk population are urgently needed. Evidence suggests that adding financial incentives to treatment helps to engage and promote health behavior change in lower-income populations; however, this has never been tested in women for obesity treatment. The purpose of this study was to examine whether adding small financial incentives to Internet weight loss treatment yields better weight loss outcomes in women from lower-income backgrounds compared with the same treatment without incentives. Weight losses in lower versus higher income women were also compared.
Methods
Data were pooled from two randomized trials in which women (N=264) received either Internet behavioral weight loss treatment (IBWL) or IBWL plus incentives (IBWL+$). Weight was objectively assessed. Data were collected and analyzed from 2011 to 2017.
Results
Women from lower-income backgrounds had significantly better weight loss outcomes in IBWL+$ compared with IBWL alone (6.4 [SD=4.9%] vs 2.6 [SD=4.6%], p=0.01). Moreover, a greater percentage achieved a ≥5% weight loss in IBWL+$ vs IBWL alone (52.6% vs 38.1%, p=0.01). Interestingly, the comparison between lower-income versus higher-income groups showed that, in IBWL alone, women with lower income achieved significantly poorer weight losses (3.4 [SD=4.2%] vs 4.9 [SD=4.0%], p=0.03). By contrast, in IBWL+$, weight loss outcomes did not differ by income status (5.0 [SD=5.6%] vs 5.3 [SD=3.8%], p=0.80), and a similar percentage of lower-versus higher-income women achieved a ≥5% weight loss (52.6% vs 53.8%, p=0.93).
Conclusions
An Internet behavioral weight loss program plus financial incentives may be an effective strategy to promote excellent weight losses in women with lower income, thereby enhancing equity in treatment outcomes in a vulnerable, high-risk population. These data also provide important evidence to support federally funded incentive initiatives for lower-income, underserved populations.
INTRODUCTION
Women from lower-income backgrounds have the highest rates of obesity and are more likely to develop costly and debilitating obesity-related health conditions.1–3 Despite their high risk, women with lower income are alarmingly underrepresented in obesity treatment programs.4,5 Moreover, when they do enroll, they tend to achieve poorer weight loss outcomes relative to women of higher SES.6 As such, innovative approaches are urgently needed to address obesity and reduce health disparities in this high-risk subgroup.
Few large trials have specifically targeted women from lower-income backgrounds for weight loss. To the authors’ knowledge, all of the trials have involved weekly, face-to-face treatment. For example, Samuel-Hodge and colleagues7 randomized women with lower income (≤200% below federal poverty line, or less thañ$50,000 per year, regardless of household size8,9) to either a behavioral weight loss intervention similar to the Diabetes Prevention Program (DPP; weekly group sessions, behavioral strategies) or a newsletter control. Results showed that the DPP-based intervention yielded significantly better weight losses compared with no treatment control. Women with lower income assigned to the intensive DPP-based intervention lost 4% of initial body weight and 47% met the 5% weight loss goal.7 Similar magnitudes of weight loss have been observed in other trials using intensive, face-to-face treatment.10,11
Although results from face-to-face interventions are encouraging, in-person interventions are expensive, and reach is particularly poor in communities of greatest need. By contrast, web-based interventions have potential for high reach among lower-income women, particularly given this population’s high Internet access (85%).12 Web programs also eliminate the need for regular in-person visits, which can be costly because of transportation and childcare expenses.13 Moreover, the asynchrony of web interventions may help to combat documented adherence barriers among lower-income populations,14–16 as it allows treatment to be accessible at any time of day, which may be especially beneficial for women working multiple jobs or jobs with unconventional hours. Although web interventions for this high-risk population may be particularly relevant and appealing,8 web-based approaches for this population have not been extensively tested. Given data showing that weight losses are often more modest in web (versus in-person) treatment,17 methods to enhance outcomes in web interventions are needed to fully exploit the potential public health impact of this approach.
