Abstract
Myalgic encephalomyelitis (ME) often also called chronic fatigue syndrome (ME/CFS) is a common, debilitating, disease of unknown origin. Although a subject of controversy and a considerable scientific literature, we think that a solid understanding of ME/CFS pathogenesis is emerging. In this study, we compiled recent findings and placed them in the context of the clinical picture and natural history of the disease. A pattern emerged, giving rise to an explanatory model. ME/CFS often starts after or during an infection. A logical explanation is that the infection initiates an autoreactive process, which affects several functions, including brain and energy metabolism. According to our model for ME/CFS pathogenesis, patients with a genetic predisposition and dysbiosis experience a gradual development of B cell clones prone to autoreactivity. Under normal circumstances these B cell offsprings would have led to tolerance. Subsequent exogenous microbial exposition (triggering) can lead to comorbidities such as fibromyalgia, thyroid disorder, and orthostatic hypotension. A decisive infectious trigger may then lead to immunization against autoantigens involved in aerobic energy production and/or hormone receptors and ion channel proteins, producing postexertional malaise and ME/CFS, affecting both muscle and brain. In principle, cloning and sequencing of immunoglobulin variable domains could reveal the evolution of pathogenic clones. Although evidence consistent with the model accumulated in recent years, there are several missing links in it. Hopefully, the hypothesis generates testable propositions that can augment the understanding of the pathogenesis of ME/CFS.
Keywords: chronic fatigue syndrome, myalgic encephalomyelitis, irritable bowel syndrome, postexertional malaise, autoimmunity
Introduction
ME/CFS is a common disease of unknown etiology characterized by postexertional malaise (PEM; a type of fatigability), cognitive disturbance, unrefreshing sleep, autonomic nerve dysfunction, and a few characteristic comorbidities, see, e.g., Ref. (1–3). It often starts with an infection and has a strong tendency to remain a chronic condition.
ME/CFS diagnostic criteria have gradually become more stringent, see, e.g., Ref. (2–7). These are based on somatic, often self-reported symptoms (8, 9). Although often used interchangeably, studies using the “CDC,” (also called the “Fukuda”) criteria (5) mainly use the term “CFS,” while those using the “Canada” (3) or International consensus (2) criteria use the term “ME.” This creates an ambiguity, which may explain some contradicting results. There are so far no specific laboratory tests (10) for ME/CFS diagnosis. Recently, a committee recommended a new name for ME/CFS, systemic exhaustion intolerance disease (SEID) (11, 12) with diagnostic criteria that emphasize PEM as the central ME/CFS symptom (13). The disease entity ME/CFS is not uncontroversial. Like many times before in medical history, psychiatric and somatic explanations compete with each other. A recent critical review, which emphasized psychiatric aspects, stated that “there is no convincing pathogenesis model for CFS” (14). However, in this review, we forward that evidence for a somatic origin of the disease is accumulating.
From a research perspective it is important that patients are diagnosed using strict criteria. A thorough clinical examination is necessary. It does not matter how sophisticated the analyses are in a study if patient selection is ambiguous. In the case of “fatigue” it is important to distinguish ME/CFS fatigue from other types of fatigue, such as burnout syndrome and depression, see, e.g., Ref. (15). In ME/CFS, repetition of a physical or mental exertion can reveal objective evidence of fatigability. This exertion-elicited fatigue, PEM, is required for the diagnosis of ME/CFS using the Canadian criteria (3), the International consensus (2), and the SEID (12), but not using CDC (5) criteria. Although the term “ME/CFS,” encompassing both “ME” and “CFS,” has a built-in ambiguity it covers much of the current studies and is operationally judged as the best available concept. Fatigue similar to PEM also occurs in Sjögren’s syndrome (SS), primary biliary cholangitis (also named primary biliary cirrhosis) (PBC), and systemic lupus erythematosus (SLE). The relation of ME/CFS to the similar condition Gulf War Illness (GWI) is uncertain, see, e.g., Ref. (16). However, a recent study describes a laboratory-based distinction between the two illnesses (17).
Recent ME/CFS reports brought optimism (18). National Institutes of Health in the US announced that it will prioritize the disease. Cornerstones are studies on PEM (12, 19) and effects of immunosuppressive treatment (20–22) although not substantiated in a phase III trial.
There are several partly competing explanatory models for ME/CFS, for example; autoimmunity, chronic infection, energy metabolic defect, imbalance in autonomous nervous system and/or hormones, and psychosomatic dysfunction. In this laboratory-oriented review, we present an overview of recent findings and attempt to bring a substantial portion of ME/CFS symptoms and its disease history into one explanatory model. The model draws analogies from more established autoimmune diseases (even if much remains to be understood in these too) is based on clinical experience and on recent immunometabolic results. Clues for further research are given in Table 1 and as separate statements in the text.
Table 1.
Some outstanding questions regarding ME/CFS, which are addressed in this conceptual review.
| The hypothesis gives rise to several verifiable general questions |
|---|
|
Trying to Place it all Under One Umbrella: a Hypothesis for ME/CFS Pathogenesis
We propose a pathogenetic model reminiscent of current thinking on the pathogenesis of autoimmunity.
A genetically predisposed person (A) is exposed to successive infections (B), e.g., in the gastrointestinal tract—manifested as dysbiosis or irritable bowel syndrome (IBS)—or in the airways, with microbes carrying epitopes mimicking human self-epitopes, or microbes which activate autoreactive B cells to produce the so-called natural antibodies with non-rearranged germ line immunoglobulin genes. Such autoreactive B cells may be deleted or persist in a state of anergy (C). A proportion of these B cells remain in spleen and lymph nodes as memory IgM+, IgA+, or IgG+ B cells (D). Individuals differ in time and extent of encounters with autoreactivity eliciting microbes. Some encounters are here postulated to give rise to autoantibodies (E) against key enzymes in energy metabolism hence causing a defective aerobic energy metabolism and PEM, the central symptom of ME/CFS, others to fibromyalgia (FM), yet others to postural orthostatic tachycardia syndrome (POTS) or other comorbidities. If the autoimmunization events are independent of each other they can occur in any order. If there are cooperativity effects they may follow a rather specific order (F). The upper case letters refer to stages in Figures 1 and 2.
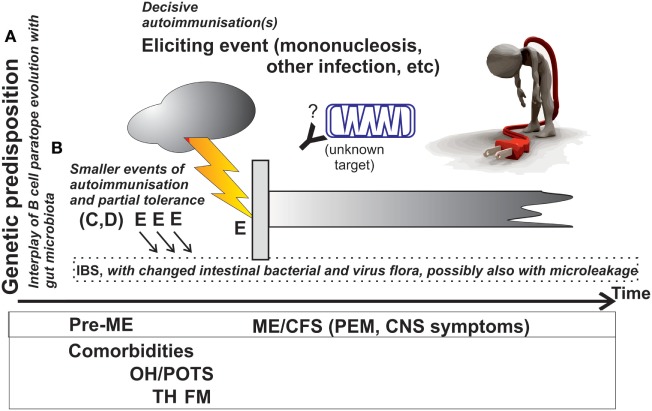
Figure 1.
Approximate course of events during which ME/CFS develops, and overview of the explanatory model. The postulated immunometabolic energy block is shown as an antibody and a mitochondrion. Italicized text refers to the explanatory model presented under “Trying to place it all under one umbrella.” Abbreviations are explained in the text.
Figure 2.
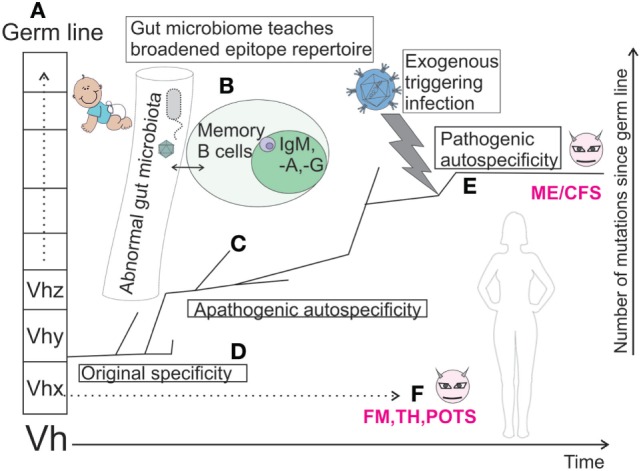
Mutational fate of a hypothetic germ line immunoglobulin heavy chain sequence (Vhy) in successive B cell clones, which gradually expand their paratope diversity in interplay with gut microbiota, T cells, and dendritic cells. If there is a chronic antigen stimulation, sequences more or less close to germ line sequence may be selected. Resulting B cells are stored as memory cells in germinal centers of gut-associated lymph nodes. Some of the developmental branches end due to clonal anergy or deletion (tolerization). Others are postulated to descend along a path to autospecificity due to an abnormality in gut commensal spectrum. An exogenous, triggering, antigenic stimulation (e.g., infection), eventually leads to overt pathogenic autospecificity (“evil” B cell clones, magenta) and ME/CFS. Similar fates of other B cell clones, which eventually turn autopathic and give comorbidities, are indicated under “F.” Characters A–F in bold refer to the stages mentioned under “Trying to place it under one umbrella.” This figure was inspired by work on the autoreactive clone VH4-34 (23, 24).
Thus, the basic property of ME/CFS patients would be a defect in tolerance coupled with a chance exposure to microbes carrying relevant mimicking autoantigen epitopes.
The italicized text of Figure 1 shows a hypothetical explanation of the events behind ME/CFS. A known function of microbes in the gut is to train, from within, the immune system to recognize and react correctly to microbes (including bacteria and viruses), which come from the outside (25–29). The correct reaction includes, among other things, anergy and unresponsiveness to microbial antigens that cross-react with self-antigens. It is known that ME/CFS patients often have IBS (30–32). In this IBS there is also a modified gut flora (33, 34). A less symptomatic gut dysbiosis may also occur (33, 35). In addition, there is also occasional epithelial barrier leakage of gut microbes. It is reasonable to assume that the innate mucosal immunity defenses have been breached or that peripheral tolerance maintenance (training function) of the gut flora has been disturbed. Normally, the mucosal immune system must maintain tolerance to harmless foreign antigens including food and commensal microbes. Presentation of antigens at mucosae often leads to tolerance (36). When there is microleakage tolerance may not function properly leading to loss of checkpoints that normally prevent development of autoreactivity (37–42). The profile of B cell subpopulations is different in ME/CFS compared with controls (43). A factor behind that could be new memory B cells with autoreactivity, which normally would be sorted out, arising and persisting. When the body is exposed to a new infection, these B cells could produce antibodies which react both to microbe and autoantigen. Autoantibodies and T cells that recognize self-peptides can damage cells which carry autoantigens. This is the so-called mimicry (antigen similarity) theory behind autoimmune disease (44). Part of the explanation for ME/CFS would then be the disturbed gut flora and microleakage from the gut. At the left side of Figure 1 is written “Genetic predisposition.” This is compatible with the increased frequency of ME/CFS in certain families. Like for many other common diseases ME/CFS could depend on both inheritance and environment.
If this hypothesis is correct, a tendency for autoreactivity would arise gradually, via a changed gut flora and microleakage from the gut. After a decisive immunization event autoimmunity leading to ME/CFS would arise, as shown in Figure 1. The prerequisites for autoimmunity would arise gradually because B cells with a tendency for autoimmunity would arise after recurring microleakage across the mucosal barrier of the gastrointestinal tract inducing a state of chronic inflammation. The normal contact between gut microbes and immune system occurs at the gut/mucosa interphase. Central tolerance often develops by elimination of autoreactive B cells. However, a proportion of autoreactive B cells remain which are kept unresponsive (anergic). When there is microleakage, the mucosal barrier is bypassed and tolerance may not be maintained. Autoreactive B cells can then be activated and differentiate to autopathic B cells.
The frequency of IBS, alterations in microbiome and extent of microleakage should be further studied in ME/CFS. Attempts to find autoreactive B cells to find their origin and their evolution should be made. Maybe it is possible to trace how they evolved by systematic sequencing of their antigen-binding structures (paratopes and idiotypes), from germ line to anti-gut microbe to autoimmune clone?
Genetic Predisposition and Premorbid Phenotype
There is evidence for a strong genetic component in some autoimmune diseases, such as complement component deficiencies in SLE which may lead to reduced self-antigen elimination. Likewise, in ME/CFS, autoimmune diseases, for example, thyroid disease (45), SS (46), and SLE (47), often occur among relatives and sometimes among the patients themselves.
Presence of an HLA association is a hallmark of many autoimmune diseases. It indicates an aberrant immune presentation to either cytotoxic T cells (HLA Class I) or T helper cells (HLA Class II) which predisposes for autoimmunity. One study found an overrepresentation of HLA Class II DQA1*01, with an odds ratio of 1.93 (48).
Specific cytokine gene polymorphisms were observed; an increase of one, for TNFα, and a decrease of one, for IFNγ, were found in CFS (49).
Recent genome-wide association studies showed an increased frequency in ME/CFS of single-nucleotide polymorphisms (SNPs), some isolated, some concentrated to three gene regions: microtubule associated protein 7, CCDC7 (coiled-coil domain containing 7) and a T-cell receptor alpha chain gene (50). The latter may confine an increased tendency to autoimmunity. The comorbidity with autoimmune disease or disease having an increased prevalence of autoantibodies, e.g., FM (51–57), IBS (58–63), POTS (64), and hypothyroidism (45, 51, 55, 65–67), also indicate a tendency for autoimmunity in ME/CFS patients (further detailed in the section on autoreactivie B cell clones and autoantibodies, including Table 4). SS (46) and SLE (47) often occur among relatives and sometimes among the patients themselves.
Table 4.
Occurrence of autoantibodies in ME/CFS and some of its comorbidities.a
| Disease (frequency in ME/CFS), reference | Antigen to which autoantibody occurs more often than in controls | |||||
|---|---|---|---|---|---|---|
| Phospholipid | Carbohydrate | Hormone | Hormone receptor | Ion channel protein | Other protein | |
| ME/CFS | Cardiolipin (54) | Ganglioside (54) | β-Adrenergic and muscarinic cholinergic (93) | HSP60 (94) | ||
| Fibromyalgia (35–73%) (95) | Potassium channel transporter (96, 97) | |||||
| (hypo)Thyroidism (thyroiditis by cytology, 40%, wide definition of chronic fatigue) (98) | Thyroperoxidase (45) | Thyroid-stimulating hormone (99) | ||||
| Postural orthostatic tachycardia syndrome and/or orthostatic hypotension (27%) (100) | Acetylcholine (101) | Calcium channel transporter (101) | ||||
| Irritable bowel syndrome (35–90%) (30–32) | Vinculin and cytolethal distending toxin B (58) | |||||
aThe list is not complete. More studies are needed to obtain better statistics. Some of these autoantibodies have the potential to become diagnostic biomarkers. Abbreviations are explained in the text.
IgG3 and mannose binding lectin deficiency were more common among ME/CFS patients than in controls (102, 103). IgG subclass deficiency is more frequent in ME/CFS than in controls (104, 105). Such deficiencies could increase the risk of recurrent infections.
In a genetic study concentrating on hormone and hormone receptor genes, certain TRPM3 and CHRNA2 SNPs were found to be more common in ME/CFS (106–108).
Are There Also Epigenetic Changes in ME/CFS?
DNA modification (methylation) of promoters of some genes associated with immune cell regulation; glucocorticoid receptors, ATPase and IL6 receptor, respectively, was reported to differ between ME/CFS and controls (109). DNA methylation depends on the one-carbon metabolism, where ME/CFS changes have been recorded. Although the reason for such hypomethylation can only be speculated upon, it is interesting that the combined action of the vitamins B12 and folic acid play a fundamental role in providing methyl groups to hundreds of substrates in various elementary cell processes (see the section “can autoimmunity explain energy metabolic disturbances and PEM”).
Gene Expression in ME/CFS
In a recent RNA-seq study, there were no specific RNAs expressed in ME/CFS compared with healthy controls and other chronic diseases (110). In another expression study, prominent differentially expressed genes were EIF4G1, EIF2B4, MRPL23, which control RNA translation, in cytoplasm and/or mitochondria (111). A differential expression of genes crucial for T-cell activation and innate response to viruses was also described (111–114) in CFS.
A novel angle was the report that the pattern in cerebrospinal fluid (CSF) and blood of another kind of RNA, the small regulatory RNAs, differed between ME/CFS, GWI, and controls (17, 115). Another pattern was found in FM (116). The pathophysiological roles of the small regulatory RNAs are still uncertain, but the findings indicate additional levels of pathophysiological regulation, which also could provide diagnostically useful biomarkers.
A prerequisite for calling a disease chronic is duration of at least 6 months. This often means that one has not been able to take samples during the period when the disease commenced. A common situation is that the patients remember that ME/CFS started with an infection, often infectious mononucleosis (IM), or a general virosis-like disease (117). When the acute infection with fever, myalgia, and swollen lymph nodes and/or cough subsides, a malaise and fatigability remains. According to the literature approximately 70% of ME/CFS cases start rather abruptly in this way. Others have a more gradual debut. The natural history of the disease should be studied systematically.
In a few cases, ME/CFS appear epidemically, with several cases being derived from a common index case. Even if epidemic outbreaks are uncommon it indicates that the disease might be contagious. Further epidemiological studies are needed.
Many Different Infections have been Observed at the Outset of ME/CFS Like Disease
There is abundant evidence for infection as a trigger of chronic fatigue in a more general sense (often manifested as fatigability) (68, 72–74, 77–79, 82, 84, 118–128) (Table 2). But negative evidence also exists (129, 130). Some of this evidence is inconclusive (131, 132). Whether all these instances of postinfectious fatigability have identical properties (e.g., Do they fulfill criteria for PEM?; For ME/CFS?; How chronic are they?; etc.) should be systematically investigated. These infections can be traced in the patient history, by direct detection of the microbe(s) (133), or by detection of antibodies to the microbe(s) (94, 119, 133–146), see, however, Ref. (147).
