Abstract
Background
Data about influenza mortality burden in northern China are limited. This study estimated mortality burden in Beijing associated with seasonal influenza from 2007 to 2013 and the 2009 H1N1 pandemic.
Methods
We estimated influenza‐associated excess mortality by fitting a negative binomial model using weekly mortality data as the outcome of interest with the percent of influenza‐positive samples by type/subtype as predictor variables.
Results
From 2007 to 2013, an average of 2375 (CI 1002‐8688) deaths was attributed to influenza per season, accounting for 3% of all deaths. Overall, 81% of the deaths attributed to influenza occurred in adults aged ≥65 years, and the influenza‐associated mortality rate in this age group was higher than the rate among those aged <65 years (113.6 [CI 49.5‐397.4] versus 4.4 [CI 1.7‐18.6] per 100 000, P < .05). The mortality rate associated with the 2009 H1N1 pandemic in 2009/2010 was comparable to that of seasonal influenza during the seasonal years (19.9 [CI 10.4‐33.1] vs 17.2 [CI 7.2‐67.5] per 100 000). People aged <65 years represented a greater proportion of all deaths during the influenza A(H1N1)pdm09 pandemic period than during the seasonal epidemics (27.0% vs 17.7%, P < .05).
Conclusions
Influenza is an important contributor to mortality in Beijing, especially among those aged ≥65 years. These results support current policies to give priority to older adults for seasonal influenza vaccination and help to define the populations at highest risk for death that could be targeted for pandemic influenza vaccination.
Keywords: Beijing, China, H1N1 pandemic, influenza, model, mortality
1. INTRODUCTION
Influenza is a major cause of global morbidity and mortality each year, especially among older adults and those with chronic diseases.1 Although several statistical models have estimated the mortality burden of influenza,2 few have focused on mainland China,3, 4, 5 and information on mortality burden in northern China is especially limited. Considering the diverse seasonality patterns,6 income levels and healthcare access across China, mortality burden may vary by region.
Beijing, the capital of China, is located in northern China. With a resident population of nearly 20 million in 2010, it is one of the most populous cities in the world. During the 2009 H1N1 pandemic, only 10 844 laboratory‐confirmed cases of influenza A(H1N1)pdm09 and 69 deaths were reported in Beijing.7 These numbers solely represent laboratory‐confirmed influenza deaths and not decedents who might have died because of pandemic influenza but were never tested.3 A mathematical modeling study estimated that the likely number of influenza A (H1N1)pdm09 infections in Beijing was 1.8 million during the pandemic period.8 To date, no study has estimated the likely number of influenza A(H1N1)pdm09‐associated deaths in Beijing.
Since 2007, the Beijing Municipal Government has provided seasonal influenza vaccination to priority populations, including adults ≥60 years of age and primary and middle school students, free of charge between September and November each year prior to the start of typical influenza virus circulation. Beijing also conducted influenza A(H1N1)pdm09 vaccination campaigns during the pandemic period.9 These programs were implemented in the absence of local data on influenza‐associated mortality burden because there was concern that this novel virus could have substantial burden on the population's health. Influenza mortality burden data allow programs to determine the potential impact of influenza vaccination and inform investments in prevention strategies. In this study, we modeled mortality data obtained from a representative mortality register system, combined with weekly influenza virus surveillance data, to provide estimates of the mortality impact associated with seasonal influenza and the influenza A(H1N1)pdm09 virus during the pandemic period by specific death categories, age groups, and influenza virus type and subtype in Beijing from 2007 to 2013.
2. METHODS
2.1. Population data
We obtained annual population data from the National Population Census in Beijing, China.10 In 2010, the total population of Beijing was nearly 20 million, of which 12‐13 million were registered residents of Beijing. The remaining 7‐8 million persons were classified as “migrants” who are not registered residents of Beijing. In this study, we used population data of registered populations only to calculate the annual mortality rates.
2.2. Mortality data
Local regulation requires that all deaths in Beijing are registered in the Mortality Register and Surveillance System, managed by Beijing Center for Disease Control and Prevention (BJCDC). We were unable to obtain reliable mortality data among migrants, as both Chinese culture and high medical expenses compel a large proportion of migrants to return to their home provinces when they are severely ill, and therefore, the majority of migrants do not die in Beijing and are not registered in the BJCDC Mortality Register and Surveillance system. In this study, we obtained weekly electronic mortality data for the registered Beijing population from 2007 to 2013, covering the influenza seasons of 2007/2008 to 2012/2013. We defined an influenza season as the period ranging from the 27th week in 1 year to the 26th week in the next year, based on influenza surveillance data.11 The registration system categorized weekly numbers of deaths into two underlying causes of death according to the International Classification of Disease, Tenth Revision [ICD‐10]: respiratory (ICD‐10 codes J00‐99) and circulatory diseases (ICD‐10 codes I00‐99) (respiratory and circulatory: R&C), and all‐cause deaths (including both respiratory and circulatory deaths which have been previously been associated with influenza‐associated deaths).2, 3, 4, 5, 6 Two age groups were considered: <65 years and ≥65 years.
2.3. Influenza virology data
We obtained influenza virology data from the Beijing influenza surveillance system from seasons 2007/2008 to 2012/2013. The influenza surveillance system, designed and managed by BJCDC, included 14 sentinel hospitals in 2007, 17 hospitals in 2008, 20 hospitals in 2011, and 23 hospitals in 2012. In this system, clinicians of surveillance clinics in internal medicine, the emergency department, the fever clinic, and the pediatric clinic were required to diagnose all influenza‐like illness (ILI) cases (patients presenting with fever ≥38°C and cough or sore throat) and to record the weekly numbers of ILI outpatient visits throughout the year. Trained clinicians collected pharyngeal swab specimens from a convenience sample of 10‐20 ILI case‐patients per sentinel hospital per week. Specimens were sent to local CDC laboratories to test for influenza by cell culture. A more detailed description of the surveillance was published in a previous study.12
2.4. Statistical model
A negative binomial model was applied to estimate influenza‐associated excess mortality, using age‐specific weekly mortality data as the outcome and proportions of specimens positive for influenza by type/subtype (not age‐specific) as the predictor variables.3, 4, 5 Models included virology surveillance time series data, as well as time terms to account for the weeks in the model and harmonic terms to account for the cyclical pattern in deaths. Because of the lack of respiratory syncytial virus virology data in Beijing, we did not include this pathogen in the model.