From an operant conditioning perspective, financial rewards for health behavior change might be particularly effective at enhancing treatment outcomes for women from lower-income backgrounds. Indeed, there are a myriad of structural factors that contribute to obesity among lower-income populations, including limited access to and affordability of healthy foods. Impoverished environments have also been shown to have few alternative sources of healthy reinforcement, making responding to basic sources of reinforcement (e.g., palatable food) more resistant to change.18 At the same time, humans have greater bias for the present (defined as having a preference for immediate rewards versus delayed rewards, or delayed discounting19), with growing evidence to suggest that being from a lower-income background is associated with higher levels of present bias.20 Thus, impoverished environments, coupled with greater present bias, may in part help to explain why health risk behaviors that provide immediate rewards (e.g., high-fat food consumption) may be selected over those that provide longer-term health benefits in economically disadvantaged populations.20 Interestingly, financial rewards, when delivered in a timely fashion, provide an alternative form of reinforcement and leverage that same bias for the present that motivates risk behaviors to actually promote health behavior change. Findings from the substance abuse and cardiac rehabilitation literature show that incentives are very effective in lower-income populations. For example, Kendzor and colleagues21 showed that adding incentives to a smoking cessation program yielded significantly better abstinence rates compared with the same program without incentives in a lower-income sample. Similarly, Gaalema and colleagues22 demonstrated that incentivizing attendance to cardiac rehabilitation appointments significantly improved adherence to cardiac rehabilitation in Medicaid patients. Despite these promising findings, a weight loss financial incentive intervention for women from disadvantaged backgrounds has never been examined.
The purpose of this study is to examine the effects of a web-based obesity treatment intervention that involved small financial incentives on weight loss outcomes in women from lower-income backgrounds. Data were pooled from two randomized trials in which participants received Internet behavioral weight loss treatment (IBWL) or Internet behavioral weight loss treatment plus modest financial incentives (IBWL+$).23,24 Results from these two trials were similar to those of previous studies demonstrating the beneficial effects of various types of financial incentives (lotteries, deposit contracts) on weight loss outcomes.25–27 Specifically, study results demonstrate that, in the overall sample (all income levels), IBWL+$ yields better weight loss outcomes than IBWL alone.23,24 Given that these studies did not examine the effects of income on treatment outcomes and that such an approach may yield important information on reducing obesity in high-risk, economically disadvantaged populations, such effects are explored in this secondary data analysis. The primary hypothesis is that women with lower income randomized to IBWL+$ would lose significantly more weight and have better treatment adherence compared with women from lower-income backgrounds randomized to IBWL without incentives. Exploratory analyses compare women with lower income to women with higher income on weight loss outcomes and treatment adherence.
METHODS
Data for the present analysis were pooled from two randomized trials that examined weight loss outcomes among adults (all income levels) enrolled in IBWL versus IBWL+$; study details, including consort diagrams, can be found in main trial publications.23,24 Data were pooled to maximize sample size. The aims of this secondary data analysis have never been examined or reported previously. All study procedures were approved by the Miriam Hospital’s IRB.
Study Population
The present analysis focused on women only (N=264; Trial 1: n=147; Trial 2: n=117). Exclusion criteria were identical in the two trials: BMI<25kg/m2, participation in another weight loss program, a medical condition that could make weight loss unsafe, planned relocation, lack of Internet access (those willing to access the web at libraries and other public places were not excluded), and non-English speaking. All participants were recruited from the greater Providence area. At baseline, women indicated their total household income: $0–$25,000; $25,001–$50,000; $50,001–$75,000; $75,001–$100,000; $100,001–$125,000; ≥$125,001. Consistent with criteria used in previous studies7–9 and federal benefit qualifications,28 participants whose total household income was ≤$50,000 per year (less than ~200% above the federal poverty line) were classified as lower income, whereas participants with household incomes >$50,000 were classified as higher income. Of note, household size is commonly unstable in lower-income populations; thus, because of this instability, household size was not taken into account when determining income level. This approach is consistent with those of previous studies focused on lower-income populations.7–9
Interventions
The two interventions were administered in the same fashion in both studies.
IBWL was 3 months in length and content was consistent with weight loss strategies prescribed in the DPP.29 Women randomized to IBWL attended a single group visit during which weight, diet, and activity goals were prescribed and self-monitoring skills were taught. Specifically, women were given the goal of losing 1–2 pounds/week and overall weight loss goals of losing 5%, and eventually 10%, of initial body weight. Calorie goals were dependent on baseline weight (<250 pounds: 1,200–1,500 kcal/day; ≥250 pounds: 1,500–1,800 kcal/day). Physical activity goals gradually increased from 50 minutes/week to 250 minutes/week. At the end of the visit, all women were oriented to the IBWL website, which was accessible via desktop or tablet. The IBWL website included weekly multimedia lessons with information on reducing caloric intake, increasing physical activity, and behavior change (e.g., goal setting). IBWL also had a self-monitoring platform where women submitted daily weight, calorie, and activity information, and received weekly, automated feedback.