Table 2.
Long-standing fatigue, or fatigability, after an infection.
| Microbe | Infection | Diagnostic term | Approximate % of fatigued post infection | Reference |
|---|---|---|---|---|
| Epstein–Barr virus | Infectious mononucleosis | Postviral fatigue | 11% (6 months); 4% (12 months) | (68, 69) |
| Coxiella burnetii | Q fever | Post Q fever fatigue | 10–20% (6–12 months) | (69–71) |
| Giardia lamblia | Giardiasis | Post Giardia fatigue | <1% (12 months) | (72, 73) |
| Ross River virus | Ross River virus infection | Post Ross River fatigue | 11% (6 months); 9% (12 months) | (69, 74) |
| Chikungunya virus | Chikungunya virus infection | Post Chikungunya fatigue (often together with arthralgia) | 20% over background (≥12 months) | (75, 76) |
| West Nile virus | West Nile virus infection | Post West Nile fatigue | 31% (6 months) | (77–79) |
| Dengue virus | Dengue fever | Post Dengue fatigue | 8% (2 months) | (80, 81) |
| Ebola virus | Ebola hemorrhagic fever | Post Ebola fatigue | Not clear, at least 10% (6 months) | (82, 83) |
| SARS corona virus | Severe acute respiratory syndrome | Post SARS syndrome | Approximately 22/400 = 6% (≥12 months) | (84) |
How often does it happen that spouses are afflicted? This would advocate a transmissible factor rather than inheritance.
Epstein–Barr virus (EBV) seems to be a frequent trigger of ME/CFS (also referred to as “postviral fatigue”). Glandular fever (127), also called IM, is most frequently caused by EBV. A reasonably specific laboratory test for IM (the “Mono” test) is based on heterophilic antibodies, which bind to carbohydrate antigens on non-human erythrocytes (148–150). If infectious triggers of ME/CFS are investigated, a positive Mono test provides an often recorded marker. Other infections are often not diagnosed as objectively. EBV belongs to the herpes virus family. It can infect and remain latent in B cells. At primary infection, EBV triggers massive activation of multiple B cell clones each secreting monoclonal antibodies which are coded by immunoglobulin heavy and light (IGH and IGL) chain genes with unique variable [immunoglobulin heavy chain variable (IGHV) and IGLV] genes, with the so-called complementarity-determining regions. The result is a polyclonal B cell stimulation, with massive release of natural antibodies, including autoreactive antibodies. Besides B cell growth stimulation, EBV stimulates production of EBI3, one of two chains of the tolerance-control heterodimer cytokines IL27 and IL35 (151). Thus, EBV is deeply influencing immune functions. EBV is also coding for antigens with highly repetitive structure (e.g., Gly–Ala–Gly–Ala repeats in EBNA1). This may be a source for antigenic mimicry and development of autoreactivity. Both the B cell growth stimulation and such antigenic mimicry make EBV a prime suspect of inducing autoreactivity. There is a correlation between occurrence of IM and the autoimmune diseases MS (152–154) and SLE (155–158). How EBV is involved, be it frequent reactivations of latent EBV or defects in the T cell and NK cell surveillance mechanisms against the virus, is not clear, but the presence of EBV, and the immune response to it, should be compared in ME/CFS, MS, and SLE, see Ref. (134).
Summarizing, EBV is especially interesting as a facilitator of autoreactivity. Some autoantibodies may have an origin in a mimicry between EBV antigen and self-antigens. EBV is a ubiquitous virus. EBV can stimulate thousands of B cells to produce thousands of different antibodies, each with its own unique antigen-binding site. It often occurs as an eliciting factor triggering ME/CFS, in this case referred to as “postviral fatigue.” As mentioned, it stimulates growth of a wide variety of B cells, and it has viral proteins that can give rise to autoantibodies (159, 160).
Transmissibility is a microbial property. Most ME/CFS cases are sporadic (118). However, there are a few recorded outbreaks, where healthy ME/CFS patient contacts developed symptoms of the disease (118, 161), forming ME/CFS outbreaks in ME/CFS, indicating a transmissible agent.
Many observations support that a condition similar to ME/CFS occurs in approximately 10% of those who had Q fever, an infection with the bacterium Coxiella burnetii (69, 70, 74) which often occurs in outbreaks. Q fever is unevenly spread throughout the world. ME/CFS is more widespread. Q fever is therefore unlikely to be a common cause of ME/CFS, globally.
A chronic postinfectious fatigue/fatigability reminiscent of PEM occurs after a number of life-threatening virus infections (Table 2). There is not much antigenic similarity between these infective agents. Many infections which fundamentally challenge or reorganize the immune system give rise to a persistent, perhaps autoimmune, malfunctioning state.
Note that the number of ME/CFS cases triggered by severe zoonotic infections such as Ebola must be very small, on a global scale. Besides IM, mild respiratory infections like those caused by mycoplasma (162–168) and chlamydia (164, 169, 170), or general infections due to parvovirus B19 (136, 171) and herpes 6 and 7 (133), have been mentioned, although the diagnostic evidence is not strong.
Although much remains unclear before the role of infection in autoimmunity is understood, there are diseases where a known antigenic challenge triggers autoimmune disease, an infection (172) or a vaccination. Surprisingly often it is the brain that is the target for this autoimmunity (Table 3).
Table 3.
Autoimmune syndromes secondary to infections–association/hypothetical relationship.
| Disease | Microbe | Type of microbe | Mimicry (likely structure) | Reference |
|---|---|---|---|---|
| Postinfectious encephalitis | Measles, Varicella-zoster, etc. | Virus | Anti-myelin oligodendrocyte glycoprotein and unknown antigens | (85, 86) |
| Guillain–Barré syndrome | Campylobacter (primarily) and Zika virus | Bacterium and virus | Gangliosides; unknown antigen | (87, 88) |
| “Nodding disease” | Onchocerca volvulus | Worm | Unknown antigen | (89) |
| Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infection (PANDAS) | Streptococcus infections, i.e., strep throat or scarlet fever | Bacterium | Carbohydrate antigens? | (90) |
| Multiple sclerosis | Epstein–Barr virus and other pathogens | Virus and bacteria | Myelin basic protein, proteolipid protein, and myelin oligodendrocyte glycoprotein | (91, 92) |
In addition to commonly known microbes (virus, bacteria, and protozoa), a large number of new ones have been discovered during the last 5 years (171, 173–179). Many of them are viruses which do not cause any known disease. We need to keep an eye on these microbes. Maybe there are some among them which can precipitate ME/CFS?
In these examples of infection elicited autoimmunity, the microbial antigen mimics epitope(s) on human cells. Such microbial epitopes may either be small molecules, like lipids, or added to proteins posttranslationally (172), randomly similar sequences, repetitive sequence motifs, or highly conserved antigenic structures.
An example of the former mechanism (posttranslational antigenic modification) is PBC. The antibodies are directed against a small fatty acid molecule, lipoic acid, added posttranslationally to a protein in the pyruvate dehydrogenase (PDH) enzyme complex. PDH is part of the energy producing machinery at the surface of mitochondria (180, 181), and governs the transition from glycolysis (anaerobic energy metabolism) to the tricarboxylic acid cycle and respiratory chain (aerobic energy metabolism), occurring inside mitochondria. Lipoylation is a posttranslational modification, which also occurs in a few bacteria, such as Novosphingobium (182). Gut infection with Novosphingobium is a possible cause of PBC. The PBC patients have a PEM reminiscent of the PEM of ME/CFS. Likewise, periodontal infection with Aggregatibacter, which citrullinates its own as well as human proteins, may provide the final trigger for rheumatoid arthritis (183).
An example of the latter mechanism (conserved epitopes) is a family of highly conserved proteins, which are present in both humans and microbes, called “heat shock proteins” (HSP). Antibodies against HSPs occur in many often studied autoimmune diseases, for example, MS and SLE (94, 184–188). We found a higher frequency and levels of antibodies against a specific portion of HSP60 in ME/CFS patients (94). Even though HSP60 is a mitochondrial protein it is unknown if these antibodies can influence mitochondrial function.
Immunological Aspects of ME/CFS
How does autoreactivity develop? Much remains to be learned. The adaptive portion of the immune system (B and T cells) has a formidable task, to distinguish “self” from “non-self,” i.e., autoantigens from antigens of invading microbes. After an infection the immune response is initially relying on players of the innate immune system with natural antibodies, receptors for pathogen-associated molecular patterns, danger-associated molecular patterns, and DNA sensors for exogenous pathogens. However, within a few weeks the immune system acquires a higher precision with the developing adaptive immune B and T cells ensuring that only the targeted microbe is destroyed. The target selection (and tolerance development) may go wrong. Some microbial targets are very similar to self-molecules. This is the basis for the so-called molecular mimicry theory, although the evolutionary lines for microbes and humans diverged long ago. There are still some structures, such as HSP, which have hardly changed at all since then. An immune defense against them thus constitutes a risk of promoting an autoreactive response.
So-called “natural antibodies,” which occur in all persons and mostly are of IgM nature, often both poly- and autoreactive, are produced by a CD20+, CD27+, and CD43+ subset of B cells (189). One function of these natural antibodies is scavenging of dead/apoptotic, damaged and infected cells. Only sometimes do they result in disease. In a healthy person, B cells that can produce autoantibodies often rest in an “anergic” state and do not produce their potentially damaging antibodies. They can be activated by the so-called “cell danger” signals. B cells which produce natural IgM have regulatory functions (190). Such “innate” immune cells which are on the border of auto- and alloreactivity may be starting points for development of autoimmune disease.
Disturbance in the composition of the gut microbiome, dysbiosis, has been detected in several diseases (33–35, 86, 191–195). A major function of the microbiome probably is to train the immune system (e.g., T cells, B cells, and dendritic cells) with a large variety of antigens. Disturbance in it may lead to a defective immune repertoire and imbalance of tolerance induction (196). As the tools for studying microbiota gradually become more precise, the possibility of more or less specific changes in microbiota predisposing to autoreactivity is increasingly being addressed. This is the case for type 1 diabetes (27, 197, 198), multiple sclerosis (199), rheumatoid arthritis (200), SLE (201), Behcet’s syndrome (202), autoimmune gastritis (203), and ankylosing spondylitis (204). ME/CFS patients also seem to have aberrations in their gut microbiota (33, 192, 205, 206).
A symptomatic variant of gut dysbiosis, IBS (207), a common comorbidity in ME/CFS, may influence mucosal tolerance induction. Indeed, ME/CFS with IBS was suggested to be a distinct subset of ME/CFS (208).
It is conceivable that if the mucosal barrier also is broken by microleakage (28, 34, 37, 41, 192, 209–210), tolerance development may become impaired, facilitating development of autoreactivity (37–42, 211–213). Autoimmunity often seems to be a hit and run phenomenon. However, a chronic underlying infection cannot be excluded, also in the ME/CFS case (214, 215).
The hypothesis presented in Figure 2 is based on findings regarding the IGHV gene sequence VH4-34 (23, 24) in SLE. It elaborates the immunoevolutionary aspect of Figure 1. Its explanatory model is similar to current thinking regarding the pathogenesis of autoimmune disease. It tries to clarify the genesis of autoreactive B cell clones from germ line to pathogenicity. The original specificity conferred to a B cell and immunoglobulin by VH4-34 is anti-branched lactosamine containing carbohydrates. This then gradually mutates, probably due to exposure to epitopes from commensal gut bacteria. The original specificity exists in the beginning of a mutational walk in the Vh genetic maze, an example of epistasis, where one mutation facilitates other mutations during avidity maturation. Other unknown antigenic stimulations then give rise to various autoantibodies, some with anti-DNA specificity. We hypothesize that pathogenic autoantibodies in ME/CFS are created by a similar mechanism. Thus, we postulate that a genetically predisposed person gets a deranged gut microbiome which gives rise to apathogenic B cells with a weak autospecificity. They are not eliminated due to a defective tolerance induction. Finally, these clones are given an antigenic stimulation from an exogenous infection which yields pathogenic B cell clones. Thus, memory B cell clones with a paratope spectrum derived from germline and subsequent exposure to commensal microbes, e.g., in gut, may be an important intermediary step before development of outright autoimmunity. It should be possible to follow the path to autopathic clones by isolation and sequencing the variable immunoglobulin chains in B lymphocytes in ME/CFS, like what was done with VH4-34.
Autoreactive B Cell Clones and Autoantibodies in ME/CFS
Several autoantibodies have been found in ME/CFS (54, 93, 94, 216–222), and some of its comorbidities (Table 4). This is circumstantial evidence for ME/CFS being an autoimmune condition. Especially interesting are the results where an increased frequency of antibodies to certain hormone receptors was found (93). Several ME/CFS symptoms may be explainable by receptor interference from such autoantibodies.
In autoimmune conditions with pathological autoantibodies, erroneously activated and mutated B cells are the root of the evil (Figure 2). These should be studied in detail (43). One can envisage large scale sequencing of immunoglobulin gene variable domains of such clones to define aberrant specificities, with autoreactivity. A characteristic variation in B cell subsets (43) has been described in ME/CFS.
This should be studied systematically. At which time point did these diseases manifest themselves, before or after the ME/CFS started? How large is the frequency of autoantibodies in patients with these conditions, preferably measured simultaneously in an antigen matrix? Maybe there are autoimmunity biomarkers which could be used for ME/CFS diagnosis?
Cytokine Patterns in Blood and CSF in ME/CFS
The immune system is engaged in ME/CFS (220). Several studies have found changes in cytokine pattern in blood and CSF, and in expression of cytokine genes (223–231), especially after exercise (232–238), concomitant with an increase in reactive oxygen species (ROS) levels and a decrease of HSP70 concentration (239), often in connection with a “flare,” an acute exacerbation of ME/CFS symptoms (237, 238). A difficulty is that cytokine patterns (Table 5) are inherently variable. The cytokine profiles may be different in different stages of the disease (225, 240).
Table 5.
A selective list of cytokines whose concentrations were reported to change in ME/CFS.
| Cytokine | Body fluid | Up- or downregulation | Reference | Comment |
|---|---|---|---|---|
| TGFα | Serum | + | (225) | |
| TGFβ | Serum | + | (226, 227) | Most consistent finding, although one inconclusive (241) |
| TNFα | Serum | + | (225) | Elevated early after debut |
| IFN-γ | Serum | + | (225) | Elevated early after debut |
| IL1α | Serum | + | (225) | Elevated in early stage of ME/CFS |
| Eotaxin-1 (CCL11) | Serum | −, + | (225, 226) | Positively correlated with severity and low early after debut |
| Eotaxin-2 (CCL24) | Serum | + | (223) | |
| Leptin | Serum | − | (230) | Inversely correlated with severity |
| IL13 | Serum | + | (226) | Positively correlated with severity |
| IL6 | Serum | + | (242) | Elevated early after debut |
| IL7 | Serum | − | (223) | |
| IL8 | Serum | + | (242) | Elevated early after debut |
| IL10 | Cerebrospinal fluid | − | (228) | |
| IL16 | Serum | − | (223) | |
| IL17A | Serum | + | (225) | Elevated early after debut |
| VEGFα | Serum | − | (223) |
A more permanent dysregulation of cytokines in plasma has also been reported (223, 225, 226, 228, 230, 243), see Table 5. A correlation with disease duration was seen (225, 242). A meta-analysis showed that an increased level of TGFβ in plasma in ME/CFS versus controls was the most consistent finding (227). Cytokines in CSF were also deranged in ME/CFS (224, 228).
Table 5 is a compilation from recent publications on cytokine abnormalities in ME/CFS. A recent meta-analysis concluded that many of the reported findings are not reproducible (227). This could reflect different levels of physical activity, the volatile nature of cytokine levels and methodological problems, such as collection, handling, and preparation of samples. There could also be a heterogeneity within the ME/CFS group which blurs the patterns, see, e.g., Ref. (224, 234).
Whether there are cytokine changes after exercise peculiar to ME/CFS is a related subject (244). A recent meta-analysis concluded that complement factor C4a split products, oxidative stress markers and leukocyte expression of IL10 and toll-like receptor 4 genes are reproducibly different from controls in ME/CFS (233). However, there may be subgroups within the ME/CFS group with radically different reactions to exercise. A clear-cut difference in gene expression after exercise between ME/CFS patients which have POTS comorbidity, and those who do not, was found (234).
The activity of the so-called natural killer cells is also changed (231, 244–248) in ME/CFS. However, a negative report came recently (249). The latter may be due to methodological differences. Both kinds of immune change (cytokines and immune cell activity) are potential biomarkers and should be studied more.
Is There a General Defect in Tolerance Development in ME/CFS?
Tolerance induction is a major property of the gut mucosal immune system (196). A special kind of T helper cells, Treg, mediate mucosal tolerance, and anergy of tolerized B cell clones, via IL10 and TGFβ. It may be more than a coincidence that a change in TGFβ levels in serum was the most consistent cytokine change in ME/CFS versus controls (Table 5).
A defective tolerance development could in principle be detectable as a tendency to develop autoimmune disease in ME/CFS. The comorbidity between ME/CFS and better studied autoimmune disorders such as SS (250), SLE, and multiple sclerosis (251) is an indication of this. Fatigability, which may or may not be related to the PEM of ME/CFS (252–255), occurs as a major symptom in some autoimmune (6, 184, 256–261), mitochondrial (262, 263) and infectious (264) diseases. Immunostimulation, e.g., with Staphylococcal vaccine, theoretically could induce tolerance to autoepitopes involved in ME/CFS pathogenesis (265–267). It was reported to be effective in ME/CFS in a double-blind study (267). Symptom relief paralleled anti-staphylococcal antibody presence (266), arguing for impaired development of tolerance to autoepitopes of microbial origin in ME/CFS. Further studies are needed.
