Abstract
Many frequently prescribed drugs are non-genotoxic carcinogens (NGC) in rodent liver. Their mode of action and health risks for humans remain to be elucidated. Here, we investigated the impact of two model NGC, the anti-epileptic drug phenobarbital (PB) and the contraceptive cyproterone acetate (CPA), on intrahepatic epithelial–mesenchymal crosstalk and on growth of first stages of hepatocarcinogenesis. Unaltered hepatocytes (HC) and preneoplastic HC (HCPREN) were isolated from rat liver for primary culture. DNA replication of HC and HCPREN was increased by in vitro treatment with 10 µM CPA, but not 1 mM PB. Next, mesenchymal cells (MC) obtained from liver of rats treated with either PB (50 mg/kg bw/day) or CPA (100 mg/kg bw/day), were cultured. Supernatants from both types of MC raised DNA synthesis of HC and HCPREN. This indicates that PB induces replication of HC and HCPREN only indirectly, via growth factors secreted by MC. CPA, however, acts on HC and HCPREN directly as well as indirectly via mesenchymal factors. Transcriptomics and bio-informatics revealed that PB and CPA induce extensive changes in the expression profile of MC affecting many growth factors and pathways. MC from PB-treated rats produced and secreted enhanced levels of HBEGF and GDF15, factors found to suppress apoptosis and/or induce DNA synthesis in cultured HC and HCPREN. MC from CPA-treated animals showed enhanced expression and secretion of HGF, which strongly raised DNA replication of HC and HCPREN. In conclusion, our findings reveal profound effects of two prototypical NGC on the hepatic mesenchyme. The resulting release of factors, which suppress apoptosis and/or enhance cell replication preferentially in cancer prestages, appears to be crucial for tumor promotion by NGC in the liver.
Electronic supplementary material
The online version of this article (doi:10.1007/s00204-017-2080-0) contains supplementary material, which is available to authorized users.
Keywords: Hepatocarcinogenesis, Liver mesenchyme, Non-genotoxic hepatocarcinogenesis, Phenobarbital, Cyproterone acetate
Introduction
Hepatocellular carcinoma is one of the leading causes of cancer death worldwide. Many risk factors for this disease have been identified so far, such as chronic inflammation secondary to hepatitis-virus infection, chronic ethanol consumption or metabolic disorders (Llovet et al. 2016). The liver is also exposed to a great variety of environmental pollutants, synthetic steroid hormones or other drugs, which act as NGC in rodent bioassays. Considering the worldwide application of such compounds, thorough knowledge on the mode of NGC action is prerequisite to better estimate the possible liver cancer risk in exposed humans (Jacobs et al. 2016; Luch 2005).
According to current concepts, the first stage of hepatocarcinogenesis may be induced by genotoxic carcinogens, causing mutations in critical (growth) regulatory genes and leading to the formation of initiated cells. NGC, however, do not affect or bind directly to DNA but alter proliferation and survival of cells, DNA methylation, transcriptome patterns and/or cell signalling, which increase the likelihood of promotion of initiated cells. These effects are largely reversible and require continuous exposure to a sufficient dose to be sustained (Ellinger-Ziegelbauer et al. 2008; Pogribny and Rusyn 2013; Schulte-Hermann et al. 1990).
For the present study, we chose two prototypical NGC: (i) the barbiturate PB, a drug used to treat certain forms of epilepsia (Trinka and Kälviäinen 2017). PB is not considered to be DNA-reactive. In rats and mice chronic administration of PB causes liver tumor formation (Elcombe et al. 2014). (ii) CPA, a steroidal synthetic progestagen and anti-androgen, is applied as chemotherapy of androgen-dependent prostate cancer and is frequently prescribed as birth control pills for women suffering from hyperandrogenic conditions, such as acne or hirsutism (Azziz 2007; Bastide et al. 2013). CPA is known for years to produce liver tumors in rats and mice (Kasper 2001).