IBWL+$ involved all IBWL components plus modest incentives for submitting self-monitoring data into the study website and achieving weight goals. Given that self-monitoring is associated with greater weight loss,30 every week women submitted ≥5 days of self-monitoring information (weight, diet, activity) into the website, they received a small financial incentive. The incentive schedule was set by investigators and was based on principles from behavioral economics31,32; incentives varied in size and to ensure that women would self-monitor on all weeks (not just high payout weeks), women were not informed of the reinforcement schedule prior to treatment. Instead, they were told that each week they submit ≥5 days of self-monitoring information, they would receive anywhere from $1 to $10. To engage and reinforce participants at intervention outset, larger incentives were delivered at the beginning of the program (Week 1: $8, Week 2: $10) and incentive size varied thereafter ($1, $2, $7, etc.). If all reporting was completed during the program, a total of $45 could be earned (maximum average of $3.75/week). The IBWL+$ website included a “bank,” which allowed for proximal reinforcement; if women engaged in ≥5 days of self-monitoring, they saw their bank increase on the website. Those who lost 5%–10% or ≥10% of initial body weight at post-treatment were entered into a $50 or $100 raffle, respectively. Ten winners were chosen from each raffle. All payouts were delivered immediately following the post-treatment assessment.
Measures
Assessments were conducted at baseline and month 3 (post-treatment) by blinded staff. Participants were compensated $25 for completing the post-treatment assessment.
Basic demographic information was collected. At baseline, height was measured using a wall-mounted stadiometer. At both baseline and post-treatment, weight was objectively assessed. Internet program adherence (log-ins, lessons viewed, and submission of self-monitoring information) was directly obtained from the study website.
Statistical Analysis
Analyses were conducted using SPSS statistics software, version 22. To test the primary hypothesis, n=58 women from lower-income backgrounds would be needed to achieve 80% power for a two-sided test at p=0.05 to detect a 3.5% difference in weight loss outcomes between IBWL+$ and IBWL. Descriptive statistics were used to examine baseline participant characteristics. Group differences in baseline characteristics were assessed with ANOVA or chi-square tests for continuous or categorical variables, respectively. All treatment (IBWL versus IBWL+$) and income (lower versus higher) effects were examined using ANOVAs. Participants who did not attend the post-treatment assessment were assumed to have remained at baseline weight. To examine intervention and income effects in completion rates and in achieving clinically meaningful (5% or 10%) weight loss,33 logistical regression was used. Given that data were pooled from two studies, study differences in participant characteristics and weight outcomes were examined. Participant characteristics (age, race, ethnicity, SES, or baseline BMI) and overall percent weight loss did not significantly differ by study (p’s≥0.07). There was a significant difference in 5% weight loss (p=0.012). Thus, to be conservative, study was included as a covariate. Data were collected and analyzed from 2011 to 2017.
RESULTS
Women (N=264) were 86.4% non-Hispanic white with a baseline BMI of 33.3 (SD=6.0) kg/m2; (Table 1). Among women with lower income (n=61), there were no significant differences in baseline characteristics by intervention arm (p’s≥0.15; Table 1). Similarly, among those with higher income (n=203), there were no differences in baseline characteristics by treatment arm (p’s≥0.30; Table 1). By contrast, a comparison of baseline characteristics between income groups revealed significant effects. Women with lower income were more likely to be from a racial/ethnic minority group (27.9% vs 9.4%, p<0.001), were significantly younger (39.9 [SD=13.2 years] vs 47.7 [SD=8.9 years], p<0.001), and had a significantly higher baseline BMI (34.5 [SD=6.6] vs 32.1 [SD=5.8], p=0.048). Income did not affect overall study completion rate (lower income: 93.4%, higher income: 89.7%, p=0.38).
Table 1.