Negative Binomial models were fit separately for the two outcomes (all‐cause and respiratory and circulatory deaths) and age groups (aged <65 years and ≥65 years) using a log link function. The final models were selected by evaluating the AIC/BIC values in combination with the statistical significance of the viral surveillance terms and the harmonic and time terms (for baseline estimation) for each of the models examined (Table S1). Further, we decided to choose the same model for each age group and outcome based on the evaluation of the separate models. We chose to use the same model for each age group for ease of interpretation and better comparison of estimates and methods. The final model selected for both all‐cause and respiratory and circulatory deaths was as follows:
Yt is the weekly variable for the time series from 2007/2008 to 2012/2013 (1‐312) and represents age‐specific weekly number of deaths, α is the offset term equal to the log of the age‐specific population size, β0 represents the intercept, β1 and β2 account for the linear and quadratic time trends, β3 and β4 account for cyclical secular trends, and β5 through β8 represent coefficients associated with the weekly proportion of specimens testing positive for each influenza subtype. Further explanation of our model selection is available in Table S1.
The number of deaths attributed to influenza was calculated as the difference between the predicted influenza‐associated deaths from the full model and the predicted baseline deaths (from the model when the co‐variables for influenza subtype were set to zero). Confidence intervals were generated for excess mortality estimates based on the confidence intervals of the model predictions. Age‐specific excess mortality rates were calculated from the estimated number of deaths attributed to influenza divided by population from the National Population Census in Beijing, China.10 All the statistical analyses were carried out using SAS University Edition (SAS Institute Inc., Cary, NC, USA). A P value < .05 was considered to be statistically significant.
2.5. Ethics approval
Study approval was obtained from the Institutional Review Board and Human Research Ethics Committee of BJCDC.
3. RESULTS
3.1. Mortality data reported from the Mortality Register and Surveillance System and influenza virus activity, from season 2007/2008 to 2012/2013
For the influenza seasons 2007/2008 to 2012/2013, the annual all‐cause mortality rate ranged from 581.7 to 602.6 per 100 000 persons for all ages, and 3238.9 to 3394.3 per 100 000 for adults aged ≥65 years. Adults aged ≥65 years accounted for 76% of all‐cause deaths among all ages. R&C causes represented 58% of all deaths. The annual R&C mortality rate ranged from 335.8 to 346.9 per 100 000 persons for all ages and 2050.0 to 2221.0 per 100 000 for adults aged ≥65 years. Adults aged ≥65 years accounted for 84% of R&C deaths among all ages (Table 1).
Table 1.
Mortality rates (per 100 000 persons) reported from the Mortality Register and Surveillance System by age, Beijing 2007/2008 to 2012/2013 influenza seasons
| All ages | Adults aged ≥65 y (% of deaths among all age) | |||||
|---|---|---|---|---|---|---|
| Population | All‐cause rate | R&C rate (% of all‐cause deaths | Population | All‐cause | R&C | |
| 2007/2008 | 12 047 617 | 581.7 | 343.4 (59) | 1 560 836 | 3394.3 (75.6) | 2221 (83.8) |
| 2008/2009 | 12 208 706 | 575 | 335.8 (58.4) | 1 614 871 | 3292.6 (75.7) | 2113.7 (83.3) |
| 2009/2010 | 12 375 798 | 602.6 | 354.2 (58.8) | 1 664 285 | 3388.4 (75.6) | 2196.3 (83.4) |
| 2010/2011 | 12 518 114 | 593.5 | 346.9 (58.4) | 1 707 318 | 3329.7 (76.5) | 2143.8 (84.3) |
| 2011/2012 | 12 678 603 | 595.3 | 340.8 (57.2) | 1 764 450 | 3274.3 (76.5) | 2064.0 (84.3) |
| 2012/2013 | 12 876 915 | 601.9 | 346.2 (57.5) | 1 840 459 | 3238.9 (76.9) | 2050.0 (84.6) |
R&C, Respiratory and circulatory diseases.
During the 6‐year study period, a total of 60 795 specimens were tested for influenza virus. An average of 15.4% specimens tested positive for influenza for the entire time series. Influenza A(H1N1), A(H1N1)pdm09, and A(H3N2) were each the predominant subtype in one season (2008/2009, 2009/2010, and 2010/2011, respectively), while influenza B predominated in 2 seasons (2007/2008 and 2011/2012), and A(H1N1)pdm09 and A(H3N2) co‐circulated in the 2012/2013 season (Figure 1). Influenza virus activity and mortality both peaked in the winter months of December‐February during the non‐pandemic period and from November of 2009 to February of 2010 during the pandemic period (Figure 1).
Figure 1.
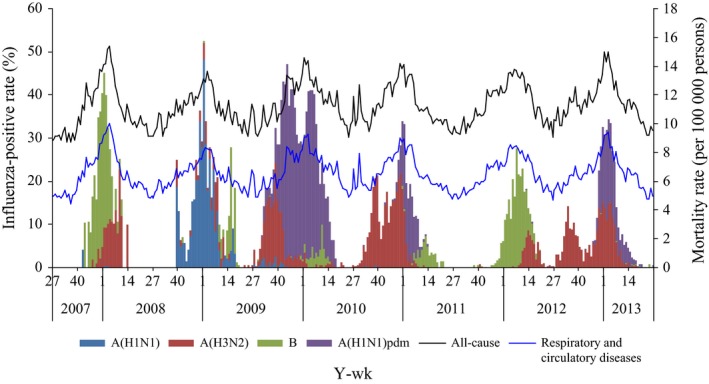
Weekly mortality rates reported from the Mortality Register and Surveillance System and proportions of specimens positive for influenza, Beijing, 2007/2008 to 2012/2013
3.2. Estimates of influenza‐associated deaths, from season 2007/2008 to 2012/2013
Figure 2 presents the weekly time series of observed, predicted, and baseline mortality using a negative binomial regression model. The predicted values fit well with the observed data.
Figure 2.