A strong argument for B cell-mediated autoimmunity in ME/CFS has been the rituximAab effect (20, 22). Around 60% of patients improved after a lag period. Rituximab is a monoclonal antibody directed against CD20, a surface antigen expressed on the majority of B cells. They are killed when the antibody binds to them. However, in a recent phase III trial there was no statistically significant effect observed (Mella, personal communication). Until results of the trial are published, it is not known whether this was due to a major placebo, or a minor rituximab, effect. CD20 is mainly present on B cells, but is neither expressed on immature B cells nor on most antibody producing cells such as plasmablasts and plasma cells (268). Part of the problem may be the subjective estimation of symptoms, prone to overestimation of placebo effects. In future double-blind studies of treatments for ME, objective symptom measures should be used to a larger extent. Another confounding factor may be heterogeneity within the ME/CFS patients although they were diagnosed according to the Canada criteria. Detailed studies are strongly recommended. Unpublished phase I and II studies have shown improvement in ME/CFS patients after treatment with the more unspecific immunosuppressant cyclophosphamide (Fluge, personal communication). It is another sign of autoimmunity contributing to ME/CFS.
In autoimmunity dependent on autoantibodies, the erroneously activated B cells are the root of the evil.
Increased Frequency of Lymphomas in ME/CFS
Chronic immune stimulation increases the risk for B cell lymphomas. This happens in many autoimmune diseases. In accordance with the autoimmune hypothesis for ME/CFS presented here, CFS patients have a greater risk of B cell non-Hodgkin lymphomas, in particular marginal zone lymphoma (OR = 1.88, 95% CI = 1.38–2.57), compared with sex and age matched controls (269).
In summary, the evidence for autoimmunity in ME/CFS is indirect or circumstantial. It rests on the effect of immunosuppression (although unsubstantiated in a double-blind trial) of anti-CD20, comorbidities with known autoimmunity (thyroiditis, thyroidism) or possible autoimmunity (FM, POTS, IBS), probable improvement after immunostimulation, and an increased frequency of certain autoantibodies and of B cell lymphomas. Of the Witebsky–Rose criteria for autoimmunity (270), direct; transfer of disease by antibody, and indirect; transfer of disease by cells to SCID mice, induction of disease by autoantigen, identification of antibodies within lesions, genetic predisposition, autoantibodies or self-reactive T cells, a few (genetic predisposition and increased frequency of autoantibodies) are partially fulfilled. Much work remains.
Can Autoimmunity Explain Energy Metabolic Disturbances and PEM?
The objective measurement of energy metabolism by repeated cardiopulmonary exercise testing revealed a defective aerobic energy production in ME/CFS (19). This is manifested as an abnormal fatigability. Fatigability, which may or may not be related to the PEM of ME/CFS (252–255), occurs as a major symptom in some autoimmune (6, 184, 256–261), mitochondrial (262, 263) and infectious (264) diseases. It remains to be studied how unique the PEM of ME/CFS is.
Several observations indicate that the oxygen dependent (aerobic) energy metabolism is disturbed in ME/CFS (8, 19, 262, 271–273) (Figure 3; Table 6). That disturbance may be the reason for PEM. Mitochondria are the main producers of energy. They derive from α-proteobacteria which, over one billion years ago, were taken up into eukaryotic cells, see, e.g., Ref. (274). It is not unreasonable to guess that an immune defense against an infecting bacterium can cause collateral damage to mitochondria. While there must be protective mechanisms against this (e.g., tolerization), they may not always work.
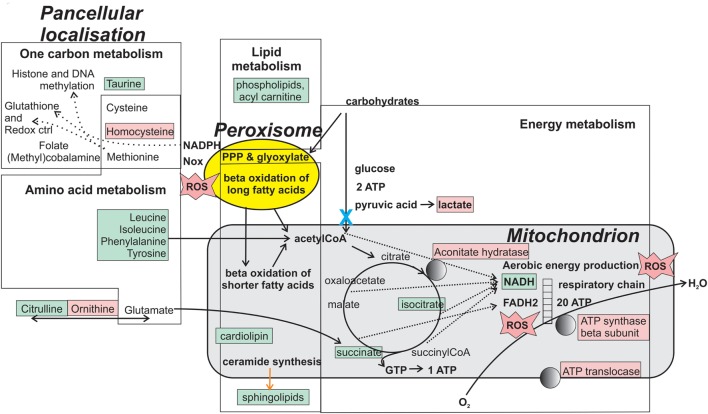
Figure 3.
Metabolites and enzymes that are reportedly changed in ME/CFS. Molecules localized in energy metabolic organelles (peroxisome and mitochondrion), and the whole cell, are shown in pink if increased in abundance and green if decreased in abundance. Changes may sometimes be visible only after exercise. The blue “X” indicates a metabolic block implicated in ME/CFS (275). Normally functioning mitochondria convert oxygen to water through the respiratory chain. If the aerobic energy production is impaired, some oxygen can be converted to hydrogen peroxide and reactive oxygen species (ROS). PPP is the pentose phosphate pathway, an alternative pathway for energy production from carbohydrates. It produces the antioxidant NADPH. Together with glutathione, a product of one-carbon metabolism, NADPH controls ROS accumulation (“Redox ctrl”). A panel including some of the marked molecules may be useful as biomarker for ME/CFS.
Table 6.
Potential energy metabolic biomarkers for ME/CFS.
| Metabolic role | Metabolite or protein | Body fluid | Gain (+) or loss (−) in ME/CFS vs healthy controls | Reference | Comment |
|---|---|---|---|---|---|
| One-carbon metabolism | Taurine | Blood | − | (276) | |
| Homocysteine | Cerebrospinal fluid (CSF) | + | (277) | ||
| Oxidation | Reactive oxygen species (peroxide, etc.) | Serum | + | (239, 278) | Measured using thiobarbituric acid reactive substances |
| Amino acid metabolism (anaplerotic amino acids) | Leucine, isoleucine, phenylalanine, and tyrosine | Blood | − | (275) | |
| Urea cycle and amino acid metabolism | Citrulline | Blood and urine | − | (279) | |
| Ornithine | Blood and urine | + | (279) | ||
| Lipid metabolism | Phospholipids, including cardiolipin | Blood | − | (280) | |
| Acyl carnitine | Blood | − | (276, 280) | ||
| (Glyco)sphingolipids | Blood | − | (280) | ||
| Glycolysis | Lactate | Blood and CSF (muscle) | + | (271, 275, 281) | Higher after exercise (physical and mental) |
| Tricarboxylic acid cycle (TCA) | Isocitrate | Blood | − | (279) | |
| TCA | Succinate | Blood and urine | − | (282) | |
| TCA | Aconitate hydratase protein | Saliva | + | (283) | |
| ATP synthase protein | Saliva | + | (283) | ||
| ATP translocase | Saliva | − | (283) | ||
A new dimension for understanding ME/CFS was added by recent publications (275, 279, 280, 282, 284). They revealed profound metabolic differences between ME/CFS patients and controls. Some of these changes may derive from an abnormal mitochondrial function in ME/CFS. Whether these abnormalities have an autoimmune origin is not known.
Evidence for Inhibition of Key Energy Metabolic Processes in ME/CFS
A number of reports indicate a metabolic disturbance, indicative of mitochondrial dysfunction (19, 273, 275, 276, 279, 280, 282, 284–286) in ME/CFS. Evidence points to a defective aerobic energy metabolism. The aerobic energy metabolism (TCA + respiratory chain) gives an around 10-fold higher yield of ATP per glucose molecule than the anaerobic metabolism. There are similarities with PBC, a model of autoantibody mediated energy blockade (180, 287–292). In analogy with PBC, where IgG were found to be energy inhibitory, circulating energy inhibitors have been found in ME/CFS (275), although their molecular nature is unknown. The demonstration of such inhibitors has the potential to explain the disease and create efficient diagnostic tests. It would be logical if, like in PBC, these circulating inhibitors turned out to be immunoglobulins, presumably directed against mitochondrial proteins.
It is an important research task to compare PEM of PBC with the PEM of ME/CFS, and PEM-like fatigability in other diseases.
Fibromyalgia is a common comorbidity of ME/CFS, which also occurs in several established autoimmune conditions (55, 293–298). The delineation of ME/CFS from FM is sometimes not straightforward. FM muscle displays metabolic abnormalities (299, 300) reminiscent of those observed in ME/CFS. Besides the comorbidity, there seem to be both common (myalgia, muscle metabolic abnormalities, increased frequency of autoantibodies) and distinct (PEM, cognitive disturbance) aspects of these conditions.
Can a Defective Energy Metabolism Also Explain the Cognitive Disturbances?
A deficient energy supply may also cause cognitive disturbance in ME/CFS (195). It can be elicited by both physical and mental (301, 302) activity. In analogy with accumulation of lactate in serum and muscle after exercise, increased concentrations of lactate in CSF have been found in ME/CFS (281, 303) and the related condition GWI (304). ME/CFS-specific changes in the CSF proteome which included accumulation of complement components, a sign of antibody activity, were also described (305).
Homocysteine is part of the one-carbon metabolism, which was reported to be deranged in ME/CFS patients, perhaps as a compensation for other energy metabolic disturbances. Homocysteine levels in CSF are a widely used marker of reduced cognition. In 1997, an investigation of homocysteine and vitamin B12 in CSF of patients who fulfilled the criteria of both FM and chronic fatigue syndrome was carried out. In comparison with a large healthy control group, all eleven patients in the study had increased homocysteine levels in CSF, although the blood levels were usually not increased. The CSF-B12 level appeared to be generally low. The high CSF-homocysteine and low CSF-B12 levels correlated significantly with ratings of mental fatigue. The results were at the time interpreted as suggesting a block of inflow over the blood brain barrier of B12 and/or folic acid (277). The derangement in one-carbon metabolism is supported by 20 years’ experience of vitamin B12 and B9 treatment in ME/CFS patients, which tends to diminish impaired cognition (“brain fog”) (306). It is not immediately evident why the one-carbon metabolic pathway would change after a block of aerobic energy production. The genesis of this metabolic aberration in ME/CFS should be further studied.
The state of the one-carbon metabolism also has profound epigenetic consequences. Both DNA and histone methylation depend on the availability of S-adenosyl-methionine.
How Are Metabolic Disturbances Related to the Flare after Exercise?
The “flare” is a central event after exercise, accounting for much of the malaise in PEM.
A link between mitochondrial dysfunction and innate immune dysregulation is suggested by recent immunometabolic findings which demonstrate that the energy producing organelles (mitochondria and peroxisomes) are coupled via mitochondrial antiviral signaling protein, a signaling molecule, to the inflammasome, which can orchestrate release of inflammatory cytokines (307–314). Another sign of mitochondrial derangement in ME/CFS is the occurrence of ROS in serum, measured as increase in thiobarbituric acid reactive substances or decrease of reduced ascorbic acid (239, 278). These tests may also become part of a biomarker panel for ME/CFS. It was recently shown that oxidation of a critical cysteine residue in pyruvate kinase M2, one of the enzymes of the pyruvate dehydrogenase complex (PDC), can lead to a block in pyruvate production, potentially mimicking an autoimmune block of PDC activity (315, 316). Thus, although the pattern of metabolic changes in ME/CFS is compatible with a PDH block (275) (blue X in Figure 3), possibly of autoimmune origin, the block could also be caused by ROS (317), frequently increased in ME/CFS. ROS are produced in four places in the cell; NADPH oxidase (in Figure 3), peroxisomes and in respiratory chain complexes I and III (318). ROS production can be evoked by starvation (319) and respiratory complex I malfunction (320). ROS influence glutathione levels and indirectly the whole one-carbon metabolism. It could be a key player in ME/CFS pathogenesis. The origin and pathobiology of ROS in ME/CFS should be investigated.
How Well do Clinical and Laboratory Data Fit into the Explanatory Model?
As shown in Table 7, much work remains before the autoimmune nature of ME/CFS can be considered established.
Table 7.
How do recent findings fit into the explanatory model?
| Proposed step | Finding | Degree of fit with presented explanatory model |
|---|---|---|
| Genetic predisposition |
|
|
| Changes in microbiota | Imperfect, needs deeper study | |
| Gut microleakage | Increased lipopolysaccharide (LPS), LPS-binding protein, and sCD14 in blood (34, 192) | Imperfect, needs deeper study |
| Autoantibodies | Yes, but maybe not disease specific (see Table 4) | Imperfect, needs deeper study |
| Triggering antigenic challenge | Epstein–Barr virus infection is a common trigger, some other infections also (see Table 2) | Imperfect. Retrospective diagnosis of infections is often problematic |
| Autopathic B cell clones | Larger study with as objective measures as possible is necessary. Autologous bone marrow transplantation could give additional evidence | |
| Defective tolerization of autoreactive B cell clones | Imperfect, needs deeper study | |
| Disturbance of energy metabolism | Clear evidence of energy metabolic disturbance (275, 276, 279, 280) | Imperfect. Needs more observations, especially with reference to exercise |
| Autoimmunity causing energy metabolic disturbance | Circulating energy inhibitory factors demonstrated (like in primary biliary cirrhosis) (275, 292) | Molecular nature of inhibitors is unknown. If they are immunoglobulins, can they reach intracellular targets? |
Which Facts Do Not Fit into the Explanatory Model?
Even if ME/CFS is of autoimmune origin, is it the metabolic block (275) or the autoantibodies to hormone receptors (93) which are most important for pathogenesis?
The mechanism behind the flare after exercise (238) is obscure. Maybe a mitochondrial defect can lead to an increased activity in the innate immune network.
The disturbance in one-carbon metabolism (277, 280) may or may not be related to the disturbed transition between glycolysis and TCA cycle. It is indicative of a wider metabolic derangement than a block of PDH (275) would be expected to lead to. There are several papers on hormones (322), including glucocorticoids (257) and transient receptor potential channel hormones (222), and their receptors (106, 107, 109), in ME/CFS. It is conceivable that parts of the autonomic dysfunction can be explained in this way.
Conclusion
ME/CFS is a challenge for the patients, for medical research and ethics, for all of public health, and for society. The intensified hunt for scientific evidence explaining ME/CFS has large consequences for many thousands of people. Many of the published results need repetition. But as shown in this article the signs that autoimmunity and energy metabolic deficiency is involved in the disease have increased. A hypothetical but logical path, from gastrointestinal tract dysbiosis, to formation of pathogenic autoimmune B cells, to inhibition of energy production and deficient cognition, to flares of cytokine production, can be delineated. The natural history indicates that in many cases infections can elicit or worsen this autoimmunity.
The recently intensified research on ME/CFS yielded many biomarker candidates, as mentioned in this study. The main consequence of this work is that the proposition that there is no logical somatic explanatory model for ME/CFS (14) can be refuted. However, like for virtually all autoimmune diseases, the explanatory model has several tentative steps which need further exploration. The elucidation of the molecular nature of circulating metabolic inhibitors in ME/CFS (275) is a central question. If they turn out to be immunoglobulins, they may directly yield diagnostically useful biomarkers and an explanation of the mechanism underlying ME/CFS.
The risk of giving a hypothetical unifying explanation, as in this study, is that hypothesis can be perceived as fact, and that it influences the perception of the disease. But contacts with ME/CFS patients and those who care for them have convinced us that most can handle the uncertainty that hypotheses involve. Without hypotheses we cannot direct the acquisition of further knowledge of ME/CFS.
Author Contributions
JB conceived of the paper and wrote most of it. C-GG added substantial parts especially regarding the clinical aspects. AE participated in the writing. She is writing a book on ME/CFS, her comprehensive knowledge was valuable. MR participated in the writing. He concentrated on checking references. AR contributed substantially, especially regarding the immunological aspects.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors thank Dr. Geraldine Cambridge for fruitful discussions on mechanisms of ME/CFS pathogenesis and Dr. Lucinda Bateman for discussions on clinical aspects of ME/CFS.
Footnotes
Funding. The authors thank the SolveME/CFS Initiative, the Swedish ME Association, the Open Medicine Foundation (project no. 1011454), and the Uppsala Academic Hospital (Grant FOU2017-0039) for economic support, as well as the Invest in ME Foundation, London, for travel grants. The funders did not influence the research or the manuscript in any way.