Baseline Participant Characteristics
| Characteristics | Total sample (N=264) | Participants with lower income (N=61) | Participants with higher income (N=203) | ||
|---|---|---|---|---|---|
|
|
|||||
| IBWL+$ | IBWL | IBWL+$ | IBWL | ||
| Age, mean (SD) | 45.9±10.6 | 39.7±11.5 | 40.0±14.0 | 47.8±7.7 | 47.7±9.3 |
| Race/ethnicity, % | |||||
| Non-Hispanic white | 86.4 | 68.4 | 73.8 | 90.4 | 90.7 |
| Non-white | 13.6 | 31.6 | 26.2 | 9.6 | 9.3 |
| African American | 8.7 | 15.8 | 21.4 | 5.8 | 5.3 |
| Asian | 0.8 | 5.3 | 0.0 | 0.0 | 0.7 |
| Native Hawaiian/Pacific Islander | 0.4 | 0.0 | 0.0 | 1.9 | 0.0 |
| Multiracial | 1.9 | 10.5 | 0 | 1.9 | 2.6 |
| Hispanic/Latino | 1.5 | 0.0 | 4.8 | 0.0 | 0.7 |
| Total household income, % | |||||
| $0–$25,000 | 1.9 | 15.8 | 4.8 | – | – |
| $25,001–$50,000 | 21.2 | 84.2 | 95.2 | – | – |
| $50,001–$75,000 | 23.9 | – | – | 32.7 | 30.5 |
| $75,001–$100,000 | 15.5 | – | – | 21.2 | 19.9 |
| $100,001–$125,000 | 19.3 | – | – | 23.1 | 25.8 |
| ≥$125,001 | 18.2 | – | – | 23.1 | 23.8 |
| BMI, kg/m2, mean (SD) | 33.3±6.0 | 34.9±7.1 | 34.4±6.5 | 32.8±6.4 | 33.0±5.6 |
IBWL, Internet behavioral weight loss; IBWL+$, Internet behavioral weight loss plus financial incentives.
Women with lower income achieved significantly better weight loss outcomes if assigned to IBWL+$ versus IBWL alone. Specifically, women from lower-income backgrounds in IBWL+$ had a 6.4 (SD=4.9) percent weight loss, whereas those in IBWL alone had a 2.6 (SD=4.6) percent weight loss (p=0.01; Figure 1). Furthermore, a greater percentage of women in IBWL+$ achieved a ≥5% weight loss (52.6%, 38.1%, p=0.01) and a ≥10% weight loss (21.1%, 4.8%, p=0.048). Regarding adherence, compared with lower income women in IBWL alone, those in IBWL+$ logged into the study website more frequently, viewed more lessons, and self-monitored more often (p’s≤0.05; Table 2). Completion rates did not significantly differ by arm (IBWL+$: 100%, IBWL: 90.5%, p=0.17).
Figure 1. Treatment effects by income status.
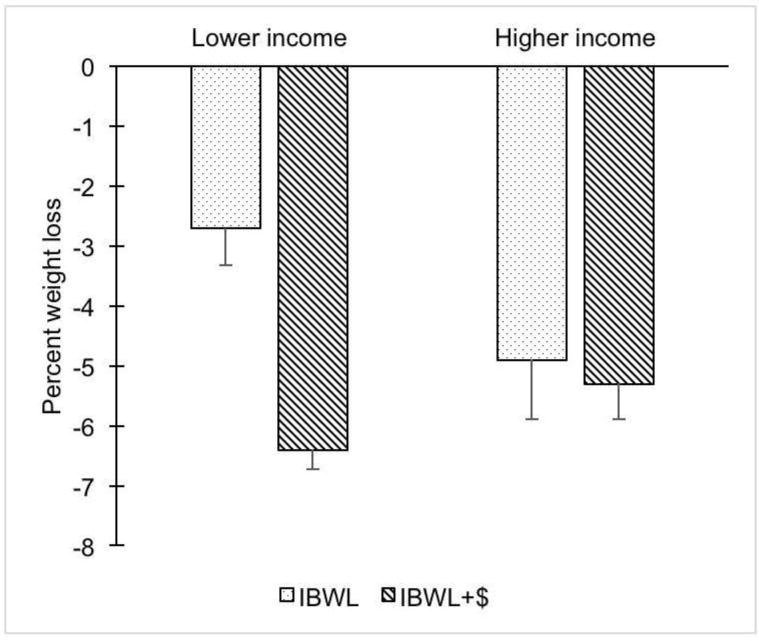
Notes: Given that study was included as a covariate, adjusted means are presented. Error bars represent SEM.
IBWL, Internet behavioral weight loss; IBWL+$, Internet behavioral weight loss plus financial incentives; SEM, SE of the mean.
Table 2.