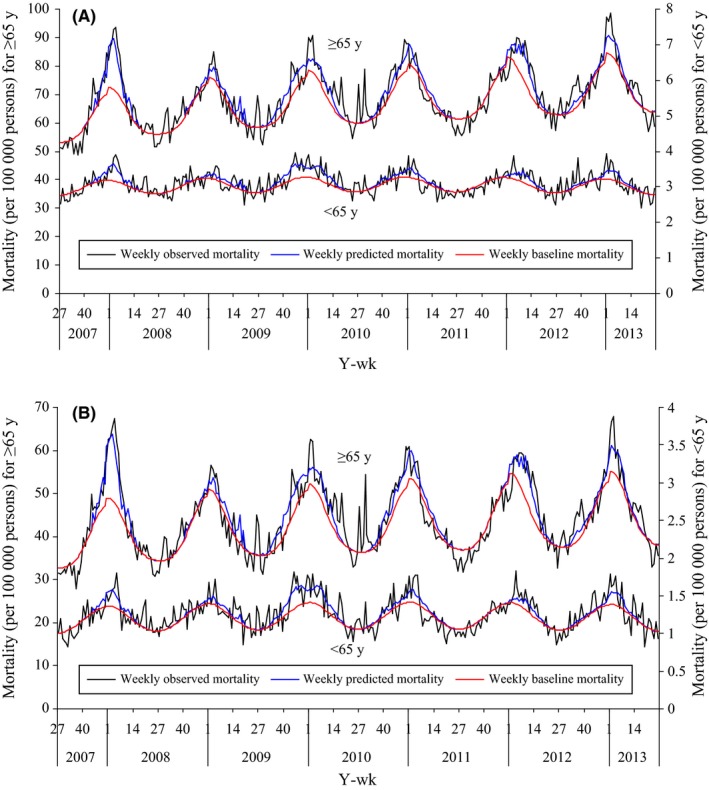
Weekly observed, predicted, and baseline mortality by negative binomial regression model, Beijing, 2007/2008 to 2012/2013. Panel (A) all cause; panel (B) respiratory and circulatory diseases
For all ages, there was year‐to‐year variability in the annual number of influenza‐associated all‐cause deaths, and the mean number of deaths from 2007/2008 to 2012/2013 was 2375(95% confidence interval [CI] 1002‐8688), with a rate of 19.1 (CI 8.1‐69.9) deaths per 100 000 persons (Table 2). Most (81%) influenza‐associated all‐cause deaths occurred among adults aged ≥65 years, and the rate in this age group was higher than the rate among those aged <65 years (113.6 [CI 49.5‐397.4] versus 4.4 [CI 1.7‐18.6] per 100 000, P < .05). There were, on average, 1873 (CI 818‐6684) influenza‐associated R&C deaths per year, with a rate of 15.1 (CI 6.6‐53.8) per 100 000. Influenza‐associated R&C mortality varied by season (ranged from 8.9 [CI 1.7‐48.1] to 23.2 [CI 10.5‐64] per 100 000) and 87% of deaths occurred in those aged ≥65 years.
Table 2.
Influenza‐associated excess deaths and influenza‐associated death rates (per 100 000 persons) by age, Beijing, 2007/2008 to 2012/2013
| Season | Influenza‐associated excess deaths | Influenza‐associated death rates | ||||
|---|---|---|---|---|---|---|
| All agesa | Age≥65 y | All agesa | Age ≥65 y | Age <65 y | ||
| No.(CI) | No. (CI) | % of all agesb | rates(CI) | rates(CI) | rates(CI) | |
| All‐cause | ||||||
| 2007/2008 | 3039 (1788‐9984) | 2562 (1579‐7803) | 84 | 25.2 (14.8‐82.9) | 164.1 (101.2‐499.9) | 4.5 (2‐20.8) |
| 2008/2009 | 1532 (317‐7787) | 1292 (286‐6000) | 84 | 12.5 (2.6‐63.8) | 80 (17.7‐371.5) | 2.3 (0.3‐16.9) |
| 2009/2010 | 3576 (1544‐10126) | 2610 (1039‐7549) | 73 | 28.9 (12.5‐81.8) | 156.8 (62.4‐453.6) | 9 (4.7‐24.1) |
| 2010/2011 | 2101 (707‐7740) | 1670 (591‐5950) | 79 | 16.8 (5.6‐61.8) | 97.8 (34.6‐348.5) | 4 (1.1‐16.6) |
| 2011/2012 | 2225 (1304‐8093) | 1893 (1164‐6371) | 85 | 17.5 (10.3‐63.8) | 107.3 (66‐361.1) | 3 (1.3‐15.8) |
| 2012/2013 | 1777 (350‐8396) | 1391 (280‐6432) | 78 | 13.8 (2.7‐65.2) | 75.6 (15.2‐349.5) | 3.5 (0.6‐17.8) |
| Mean (all years) | 2375 (1002‐8688) | 2375 (1002‐8688) | 81 | 19.1 (8.1‐69.9) | 113.6 (49.5‐397.4) | 4.4 (1.7‐18.6) |
| Mean (seasonal yearsc) | 2135 (893‐8400) | 2135 (893‐8400) | 82 | 17.2 (7.2‐67.5) | 105 (46.9‐386.1) | 3.5 (0.9‐14.6) |
| R&C | ||||||
| 2007/2008 | 2194 (1344‐6467) | 2194 (1344‐6467) | 91 | 20.1 (11.6‐64.7) | 140.6 (86.1‐414.3) | 2.1 (0.6‐12.7) |
| 2008/2009 | 957 (201‐4747) | 957 (201‐4747) | 88 | 8.9 (1.7‐48.1) | 59.3 (12.4‐294) | 1.2 (0.1‐10.7) |
| 2009/2010 | 2284 (995‐6271) | 2284 (995‐6271) | 79 | 23.2 (10.5‐64) | 137.2 (59.8‐376.8) | 5.5 (2.9‐15.4) |
| 2010/2011 | 1489 (613‐4907) | 1489 (613‐4907) | 86 | 13.8 (5.3‐48.1) | 87.2 (35.9‐287.4) | 2.2 (0.5‐10.3) |
| 2011/2012 | 1524 (931‐5061) | 1524 (931‐5061) | 92 | 13.1 (7.6‐47.9) | 86.4 (52.8‐286.8) | 1.3 (0.3‐9.3) |
| 2012/2013 | 1248 (329‐5215) | 1248 (329‐5215) | 85 | 11.4 (2.8‐49.9) | 67.8 (17.9‐283.4) | 2 (0.3‐10.9) |
| Mean (all years) | 1873 (818‐6684) | 1616 (736‐5445) | 87 | 15.1 (6.6‐53.8) | 96.4 (44.1‐323.8) | 2.4 (0.8‐11.5) |
| Mean (seasonal yearsc) | 1673 (721‐6437) | 1482 (684‐5279) | 88 | 13.5 (5.8‐51.7) | 88.2 (41‐313.2) | 1.8 (0.3‐9) |
CI, 95% confidence interval; R&C, Respiratory and circulatory diseases.
The sum of the estimates of influenza‐associated deaths for persons aged ≥65 y and persons aged<65 y.
% of all ages = Influenza‐associated excess deaths for persons aged ≥65 y ÷ Influenza‐associated excess deaths for all ages.
seasonal years: all years excluding 2009/2010.