References
- 1.Nacul LC, Lacerda EM, Pheby D, Campion P, Molokhia M, Fayyaz S, et al. Prevalence of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) in three regions of England: a repeated cross-sectional study in primary care. BMC Med (2011) 9:91. 10.1186/1741-7015-9-91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carruthers BM, van de Sande MI, De Meirleir KL, Klimas NG, Broderick G, Mitchell T, et al. Myalgic encephalomyelitis: International Consensus Criteria. J Intern Med (2011) 270:327–38. 10.1111/j.1365-2796.2011.02428.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carruthers BM. Definitions and aetiology of myalgic encephalomyelitis: how the Canadian consensus clinical definition of myalgic encephalomyelitis works. J Clin Pathol (2007) 60:117–9. 10.1136/jcp.2006.042754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jason LA, McManimen S, Sunnquist M, Brown A, Furst J, Newton JL, et al. Case definitions integrating empiric and consensus perspectives. Fatigue (2016) 4:1–23. 10.1080/21641846.2015.1124520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fukuda K, Straus SE, Hickie I, Sharpe MC, Dobbins JG, Komaroff A. The chronic fatigue syndrome: a comprehensive approach to its definition and study. International Chronic Fatigue Syndrome Study Group. Ann Intern Med (1994) 121:953–9. 10.7326/0003-4819-121-12-199412150-00009 [DOI] [PubMed] [Google Scholar]
- 6.Bansal AS. Investigating unexplained fatigue in general practice with a particular focus on CFS/ME. BMC Fam Pract (2016) 17:81. 10.1186/s12875-016-0493-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Unger ER, Lin JS, Brimmer DJ, Lapp CW, Komaroff AL, Nath A, et al. Chronic fatigue syndrome – advancing research and clinical education. MMWR Morb Mortal Wkly Rep (2016) 65:1434–8. 10.15585/mmwr.mm655051a4 [DOI] [PubMed] [Google Scholar]
- 8.Davenport TE, Stevens SR, Baroni K, Van Ness M, Snell CR. Diagnostic accuracy of symptoms characterising chronic fatigue syndrome. Disabil Rehabil (2011) 33:1768–75. 10.3109/09638288.2010.546936 [DOI] [PubMed] [Google Scholar]
- 9.Davenport TE, Stevens SR, Baroni K, Van Ness JM, Snell CR. Reliability and validity of Short Form 36 Version 2 to measure health perceptions in a sub-group of individuals with fatigue. Disabil Rehabil (2011) 33:2596–604. 10.3109/09638288.2011.582925 [DOI] [PubMed] [Google Scholar]
- 10.Haney E, Smith ME, McDonagh M, Pappas M, Daeges M, Wasson N, et al. Diagnostic methods for myalgic encephalomyelitis/chronic fatigue syndrome: a systematic review for a National Institutes of Health Pathways to Prevention Workshop. Ann Intern Med (2015) 162:834–40. 10.7326/M15-0443 [DOI] [PubMed] [Google Scholar]
- 11.Jason LA, Sunnquist M, Brown A, Newton JL, Strand EB, Vernon SD. Chronic fatigue syndrome versus systemic exertion intolerance disease. Fatigue (2015) 3:127–41. 10.1080/21641846.2015.1051291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Committee_on_Diagnostic_Criteria_for_Myalgic_Encephalomyelitis_Chronic_Fatigue_Syndrome. Beyond Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Redefining an Illness. Washington (DC): Institute of Medicine; (2015). [Google Scholar]
- 13.Chu L, Friedberg F, Friedman KJ, Littrell N, Stevens S, Vallings R. Exercise and chronic fatigue syndrome: maximize function, minimize post-exertional malaise. Eur J Clin Invest (2012) 42:1362; author reply 1363–5. 10.1111/j.1365-2362.2012.02723.x [DOI] [PubMed] [Google Scholar]
- 14.Rollnik JD. [Chronic fatigue syndrome: a critical review]. Fortschr Neurol Psychiatr (2017) 85:79–85. 10.1055/s-0042-121259 [DOI] [PubMed] [Google Scholar]
- 15.Bianchi R, Schonfeld IS, Laurent E. Is it time to consider the “Burnout syndrome” a distinct illness? Front Public Health (2015) 3:158. 10.3389/fpubh.2015.00158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.White RF, Steele L, O’Callaghan JP, Sullivan K, Binns JH, Golomb BA, et al. Recent research on Gulf War illness and other health problems in veterans of the 1991 Gulf War: effects of toxicant exposures during deployment. Cortex (2016) 74:449–75. 10.1016/j.cortex.2015.08.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baraniuk JN, Shivapurkar N. Exercise – induced changes in cerebrospinal fluid miRNAs in Gulf War Illness, chronic fatigue syndrome and sedentary control subjects. Sci Rep (2017) 7:15338. 10.1038/s41598-017-15383-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Edwards JC, McGrath S, Baldwin A, Livingstone M, Kewley A. The biological challenge of myalgic encephalomyelitis/chronic fatigue syndrome: a solvable problem. Fatigue (2016) 4:63–9. 10.1080/21641846.2016.1160598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Keller BA, Pryor JL, Giloteaux L. Inability of myalgic encephalomyelitis/chronic fatigue syndrome patients to reproduce VO(2)peak indicates functional impairment. J Transl Med (2014) 12:104. 10.1186/1479-5876-12-104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fluge O, Bruland O, Risa K, Storstein A, Kristoffersen EK, Sapkota D, et al. Benefit from B-lymphocyte depletion using the anti-CD20 antibody rituximab in chronic fatigue syndrome. A double-blind and placebo-controlled study. PLoS One (2011) 6:e26358. 10.1371/journal.pone.0026358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fluge O, Mella O. Clinical impact of B-cell depletion with the anti-CD20 antibody rituximab in chronic fatigue syndrome: a preliminary case series. BMC Neurol (2009) 9:28. 10.1186/1471-2377-9-28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fluge O, Risa K, Lunde S, Alme K, Rekeland IG, Sapkota D, et al. B-lymphocyte depletion in myalgic encephalopathy/chronic fatigue syndrome. An open-label phase II study with rituximab maintenance treatment. PLoS One (2015) 10:e0129898. 10.1371/journal.pone.0129898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tipton CM, Fucile CF, Darce J, Chida A, Ichikawa T, Gregoretti I, et al. Diversity, cellular origin and autoreactivity of antibody-secreting cell population expansions in acute systemic lupus erythematosus. Nat Immunol (2015) 16:755–65. 10.1038/ni.3175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pugh-Bernard AE, Silverman GJ, Cappione AJ, Villano ME, Ryan DH, Insel RA, et al. Regulation of inherently autoreactive VH4-34 B cells in the maintenance of human B cell tolerance. J Clin Invest (2001) 108:1061–70. 10.1172/JCI200112462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vaz NM, Carvalho CR. On the origin of immunopathology. J Theor Biol (2015) 375:61–70. 10.1016/j.jtbi.2014.06.006 [DOI] [PubMed] [Google Scholar]
- 26.Ferreira CM, Vieira AT, Vinolo MA, Oliveira FA, Curi R, Martins Fdos S. The central role of the gut microbiota in chronic inflammatory diseases. J Immunol Res (2014) 2014:689492. 10.1155/2014/689492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vaarala O. Gut microbiota and type 1 diabetes. Rev Diabet Stud (2012) 9:251–9. 10.1900/RDS.2012.9.251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fasano A, Shea-Donohue T. Mechanisms of disease: the role of intestinal barrier function in the pathogenesis of gastrointestinal autoimmune diseases. Nat Clin Pract Gastroenterol Hepatol (2005) 2:416–22. 10.1038/ncpgasthep0259 [DOI] [PubMed] [Google Scholar]
- 29.Noverr MC, Huffnagle GB. Does the microbiota regulate immune responses outside the gut? Trends Microbiol (2004) 12:562–8. 10.1016/j.tim.2004.10.008 [DOI] [PubMed] [Google Scholar]
- 30.Aaron LA, Arguelles LM, Ashton S, Belcourt M, Herrell R, Goldberg J, et al. Health and functional status of twins with chronic regional and widespread pain. J Rheumatol (2002) 29:2426–34. [PubMed] [Google Scholar]
- 31.Aaron LA, Herrell R, Ashton S, Belcourt M, Schmaling K, Goldberg J, et al. Comorbid clinical conditions in chronic fatigue: a co-twin control study. J Gen Intern Med (2001) 16:24–31. 10.1111/j.1525-1497.2001.03419.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hausteiner-Wiehle C, Henningsen P. Irritable bowel syndrome: relations with functional, mental, and somatoform disorders. World J Gastroenterol (2014) 20:6024–30. 10.3748/wjg.v20.i20.6024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Navaneetharaja N, Griffiths V, Wileman T, Carding SR. A role for the intestinal microbiota and virome in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)? J Clin Med (2016) 5:1–22. 10.3390/jcm5060055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shukla SK, Cook D, Meyer J, Vernon SD, Le T, Clevidence D, et al. Changes in gut and plasma microbiome following exercise challenge in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). PLoS One (2015) 10:e0145453. 10.1371/journal.pone.0145453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nagy-Szakal D, Williams BL, Mishra N, Che X, Lee B, Bateman L, et al. Fecal metagenomic profiles in subgroups of patients with myalgic encephalomyelitis/chronic fatigue syndrome. Microbiome (2017) 5:44. 10.1186/s40168-017-0261-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Holmgren J, Czerkinsky C. Mucosal immunity and vaccines. Nat Med (2005) 11:S45–53. 10.1038/nm1213 [DOI] [PubMed] [Google Scholar]
- 37.Quigley EM. Leaky gut – concept or clinical entity? Curr Opin Gastroenterol (2016) 32:74–9. 10.1097/MOG.0000000000000243 [DOI] [PubMed] [Google Scholar]
- 38.Michielan A, D’Inca R. Intestinal permeability in inflammatory bowel disease: pathogenesis, clinical evaluation, and therapy of leaky gut. Mediators Inflamm (2015) 2015:628157. 10.1155/2015/628157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lin R, Zhou L, Zhang J, Wang B. Abnormal intestinal permeability and microbiota in patients with autoimmune hepatitis. Int J Clin Exp Pathol (2015) 8:5153–60. [PMC free article] [PubMed] [Google Scholar]
- 40.Taneja V. Arthritis susceptibility and the gut microbiome. FEBS Lett (2014) 588:4244–9. 10.1016/j.febslet.2014.05.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fasano A. Leaky gut and autoimmune diseases. Clin Rev Allergy Immunol (2012) 42:71–8. 10.1007/s12016-011-8291-x [DOI] [PubMed] [Google Scholar]
- 42.de Kort S, Keszthelyi D, Masclee AA. Leaky gut and diabetes mellitus: what is the link? Obes Rev (2011) 12:449–58. 10.1111/j.1467-789X.2010.00845.x [DOI] [PubMed] [Google Scholar]
- 43.Mensah F, Bansal A, Berkovitz S, Sharma A, Reddy V, Leandro MJ, et al. Extended B cell phenotype in patients with myalgic encephalomyelitis/chronic fatigue syndrome: a cross-sectional study. Clin Exp Immunol (2016) 184:237–47. 10.1111/cei.12749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Oldstone MB. Molecular mimicry: its evolution from concept to mechanism as a cause of autoimmune diseases. Monoclon Antib Immunodiagn Immunother (2014) 33:158–65. 10.1089/mab.2013.0090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lee HJ, Li CW, Hammerstad SS, Stefan M, Tomer Y. Immunogenetics of autoimmune thyroid diseases: a comprehensive review. J Autoimmun (2015) 64:82–90. 10.1016/j.jaut.2015.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Theander E, Jacobsson LT. Relationship of Sjogren’s syndrome to other connective tissue and autoimmune disorders. Rheum Dis Clin North Am (2008) 34:935–47,viii–ix. 10.1016/j.rdc.2008.08.009 [DOI] [PubMed] [Google Scholar]
- 47.Kurien BT, Scofield RH. Autoantibody determination in the diagnosis of systemic lupus erythematosus. Scand J Immunol (2006) 64:227–35. 10.1111/j.1365-3083.2006.01819.x [DOI] [PubMed] [Google Scholar]
- 48.Smith J, Fritz EL, Kerr JR, Cleare AJ, Wessely S, Mattey DL. Association of chronic fatigue syndrome with human leucocyte antigen class II alleles. J Clin Pathol (2005) 58:860–3. 10.1136/jcp.2004.022681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Carlo-Stella N, Badulli C, De Silvestri A, Bazzichi L, Martinetti M, Lorusso L, et al. A first study of cytokine genomic polymorphisms in CFS: positive association of TNF-857 and IFNgamma 874 rare alleles. Clin Exp Rheumatol (2006) 24:179–82. [PubMed] [Google Scholar]
- 50.Schlauch KA, Khaiboullina SF, De Meirleir KL, Rawat S, Petereit J, Rizvanov AA, et al. Genome-wide association analysis identifies genetic variations in subjects with myalgic encephalomyelitis/chronic fatigue syndrome. Transl Psychiatry (2016) 6:e730. 10.1038/tp.2015.208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ahmad J, Blumen H, Tagoe CE. Association of antithyroid peroxidase antibody with fibromyalgia in rheumatoid arthritis. Rheumatol Int (2015) 35:1415–21. 10.1007/s00296-015-3278-1 [DOI] [PubMed] [Google Scholar]
- 52.Giacomelli C, Talarico R, Bombardieri S, Bazzichi L. The interaction between autoimmune diseases and fibromyalgia: risk, disease course and management. Expert Rev Clin Immunol (2013) 9:1069–76. 10.1586/1744666X.2013.849440 [DOI] [PubMed] [Google Scholar]
- 53.Suk JH, Lee JH, Kim JM. Association between thyroid autoimmunity and fibromyalgia. Exp Clin Endocrinol Diabetes (2012) 120:401–4. 10.1055/s-0032-1309008 [DOI] [PubMed] [Google Scholar]
- 54.Klein R, Berg PA. High incidence of antibodies to 5-hydroxytryptamine, gangliosides and phospholipids in patients with chronic fatigue and fibromyalgia syndrome and their relatives: evidence for a clinical entity of both disorders. Eur J Med Res (1995) 1:21–6. [PubMed] [Google Scholar]
- 55.Bazzichi L, Rossi A, Zirafa C, Monzani F, Tognini S, Dardano A, et al. Thyroid autoimmunity may represent a predisposition for the development of fibromyalgia? Rheumatol Int (2012) 32:335–41. 10.1007/s00296-010-1620-1 [DOI] [PubMed] [Google Scholar]
- 56.Borchers AT, Gershwin ME. Fibromyalgia: a critical and comprehensive review. Clin Rev Allergy Immunol (2015) 49:100–51. 10.1007/s12016-015-8509-4 [DOI] [PubMed] [Google Scholar]
- 57.Wallace DJ, Gavin IM, Karpenko O, Barkhordar F, Gillis BS. Cytokine and chemokine profiles in fibromyalgia, rheumatoid arthritis and systemic lupus erythematosus: a potentially useful tool in differential diagnosis. Rheumatol Int (2015) 35:991–6. 10.1007/s00296-014-3172-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pimentel M, Morales W, Rezaie A, Marsh E, Lembo A, Mirocha J, et al. Development and validation of a biomarker for diarrhea-predominant irritable bowel syndrome in human subjects. PLoS One (2015) 10:e0126438. 10.1371/journal.pone.0126438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.van Tilburg MA, Zaki EA, Venkatesan T, Boles RG. Irritable bowel syndrome may be associated with maternal inheritance and mitochondrial DNA control region sequence variants. Dig Dis Sci (2014) 59:1392–7. 10.1007/s10620-014-3045-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Van Oudenhove L, Vandenberghe J, Vos R, Holvoet L, Tack J. Factors associated with co-morbid irritable bowel syndrome and chronic fatigue-like symptoms in functional dyspepsia. Neurogastroenterol Motil (2011) 23:524–e202. 10.1111/j.1365-2982.2010.01667.x [DOI] [PubMed] [Google Scholar]
- 61.Sperber AD, Dekel R. Irritable bowel syndrome and co-morbid gastrointestinal and extra-gastrointestinal functional syndromes. J Neurogastroenterol Motil (2010) 16:113–9. 10.5056/jnm.2010.16.2.113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lakhan SE, Kirchgessner A. Gut inflammation in chronic fatigue syndrome. Nutr Metab (Lond) (2010) 7:79. 10.1186/1743-7075-7-79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hamilton WT, Gallagher AM, Thomas JM, White PD. Risk markers for both chronic fatigue and irritable bowel syndromes: a prospective case-control study in primary care. Psychol Med (2009) 39:1913–21. 10.1017/S0033291709005601 [DOI] [PubMed] [Google Scholar]
- 64.Dahan S, Tomljenovic L, Shoenfeld Y. Postural orthostatic tachycardia syndrome (POTS) – a novel member of the autoimmune family. Lupus (2016) 25:339–42. 10.1177/0961203316629558 [DOI] [PubMed] [Google Scholar]
- 65.Tagoe CE. Rheumatic symptoms in autoimmune thyroiditis. Curr Rheumatol Rep (2015) 17:5. 10.1007/s11926-014-0479-7 [DOI] [PubMed] [Google Scholar]
- 66.Ahmad J, Tagoe CE. Fibromyalgia and chronic widespread pain in autoimmune thyroid disease. Clin Rheumatol (2014) 33:885–91. 10.1007/s10067-014-2490-9 [DOI] [PubMed] [Google Scholar]