Participant Adherence
| IBWL | IBWL + $ | |||
|---|---|---|---|---|
|
|
||||
| Adherence and earnings | Lower income |
Higher income |
Lower income |
Higher income |
| Percentage of weeks participants logged in | 70.2% | 82.1% | 78.6% | 90.9% |
| Percentage of lessons viewed | 47.1% | 59.6% | 67.2% | 62.0% |
| Percentage of weeks participants submitted at least 5 days of self-monitoring data | 23.6% | 48.7% | 49.0% | 60.9% |
| Total self-monitoring earnings, mean (SD) | – | – | $17.8±17.9 | $27.4±14.9 |
| Percentage of eligible participants who won a raffle prize | – | – | 30.0% | 30.0% |
| Completion rate | 90.5% | 88.7% | 100% | 92.3% |
Note: Given that study was included as a covariate, adjusted means are presented.
IBWL, Internet behavioral weight loss; IBWL+$, Internet behavioral weight loss plus financial incentives
In IBWL, treatment effects differed by income status. Women with lower income had significantly poorer weight losses compared with women with higher income (p=0.03; Figure 1). Proportion of participants achieving 5% and 10% weight losses differed by income status (5%–10%: lower income 38.1%, higher income 53.6%; ≥10%: lower income 4.8%, higher income 11.9%), but effects did not reach statistical significance (p=0.11, p=0.20). Whether adherence to the IBWL program differed by income category was also examined (Table 2). In IBWL, the percentage of weeks that women submitted ≥5 days of self-monitoring information into the study website differed by income (lower income: 23.6% of weeks, higher income: 48.7% of weeks, p=0.001). Login weeks, lessons viewed, and completion rates did not differ by income status (p’s≥0.22; Table 2).
In contrast to the findings noted above in IBWL alone, in IBWL+$, weight losses achieved were comparable for women with lower versus higher income (p=0.80; Figure 1). Furthermore, a similar percentage of women with lower income achieved a ≥5% weight loss (52.6% vs 53.8%, p=0.93) and ≥10% weight loss (21.1% vs 13.5%, p=0.43). Regarding adherence, income level did not impact lessons viewed (p=0.55) or study completion (p=0.21; Table 2). However, women with lower income logged into the study website less often (p=0.02) and were less likely to complete ≥5 days of self-monitoring compared with women with higher income (p=0.04; Table 2). Consequently, women with lower income earned less money for self-monitoring (p=0.03). Among participants eligible for raffles, randomly chosen winners were equally distributed across income group (p=0.85).
DISCUSSION
This study has important implications for the treatment of obesity in women from economically disadvantaged backgrounds. Consistent with hypotheses, women with lower income who received an Internet weight loss program plus small incentives achieved a significantly greater percent weight loss compared with women with lower income who received the Internet program alone (6.4% vs 2.6%). In fact, women in the incentives arm lost nearly three times as much weight. In addition, consistent with previous research,34 lower-income women had significantly poorer weight loss outcomes in the Internet intervention alone (no incentives) compared with women with higher income; however, when incentives were added to the intervention, these differences in treatment outcomes were eliminated. These findings suggest that adding very modest incentives to a weight loss intervention may help to reduce health disparities for lower-income women.
Although adding incentives to web-based treatment increases cost, given the high rates of obesity-related medical comorbidities in women from lower-income backgrounds, the addition of an incentive may substantially improve health outcomes and outweigh medical costs associated with treating obesity-related health conditions (e.g., diabetes, heart disease).35 In addition, the use of small incentives, as studied herein, is substantially less expensive than in-person treatment.23 Moreover, Medicaid currently supports the use of financial incentive interventions with lower-income women,36 thus providing a vehicle for translation. Specifically, the Centers for Medicare and Medicaid Services (CMS) has allocated more than $100 million dollars to ten states for the use of incentives for health behavior change (weight loss, smoking cessation) in lower-income populations. CMS does not prescribe a specific incentive structure, but requires that all incentive structures be evidence-based and that program evaluation be conducted; such an approach could help to identify optimal incentive structures for underserved, high-risk populations and ensure appropriate use of health incentives among participants. Taken together, results from this study may provide compelling evidence for the use of the incentive paradigm tested herein. As such, the implementation of this paradigm within CMS programs has potential for significant public health impact.