Table 3 lists influenza death rates by virus type/subtype from season 2007/2008 to 2012/2013. For all ages, the mortality rate associated with influenza B was 7.7 (CI 4.6‐20.3) per 100 000 persons per season for all‐cause mortality, followed by A(H1N1)pdm09 (7.1 [CI 4.1‐19.3] per 100 000 for 2009/2010‐2012/2013) and A(H3N2) (5.6 [CI 1.4‐18.3] per 100 000). Influenza B caused the highest mortality burden (20.5 [CI 14.2‐34.9] per 100 000) when influenza B virus predominated in 2007/2008. A similar pattern was observed among both those aged <65 years and those aged ≥65 years, and also within all respiratory and circulatory deaths (Table 4).
Table 3.
Influenza‐associated death rates (per 100 000 persons) by virus subtype, Beijing, 2007/2008 to 2012/2013
| Season | All | Rates (% of deaths) by virus subtypes | The predominant virus circulating | |||
|---|---|---|---|---|---|---|
| A(H1N1) | A(H3N2) | B | A(H1N1)pdm09 | |||
| All‐cause | ||||||
| 2007/2008 | 25.2 | 0.1 (0.3) | 4.6 (18.3) | 20.5 (81.4) | 0 (0) | B |
| 2008/2009 | 12.5 | 6.4 (51) | 2.2 (17.4) | 4 (31.5) | 0 (0) | A(H1N1) |
| 2009/2010 | 28.9 | 0.3 (0.9) | 6 (20.7) | 2.7 (9.5) | 19.9 (68.9) | A(H1N1)pdm |
| 2010/2011 | 16.8 | 0 (0.1) | 10.3 (61.3) | 2.9 (17.6) | 3.5 (21.1) | A(H3N2) |
| 2011/2012 | 17.5 | 0 (0) | 1.9 (11.1) | 15.6 (88.8) | 0 (0.1) | B |
| 2012/2013 | 13.8 | 0 (0) | 8.7 (63) | 0.2 (1.2) | 4.9 (35.8) | A(H1N1)pdm, A(H3N2) |
| Mean (all years) | 19.1 | 1.1 (8.7) | 5.6 (32) | 7.7 (38.3) | 7.1 (36.6)a | |
| Mean (seasonal yearsb) | 17.2 | 1.3 (5.2) | 5.5 (32.6) | 8.6 (49.9) | 2.8 (17.7)a | |
| R&C | ||||||
| 2007/2008 | 20.1 | 0.1 (0.3) | 4.1 (20.6) | 15.9 (79.1) | 0 (0) | B |
| 2008/2009 | 8.9 | 4.2 (46.9) | 1.9 (21.3) | 2.8 (31.9) | 0 (0) | A(H1N1) |
| 2009/2010 | 23.2 | 0.1 (0.6) | 5 (21.7) | 2.1 (8.8) | 16 (68.9) | A(H1N1)pdm |
| 2010/2011 | 13.8 | 0 (0.1) | 8.8 (64) | 2.1 (15.3) | 2.8 (20.7) | A(H3N2) |
| 2011/2012 | 13.1 | 0 (0) | 1.6 (12.3) | 11.5 (87.7) | 0 (0) | B |
| 2012/2013 | 11.4 | 0 (0) | 7.4 (64.9) | 0.1 (0.9) | 3.9 (34.2) | A(H1N1)pdm, A(H3N2) |
| Mean (all years) | 15.1 | 0.7 (8) | 4.8 (34.1) | 5.7 (37.3) | 5.7 (36.7)a | |
| Mean (seasonal yearsb) | 13.5 | 0.5 (6.2) | 4.7 (35.8) | 6.5 (47.8) | 2.3 (17.7)a | |
Number (proportion) presented.
R&C, Respiratory and circulatory diseases.
Estimates for seasons 2009 to 2013.
seasonal years: all years excluding 2009/2010.
Table 4.
Influenza‐associated death rates (per 100 000 persons) by virus subtype and by age group, Beijing, 2007/2008 to 2012/2013
| Season | Age ≥65 y | Age <65 y | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| All | Rates (% of deaths) by virus subtypes | All | Rates (% of deaths) by virus subtypes | |||||||
| A(H1N1) | A(H3N2) | B | A(H1N1)pdm09 | A(H1N1) | A(H3N2) | B | A(H1N1)pdm09 | |||
| All‐cause | ||||||||||
| 2007/2008 | 164.1 | 0.6 (0.4) | 29 (17.6) | 134.6 (82) | 0 (0) | 4.5 | 0 (0.2) | 1 (21.6) | 3.6 (78.2) | 0 (0) |
| 2008/2009 | 80.0 | 41.4 (51.8) | 13.5 (16.9) | 25.1 (31.3) | 0 (0) | 2.3 | 1.1 (47.1) | 0.5 (20.4) | 0.7 (32.5) | 0 (0) |
| 2009/2010 | 156.8 | 1.7 (1.1) | 36 (23) | 17.2 (11) | 101.8 (64.9) | 9.0 | 0 (0.2) | 1.3 (14.8) | 0.5 (5.4) | 7.2 (79.6) |
| 2010/2011 | 97.8 | 0.1 (0.1) | 61.4 (62.8) | 18.2 (18.6) | 18 (18.4) | 4.0 | 0 (0) | 2.2 (55.2) | 0.5 (13.5) | 1.2 (31.3) |
| 2011/2012 | 107.3 | 0.1 (0.1) | 11.4 (10.7) | 95.7 (89.2) | 0.1 (0.1) | 3.0 | 0 (0) | 0.4 (13.3) | 2.6 (86.7) | 0 (0) |
| 2012/2013 | 75.6 | 0 (0) | 50 (66.1) | 1 (1.4) | 24.6 (32.5) | 3.5 | 0 (0) | 1.8 (51.8) | 0 (0.5) | 1.7 (47.7) |
| Mean(all years) | 113.6 | 7.3 (8.9) | 33.6 (32.8) | 48.6 (38.9) | 36.2 (32.5)a | 4.4 | 0.2 (7.9) | 1.2 (29.5) | 1.3 (36.1) | 2.5 (39.6)a |
| Mean (seasonal yearsb) | 105.0 | 8.4 (7.7) | 33.1 (32.3) | 54.9 (51.4) | 14.2 (15.4)a | 3.5 | 0.2 (6.1) | 1.2 (34) | 1.5 (42.8) | 1.0 (26.3)a |
| R&C | ||||||||||
| 2007/2008 | 140.6 | 0.4 (0.3) | 28.3 (20.1) | 111.8 (79.5) | 0 (0) | 2.1 | 0 (0.4) | 0.5 (24.6) | 1.6 (75) | 0 (0) |
| 2008/2009 | 59.3 | 27.1 (45.8) | 12.7 (21.4) | 19.4 (32.8) | 0 (0) | 1.2 | 0.7 (55) | 0.2 (20.2) | 0.3 (24.8) | 0 (0) |
| 2009/2010 | 137.2 | 1 (0.7) | 33 (24.1) | 13.9 (10.1) | 89.3 (65.1) | 5.5 | 0 (0) | 0.7 (12.5) | 0.2 (3.9) | 4.6 (83.6) |
| 2010/2011 | 87.2 | 0.1 (0.1) | 57.1 (65.5) | 14.1 (16.2) | 15.9 (18.3) | 2.2 | 0 (0) | 1.2 (54.3) | 0.2 (9.8) | 0.8 (35.9) |
| 2011/2012 | 86.4 | 0 (0) | 10.4 (12.1) | 75.9 (87.9) | 0 (0) | 1.3 | 0 (0) | 0.2 (14.9) | 1.1 (85.1) | 0 (0) |
| 2012/2013 | 67.8 | 0 (0) | 46.1 (67.9) | 0.7 (1) | 21 (31) | 2.0 | 0 (0) | 1 (48.2) | 0 (0) | 1.1 (51.8) |
| Mean (all years) | 96.4 | 4.8 (7.8) | 31.3 (35.2) | 39.3 (37.9) | 31.6 (32.8)a | 2.4 | 0.1 (9.2) | 0.6 (29.1) | 0.6 (33.1) | 1.6 (42.8)a |
| Mean (seasonal yearsb) | 88.2 | 5.5 (6) | 30.9 (35.8) | 44.4 (49.2) | 12.3 (15.5)a | 1.8 | 0.1 (7.6) | 0.6 (35.4) | 0.6 (36) | 0.6 (29.2)a |
Number (proportion) presented.