- 67.Carayanniotis G. The cryptic self in thyroid autoimmunity: the paradigm of thyroglobulin. Autoimmunity (2003) 36:423–8. 10.1080/08916930310001602975 [DOI] [PubMed] [Google Scholar]
- 68.Katz BZ, Jason LA. Chronic fatigue syndrome following infections in adolescents. Curr Opin Pediatr (2013) 25:95–102. 10.1097/MOP.0b013e32835c1108 [DOI] [PubMed] [Google Scholar]
- 69.Hickie I, Davenport T, Wakefield D, Vollmer-Conna U, Cameron B, Vernon SD, et al. Post-infective and chronic fatigue syndromes precipitated by viral and non-viral pathogens: prospective cohort study. BMJ (2006) 333:575. 10.1136/bmj.38933.585764.AE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Morroy G, Keijmel SP, Delsing CE, Bleijenberg G, Langendam M, Timen A, et al. Fatigue following acute Q-fever: a systematic literature review. PLoS One (2016) 11:e0155884. 10.1371/journal.pone.0155884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Parker NR, Barralet JH, Bell AM. Q fever. Lancet (2006) 367:679–88. 10.1016/S0140-6736(06)68266-4 [DOI] [PubMed] [Google Scholar]
- 72.Wensaas KA, Langeland N, Hanevik K, Morch K, Eide GE, Rortveit G. Irritable bowel syndrome and chronic fatigue 3 years after acute giardiasis: historic cohort study. Gut (2012) 61:214–9. 10.1136/gutjnl-2011-300220 [DOI] [PubMed] [Google Scholar]
- 73.Hunskar GS, Langeland N, Wensaas KA, Hanevik K, Eide GE, Morch K, et al. The impact of atopic disease on the risk of post-infectious fatigue and irritable bowel syndrome 3 years after Giardia infection. A historic cohort study. Scand J Gastroenterol (2012) 47:956–61. 10.3109/00365521.2012.696681 [DOI] [PubMed] [Google Scholar]
- 74.Cvejic E, Lemon J, Hickie IB, Lloyd AR, Vollmer-Conna U. Neurocognitive disturbances associated with acute infectious mononucleosis, Ross River fever and Q fever: a preliminary investigation of inflammatory and genetic correlates. Brain Behav Immun (2014) 36:207–14. 10.1016/j.bbi.2013.11.002 [DOI] [PubMed] [Google Scholar]
- 75.Soumahoro MK, Gerardin P, Boelle PY, Perrau J, Fianu A, Pouchot J, et al. Impact of Chikungunya virus infection on health status and quality of life: a retrospective cohort study. PLoS One (2009) 4:e7800. 10.1371/journal.pone.0007800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Elsinga J, Gerstenbluth I, van der Ploeg S, Halabi Y, Lourents NT, Burgerhof JG, et al. Long-term Chikungunya Sequelae in Curacao: burden, determinants, and a novel classification tool. J Infect Dis (2017) 216:573–81. 10.1093/infdis/jix312 [DOI] [PubMed] [Google Scholar]
- 77.Garcia MN, Hause AM, Walker CM, Orange JS, Hasbun R, Murray KO. Evaluation of prolonged fatigue post-West Nile virus infection and association of fatigue with elevated antiviral and proinflammatory cytokines. Viral Immunol (2014) 27:327–33. 10.1089/vim.2014.0035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Berg PJ, Smallfield S, Svien L. An investigation of depression and fatigue post West Nile virus infection. S D Med (2010) 63:127–9. [PubMed] [Google Scholar]
- 79.Sejvar JJ, Curns AT, Welburg L, Jones JF, Lundgren LM, Capuron L, et al. Neurocognitive and functional outcomes in persons recovering from West Nile virus illness. J Neuropsychol (2008) 2:477–99. 10.1348/174866407X218312 [DOI] [PubMed] [Google Scholar]
- 80.Stanaway JD, Shepard DS, Undurraga EA, Halasa YA, Coffeng LE, Brady OJ, et al. The global burden of dengue: an analysis from the Global Burden of Disease Study 2013. Lancet Infect Dis (2016) 16:712–23. 10.1016/S1473-3099(16)00026-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Seet RC, Quek AM, Lim EC. Post-infectious fatigue syndrome in dengue infection. J Clin Virol (2007) 38:1–6. 10.1016/j.jcv.2006.10.011 [DOI] [PubMed] [Google Scholar]
- 82.Carod-Artal FJ. Post-Ebolavirus disease syndrome: what do we know? Expert Rev Anti Infect Ther (2015) 13:1185–7. 10.1586/14787210.2015.1079128 [DOI] [PubMed] [Google Scholar]
- 83.Epstein L, Wong KK, Kallen AJ, Uyeki TM. Post-Ebola signs and symptoms in U.S. Survivors. N Engl J Med (2015) 373:2484–6. 10.1056/NEJMc1506576 [DOI] [PubMed] [Google Scholar]
- 84.Moldofsky H, Patcai J. Chronic widespread musculoskeletal pain, fatigue, depression and disordered sleep in chronic post-SARS syndrome; a case-controlled study. BMC Neurol (2011) 11:37. 10.1186/1471-2377-11-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Pohl D, Alper G, Van Haren K, Kornberg AJ, Lucchinetti CF, Tenembaum S, et al. Acute disseminated encephalomyelitis: updates on an inflammatory CNS syndrome. Neurology (2016) 87:S38–45. 10.1212/WNL.0000000000002825 [DOI] [PubMed] [Google Scholar]
- 86.Lim M, Hacohen Y, Vincent A. Autoimmune encephalopathies. Pediatr Clin North Am (2015) 62:667–85. 10.1016/j.pcl.2015.03.011 [DOI] [PubMed] [Google Scholar]
- 87.Nyati KK, Nyati R. Role of Campylobacter jejuni infection in the pathogenesis of Guillain-Barre syndrome: an update. Biomed Res Int (2013) 2013:852195. 10.1155/2013/852195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ozkurt Z, Tanriverdi EC. Global alert: Zika virus-an emerging arbovirus. Eurasian J Med (2017) 49:142–7. 10.5152/eurasianjmed.2017.17147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Johnson TP, Tyagi R, Lee PR, Lee MH, Johnson KR, Kowalak J, et al. Nodding syndrome may be an autoimmune reaction to the parasitic worm Onchocerca volvulus. Sci Transl Med (2017) 9:1–10. 10.1126/scitranslmed.aaf6953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Cunningham MW. Post-streptococcal autoimmune sequelae: rheumatic fever and beyond. In: Ferretti JJ, Stevens DL, Fischetti VA, editors. Streptococcus pyogenes: Basic Biology to Clinical Manifestations. Oklahoma City, OK: University of Oklahoma Health Sciences Center; (2016). [PubMed] [Google Scholar]
- 91.Libbey JE, Cusick MF, Fujinami RS. Role of pathogens in multiple sclerosis. Int Rev Immunol (2014) 33:266–83. 10.3109/08830185.2013.823422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Greenlee JE. Encephalitis and postinfectious encephalitis. Continuum (Minneap Minn) (2012) 18:1271–89. 10.1212/01.CON.0000423847.40147.06 [DOI] [PubMed] [Google Scholar]
- 93.Loebel M, Grabowski P, Heidecke H, Bauer S, Hanitsch LG, Wittke K, et al. Antibodies to beta adrenergic and muscarinic cholinergic receptors in patients with chronic fatigue syndrome. Brain Behav Immun (2016) 52:32–9. 10.1016/j.bbi.2015.09.013 [DOI] [PubMed] [Google Scholar]
- 94.Elfaitouri A, Herrmann B, Bolin-Wiener A, Wang Y, Gottfries CG, Zachrisson O, et al. Epitopes of microbial and human heat shock protein 60 and their recognition in myalgic encephalomyelitis. PLoS One (2013) 8:e81155. 10.1371/journal.pone.0081155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.McManimen SL, Jason LA. Post-exertional malaise in patients with ME and CFS with comorbid fibromyalgia. SRL Neurol Neurosurg (2017) 3:22–7. [PMC free article] [PubMed] [Google Scholar]
- 96.Goebel A. Autoantibody pain. Autoimmun Rev (2016) 15:552–7. 10.1016/j.autrev.2016.02.011 [DOI] [PubMed] [Google Scholar]
- 97.Klein CJ, Lennon VA, Aston PA, McKeon A, Pittock SJ. Chronic pain as a manifestation of potassium channel-complex autoimmunity. Neurology (2012) 79:1136–44. 10.1212/WNL.0b013e3182698cab [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Wikland B, Lowhagen T, Sandberg PO. Fine-needle aspiration cytology of the thyroid in chronic fatigue. Lancet (2001) 357:956–7. 10.1016/S0140-6736(05)71654-8 [DOI] [PubMed] [Google Scholar]
- 99.Akamizu T, Kohn LD, Mori T. Molecular studies on thyrotropin (TSH) receptor and anti-TSH receptor antibodies. Endocr J (1995) 42:617–27. 10.1507/endocrj.42.617 [DOI] [PubMed] [Google Scholar]
- 100.Hoad A, Spickett G, Elliott J, Newton J. Postural orthostatic tachycardia syndrome is an under-recognized condition in chronic fatigue syndrome. QJM (2008) 101:961–5. 10.1093/qjmed/hcn123 [DOI] [PubMed] [Google Scholar]
- 101.Kimpinski K, Iodice V, Vernino S, Sandroni P, Low PA. Association of N-type calcium channel autoimmunity in patients with autoimmune autonomic ganglionopathy. Auton Neurosci (2009) 150:136–9. 10.1016/j.autneu.2009.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Lobel M, Mooslechner AA, Bauer S, Gunther S, Letsch A, Hanitsch LG, et al. Polymorphism in COMT is associated with IgG3 subclass level and susceptibility to infection in patients with chronic fatigue syndrome. J Transl Med (2015) 13:264. 10.1186/s12967-015-0628-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Guenther S, Loebel M, Mooslechner AA, Knops M, Hanitsch LG, Grabowski P, et al. Frequent IgG subclass and mannose binding lectin deficiency in patients with chronic fatigue syndrome. Hum Immunol (2015) 76:729–35. 10.1016/j.humimm.2015.09.028 [DOI] [PubMed] [Google Scholar]
- 104.Natelson BH, Haghighi MH, Ponzio NM. Evidence for the presence of immune dysfunction in chronic fatigue syndrome. Clin Diagn Lab Immunol (2002) 9:747–52. 10.1128/CDLI.9.4.747-752.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Robertson MJ, Schacterle RS, Mackin GA, Wilson SN, Bloomingdale KL, Ritz J, et al. Lymphocyte subset differences in patients with chronic fatigue syndrome, multiple sclerosis and major depression. Clin Exp Immunol (2005) 141:326–32. 10.1111/j.1365-2249.2005.02833.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Marshall-Gradisnik S, Johnston S, Chacko A, Nguyen T, Smith P, Staines D. Single nucleotide polymorphisms and genotypes of transient receptor potential ion channel and acetylcholine receptor genes from isolated B lymphocytes in myalgic encephalomyelitis/chronic fatigue syndrome patients. J Int Med Res (2016) 44:1381–94. 10.1177/0300060516671622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Marshall-Gradisnik S, Huth T, Chacko A, Johnston S, Smith P, Staines D. Natural killer cells and single nucleotide polymorphisms of specific ion channels and receptor genes in myalgic encephalomyelitis/chronic fatigue syndrome. Appl Clin Genet (2016) 9:39–47. 10.2147/TACG.S99405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Johnston S, Staines D, Klein A, Marshall-Gradisnik S. A targeted genome association study examining transient receptor potential ion channels, acetylcholine receptors, and adrenergic receptors in chronic fatigue syndrome/myalgic encephalomyelitis. BMC Med Genet (2016) 17:79. 10.1186/s12881-016-0342-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Vangeel E, Van Den Eede F, Hompes T, Izzi B, Del Favero J, Moorkens G, et al. Chronic fatigue syndrome and DNA hypomethylation of the glucocorticoid receptor gene promoter 1F region: associations with HPA axis hypofunction and childhood trauma. Psychosom Med (2015) 77:853–62. 10.1097/PSY.0000000000000224 [DOI] [PubMed] [Google Scholar]
- 110.Bouquet J, Gardy JL, Brown S, Pfeil J, Miller RR, Morshed M, et al. RNA-seq analysis of gene expression, viral pathogen, and B-cell/T-cell receptor signatures in complex chronic disease. Clin Infect Dis (2017) 64:476–81. 10.1093/cid/ciw767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Kaushik N, Fear D, Richards SC, McDermott CR, Nuwaysir EF, Kellam P, et al. Gene expression in peripheral blood mononuclear cells from patients with chronic fatigue syndrome. J Clin Pathol (2005) 58:826–32. 10.1136/jcp.2005.025718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Fang H, Xie Q, Boneva R, Fostel J, Perkins R, Tong W. Gene expression profile exploration of a large dataset on chronic fatigue syndrome. Pharmacogenomics (2006) 7:429–40. 10.2217/14622416.7.3.429 [DOI] [PubMed] [Google Scholar]
- 113.Maes M, Mihaylova I, Leunis JC. Chronic fatigue syndrome is accompanied by an IgM-related immune response directed against neopitopes formed by oxidative or nitrosative damage to lipids and proteins. Neuro Endocrinol Lett (2006) 27:615–21. 10.1097/YCO.0b013e32831a4728 [DOI] [PubMed] [Google Scholar]
- 114.De Meirleir K, Bisbal C, Campine I, De Becker P, Salehzada T, Demettre E, et al. A 37 kDa 2-5A binding protein as a potential biochemical marker for chronic fatigue syndrome. Am J Med (2000) 108:99–105. 10.1016/S0002-9343(99)00300-9 [DOI] [PubMed] [Google Scholar]
- 115.Brenu EW, Ashton KJ, Batovska J, Staines DR, Marshall-Gradisnik SM. High-throughput sequencing of plasma microRNA in chronic fatigue syndrome/myalgic encephalomyelitis. PLoS One (2014) 9:e102783. 10.1371/journal.pone.0102783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Cerda-Olmedo G, Mena-Duran AV, Monsalve V, Oltra E. Identification of a microRNA signature for the diagnosis of fibromyalgia. PLoS One (2015) 10:e0121903. 10.1371/journal.pone.0121903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Bested AC, Marshall LM. Review of myalgic encephalomyelitis/chronic fatigue syndrome: an evidence-based approach to diagnosis and management by clinicians. Rev Environ Health (2015) 30:223–49. 10.1515/reveh-2015-0026 [DOI] [PubMed] [Google Scholar]
- 118.Underhill RA. Myalgic encephalomyelitis, chronic fatigue syndrome: an infectious disease. Med Hypotheses (2015) 85:765–73. 10.1016/j.mehy.2015.10.011 [DOI] [PubMed] [Google Scholar]
- 119.Loebel M, Strohschein K, Giannini C, Koelsch U, Bauer S, Doebis C, et al. Deficient EBV-specific B- and T-cell response in patients with chronic fatigue syndrome. PLoS One (2014) 9:e85387. 10.1371/journal.pone.0085387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Moss-Morris R, Spence MJ, Hou R. The pathway from glandular fever to chronic fatigue syndrome: can the cognitive behavioural model provide the map? Psychol Med (2011) 41:1099–107. 10.1017/S003329171000139X [DOI] [PubMed] [Google Scholar]
- 121.Komaroff AL, Cho TA. Role of infection and neurologic dysfunction in chronic fatigue syndrome. Semin Neurol (2011) 31:325–37. 10.1055/s-0031-1287654 [DOI] [PubMed] [Google Scholar]
- 122.Katz BZ, Stewart JM, Shiraishi Y, Mears CJ, Taylor R. Autonomic symptoms at baseline and following infectious mononucleosis in a prospective cohort of adolescents. Arch Pediatr Adolesc Med (2011) 165:765–6. 10.1001/archpediatrics.2011.124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Naess H, Sundal E, Myhr KM, Nyland HI. Postinfectious and chronic fatigue syndromes: clinical experience from a tertiary-referral centre in Norway. In Vivo (2010) 24:185–8. [PubMed] [Google Scholar]
- 124.Katz BZ, Boas S, Shiraishi Y, Mears CJ, Taylor R. Exercise tolerance testing in a prospective cohort of adolescents with chronic fatigue syndrome and recovered controls following infectious mononucleosis. J Pediatr (2010) 157:468–72,472.e1. 10.1016/j.jpeds.2010.03.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Huang Y, Katz BZ, Mears C, Kielhofner GW, Taylor R. Postinfectious fatigue in adolescents and physical activity. Arch Pediatr Adolesc Med (2010) 164:803–9. 10.1001/archpediatrics.2010.144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Rees CJ, Henderson AH, Belafsky PC. Postviral vagal neuropathy. Ann Otol Rhinol Laryngol (2009) 118:247–52. 10.1177/000348940911800402 [DOI] [PubMed] [Google Scholar]