This is the first study to examine the effects of financial incentives for obesity treatment in women from lower-income backgrounds. All prior incentive weight loss studies have focused on both men and women and individuals from all income levels. Moreover, most incentive interventions have used large incentives ($150–$600/person).25,26,37 With such large incentives, individuals are thought to experience a greater boomerang effect when the incentive is removed and revert to old habits.38 Previous work suggests that the use of small incentives, as used here, eliminates such an effect,23 which may have important health implications for this high-risk, vulnerable population. It’s also important to note that the weight losses produced in the Internet incentive intervention herein were better than weight losses achieved in previous intensive face-to-face treatments that targeted lower-income women (6.4% vs 4%).9 The inclusion of incentives could certainly account for these effects. Moreover, the web-based nature of this program may have appealed to this population, circumventing salient barriers to in-person treatment.13–17 Moreover, given the limited reliance on human support and the small incentive size, this Internet incentive approach might be more cost effective than in-person treatment. Future studies may consider examining the effectiveness and cost effectiveness of web versus in-person treatment for this population in a head-to-head comparison.
Limitations
Limitations of this study include a predominantly non-Hispanic white sample and a smaller sample of women from lower-income backgrounds. Future studies should examine the effects of incentives in a larger, more diverse sample. It may also be informative to examine the efficacy of this intervention in women with even lower incomes and explore potential mechanisms of treatment effects (e.g., delayed discounting). This study also has several notable strengths. It focuses on an understudied, high-risk population—lower-income women. Completion was excellent. It also included an active treatment control condition, which is historically lacking in weight loss interventions targeting women with lower income.7–9 Moreover, the design isolated the effects of financial incentives on weight loss outcomes, and weight and adherence data were objectively assessed. Finally, this study is the first to examine the effects of an incentivized Internet intervention for obesity treatment in high-risk lower-income women; such an approach has potential for public health impact.
CONCLUSIONS
Adding modest financial incentives to web-based obesity treatment significantly improves short-term weight loss outcomes among women from economically disadvantaged backgrounds. Such an approach is scalable and could help to mitigate health disparities in this high risk, underserved population.
Acknowledgments
This study was funded by NIH (grant number R18 DK083248). NIH was not directly involved in study conduct or reporting of study results.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
References
- 1.Ogden CL, Lamb MM, Carroll MD, Flegal KM. Obesity and socioeconomic status in adults: United States, 2005–2008. NCHS Data Brief. 2010;50:1–8. [PubMed] [Google Scholar]
- 2.Franks P, Winters PC, Tancredi DJ, Fiscella KA. Do changes in traditional coronary heart disease risk factors over time explain the association between socio-economic status and coronary heart disease? BMC Cardiovasc Disord. 2011;11:28. doi: 10.1186/1471-2261-11-28. https://doi.org/10.1186/1471-2261-11-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and Trends in Diabetes Among Adults in the United States, 1988–2012. JAMA. 2015;314(10):1021–1029. doi: 10.1001/jama.2015.10029. https://doi.org/10.1001/jama.2015.10029. [DOI] [PubMed] [Google Scholar]
- 4.Svetkey LP, Stevens VJ, Brantley PJ, et al. Comparison of strategies for sustaining weight loss: The weight loss maintenance randomized controlled trial. JAMA. 2008;299(10):1139–1148. doi: 10.1001/jama.299.10.1139. https://doi.org/10.1001/jama.299.10.1139. [DOI] [PubMed] [Google Scholar]