R&C, Respiratory and circulatory diseases.
Estimates for seasons 2009 to 2013.
seasonal years: all years excluding 2009/2010.
3.3. Comparisons of mortality burden between seasonal epidemics and the influenza A(H1N1)pdm09 pandemic period
Table 5 shows comparisons of mortality burden between seasonal epidemics and the influenza A(H1N1)pdm09 pandemic period from this study and previous studies. The all‐cause mortality rate associated with the influenza A(H1N1)pdm09 was comparable to the mortality rate of seasonal influenza during the non‐pandemic seasons (19.9 [CI 10.4‐33.1] vs 17.2 [CI 7.2‐67.5] per 100 000). The mortality impact of the influenza A(H1N1)pdm09 was about double that of seasonal epidemics in non‐pandemic seasons among persons aged <65 years (7.2 [CI 4.4‐10.9] vs 3.5 [CI 0.9‐14.6] per 100 000), but almost equal among older adults (101.8 [CI 48.4‐175.9] vs 105 [CI 46.9‐386.1] per 100 000). However, the differences did not reach statistical significance (P > .05). Persons aged <65 years represented a greater proportion of all deaths during the influenza A(H1N1)pdm09 pandemic period than during the seasonal epidemics (27.0% vs 17.7%, P < .05). A similar mortality burden age shift toward persons <65 years of age was also observed for respiratory and circulatory deaths.
Table 5.
Comparisons of influenza‐associated death rates (per 100 000 persons) by age and death category in this study with previous studies from China
| Modela | Study period | All ages | Age ≥65 y | Age <65 y | % of deaths in age <65 yb | |
|---|---|---|---|---|---|---|
| All deaths: seasonal | ||||||
| China(Beijing, this study) | NB | 2007‐2013 | 17.2 (7.2‐67.5) | 105 (46.9‐386.1) | 3.5 (0.9‐14.6) | 17.7 |
| China(Northern cities)3 | NB | 2003‐2008 | 18 (10.9‐32.7) | 150.8 (66.2‐502.5) | 1.3 | 6.3 |
| China(Southern cities)3 | NB | 2003‐2008 | 11.3 (1.4‐50.4) | 75.4 (11.0‐313.6) | 1.8 | 13.7 |
| China4 | NB | 2004‐2010 | 15.1 (6.3‐48.9) | 145.5 (95.8‐227.3) | 3.7 (1.2‐14.8) | 22.4 |
| China(Guangzhou city)13 | P | 2004‐2006 | 10.6 (0.6‐17.3) | 111.3 (19.4‐203.2) | ‐ | ‐ |
| China(Guangzhou city)5 | NB | 2010‐2012 | 14.7 (12.1‐17.3) | 185.6 (152.5‐218.7) | 2.5 (2‐3) | 34.8 |
| Hong Kong, China14 | P | 1996‐1999 | 16.4 (9.4‐23.3) | 136.1 (83.7‐188.4) | 11.8 (3.8‐20.1) | 21.2 |
| Hong Kong, China13 | P | 2004‐2006 | 13.4 (5.4‐20.9) | 103.7 (40.2‐117.1) | ‐ | ‐ |
| All deaths: 2009 pandemic | ||||||
| China(Beijing, this study) | NB | 2007‐2013 | 19.9 (10.4‐33.1) | 101.8 (48.4‐175.9) | 7.2 (4.4‐10.9) | 27.0 |
| China4 | NB | 2004‐2010 | 13.8 (6.3‐28.1) | 125.8 (59.3‐250.2) | 3.9 (1.7‐8.6) | 26.3 |
| Hong Kong, China15 | P | 1998‐2009 | 1.8 (0‐3.7) | ‐ | ‐ | 8.7 |
| R&C Deaths: Seasonal | ||||||
| China(Beijing, this study) | NB | 2007‐2013 | 13.5 (5.8‐51.7) | 88.2 (41‐313.2) | 1.8 (0.3‐9) | 11.7 |
| China(Northern cities)3 | NB | 2003‐2008 | 12.4 (7.4‐22.2) | 106 (46.7‐344.1) | 0.6 | 4.3 |
| China(Southern cities)3 | NB | 2003‐2008 | 8.8 (1.8‐35.1) | 64.3 (14.0‐243.7) | 0.6 | 6 |
| China4 | NB | 2004‐2010 | 11.1 (5‐32.2) | 117.8 (54.8‐329.3) | 1.7 (0.6‐6.1) | 14.5 |
| China(Guangzhou city)13 | P | 2004‐2006 | 9.9 (2‐17.6) | 104.1 (27.5‐177.5) | ‐ | ‐ |
| China(Guangzhou city)5 | NB | 2010‐2012 | 11.4 (9.4‐13.4) | 146.9 (120.7‐173) | 1.7 (1.4‐2) | 18 |
| Hong Kong, China14 | P | 1996‐1999 | 12.4 (7.7‐17.1) | 102.4 (61.2‐142.7) | 7.3 (3.1‐11.4) | 17.2 |
| Hong Kong, China13 | P | 2004‐2006 | 9.5 (4.5‐14.6) | 78.7 (40.2‐117.1) | ‐ | ‐ |
| R&C deaths: 2009 pandemic | ||||||
| China(Beijing, this study) | NB | 2007‐2013 | 16 (8.6‐26.2) | 89.3 (45.5‐149.3) | 4.6 (2.8‐7.1) | 20.6 |
| China4 | NB | 2004‐2010 | 9.4 (4.6‐18.6) | 94.6 (44.5‐187.1) | 2 (1‐3.8) | 19 |
| Hong Kong, China15 | P | 1998‐2009 | 1.6 (0.4‐2.9) | ‐ | ‐ | 15.7 |
rate (95% confidence interval) presented.