- 127.Katz BZ, Shiraishi Y, Mears CJ, Binns HJ, Taylor R. Chronic fatigue syndrome after infectious mononucleosis in adolescents. Pediatrics (2009) 124:189–93. 10.1542/peds.2008-1879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Leis AA, Stokic DS. Neuromuscular manifestations of west nile virus infection. Front Neurol (2012) 3:37. 10.3389/fneur.2012.00037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Sullivan PF, Allander T, Lysholm F, Goh S, Persson B, Jacks A, et al. An unbiased metagenomic search for infectious agents using monozygotic twins discordant for chronic fatigue. BMC Microbiol (2011) 11:2. 10.1186/1471-2180-11-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Zhang L, Gough J, Christmas D, Mattey DL, Richards SC, Main J, et al. Microbial infections in eight genomic subtypes of chronic fatigue syndrome/myalgic encephalomyelitis. J Clin Pathol (2010) 63:156–64. 10.1136/jcp.2009.072561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Lane RJ, Soteriou BA, Zhang H, Archard LC. Enterovirus related metabolic myopathy: a postviral fatigue syndrome. J Neurol Neurosurg Psychiatry (2003) 74:1382–6. 10.1136/jnnp.74.10.1382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Bowman SJ, Brostoff J, Newman S, Mowbray JF. Postviral syndrome – how can a diagnosis be made? A study of patients undergoing a Monospot test. J R Soc Med (1989) 82:712–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Chapenko S, Krumina A, Logina I, Rasa S, Chistjakovs M, Sultanova A, et al. Association of active human herpesvirus-6, -7 and parvovirus b19 infection with clinical outcomes in patients with myalgic encephalomyelitis/chronic fatigue syndrome. Adv Virol (2012) 2012:205085. 10.1155/2012/205085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Loebel M, Eckey M, Sotzny F, Hahn E, Bauer S, Grabowski P, et al. Serological profiling of the EBV immune response in chronic fatigue syndrome using a peptide microarray. PLoS One (2017) 12:e0179124. 10.1371/journal.pone.0179124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Halpin P, Williams MV, Klimas NG, Fletcher MA, Barnes Z, Ariza ME. Myalgic encephalomyelitis/chronic fatigue syndrome and gulf war illness patients exhibit increased humoral responses to the herpesviruses-encoded dUTPase: implications in disease pathophysiology. J Med Virol (2017) 89:1636–45. 10.1002/jmv.24810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Kerr JR, Gough J, Richards SC, Main J, Enlander D, McCreary M, et al. Antibody to parvovirus B19 nonstructural protein is associated with chronic arthralgia in patients with chronic fatigue syndrome/myalgic encephalomyelitis. J Gen Virol (2010) 91:893–7. 10.1099/vir.0.017590-0 [DOI] [PubMed] [Google Scholar]
- 137.Kato YH, Yamate M, Tsujikawa M, Nishigaki H, Tanaka Y, Yunoki M, et al. No apparent difference in the prevalence of parvovirus B19 infection between chronic fatigue syndrome patients and healthy controls in Japan. J Clin Virol (2009) 44:246–7. 10.1016/j.jcv.2009.01.001 [DOI] [PubMed] [Google Scholar]
- 138.Seishima M, Mizutani Y, Shibuya Y, Arakawa C. Chronic fatigue syndrome after human parvovirus B19 infection without persistent viremia. Dermatology (2008) 216:341–6. 10.1159/000116723 [DOI] [PubMed] [Google Scholar]
- 139.McGhee SA, Kaska B, Liebhaber M, Stiehm ER. Persistent parvovirus-associated chronic fatigue treated with high dose intravenous immunoglobulin. Pediatr Infect Dis J (2005) 24:272–4. 10.1097/01.inf.0000155194.66797.20 [DOI] [PubMed] [Google Scholar]
- 140.Knosel T, Meisel H, Borgmann A, Riebel T, Krenn V, Schewe C, et al. Parvovirus B19 infection associated with unilateral cervical lymphadenopathy, apoptotic sinus histiocytosis, and prolonged fatigue. J Clin Pathol (2005) 58:872–5. 10.1136/jcp.2004.022756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Matano S, Kinoshita H, Tanigawa K, Terahata S, Sugimoto T. Acute parvovirus B19 infection mimicking chronic fatigue syndrome. Intern Med (2003) 42:903–5. 10.2169/internalmedicine.42.903 [DOI] [PubMed] [Google Scholar]
- 142.Kerr JR, Bracewell J, Laing I, Mattey DL, Bernstein RM, Bruce IN, et al. Chronic fatigue syndrome and arthralgia following parvovirus B19 infection. J Rheumatol (2002) 29:595–602. [PubMed] [Google Scholar]
- 143.Kerr JR, Cunniffe VS. Antibodies to parvovirus B19 non-structural protein are associated with chronic but not acute arthritis following B19 infection. Rheumatology (Oxford) (2000) 39:903–8. 10.1093/rheumatology/39.8.903 [DOI] [PubMed] [Google Scholar]
- 144.Jacobson SK, Daly JS, Thorne GM, McIntosh K. Chronic parvovirus B19 infection resulting in chronic fatigue syndrome: case history and review. Clin Infect Dis (1997) 24:1048–51. 10.1086/513627 [DOI] [PubMed] [Google Scholar]
- 145.Ilaria RL, Jr, Komaroff AL, Fagioli LR, Moloney WC, True CA, Naides SJ. Absence of parvovirus B19 infection in chronic fatigue syndrome. Arthritis Rheum (1995) 38:638–41. 10.1002/art.1780380510 [DOI] [PubMed] [Google Scholar]
- 146.Leventhal LJ, Naides SJ, Freundlich B. Fibromyalgia and parvovirus infection. Arthritis Rheum (1991) 34:1319–24. 10.1002/art.1780341018 [DOI] [PubMed] [Google Scholar]
- 147.Baboonian C, Halliday D, Venables PJ, Pawlowski T, Millman G, Maini RN. Antibodies in rheumatoid arthritis react specifically with the glycine alanine repeat sequence of Epstein-Barr nuclear antigen-1. Rheumatol Int (1989) 9:161–6. [PubMed] [Google Scholar]
- 148.Patarca R, Fletcher MA. Structure and pathophysiology of the erythrocyte membrane-associated Paul-Bunnell heterophile antibody determinant in Epstein-Barr virus-associated disease. Crit Rev Oncog (1995) 6:305–26. 10.1615/CritRevOncog.v6.i3-6.70 [DOI] [PubMed] [Google Scholar]
- 149.Fletcher MA, Klimas NG, Latif ZA, Caldwell KE. Serodiagnosis of infectious mononucleosis with a bovine erythrocyte glycoprotein. J Clin Microbiol (1983) 18:495–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Fletcher MA, Lo TM, Graves WR. Immunochemical studies of infectious mononucleosis. VII. Isolation and partial characterization of a glycopeptide from bovine erythrocytes. Vox Sang (1977) 33:150–63. 10.1159/000467504 [DOI] [PubMed] [Google Scholar]
- 151.Tedder TF, Leonard WJ. Autoimmunity: regulatory B cells – IL-35 and IL-21 regulate the regulators. Nat Rev Rheumatol (2014) 10:452–3. 10.1038/nrrheum.2014.95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Lunemann JD, Munz C. Epstein-Barr virus and multiple sclerosis. Curr Neurol Neurosci Rep (2007) 7:253–8. 10.1007/s11910-007-0038-y [DOI] [PubMed] [Google Scholar]
- 153.Marquez AC, Horwitz MS. The role of latently infected B cells in CNS autoimmunity. Front Immunol (2015) 6:544. 10.3389/fimmu.2015.00544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Posnett DN. Herpesviruses and autoimmunity. Curr Opin Investig Drugs (2008) 9:505–14. [PubMed] [Google Scholar]
- 155.Cuomo L, Cirone M, Di Gregorio AO, Vitillo M, Cattivelli M, Magliocca V, et al. Elevated antinuclear antibodies and altered anti-Epstein-Barr virus immune responses. Virus Res (2015) 195:95–9. 10.1016/j.virusres.2014.09.014 [DOI] [PubMed] [Google Scholar]
- 156.Nelson P, Rylance P, Roden D, Trela M, Tugnet N. Viruses as potential pathogenic agents in systemic lupus erythematosus. Lupus (2014) 23:596–605. 10.1177/0961203314531637 [DOI] [PubMed] [Google Scholar]
- 157.Niller HH, Wolf H, Ay E, Minarovits J. Epigenetic dysregulation of epstein-barr virus latency and development of autoimmune disease. Adv Exp Med Biol (2011) 711:82–102. 10.1007/978-1-4419-8216-2_7 [DOI] [PubMed] [Google Scholar]
- 158.Fust G. The role of the Epstein-Barr virus in the pathogenesis of some autoimmune disorders – similarities and differences. Eur J Microbiol Immunol (Bp) (2011) 1:267–78. 10.1556/EuJMI.1.2011.4.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Lindsey JW, deGannes SL, Pate KA, Zhao X. Antibodies specific for Epstein-Barr virus nuclear antigen-1 cross-react with human heterogeneous nuclear ribonucleoprotein L. Mol Immunol (2016) 69:7–12. 10.1016/j.molimm.2015.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Elliott SE, Parchim NF, Kellems RE, Xia Y, Soffici AR, Daugherty PS. A pre-eclampsia-associated Epstein-Barr virus antibody cross-reacts with placental GPR50. Clin Immunol (2016) 168:64–71. 10.1016/j.clim.2016.05.002 [DOI] [PubMed] [Google Scholar]
- 161.Wallis AL. An unusual epidemic. Lancet (1955) 269:290. 10.1016/S0140-6736(55)92711-2 [DOI] [PubMed] [Google Scholar]
- 162.Endresen GK. [Systemic Mycoplasma blood infection in fibromyalgia and chronic fatigue syndrome]. Tidsskr Nor Laegeforen (2004) 124:203–5. [PubMed] [Google Scholar]
- 163.Vernon SD, Shukla SK, Reeves WC. Absence of Mycoplasma species DNA in chronic fatigue syndrome. J Med Microbiol (2003) 52:1027–8. 10.1099/jmm.0.05316-0 [DOI] [PubMed] [Google Scholar]
- 164.Nicolson GL, Gan R, Haier J. Multiple co-infections (Mycoplasma, Chlamydia, human herpes virus-6) in blood of chronic fatigue syndrome patients: association with signs and symptoms. APMIS (2003) 111:557–66. 10.1034/j.1600-0463.2003.1110504.x [DOI] [PubMed] [Google Scholar]
- 165.Endresen GK. Mycoplasma blood infection in chronic fatigue and fibromyalgia syndromes. Rheumatol Int (2003) 23:211–5. 10.1007/s00296-003-0355-7 [DOI] [PubMed] [Google Scholar]
- 166.Vojdani A, Choppa PC, Tagle C, Andrin R, Samimi B, Lapp CW. Detection of Mycoplasma genus and Mycoplasma fermentans by PCR in patients with chronic fatigue syndrome. FEMS Immunol Med Microbiol (1998) 22:355–65. 10.1111/j.1574-695X.1998.tb01226.x [DOI] [PubMed] [Google Scholar]
- 167.Choppa PC, Vojdani A, Tagle C, Andrin R, Magtoto L. Multiplex PCR for the detection of Mycoplasma fermentans, M. hominis and M. penetrans in cell cultures and blood samples of patients with chronic fatigue syndrome. Mol Cell Probes (1998) 12:301–8. 10.1006/mcpr.1998.0186 [DOI] [PubMed] [Google Scholar]
- 168.Komaroff AL, Bell DS, Cheney PR, Lo SC. Absence of antibody to Mycoplasma fermentans in patients with chronic fatigue syndrome. Clin Infect Dis (1993) 17:1074–5. 10.1093/clinids/17.6.1074 [DOI] [PubMed] [Google Scholar]
- 169.Chia JK, Chia LY. Chronic Chlamydia pneumoniae infection: a treatable cause of chronic fatigue syndrome. Clin Infect Dis (1999) 29:452–3. 10.1086/520239 [DOI] [PubMed] [Google Scholar]
- 170.Komaroff AL, Wang SP, Lee J, Grayston JT. No association of chronic Chlamydia pneumoniae infection with chronic fatigue syndrome. J Infect Dis (1992) 165:184. 10.1093/infdis/165.1.184 [DOI] [PubMed] [Google Scholar]
- 171.Kerr JR. The role of parvovirus B19 in the pathogenesis of autoimmunity and autoimmune disease. J Clin Pathol (2016) 69:279–91. 10.1136/jclinpath-2015-203455 [DOI] [PubMed] [Google Scholar]
- 172.Binder CJ, Horkko S, Dewan A, Chang MK, Kieu EP, Goodyear CS, et al. Pneumococcal vaccination decreases atherosclerotic lesion formation: molecular mimicry between Streptococcus pneumoniae and oxidized LDL. Nat Med (2003) 9:736–43. 10.1038/nm876 [DOI] [PubMed] [Google Scholar]
- 173.Moens U, Van Ghelue M, Song X, Ehlers B. Serological cross-reactivity between human polyomaviruses. Rev Med Virol (2013) 23:250–64. 10.1002/rmv.1747 [DOI] [PubMed] [Google Scholar]
- 174.Van Ghelue M, Khan MT, Ehlers B, Moens U. Genome analysis of the new human polyomaviruses. Rev Med Virol (2012) 22:354–77. 10.1002/rmv.1711 [DOI] [PubMed] [Google Scholar]
- 175.Berry M, Gamieldien J, Fielding BC. Identification of new respiratory viruses in the new millennium. Viruses (2015) 7:996–1019. 10.3390/v7030996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Fallahi P, Ferrari SM, Vita R, Benvenga S, Antonelli A. The role of human parvovirus B19 and hepatitis C virus in the development of thyroid disorders. Rev Endocr Metab Disord (2016) 17:529–35. 10.1007/s11154-016-9361-4 [DOI] [PubMed] [Google Scholar]
- 177.Young JC, Chehoud C, Bittinger K, Bailey A, Diamond JM, Cantu E, et al. Viral metagenomics reveal blooms of anelloviruses in the respiratory tract of lung transplant recipients. Am J Transplant (2015) 15:200–9. 10.1111/ajt.13031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Gorzer I, Jaksch P, Kundi M, Seitz T, Klepetko W, Puchhammer-Stockl E. Pre-transplant plasma Torque Teno virus load and increase dynamics after lung transplantation. PLoS One (2015) 10:e0122975. 10.1371/journal.pone.0122975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Walton AH, Muenzer JT, Rasche D, Boomer JS, Sato B, Brownstein BH, et al. Reactivation of multiple viruses in patients with sepsis. PLoS One (2014) 9:e98819. 10.1371/journal.pone.0098819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Chen RC, Naiyanetr P, Shu SA, Wang J, Yang GX, Kenny TP, et al. Antimitochondrial antibody heterogeneity and the xenobiotic etiology of primary biliary cirrhosis. Hepatology (2013) 57:1498–508. 10.1002/hep.26157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Kaplan MM. Novosphingobium aromaticivorans: a potential initiator of primary biliary cirrhosis. Am J Gastroenterol (2004) 99:2147–9. 10.1111/j.1572-0241.2004.41121.x [DOI] [PubMed] [Google Scholar]
- 182.Smyk DS, Rigopoulou EI, Bogdanos DP. Potential roles for infectious agents in the pathophysiology of primary biliary cirrhosis: what’s new? Curr Infect Dis Rep (2013) 15:14–24. 10.1007/s11908-012-0304-2 [DOI] [PubMed] [Google Scholar]
- 183.Konig MF, Abusleme L, Reinholdt J, Palmer RJ, Teles RP, Sampson K, et al. Aggregatibacter actinomycetemcomitans-induced hypercitrullination links periodontal infection to autoimmunity in rheumatoid arthritis. Sci Transl Med (2016) 8:369ra176. 10.1126/scitranslmed.aaj1921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Bardsen K, Nilsen MM, Kvaloy JT, Norheim KB, Jonsson G, Omdal R. Heat shock proteins and chronic fatigue in primary Sjogren’s syndrome. Innate Immun (2016) 22:162–7. 10.1177/1753425916633236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Zilaee M, Ferns GA, Ghayour-Mobarhan M. Heat shock proteins and cardiovascular disease. Adv Clin Chem (2014) 64:73–115. 10.1016/B978-0-12-800263-6.00002-1 [DOI] [PubMed] [Google Scholar]
- 186.Rai R, Chauhan SK, Singh VV, Rai M, Rai G. Heat shock protein 27 and its regulatory molecules express differentially in SLE patients with distinct autoantibody profiles. Immunol Lett (2015) 164:25–32. 10.1016/j.imlet.2015.01.007 [DOI] [PubMed] [Google Scholar]
- 187.Shukla HD, Pitha PM. Role of hsp90 in systemic lupus erythematosus and its clinical relevance. Autoimmune Dis (2012) 2012:728605. 10.1155/2012/728605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Komiya I, Arimura Y, Nakabayashi K, Yamada A, Osaki T, Yamaguchi H, et al. Increased concentrations of antibody against heat shock protein in patients with myeloperoxidase anti-neutrophil cytoplasmic autoantibody positive microscopic polyangiitis. Microbiol Immunol (2011) 55:531–8. 10.1111/j.1348-0421.2011.00351.x [DOI] [PubMed] [Google Scholar]
- 189.Rothstein TL, Quach TD. The human counterpart of mouse B-1 cells. Ann N Y Acad Sci (2015) 1362:143–52. 10.1111/nyas.12790 [DOI] [PubMed] [Google Scholar]
- 190.Baumgarth N. B-1 cell heterogeneity and the regulation of natural and antigen-induced IgM production. Front Immunol (2016) 7:324. 10.3389/fimmu.2016.00324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Giloteaux L, Hanson MR, Keller BA. A pair of identical twins discordant for myalgic encephalomyelitis/chronic fatigue syndrome differ in physiological parameters and gut microbiome composition. Am J Case Rep (2016) 17:720–9. 10.12659/AJCR.900314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Giloteaux L, Goodrich JK, Walters WA, Levine SM, Ley RE, Hanson MR. Reduced diversity and altered composition of the gut microbiome in individuals with myalgic encephalomyelitis/chronic fatigue syndrome. Microbiome (2016) 4:30. 10.1186/s40168-016-0171-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Buchwald D, Ashley RL, Pearlman T, Kith P, Komaroff AL. Viral serologies in patients with chronic fatigue and chronic fatigue syndrome. J Med Virol (1996) 50:25–30. [DOI] [PubMed] [Google Scholar]
- 194.Morris G, Berk M, Walder K, Maes M. Central pathways causing fatigue in neuro-inflammatory and autoimmune illnesses. BMC Med (2015) 13:28. 10.1186/s12916-014-0259-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Nakatomi Y, Mizuno K, Ishii A, Wada Y, Tanaka M, Tazawa S, et al. Neuroinflammation in patients with chronic fatigue syndrome/myalgic encephalomyelitis: an (1)(1)C-(R)-PK11195 PET study. J Nucl Med (2014) 55:945–50. 10.2967/jnumed.113.131045 [DOI] [PubMed] [Google Scholar]