- 5.Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. doi: 10.1056/NEJMoa012512. https://doi.org/10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kalarchian MA, Levine MD, Klem ML, Burke LE, Soulakova JN, Marcus MD. Impact of addressing reasons for weight loss on behavioral weight-control outcome. Am J Prev Med. 2011;40(1):18–24. doi: 10.1016/j.amepre.2010.09.019. https://doi.org/10.1016/j.amepre.2010.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Samuel-Hodge CD, Johnston LF, Gizlice Z, et al. Randomized trial of a behavioral weight loss intervention for low-income women: the Weight Wise Program. Obesity (Silver Spring) 2009;17(10):1891–1899. doi: 10.1038/oby.2009.128. https://doi.org/10.1038/oby.2009.128. [DOI] [PubMed] [Google Scholar]
- 8.Samuel-Hodge CD, Garcia BA, Johnston LF, et al. A pilot study comparing two weight loss maintenance interventions among low-income, mid-life women. BMC Public Health. 2013;13:635–644. doi: 10.1186/1471-2458-13-653. https://doi.org/10.1186/1471-2458-13-653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lanpher MG, Askew S, Bennett GG. Health literacy and weight change in a digital health intervention for women: A randomized controlled trial in primary care practice. J Health Commun. 2016;21(suppl 1):34–42. doi: 10.1080/10810730.2015.1131773. https://doi.org/10.1080/10810730.2015.1131773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mayer-Davis EJ, D’Antonio AM, Smith SM, et al. Pounds off with empowerment (POWER): a clinical trial of weight management strategies for black and white adults with diabetes who live in medically underserved rural communities. Am J Public Health. 2004;94(10):1736–1742. doi: 10.2105/ajph.94.10.1736. https://doi.org/10.2105/AJPH.94.10.1736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Samuel-Hodge CD, Garcia BA, Johnston LF, et al. Translation of a behavioral weight loss intervention for mid-life, low-income women in local health departments. Obesity (Silver Spring) 2013;21(9):1764–1773. doi: 10.1002/oby.20317. https://doi.org/10.1002/oby.20317. [DOI] [PubMed] [Google Scholar]
- 12.Perrin A, Duggan M. Americans’ Internet access: 2000–2015. Pew Research Center; 2015. [Google Scholar]
- 13.Swanson GM, Ward AJ. Recruiting minorities into clinical trials: toward a participant-friendly system. J Natl Cancer Inst. 1995;87(23):1747–1759. doi: 10.1093/jnci/87.23.1747. https://doi.org/10.1093/jnci/87.23.1747. [DOI] [PubMed] [Google Scholar]
- 14.Davis MP, Rhode PC, Dutton GR, Redmann SM, Ryan DH, Brantley PJ. A primary care weight management intervention for low-income African American women. Obesity (Silver Spring) 2006;14(8):1412–1420. doi: 10.1038/oby.2006.160. https://doi.org/10.1038/oby.2006.160. [DOI] [PubMed] [Google Scholar]
- 15.Kumanyika S. Nutrition and chronic disease prevention: Priorities for U.S. minority groups. Nutr Rev. 2006;64(suppl 1):S9–14. doi: 10.1111/j.1753-4887.2006.tb00238.x. https://doi.org/10.1111/j.1753-4887.2006.tb00238.x. [DOI] [PubMed] [Google Scholar]
- 16.Graffagnino CL, Falki JM, La Londe M, et al. Effect of a community-based weight management program on weight loss and cardiovascular disease risk factors. Obesity (Silver Spring) 2006;14(2):280–288. doi: 10.1038/oby.2006.36. https://doi.org/10.1038/oby.2006.36. [DOI] [PubMed] [Google Scholar]
- 17.Harvey-Berino J, West D, Krukowski R, et al. Internet delivered behavioral obesity treatment. Prev Med. 2010;51(2):123–128. doi: 10.1016/j.ypmed.2010.04.018. https://doi.org/10.1016/j.ypmed.2010.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carroll ME. The economic context of drug and non-drug reinforcers affects acquisition and maintenance of drug-reinforced behavior and withdrawal effects. Drug Alcohol Depend. 1993;33(2):201–210. doi: 10.1016/0376-8716(93)90061-t. https://doi.org/10.1016/0376-8716(93)90061-T. [DOI] [PubMed] [Google Scholar]
- 19.Loewenstein G, Brennan T, Volpp KG. Asymmetric paternalism to improve health behaviors. JAMA. 2007;298(20):2415–2417. doi: 10.1001/jama.298.20.2415. https://doi.org/10.1001/jama.298.20.2415. [DOI] [PubMed] [Google Scholar]
- 20.Green L, Myerson J, Lichtman D, Rosen S, Fry A. Temporal discounting in choice between delayed rewards: the role of age and income. Psychol Aging. 1996;11(1):79–84. doi: 10.1037//0882-7974.11.1.79. https://doi.org/10.1037/0882-7974.11.1.79. [DOI] [PubMed] [Google Scholar]