NB denotes negative binomial model; P denotes Poisson model.
% of deaths in persons aged<65 years was a calculation of estimated numbers of influenza.
4. DISCUSSION
This study estimated the mortality burden of seasonal influenza 2007/2008‐2012/2013 and influenza A(H1N1)pdm09 in Beijing based on robust vital statistics and mortality data. We estimated an average of 2375 (CI 1002‐8688) influenza‐associated all‐cause deaths per year, accounting for 3% (CI 2‐4%) of all reported deaths from the Mortality Register and Surveillance System. All‐cause mortality rates associated with influenza A(H1N1)pdm09 and seasonal influenza 2007/2008‐2012/2013 were 19.9 (CI 10.4‐33.1) and 17.2 (CI 7.2‐67.5) per 100 000 persons, respectively.
Our estimates are consistent with previous studies that have shown that the majority of influenza‐associated deaths occurred in persons aged ≥65 years (Table 5).3, 4, 5, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23 Notably, our study observed that influenza B caused the highest burden (20.5 [CI 14.2‐34.9] per 100 000) when influenza B virus predominated in 2007/2008. This mortality pattern is consistent with those described in studies conducted by China CDC and Guangzhou CDC,3, 5 but differs from studies conducted in other regions such as Hong Kong,14 Singapore,16 Thailand,17 United States,18, 19 and New Zealand,23 where the highest death rates were associated with influenza A(H3N2). In addition, the highest mortality burden was not observed in 2011/2012 when influenza B also predominated in Beijing. In 2007/2008, the circulating influenza B viruses originated from the B/Yamagata/16/88 lineage and did not match the vaccine strain, which originated from a different and antigenically distinct lineage of influenza B virus (B/Victoria/2/87).24 The mismatch of the influenza B strain included in the Northern Hemisphere vaccine with the circulating influenza B strain had a negative impact on the effectiveness of the vaccine in the targeted population.25 In contrast, the 2012/2013 influenza vaccine was moderately effective against influenza B.26 Thus, the very low vaccine effectiveness may have led to a higher influenza B infection incidence and mortality in 2007/2008.
Our findings for the all‐age mortality burden of seasonal influenza are comparable with previous studies derived from similar approaches in China (Table 5) 3, 4, 5 and other areas, such as Hong Kong,14 Singapore,16 USA,18 and Mexico.20 For adults aged ≥65 years, however, our estimate is lower than previous estimates made for China overall, 3 northern cities in China, and a southern city in China (105 [46.9‐386.1] vs 145.5 [95.8‐227.3], 150.8 [66.2‐502.5], and 185.6 [152.5‐218.7] per 100 000, respectively).3, 4, 5 One explanation for this lower burden of seasonal influenza mortality among older adults in Beijing may be the higher seasonal influenza vaccine coverage among older adults in Beijing compared with older adults in the rest of China. Since 2007, the Beijing Municipal Government has provided annual seasonal influenza vaccination to older adults free of charge, and the vaccine coverage rate for this population in season 2010/2011 was 43%.9 In most regions of China, older adults must pay for the seasonal influenza vaccine out of pocket, leading to very low vaccine coverage. One study estimated that the vaccine coverage in the Chinese population overall was only 2% in 2009.27 Second, as the largest proportion of influenza‐associated deaths among older adults is among those aged ≥75 years,18 different age distributions across regions may contribute to differences in influenza‐associated mortality burden. Beijing is a large city with a very high population aging rate that has reached the average level of developed countries.28 A higher proportion of adults aged ≥75 years in Beijing may contribute to a higher mortality burden among all adults aged ≥65 years. However, as Beijing is also one of the most developed regions in China, on average, its residents have higher socioeconomic status and better access to health care than residents in other Chinese regions which, in turn, may contribute to a lower mortality burden among older adults.
We estimated that the all‐cause mortality rate associated with influenza A(H1N1)pdm09 was comparable to the mortality impact of seasonal epidemics during the non‐pandemic seasons (19.9 vs 17.2 per 100 000). Although the influenza A(H1N1)pdm09 mortality rate in this study is similar to that estimated by another study in China,4 it is lower than the rate described in Mexico,20 and higher than rates estimated in the United States.29 The case fatality rate of pH1N1 infection during the pandemic was higher in Mexico than in Beijing (1.2% vs 0.6%),30 contributing to the higher influenza A(H1N1)pdm09 mortality rate described in Mexico. Many factors may have contributed to the regional difference in the mortality impact of the pandemic virus between Mexico and Beijing, including epidemic intensity, use of influenza vaccine and antiviral drugs, and healthcare access. Meanwhile, the lower rates described in the United States may have been associated with the higher vaccination coverage for influenza A(H1N1)pdm09 achieved in the United States compared with Beijing (20% vs 13%, respectively).31, 32 Finally, treatment factors may have contributed to different pandemic mortality rates in the United States and Beijing. Due to limited supply of antiviral drugs in Beijing, most patients with mild influenza illness did not take neuraminidase inhibitors within 48 hours of illness onset, increasing the likelihood of severe or fatal outcomes.7 In addition, although approximately 80% of patients with severe illness from influenza A(H1N1)pdm09 in Beijing were treated with neuraminidase inhibitors at some point during the course of their illness, in most cases, treatment was not initiated within 48 hours of illness onset.7
Consistent with studies conducted in other countries, our study found that, compared with seasonal epidemics, there was an “age shift” in age‐specific mortality burden toward persons <65 years of age during the influenza A(H1N1)pdm09 pandemic period.4, 20, 29, 33, 34, 35, 36 A previous meta‐analysis from 27 studies showed that the influenza A(H1N1)pdm09 cumulative incidence varied significantly by age with much higher incidence in younger people.37 In addition, a study comparing seasonal influenza and influenza A(H1N1)pdm09 demonstrated that younger people had 2‐4 times the risk of severe outcomes from influenza A(H1N1)pdm09 than persons of the same ages with seasonal influenza.38 These findings suggest that prevention and control measures during pandemics may need to target younger adults who are not considered high risk during seasonal epidemics.