- 196.Chistiakov DA, Bobryshev YV, Kozarov E, Sobenin IA, Orekhov AN. Intestinal mucosal tolerance and impact of gut microbiota to mucosal tolerance. Front Microbiol (2014) 5:781. 10.3389/fmicb.2014.00781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.de Goffau MC, Luopajarvi K, Knip M, Ilonen J, Ruohtula T, Harkonen T, et al. Fecal microbiota composition differs between children with beta-cell autoimmunity and those without. Diabetes (2013) 62:1238–44. 10.2337/db12-0526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Mejia-Leon ME, Petrosino JF, Ajami NJ, Dominguez-Bello MG, de la Barca AM. Fecal microbiota imbalance in Mexican children with type 1 diabetes. Sci Rep (2014) 4:3814. 10.1038/srep03814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Chen J, Chia N, Kalari KR, Yao JZ, Novotna M, Soldan MM, et al. Multiple sclerosis patients have a distinct gut microbiota compared to healthy controls. Sci Rep (2016) 6:28484. 10.1038/srep28484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Scher JU, Sczesnak A, Longman RS, Segata N, Ubeda C, Bielski C, et al. Expansion of intestinal Prevotella copri correlates with enhanced susceptibility to arthritis. Elife (2013) 2:e01202. 10.7554/eLife.01202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.He Z, Shao T, Li H, Xie Z, Wen C. Alterations of the gut microbiome in Chinese patients with systemic lupus erythematosus. Gut Pathog (2016) 8:64. 10.1186/s13099-016-0146-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Consolandi C, Turroni S, Emmi G, Severgnini M, Fiori J, Peano C, et al. Behcet’s syndrome patients exhibit specific microbiome signature. Autoimmun Rev (2015) 14:269–76. 10.1016/j.autrev.2014.11.009 [DOI] [PubMed] [Google Scholar]
- 203.D’Elios MM, Appelmelk BJ, Amedei A, Bergman MP, Del Prete G. Gastric autoimmunity: the role of Helicobacter pylori and molecular mimicry. Trends Mol Med (2004) 10:316–23. 10.1016/j.molmed.2004.06.001 [DOI] [PubMed] [Google Scholar]
- 204.Wen C, Zheng Z, Shao T, Liu L, Xie Z, Le Chatelier E, et al. Quantitative metagenomics reveals unique gut microbiome biomarkers in ankylosing spondylitis. Genome Biol (2017) 18:142. 10.1186/s13059-017-1271-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Billing-Ross P, Germain A, Ye K, Keinan A, Gu Z, Hanson MR. Mitochondrial DNA variants correlate with symptoms in myalgic encephalomyelitis/chronic fatigue syndrome. J Transl Med (2016) 14:19. 10.1186/s12967-016-0771-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Wallis A, Butt H, Ball M, Lewis DP, Bruck D. Support for the microgenderome: associations in a human clinical population. Sci Rep (2016) 6:19171. 10.1038/srep19171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Ford AC, Talley NJ. Mucosal inflammation as a potential etiological factor in irritable bowel syndrome: a systematic review. J Gastroenterol (2011) 46:421–31. 10.1007/s00535-011-0379-9 [DOI] [PubMed] [Google Scholar]
- 208.Fukuda S, Nojima J, Kajimoto O, Yamaguti K, Nakatomi Y, Kuratsune H, et al. Ubiquinol-10 supplementation improves autonomic nervous function and cognitive function in chronic fatigue syndrome. Biofactors (2016) 42:431–40. 10.1002/biof.1293 [DOI] [PubMed] [Google Scholar]
- 209.Kell DB, Pretorius E. On the translocation of bacteria and their lipopolysaccharides between blood and peripheral locations in chronic, inflammatory diseases: the central roles of LPS and LPS-induced cell death. Integr Biol (Camb) (2015) 7:1339–77. 10.1039/c5ib00158g [DOI] [PubMed] [Google Scholar]
- 210.Hollander D. Intestinal permeability, leaky gut, and intestinal disorders. Curr Gastroenterol Rep (1999) 1:410–6. 10.1007/s11894-999-0023-5 [DOI] [PubMed] [Google Scholar]
- 211.Odenwald MA, Turner JR. Intestinal permeability defects: is it time to treat? Clin Gastroenterol Hepatol (2013) 11:1075–83. 10.1016/j.cgh.2013.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Anders HJ, Andersen K, Stecher B. The intestinal microbiota, a leaky gut, and abnormal immunity in kidney disease. Kidney Int (2013) 83:1010–6. 10.1038/ki.2012.440 [DOI] [PubMed] [Google Scholar]
- 213.Gecse K, Roka R, Sera T, Rosztoczy A, Annahazi A, Izbeki F, et al. Leaky gut in patients with diarrhea-predominant irritable bowel syndrome and inactive ulcerative colitis. Digestion (2012) 85:40–6. 10.1159/000333083 [DOI] [PubMed] [Google Scholar]
- 214.Montoya JG, Kogelnik AM, Bhangoo M, Lunn MR, Flamand L, Merrihew LE, et al. Randomized clinical trial to evaluate the efficacy and safety of valganciclovir in a subset of patients with chronic fatigue syndrome. J Med Virol (2013) 85:2101–9. 10.1002/jmv.23713 [DOI] [PubMed] [Google Scholar]
- 215.Watt T, Oberfoell S, Balise R, Lunn MR, Kar AK, Merrihew L, et al. Response to valganciclovir in chronic fatigue syndrome patients with human herpesvirus 6 and Epstein-Barr virus IgG antibody titers. J Med Virol (2012) 84:1967–74. 10.1002/jmv.23411 [DOI] [PubMed] [Google Scholar]
- 216.Hokama Y, Campora CE, Hara C, Kuribayashi T, Le Huynh D, Yabusaki K. Anticardiolipin antibodies in the sera of patients with diagnosed chronic fatigue syndrome. J Clin Lab Anal (2009) 23:210–2. 10.1002/jcla.20325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Hokama Y, Empey-Campora C, Hara C, Higa N, Siu N, Lau R, et al. Acute phase phospholipids related to the cardiolipin of mitochondria in the sera of patients with chronic fatigue syndrome (CFS), chronic Ciguatera fish poisoning (CCFP), and other diseases attributed to chemicals, Gulf War, and marine toxins. J Clin Lab Anal (2008) 22:99–105. 10.1002/jcla.20217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Morris G, Berk M, Galecki P, Maes M. The emerging role of autoimmunity in myalgic encephalomyelitis/chronic fatigue syndrome (ME/cfs). Mol Neurobiol (2014) 49:741–56. 10.1007/s12035-013-8553-0 [DOI] [PubMed] [Google Scholar]
- 219.Ortega-Hernandez OD, Cuccia M, Bozzini S, Bassi N, Moscavitch S, Diaz-Gallo LM, et al. Autoantibodies, polymorphisms in the serotonin pathway, and human leukocyte antigen class II alleles in chronic fatigue syndrome: are they associated with age at onset and specific symptoms? Ann N Y Acad Sci (2009) 1173:589–99. 10.1111/j.1749-6632.2009.04802.x [DOI] [PubMed] [Google Scholar]
- 220.Lorusso L, Mikhaylova SV, Capelli E, Ferrari D, Ngonga GK, Ricevuti G. Immunological aspects of chronic fatigue syndrome. Autoimmun Rev (2009) 8:287–91. 10.1016/j.autrev.2008.08.003 [DOI] [PubMed] [Google Scholar]
- 221.Nancy AL, Shoenfeld Y. Chronic fatigue syndrome with autoantibodies – the result of an augmented adjuvant effect of hepatitis-B vaccine and silicone implant. Autoimmun Rev (2008) 8:52–5. 10.1016/j.autrev.2008.07.026 [DOI] [PubMed] [Google Scholar]
- 222.Staines DR. Is chronic fatigue syndrome an autoimmune disorder of endogenous neuropeptides, exogenous infection and molecular mimicry? Med Hypotheses (2004) 62:646–52. 10.1016/j.mehy.2004.01.010 [DOI] [PubMed] [Google Scholar]
- 223.Landi A, Broadhurst D, Vernon SD, Tyrrell DL, Houghton M. Reductions in circulating levels of IL-16, IL-7 and VEGF-A in myalgic encephalomyelitis/chronic fatigue syndrome. Cytokine (2016) 78:27–36. 10.1016/j.cyto.2015.11.018 [DOI] [PubMed] [Google Scholar]
- 224.Hornig M, Gottschalk CG, Eddy ML, Che X, Ukaigwe JE, Peterson DL, et al. Immune network analysis of cerebrospinal fluid in myalgic encephalomyelitis/chronic fatigue syndrome with atypical and classical presentations. Transl Psychiatry (2017) 7:e1080. 10.1038/tp.2017.44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Hornig M, Montoya JG, Klimas NG, Levine S, Felsenstein D, Bateman L, et al. Distinct plasma immune signatures in ME/CFS are present early in the course of illness. Sci Adv (2015) 1:1–10. 10.1126/sciadv.1400121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Montoya JG, Holmes TH, Anderson JN, Maecker HT, Rosenberg-Hasson Y, Valencia IJ, et al. Cytokine signature associated with disease severity in chronic fatigue syndrome patients. Proc Natl Acad Sci U S A (2017) 114:E7150–8. 10.1073/pnas.1710519114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Blundell S, Ray KK, Buckland M, White PD. Chronic fatigue syndrome and circulating cytokines: a systematic review. Brain Behav Immun (2015) 50:186–95. 10.1016/j.bbi.2015.07.004 [DOI] [PubMed] [Google Scholar]
- 228.Peterson D, Brenu EW, Gottschalk G, Ramos S, Nguyen T, Staines D, et al. Cytokines in the cerebrospinal fluids of patients with chronic fatigue syndrome/myalgic encephalomyelitis. Mediators Inflamm (2015) 2015:929720. 10.1155/2015/929720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Hardcastle SL, Brenu EW, Johnston S, Nguyen T, Huth T, Ramos S, et al. Longitudinal analysis of immune abnormalities in varying severities of chronic fatigue syndrome/myalgic encephalomyelitis patients. J Transl Med (2015) 13:299. 10.1186/s12967-015-0653-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Stringer EA, Baker KS, Carroll IR, Montoya JG, Chu L, Maecker HT, et al. Daily cytokine fluctuations, driven by leptin, are associated with fatigue severity in chronic fatigue syndrome: evidence of inflammatory pathology. J Transl Med (2013) 11:93. 10.1186/1479-5876-11-93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Brenu EW, van Driel ML, Staines DR, Ashton KJ, Ramos SB, Keane J, et al. Immunological abnormalities as potential biomarkers in chronic fatigue syndrome/myalgic encephalomyelitis. J Transl Med (2011) 9:81. 10.1186/1479-5876-9-81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.James K, Al-Ali S, Tarn J, Cockell SJ, Gillespie CS, Hindmarsh V, et al. A transcriptional signature of fatigue derived from patients with Primary Sjogren’s syndrome. PLoS One (2015) 10:e0143970. 10.1371/journal.pone.0143970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Nijs J, Nees A, Paul L, De Kooning M, Ickmans K, Meeus M, et al. Altered immune response to exercise in patients with chronic fatigue syndrome/myalgic encephalomyelitis: a systematic literature review. Exerc Immunol Rev (2014) 20:94–116. [PubMed] [Google Scholar]
- 234.Light KC, Agarwal N, Iacob E, White AT, Kinney AY, VanHaitsma TA, et al. Differing leukocyte gene expression profiles associated with fatigue in patients with prostate cancer versus chronic fatigue syndrome. Psychoneuroendocrinology (2013) 38:2983–95. 10.1016/j.psyneuen.2013.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.White AT, Light AR, Hughen RW, Vanhaitsma TA, Light KC. Differences in metabolite-detecting, adrenergic, and immune gene expression after moderate exercise in patients with chronic fatigue syndrome, patients with multiple sclerosis, and healthy controls. Psychosom Med (2012) 74:46–54. 10.1097/PSY.0b013e31824152ed [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Light AR, Bateman L, Jo D, Hughen RW, Vanhaitsma TA, White AT, et al. Gene expression alterations at baseline and following moderate exercise in patients with chronic fatigue syndrome and fibromyalgia syndrome. J Intern Med (2012) 271:64–81. 10.1111/j.1365-2796.2011.02405.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.White AT, Light AR, Hughen RW, Bateman L, Martins TB, Hill HR, et al. Severity of symptom flare after moderate exercise is linked to cytokine activity in chronic fatigue syndrome. Psychophysiology (2010) 47:615–24. 10.1111/j.1469-8986.2010.00978.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Light AR, White AT, Hughen RW, Light KC. Moderate exercise increases expression for sensory, adrenergic, and immune genes in chronic fatigue syndrome patients but not in normal subjects. J Pain (2009) 10:1099–112. 10.1016/j.jpain.2009.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Jammes Y, Steinberg JG, Delliaux S. Chronic fatigue syndrome: acute infection and history of physical activity affect resting levels and response to exercise of plasma oxidant/antioxidant status and heat shock proteins. J Intern Med (2012) 272:74–84. 10.1111/j.1365-2796.2011.02488.x [DOI] [PubMed] [Google Scholar]
- 240.Hornig M, Gottschalk G, Peterson DL, Knox KK, Schultz AF, Eddy ML, et al. Cytokine network analysis of cerebrospinal fluid in myalgic encephalomyelitis/chronic fatigue syndrome. Mol Psychiatry (2016) 21:261–9. 10.1038/mp.2015.29 [DOI] [PubMed] [Google Scholar]
- 241.Clark LV, Buckland M, Murphy G, Taylor N, Vleck V, Mein C, et al. Cytokine responses to exercise and activity in patients with chronic fatigue syndrome: case-control study. Clin Exp Immunol (2017) 190:360–71. 10.1111/cei.13023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Russell L, Broderick G, Taylor R, Fernandes H, Harvey J, Barnes Z, et al. Illness progression in chronic fatigue syndrome: a shifting immune baseline. BMC Immunol (2016) 17:3. 10.1186/s12865-016-0142-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Keijmel SP, Raijmakers RP, Bleeker-Rovers CP, van der Meer JW, Netea MG, Schoffelen T, et al. Altered interferon-gamma response in patients with Q-fever fatigue syndrome. J Infect (2016) 72:478–85. 10.1016/j.jinf.2016.01.004 [DOI] [PubMed] [Google Scholar]
- 244.Smylie AL, Broderick G, Fernandes H, Razdan S, Barnes Z, Collado F, et al. A comparison of sex-specific immune signatures in Gulf War illness and chronic fatigue syndrome. BMC Immunol (2013) 14:29. 10.1186/1471-2172-14-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Petty RD, McCarthy NE, Le Dieu R, Kerr JR. MicroRNAs hsa-miR-99b, hsa-miR-330, hsa-miR-126 and hsa-miR-30c: potential diagnostic biomarkers in natural killer (NK) cells of patients with chronic fatigue syndrome (CFS)/myalgic encephalomyelitis (ME). PLoS One (2016) 11:e0150904. 10.1371/journal.pone.0150904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Brenu EW, van Driel ML, Staines DR, Ashton KJ, Hardcastle SL, Keane J, et al. Longitudinal investigation of natural killer cells and cytokines in chronic fatigue syndrome/myalgic encephalomyelitis. J Transl Med (2012) 10:88. 10.1186/1479-5876-10-88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Klimas NG, Koneru AO. Chronic fatigue syndrome: inflammation, immune function, and neuroendocrine interactions. Curr Rheumatol Rep (2007) 9:482–7. 10.1007/s11926-007-0078-y [DOI] [PubMed] [Google Scholar]
- 248.Brenu EW, Ashton KJ, van Driel M, Staines DR, Peterson D, Atkinson GM, et al. Cytotoxic lymphocyte microRNAs as prospective biomarkers for chronic fatigue syndrome/myalgic encephalomyelitis. J Affect Disord (2012) 141:261–9. 10.1016/j.jad.2012.03.037 [DOI] [PubMed] [Google Scholar]
- 249.Theorell J, Bileviciute-Ljungar I, Tesi B, Schlums H, Johnsgaard MS, Asadi-Azarbaijani B, et al. Unperturbed cytotoxic lymphocyte phenotype and function in myalgic encephalomyelitis/chronic fatigue syndrome patients. Front Immunol (2017) 8:723. 10.3389/fimmu.2017.00723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Calabrese LH, Davis ME, Wilke WS. Chronic fatigue syndrome and a disorder resembling Sjogren’s syndrome: preliminary report. Clin Infect Dis (1994) 18(Suppl 1):S28–31. 10.1093/clinids/18.Supplement_1.S28 [DOI] [PubMed] [Google Scholar]
- 251.Morris G, Maes M. Myalgic encephalomyelitis/chronic fatigue syndrome and encephalomyelitis disseminata/multiple sclerosis show remarkable levels of similarity in phenomenology and neuroimmune characteristics. BMC Med (2013) 11:205. 10.1186/1741-7015-11-205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Klimas NG, Broderick G, Fletcher MA. Biomarkers for chronic fatigue. Brain Behav Immun (2012) 26:1202–10. 10.1016/j.bbi.2012.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Norheim KB, Jonsson G, Omdal R. Biological mechanisms of chronic fatigue. Rheumatology (Oxford) (2011) 50:1009–18. 10.1093/rheumatology/keq454 [DOI] [PubMed] [Google Scholar]
- 254.Nijs J, Van Oosterwijck J, Meeus M, Lambrecht L, Metzger K, Fremont M, et al. Unravelling the nature of postexertional malaise in myalgic encephalomyelitis/chronic fatigue syndrome: the role of elastase, complement C4a and interleukin-1beta. J Intern Med (2010) 267:418–35. 10.1111/j.1365-2796.2009.02178.x [DOI] [PubMed] [Google Scholar]
- 255.Stein E, MacQuarrie M. Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) program and interdisciplinary research symposium on disabling fatigue in chronic illness. Chronic Dis Can (2009) 29:136–8. [PubMed] [Google Scholar]