- 21.Kendzor DE, Businelle MS, Poonawalla IB, et al. Financial incentives for abstinence among socioeconomically disadvantaged individuals in smoking cessation treatment. Am J Public Health. 2015;105(6):1198–1205. doi: 10.2105/AJPH.2014.302102. https://doi.org/10.2105/AJPH.2014.302102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gaalema DE, Savage PD, Rengo JL, Cutler AY, Higgins ST, Ades PA. Financial incentives to promote cardiac rehabilitation participation and adherence among Medicaid patients. Prev Med. 2016;92:47–50. doi: 10.1016/j.ypmed.2015.11.032. https://doi.org/10.1016/j.ypmed.2015.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leahey TM, Subak LL, Fava JL, et al. Benefits of adding small financial incentives oroptional group meetings to a Web-based statewide obesity initiative. Obesity (Silver Spring) 2015;23(1):70–76. doi: 10.1002/oby.20937. https://doi.org/10.1002/oby.20937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leahey TM, Thomas G, Fava JL, et al. Adding evidence-based behavioral weight loss strategies to a statewide wellness campaign: A randomized trial. Am J Public Health. 2014;104(7):1300–1306. doi: 10.2105/AJPH.2014.301870. https://doi.org/10.2105/AJPH.2014.301870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Volpp KG, John LK, Troxel AB, Norton L, Fassbender J, Loewenstein G. Financial incentive-based approaches for weight loss: a randomized trial. JAMA. 2008;300(22):2631–2637. doi: 10.1001/jama.2008.804. https://doi.org/10.1001/jama.2008.804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kullgren JT, Troxel AB, Loewenstein G, et al. Individual-versus group-based financial incentives for weight loss: a randomized, controlled trial. Ann Intern Med. 2013;158(7):505–514. doi: 10.7326/0003-4819-158-7-201304020-00002. https://doi.org/10.7326/0003-4819-158-7-201304020-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jeffery RW. Financial incentives and weight control. Prev Med. 2012;55(Suppl):S61–67. doi: 10.1016/j.ypmed.2011.12.024. https://doi.org/10.1016/j.ypmed.2011.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Obamacare Facts. The 2016 Federal Poverty Level Guidelines (Used in 2016 and 2017) https://obamacarefacts.com/2016-2017-federal-poverty-guidelines/. Accessed May 1, 2017.
- 29.Diabetes Prevention Program Research Group. The Diabetes Prevention Program: Description of the Lifestyle Intervention. Diabetes Care. 2002;25(12):2165–2171. doi: 10.2337/diacare.25.12.2165. https://doi.org/10.2337/diacare.25.12.2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Johnson F, Wardle J. The association between weight loss and engagement with a web-based food and exercise diary in a commercial weight loss programme: a retrospective analysis. Int J Behav Nutr Phys Act. 2011;8:83. doi: 10.1186/1479-5868-8-83. https://doi.org/10.1186/1479-5868-8-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thaler R. Some empirical evidence on dynamic inconsistency. Econ Lett. 1981;8(3):201–207. https://doi.org/10.1016/0165-1765(81)90067-7. [Google Scholar]
- 32.Bickel W, Vuchinich RE, editors. Reframing Health Behavior Change with Behavioral Economics. Mahwah, NJ: Lawrence Erlbaum Associates; 2000. [Google Scholar]
- 33.NIH. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults–The Evidence Report. Obes Res. 1998;6(suppl 2):51S–209S. [PubMed] [Google Scholar]
- 34.Haff N, Patel MS, Lim R, et al. The role of behavioral economic incentive design and demographic characteristics in financial incentive-based approaches to changing health behaviors: a meta-analysis. Am J Health Promot. 2015;29(5):314–323. doi: 10.4278/ajhp.140714-LIT-333. https://doi.org/10.4278/ajhp.140714-LIT-333. [DOI] [PubMed] [Google Scholar]
- 35.Finkelstein EA, Fiebelkorn IC, Wang G. State-level estimates of annual medical expenditures attributable to obesity. Obes Res. 2004;12(1):18–24. doi: 10.1038/oby.2004.4. https://doi.org/10.1038/oby.2004.4. [DOI] [PubMed] [Google Scholar]
- 36.Centers for Medicare and Medicaid Services. www.cms.gov. Accessed May 1, 2017.
- 37.John LK, Loewenstein G, Troxel AB, Norton L, Fassbender JE, Volpp KG. Financial incentives for extended weight loss: a randomized, controlled trial. J Gen Intern Med. 2011;26(6):621–626. doi: 10.1007/s11606-010-1628-y. https://doi.org/10.1007/s11606-010-1628-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Promberger M, Marteau TM. When do financial incentives reduce intrinsic motivation? Comparing behaviors studied in psychological and economic literatures. Health Psych. 2013;32(9):950–957. doi: 10.1037/a0032727. https://doi.org/10.1037/a0032727. [DOI] [PMC free article] [PubMed] [Google Scholar]