This study has several limitations. First, although underreporting of deaths in Beijing is low when compared to China overall (4‐7% vs 17%),39, 40, 41 it is possible that underreporting still led to an underestimation of influenza mortality. Second, because Beijing does not have access to local respiratory syncytial virus (RSV) virology data, we were unable to control for RSV co‐circulation. As RSV is associated with substantial mortality,18 not accounting for RSV may have inflated our influenza‐related mortality burden estimate. While it is possible that our estimates might be an overestimate of influenza‐associated deaths, the inclusion of viral surveillance terms significantly reduces the chance of overestimation. Prior to including these terms, we evaluated the surveillance data to ensure that it was robust and did not show instances of bias due to few specimens being collected. We also compared our viral surveillance data to the national system which showed a similar pattern in influenza virus circulation for the northern region of China. Third, we did not have the sample size available to obtain reliable estimates within more refined age categories. There were also several factors that may contribute to deaths in Beijing that we were unable to include in our model, such as air quality, which is particularly poor in Beijing especially when compared to cities outside of China. Finally, our estimates were based on an ecological study design, and therefore, we cannot confirm a causal relationship between influenza activity and our estimates of mortality burden.
5. CONCLUSIONS
Our study demonstrates a substantial influenza‐related mortality burden in Beijing, China from 2007/2008 to 2012/2013, especially among older adults. Influenza B caused highest mortality when influenza B virus was the predominant circulating virus in 2007/2008. Although this study did not find any increase in all‐age influenza‐associated mortality during the influenza A(H1N1)pdm09 pandemic period, the mortality burden in 2009/2010 increased among persons aged <65 years. These findings inform local influenza prevention and control strategies. First, the results support policies that give priority to older adults for seasonal influenza vaccination as they have done since 2007, and efforts to identify strategies to increase vaccine coverage in this population at highest risk for seasonal influenza‐related mortality. Second, the increased influenza‐associated mortality rates among persons <65 years of age during the influenza A(H1N1)pdm09 pandemic period suggest that the most effective pandemic vaccination strategies may differ from those used for seasonal influenza; it is important to identify and vaccinate populations at highest risk for morbidity and mortality during each pandemic.
CONFLICT OF INTEREST
The authors declare that they have no competing interests.
AUTHORS’ CONTRIBUTION
WS, WZ, YP, and WQ designed the study; WS and SJ performed the data collection; WQ and WZ coordinated and supervised the data collection; WS analyzed the data; WS, YP, CG, SY, and AI participated in the interpretation of data; WS drafted the initial manuscript; WS, CG, SY, and AI revised the manuscript. All authors have read and approved the final version of the manuscript.
Supporting information
ACKNOWLEDGEMENTS
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the United States Centers for Disease Control and Prevention.
Wu S, Wei Z, Greene CM, et al. Mortality burden from seasonal influenza and 2009 H1N1 pandemic influenza in Beijing, China, 2007‐2013. Influenza Other Respi Viruses. 2018;12:88–97. https://doi.org/10.1111/irv.12515
Funding information
This work was supported by Expanding the Use of Seasonal Influenza Vaccine in Public Health Programs in China (1U51IP000819‐01), Beijing Science and Technology Planning Project (D141100003114002), The Capital Health Research and Development of Special (2014‐1‐1011), Beijing Talents Fund (2014000021223ZK36) and Beijing Health System High Level Health Technology Talent Cultivation Plan (2013‐3‐098). APC for this article is funded by World Health Organization (WHO).
Shuangsheng Wu and Zaihua Wei contributed equally to this article.
The copyright line for this article was changed on 25 January 2018 after original online publication
[Correction added on 25 January 2018, after first online publication: Funding information has been updated.]
REFERENCES
- 1. World Health Organization . Influenza. [cited 18 October 2016]. Available at http://www.who.int/biologicals/vaccines/influenza/en/
- 2. Thompson WW, Ridenhour BL, Barile JP, Shay DK. Time‐series analyses of count data to estimate the burden of seasonal infectious diseases. Epidemiology. 2012;23:839‐842. discussion 843‐4. [DOI] [PubMed] [Google Scholar]
- 3. Feng L, Shay DK, Jiang Y, et al. Influenza‐associated mortality in temperate and subtropical Chinese cities, 2003‐2008. Bull World Health Organ. 2012;90:279‐288B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Yu H, Feng L, Viboud CG, et al. Regional variation in mortality impact of the 2009 A(H1N1) influenza pandemic in China. Influenza Other Respir Viruses. 2013;7:1350‐1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wang H, Fu C, Li K, et al. Influenza associated mortality in Southern China, 2010‐2012. Vaccine. 2014;32:973‐978. [DOI] [PubMed] [Google Scholar]
- 6. Yu H, Alonso WJ, Feng L, et al. Characterization of regional influenza seasonality patterns in China and implications for vaccination strategies: spatio‐temporal modeling of surveillance data. PLoS Med. 2013;10:e1001552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Yang P, Deng Y, Pang X, et al. Severe, critical and fatal cases of 2009 H1N1 influenza in China. J Infect. 2010;61:277‐283. [DOI] [PubMed] [Google Scholar]
- 8. Wang X, Yang P, Seale H, et al. Estimates of the true number of cases of pandemic (H1N1) 2009, Beijing, China. Emerg Infect Dis. 2010;16:1786‐1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wu S, Yang P, Li H, Ma C, Zhang Y, Wang Q. Influenza vaccination coverage rates among adults before and after the 2009 influenza pandemic and the reasons for non‐vaccination in Beijing, China: a cross‐sectional study. BMC Public Health. 2013;8:636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Beijing Bureau of Statistics . Release on Major Figures of the 2010 National Population Census in Beijing, China. [cited 18 October 2016]. Available at http://www.bjstats.gov.cn/tjnj/rkpc-2010/indexch.htm.