- 256.Piche T, Gelsi E, Schneider SM, Hebuterne X, Giudicelli J, Ferrua B, et al. Fatigue is associated with high circulating leptin levels in chronic hepatitis C. Gut (2002) 51:434–9. 10.1136/gut.51.3.434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Harvey JM, Broderick G, Bowie A, Barnes ZM, Katz BZ, O’Gorman MR, et al. Tracking post-infectious fatigue in clinic using routine Lab tests. BMC Pediatr (2016) 16:54. 10.1186/s12887-016-0596-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Clark JE, Fai Ng W, Watson S, Newton JL. The aetiopathogenesis of fatigue: unpredictable, complex and persistent. Br Med Bull (2016) 117:139–48. 10.1093/bmb/ldv057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Maughan D, Toth M. Discerning primary and secondary factors responsible for clinical fatigue in multisystem diseases. Biology (Basel) (2014) 3:606–22. 10.3390/biology3030606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Light AR, Vierck CJ, Light KC. Myalgia and fatigue: translation from mouse sensory neurons to fibromyalgia and chronic fatigue syndromes. In: Kruger L, Light AR, editors. Translational Pain Research: From Mouse to Man. Boca Raton, FL: CRC Press; (2010). [PubMed] [Google Scholar]
- 261.Abbas G, Jorgensen RA, Lindor KD. Fatigue in primary biliary cirrhosis. Nat Rev Gastroenterol Hepatol (2010) 7:313–9. 10.1038/nrgastro.2010.62 [DOI] [PubMed] [Google Scholar]
- 262.Gorman GS, Elson JL, Newman J, Payne B, McFarland R, Newton JL, et al. Perceived fatigue is highly prevalent and debilitating in patients with mitochondrial disease. Neuromuscul Disord (2015) 25:563–6. 10.1016/j.nmd.2015.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Finsterer J, Ahting U. Mitochondrial depletion syndromes in children and adults. Can J Neurol Sci (2013) 40:635–44. 10.1017/S0317167100014852 [DOI] [PubMed] [Google Scholar]
- 264.Piraino B, Vollmer-Conna U, Lloyd AR. Genetic associations of fatigue and other symptom domains of the acute sickness response to infection. Brain Behav Immun (2012) 26:552–8. 10.1016/j.bbi.2011.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Proal AD, Albert PJ, Marshall TG, Blaney GP, Lindseth IA. Immunostimulation in the treatment for chronic fatigue syndrome/myalgic encephalomyelitis. Immunol Res (2013) 56:398–412. 10.1007/s12026-013-8413-z [DOI] [PubMed] [Google Scholar]
- 266.Zachrisson O, Colque-Navarro P, Gottfries CG, Regland B, Mollby R. Immune modulation with a staphylococcal preparation in fibromyalgia/chronic fatigue syndrome: relation between antibody levels and clinical improvement. Eur J Clin Microbiol Infect Dis (2004) 23:98–105. 10.1007/s10096-003-1062-8 [DOI] [PubMed] [Google Scholar]
- 267.Andersson M, Bagby JR, Dyrehag L, Gottfries C. Effects of staphylococcus toxoid vaccine on pain and fatigue in patients with fibromyalgia/chronic fatigue syndrome. Eur J Pain (1998) 2:133–42. 10.1016/S1090-3801(98)90006-4 [DOI] [PubMed] [Google Scholar]
- 268.Tedder TF. CD19: a promising B cell target for rheumatoid arthritis. Nat Rev Rheumatol (2009) 5:572–7. 10.1038/nrrheum.2009.184 [DOI] [PubMed] [Google Scholar]
- 269.Chang CM, Warren JL, Engels EA. Chronic fatigue syndrome and subsequent risk of cancer among elderly US adults. Cancer (2012) 118:5929–36. 10.1002/cncr.27612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Rose NR, Bona C. Defining criteria for autoimmune diseases (Witebsky’s postulates revisited). Immunol Today (1993) 14:426–30. 10.1016/0167-5699(93)90244-F [DOI] [PubMed] [Google Scholar]
- 271.Rutherford G, Manning P, Newton JL. Understanding muscle dysfunction in chronic fatigue syndrome. J Aging Res (2016) 2016:2497348. 10.1155/2016/2497348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Twisk FN. Accurate diagnosis of myalgic encephalomyelitis and chronic fatigue syndrome based upon objective test methods for characteristic symptoms. World J Methodol (2015) 5:68–87. 10.5662/wjm.v5.i2.68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Snell CR, Stevens SR, Davenport TE, Van Ness JM. Discriminative validity of metabolic and workload measurements for identifying people with chronic fatigue syndrome. Phys Ther (2013) 93:1484–92. 10.2522/ptj.20110368 [DOI] [PubMed] [Google Scholar]
- 274.Margulis L. Origin of Eukaryotic Cells. New Haven, CT: Yale University Press; (1970). [Google Scholar]
- 275.Fluge O, Mella O, Bruland O, Risa K, Dyrstad SE, Alme K, et al. Metabolic profiling indicates impaired pyruvate dehydrogenase function in myalgic encephalopathy/chronic fatigue syndrome. JCI Insight (2016) 1:e89376. 10.1172/jci.insight.89376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Germain A, Ruppert D, Levine SM, Hanson MR. Metabolic profiling of a myalgic encephalomyelitis/chronic fatigue syndrome discovery cohort reveals disturbances in fatty acid and lipid metabolism. Mol Biosyst (2017) 13:371–9. 10.1039/c6mb00600k [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Regland B, Andersson M, Abrahamsson L, Bagby J, Dyrehag LE, Gottfries CG. Increased concentrations of homocysteine in the cerebrospinal fluid in patients with fibromyalgia and chronic fatigue syndrome. Scand J Rheumatol (1997) 26:301–7. 10.3109/03009749709105320 [DOI] [PubMed] [Google Scholar]
- 278.Fenouillet E, Vigouroux A, Steinberg JG, Chagvardieff A, Retornaz F, Guieu R, et al. Association of biomarkers with health-related quality of life and history of stressors in myalgic encephalomyelitis/chronic fatigue syndrome patients. J Transl Med (2016) 14:251. 10.1186/s12967-016-1010-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Yamano E, Sugimoto M, Hirayama A, Kume S, Yamato M, Jin G, et al. Index markers of chronic fatigue syndrome with dysfunction of TCA and urea cycles. Sci Rep (2016) 6:34990. 10.1038/srep34990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Naviaux RK, Naviaux JC, Li K, Bright AT, Alaynick WA, Wang L, et al. Metabolic features of chronic fatigue syndrome. Proc Natl Acad Sci U S A (2016) 113:E5472–80. 10.1073/pnas.1607571113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Shungu DC, Weiduschat N, Murrough JW, Mao X, Pillemer S, Dyke JP, et al. Increased ventricular lactate in chronic fatigue syndrome. III. Relationships to cortical glutathione and clinical symptoms implicate oxidative stress in disorder pathophysiology. NMR Biomed (2012) 25:1073–87. 10.1002/nbm.2772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Armstrong CW, McGregor NR, Butt HL, Gooley PR. Metabolism in chronic fatigue syndrome. Adv Clin Chem (2014) 66:121–72. 10.1016/B978-0-12-801401-1.00005-0 [DOI] [PubMed] [Google Scholar]
- 283.Ciregia F, Kollipara L, Giusti L, Zahedi RP, Giacomelli C, Mazzoni MR, et al. Bottom-up proteomics suggests an association between differential expression of mitochondrial proteins and chronic fatigue syndrome. Transl Psychiatry (2016) 6:e904. 10.1038/tp.2016.184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Armstrong CW, McGregor NR, Sheedy JR, Buttfield I, Butt HL, Gooley PR. NMR metabolic profiling of serum identifies amino acid disturbances in chronic fatigue syndrome. Clin Chim Acta (2012) 413:1525–31. 10.1016/j.cca.2012.06.022 [DOI] [PubMed] [Google Scholar]
- 285.Myhill S, Booth NE, McLaren-Howard J. Targeting mitochondrial dysfunction in the treatment of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) – a clinical audit. Int J Clin Exp Med (2013) 6:1–15. [PMC free article] [PubMed] [Google Scholar]
- 286.Booth NE, Myhill S, McLaren-Howard J. Mitochondrial dysfunction and the pathophysiology of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Int J Clin Exp Med (2012) 5:208–20. [PMC free article] [PubMed] [Google Scholar]
- 287.Purohit T, Cappell MS. Primary biliary cirrhosis: pathophysiology, clinical presentation and therapy. World J Hepatol (2015) 7:926–41. 10.4254/wjh.v7.i7.926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Zavala-Cerna MG, Martinez-Garcia EA, Torres-Bugarin O, Rubio-Jurado B, Riebeling C, Nava A. The clinical significance of posttranslational modification of autoantigens. Clin Rev Allergy Immunol (2014) 47:73–90. 10.1007/s12016-014-8424-0 [DOI] [PubMed] [Google Scholar]
- 289.Wang L, Wang FS, Chang C, Gershwin ME. Breach of tolerance: primary biliary cirrhosis. Semin Liver Dis (2014) 34:297–317. 10.1055/s-0034-1383729 [DOI] [PubMed] [Google Scholar]
- 290.Juran BD, Lazaridis KN. Environmental factors in primary biliary cirrhosis. Semin Liver Dis (2014) 34:265–72. 10.1055/s-0034-1383726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Christen U, Hintermann E. Pathogen infection as a possible cause for autoimmune hepatitis. Int Rev Immunol (2014) 33:296–313. 10.3109/08830185.2014.921162 [DOI] [PubMed] [Google Scholar]
- 292.Kadaja L, Kisand KE, Peet N, Braun U, Metskula K, Teesalu K, et al. IgG from patients with liver diseases inhibit mitochondrial respiration in permeabilized oxidative muscle cells: impaired function of intracellular energetic units? Mol Cell Biochem (2004) 256-257(1–2):291–303. 10.1023/B:MCBI.0000009876.23921.e6 [DOI] [PubMed] [Google Scholar]
- 293.Torrente-Segarra V, Salman-Monte TC, Rua-Figueroa I, Perez-Vicente S, Lopez-Longo FJ, Galindo-Izquierdo M, et al. Fibromyalgia prevalence and related factors in a large registry of patients with systemic lupus erythematosus. Clin Exp Rheumatol (2016) 34:40–7. [PubMed] [Google Scholar]
- 294.Giacomelli C, Talarico R, Baldini C, Bazzichi L. Pain in Sjogren’s syndrome. Reumatismo (2014) 66:39–43. 10.4081/reumatismo.2014.763 [DOI] [PubMed] [Google Scholar]
- 295.Fox RI. Sjogren’s syndrome. Lancet (2005) 366:321–31. 10.1016/S0140-6736(05)66990-5 [DOI] [PubMed] [Google Scholar]
- 296.Bonafede RP, Downey DC, Bennett RM. An association of fibromyalgia with primary Sjogren’s syndrome: a prospective study of 72 patients. J Rheumatol (1995) 22:133–6. [PubMed] [Google Scholar]
- 297.Donmez S, Pamuk ON, Umit EG, Top MS. Autoimmune rheumatic disease associated symptoms in fibromyalgia patients and their influence on anxiety, depression and somatisation: a comparative study. Clin Exp Rheumatol (2012) 30:65–9. [PubMed] [Google Scholar]
- 298.Aaron LA, Burke MM, Buchwald D. Overlapping conditions among patients with chronic fatigue syndrome, fibromyalgia, and temporomandibular disorder. Arch Intern Med (2000) 160:221–7. 10.1001/archinte.160.2.221 [DOI] [PubMed] [Google Scholar]
- 299.Gerdle B, Forsgren MF, Bengtsson A, Leinhard OD, Soren B, Karlsson A, et al. Decreased muscle concentrations of ATP and PCR in the quadriceps muscle of fibromyalgia patients – a 31P-MRS study. Eur J Pain (2013) 17:1205–15. 10.1002/j.1532-2149.2013.00284.x [DOI] [PubMed] [Google Scholar]
- 300.Lund E, Kendall SA, Janerot-Sjoberg B, Bengtsson A. Muscle metabolism in fibromyalgia studied by P-31 magnetic resonance spectroscopy during aerobic and anaerobic exercise. Scand J Rheumatol (2003) 32:138–45. 10.1080/03009740310002461 [DOI] [PubMed] [Google Scholar]
- 301.Cook DB, O’Connor PJ, Lange G, Steffener J. Functional neuroimaging correlates of mental fatigue induced by cognition among chronic fatigue syndrome patients and controls. Neuroimage (2007) 36:108–22. 10.1016/j.neuroimage.2007.02.033 [DOI] [PubMed] [Google Scholar]
- 302.Keech A, Sandler CX, Vollmer-Conna U, Cvejic E, Lloyd AR, Barry BK. Capturing the post-exertional exacerbation of fatigue following physical and cognitive challenge in patients with chronic fatigue syndrome. J Psychosom Res (2015) 79:537–49. 10.1016/j.jpsychores.2015.08.008 [DOI] [PubMed] [Google Scholar]
- 303.Murrough JW, Mao X, Collins KA, Kelly C, Andrade G, Nestadt P, et al. Increased ventricular lactate in chronic fatigue syndrome measured by 1H MRS imaging at 3.0 T. II: comparison with major depressive disorder. NMR Biomed (2010) 23:643–50. 10.1002/nbm.1512 [DOI] [PubMed] [Google Scholar]
- 304.Rayhan RU, Raksit MP, Timbol CR, Adewuyi O, Vanmeter JW, Baraniuk JN. Prefrontal lactate predicts exercise-induced cognitive dysfunction in Gulf War Illness. Am J Transl Res (2013) 5:212–23. [PMC free article] [PubMed] [Google Scholar]
- 305.Schutzer SE, Angel TE, Liu T, Schepmoes AA, Clauss TR, Adkins JN, et al. Distinct cerebrospinal fluid proteomes differentiate post-treatment lyme disease from chronic fatigue syndrome. PLoS One (2011) 6:e17287. 10.1371/journal.pone.0017287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Regland B, Forsmark S, Halaouate L, Matousek M, Peilot B, Zachrisson O, et al. Response to vitamin B12 and folic acid in myalgic encephalomyelitis and fibromyalgia. PLoS One (2015) 10:e0124648. 10.1371/journal.pone.0124648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Prochnicki T, Mangan MS, Latz E. Recent insights into the molecular mechanisms of the NLRP3 inflammasome activation. F1000Res (2016) 5:1–15. 10.12688/f1000research.8614.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Weinberg SE, Sena LA, Chandel NS. Mitochondria in the regulation of innate and adaptive immunity. Immunity (2015) 42:406–17. 10.1016/j.immuni.2015.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Zevini A, Olagnier D, Hiscott J. Crosstalk between cytoplasmic RIG-I and STING sensing pathways. Trends Immunol (2017) 38: 194–205. 10.1016/j.it.2016.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Sandhir R, Halder A, Sunkaria A. Mitochondria as a centrally positioned hub in the innate immune response. Biochim Biophys Acta (2016) 1863:1090–7. 10.1016/j.bbadis.2016.10.020 [DOI] [PubMed] [Google Scholar]
- 311.Bender S, Reuter A, Eberle F, Einhorn E, Binder M, Bartenschlager R. Activation of type I and III interferon response by mitochondrial and peroxisomal MAVS and inhibition by hepatitis C virus. PLoS Pathog (2015) 11:e1005264. 10.1371/journal.ppat.1005264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Zeng M, Hu Z, Shi X, Li X, Zhan X, Li XD, et al. MAVS, cGAS, and endogenous retroviruses in T-independent B cell responses. Science (2014) 346:1486–92. 10.1126/science.346.6216.1486 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 313.Ding S, Robek MD. Peroxisomal MAVS activates IRF1-mediated IFN-lambda production. Nat Immunol (2014) 15:700–1. 10.1038/ni.2924 [DOI] [PubMed] [Google Scholar]
- 314.Sasaki O, Yoshizumi T, Kuboyama M, Ishihara T, Suzuki E, Kawabata S, et al. A structural perspective of the MAVS-regulatory mechanism on the mitochondrial outer membrane using bioluminescence resonance energy transfer. Biochim Biophys Acta (2013) 1833:1017–27. 10.1016/j.bbamcr.2013.01.010 [DOI] [PubMed] [Google Scholar]
- 315.Holmstrom KM, Finkel T. Cellular mechanisms and physiological consequences of redox-dependent signalling. Nat Rev Mol Cell Biol (2014) 15:411–21. 10.1038/nrm3801 [DOI] [PubMed] [Google Scholar]
- 316.Anastasiou D, Poulogiannis G, Asara JM, Boxer MB, Jiang JK, Shen M, et al. Inhibition of pyruvate kinase M2 by reactive oxygen species contributes to cellular antioxidant responses. Science (2011) 334:1278–83. 10.1126/science.1211485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Hurd TR, Collins Y, Abakumova I, Chouchani ET, Baranowski B, Fearnley IM, et al. Inactivation of pyruvate dehydrogenase kinase 2 by mitochondrial reactive oxygen species. J Biol Chem (2012) 287:35153–60. 10.1074/jbc.M112.400002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Raha S, Robinson BH. Mitochondria, oxygen free radicals, disease and ageing. Trends Biochem Sci (2000) 25:502–8. 10.1016/S0968-0004(00)01674-1 [DOI] [PubMed] [Google Scholar]
- 319.Scherz-Shouval R, Elazar Z. Monitoring starvation-induced reactive oxygen species formation. Methods Enzymol (2009) 452:119–30. 10.1016/S0076-6879(08)03608-2 [DOI] [PubMed] [Google Scholar]
- 320.Guaras A, Perales-Clemente E, Calvo E, Acin-Perez R, Loureiro-Lopez M, Pujol C, et al. The CoQH2/CoQ ratio serves as a sensor of respiratory chain efficiency. Cell Rep (2016) 15:197–209. 10.1016/j.celrep.2016.03.009 [DOI] [PubMed] [Google Scholar]
- 321.Zachrisson O, Regland B, Jahreskog M, Jonsson M, Kron M, Gottfries CG. Treatment with staphylococcus toxoid in fibromyalgia/chronic fatigue syndrome – a randomised controlled trial. Eur J Pain (2002) 6:455–66. 10.1016/S1090-3801(02)00044-7 [DOI] [PubMed] [Google Scholar]
- 322.Moutschen M, Triffaux JM, Demonty J, Legros JJ, Lefebvre PJ. Pathogenic tracks in fatigue syndromes. Acta Clin Belg (1994) 49:274–89. 10.1080/17843286.1994.11718404 [DOI] [PubMed] [Google Scholar]