- 11. Wu S, Yang P, Shi W, et al. Influenza‐like illness and influenza virologic surveillance in Beijing, 2007‐2012. Int J Virol. 2013;20:11‐16. (Article in Chinese) [Google Scholar]
- 12. Yang P, Duan W, Lv M, et al. Review of an influenza surveillance system, Beijing, People's Republic of China. Emerg Infect Dis. 2009;15:1603‐1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Yang L, Ma S, Chen PY, et al. Influenza associated mortality in the subtropics and tropics: results from three Asian cities. Vaccine. 2011;29:8909‐8914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wu P, Presanis AM, Bond HS, Lau EHY, Fang VJ, Cowling BJ. A joint analysis of influenza‐associated hospitalizations and mortality in Hong Kong, 1998‐2013. Sci Rep. 2017;7:929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Yang L, Chan KP, Cowling BJ, et al. Excess mortality associated with the 2009 pandemic of influenza A(H1N1) in Hong Kong. Epidemiol Infect. 2012;140:1542‐1550. [DOI] [PubMed] [Google Scholar]
- 16. Chow A, Ma S, Ling AE, Chew SK. Influenza‐associated deaths in tropical Singapore. Emerg Infect Dis. 2006;12:114‐121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Aungkulanon S. Influenza‐associated mortality in Thailand, 2006‐2011. Influenza Other Respir Viruses. 2015;6:298‐304. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Matias G, Taylor R, Haguinet F, Schuck‐Paim C, Lustig R, Shinde V. Estimates of mortality attributable to influenza and RSV in the United States during 1997‐2009 by influenza type or subtype, age, cause of death, and risk status. Influenza Other Respir Viruses. 2014;8:507‐515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Thompson WW, Weintraub E, Dhankhar P, et al. Estimates of US influenza‐associated deaths made using four different methods. Influenza Other Respir Viruses. 2009;3:37‐49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Charu V, Chowell G, Palacio Mejia LS, et al. Mortality burden of the A/H1N1 pandemic in Mexico: a comparison of deaths and years of life lost to seasonal influenza. Clin Infect Dis. 2011;53:985‐993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Nielsen J, Mazick A, Glismann S, Mølbak K. Excess mortality related to seasonal influenza and extreme temperatures in Denmark, 1994‐2010. BMC Infect Dis. 2011;16:350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Newall AT, Wood JG, Macintyre CR. Influenza‐related hospitalisation and death in Australians aged 50 years and older. Vaccine. 2008;26:2135‐2141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kessaram T, Stanley J, Baker MG. Estimating influenza‐associated mortality in New Zealand from 1990 to 2008. Influenza Other Respir Viruses. 2015;9:14‐19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Yang P, Wang Q, Shi W, et al. Pre‐warning analysis of influenza surveillance in Beijing, 2007‐2008. Chin J Dis Control Prev. 2010;14:108‐111. [Article in Chinese] [Google Scholar]
- 25. Mook P, Ellis J, Watson JM, et al. Public health implications of influenza B outbreaks in closed settings in the United Kingdom in the 2007/08 influenza season. Euro Surveill. 2008;13 pii: 18986. [PubMed] [Google Scholar]
- 26. Rondy M, Launay O, Puig‐Barberà J, et al. 2012/13 influenza vaccine effectiveness against hospitalised influenza A(H1N1)pdm09, A(H3N2) and B: estimates from a European network of hospitals. Euro Surveill. 2015;20 pii: 21011. [DOI] [PubMed] [Google Scholar]
- 27. Feng L, Mounts AW, Feng Y, et al. Seasonal influenza vaccine supply and target vaccinated population in China, 2004‐2009. Vaccine. 2010;28:6778‐6782. [DOI] [PubMed] [Google Scholar]
- 28. Lin B. Study of the problem and strategic choice of dealing with population aging in Beijing. Soc Sci Beijing. 2011;1:9‐13. [Article in Chinese] [Google Scholar]
- 29. Charu V, Simonsen L, Lustig R, Steiner C, Viboud C. Mortality burden of the 2009‐10 influenza pandemic in the United States: improving the timeliness of influenza severity estimates using inpatient mortality records. Influenza Other Respir Viruses. 2013;7:863‐871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Chowell G, Echevarría‐Zuno S, Viboud C, et al. Characterizing the epidemiology of the 2009 influenza A/H1N1 pandemic in Mexico. PLoS Med. 2011;8:e1000436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Pang XH, Liu DL, Lu L, et al. Factors associated with immunization of novel influenza A (H1N1) vaccine in Beijing, 2009. Zhonghua Liu Xing Bing Xue Za Zhi. 2010;31:588‐590. [Article in Chinese] [PubMed] [Google Scholar]
- 32. Reed C, Katz JM, Hancock K, Balish A, Fry AM, H1N1 Serosurvey Working Group . Prevalence of seropositivity to pandemic influenza A/H1N1 virus in the United States following the 2009 pandemic. PLoS One. 2012;7:e48187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lemaitre M, Carrat F, Rey G, Miller M, Simonsen L, Viboud C. Mortality burden of the 2009 A/H1N1 influenza pandemic in France: comparison to seasonal influenza and the A/H3N2 pandemic. PLoS One. 2012;7:e45051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hardelid P, Andrews N, Pebody R. Excess mortality monitoring in England and Wales during the influenza A(H1N1) 2009 pandemic. Epidemiol Infect. 2011;139:1431‐1439. [DOI] [PubMed] [Google Scholar]
- 35. Wijngaard CC, Asten LV, Koopmans MP. Comparing pandemic to seasonal influenza mortality: moderate impact overall but high mortality in young children. PLoS One. 2012;7:e31197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Muscatello DJ, Newall AT, Dwyer DE, Macintyre CR. Mortality attributable to seasonal and pandemic influenza, Australia, 2003 to 2009, using a novel time series smoothing approach. PLoS One. 2013;8:e64734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Van Kerkhove MD, Hirve S, Koukounari A, Mounts AW, H1N1pdm serology working group . Estimating age‐specific cumulative incidence for the 2009 influenza pandemic: a meta‐analysis of A(H1N1)pdm09 serological studies from 19 countries. Influenza Other Respir Viruses. 2013;7:872‐886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Reed C, Chaves SS, Perez A, et al. Complications among adults hospitalized with influenza: a comparison of seasonal influenza and the 2009 H1N1 pandemic. Clin Infect Dis. 2014;59:166‐174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Zhou YL, Pan JH, Huang H, et al. Survey on underreporting of mortality surveillance from 2009 to 2011 in Dongcheng District of Beijing City, China. Chronic Pathemathol J. 2013;14:187‐189. [Article in Chinese] [Google Scholar]
- 40. Xie CX, Wang XY, Ding XD, et al. Survey on underreporting of mortality surveillance from 2007 to 2019 in Changping District of Beijing City, China. Chin J Prev Chronic Dis. 2012;20:145. [Article in Chinese] [Google Scholar]
- 41. Wang L, Wang LJ, Cai Y, Ma LM, Zhou MG. Analysis of under‐reporting of mortality surveillance from 2006 to 2008 in China. Zhonghua Yu Fang Yi Xue Za Zhi. 2011;45:1061‐1064. [Article in Chinese] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