With regard to the molecular mode of action in the liver, PB activates the nuclear receptor constitutive androstane receptor (CAR), while CPA is a ligand preferentially for pregnane X receptor (PXR) or steroid hormone receptors (Elcombe et al. 2014; Kasper 2001; Schuetz et al. 1998). These receptor interactions mediate hepatic growth and adaptive increases of specific enzyme groups or organelles. Induction of liver growth by NGC is a self-limited and tightly controlled process, which is per se not carcinogenic. However, initiated/preneoplastic HC (HCPREN) and their successors show an altered response to PB or CPA, including excessive proliferation and insufficient elimination by apoptosis. Withdrawal of PB or CPA increases dramatically the apoptotic activity in the preneoplastic lesions, reversing the process of hepatocarcinogenesis (Schulte-Hermann et al. 1990; Grasl-Kraupp et al. 1997). However, the growth factors driving these PB- or CPA-induced shifts between cell renewal and cell death remain to be identified.
Increasing evidence attributes an important role to the hepatic stroma, driving tumor development by a complex pattern of bidirectional signaling between epithelium and microenvironment and involving a plethora of growth stimulatory and inhibitory factors. Thus, hepatocarcinogenesis may largely result from alterations in the normal stromal-epithelial dialogue. We and others have shown that several NGC activate mesenchymal liver cells (MC), resulting in secretion of pro-inflammatory cytokines and reactive oxygen species (Riegler et al. 2015; Roberts et al. 2007). Furthermore, PB caused an elevated secretion of the mesenchymal pro-inflammatory cytokine TNFα. This induced nuclear translocation of NFkB and suppression of the apoptotic activity in HC, an effect being crucial for tumor promotion by this NGC (Riegler et al. 2015). However, it remained to be elucidated whether NGC alter the intrahepatic stromal-epithelial dialogue and form paracrine growth loops to enhance growth of cancer prestages.
Considering the daily intake of PB, CPA, or other NGC by millions of humans and in view of the lack of adequate systems to test the impact of these compounds on human liver, we applied a unique cell culture model for epithelial–mesenchymal interactions and growth control of the very first stages of hepatocarcinogenesis. A few days after treatment of rats with the genotoxic hepatocarcinogen N-nitrosomorpholine (NNM), single HCPREN appear, which are detectable by their selective immunoreactivity for placental glutathione-S-transferase (GSTp) (Grasl-Kraupp et al. 2000). A considerable fraction of these cells develops into preneoplastic lesions. In primary culture, HCPREN show an inherent growth advantage and overresponse to known growth stimulators or suppressors, as observed in vivo (Löw-Baselli et al. 2000). Here, we investigated whether MC are involved in NGC-driven hepatocarcinogenesis. A combination of transcriptomics, bioinformatic analyses and subsequent experimentation enabled to identify growth factors which are released from PB- or CPA-treated MC and which suppress apoptosis and/or enhance cell replication preferentially in the first stages of hepatocarcinogenesis. Thus, NGC-induced alterations in the liver stroma appear crucial for the action of NGC and have to be considered for a better mechanistic understanding of non-genotoxic hepatocarcinogenesis.
Materials and methods
Animals and treatment
Male and female Han-Wistar rats, 6–8 weeks old, were obtained from Charles River (FRG). They were kept under standardized SPF-conditions. Male rats were treated with PB (5-ethyl-5-phenylbarbituric acid sodium salt; Sigma, St. Louis, MO) at 50 mg/1000 g body weight as single gavage or via drinking water for a period of 7 or 14 days. Controls received tap water only. Female SPF Wistar rats were treated with CPA (Sigma, St. Louis, MO) at 100 mg/10 ml corn oil/1000 g body weight by single gavage on one day or on 6 consecutive days. Oil-treated rats served as control.
Separately, NNM (Sigma, St. Louis, MO), dissolved in phosphate-buffered saline (PBS, pH 7.4), was applied as a single dose (250 mg/10 ml PBS/1000 g body weight) by gavage to 3–5 week old rats. All experiments were approved by the “Committee of Animal Protection” of the Austrian government and performed according to Austrian regulations.
Separation of liver cells and primary cultures
Livers of untreated or treated rats were perfused with collagenase (Worthington, Lakewood, NJ). The cell suspension obtained was used to separate MC from HC by low-speed centrifugation in percoll-gradients. MC were further separated by selective cell adherence into an endothelial cell (EC)-enriched fraction and a fraction consisting mainly of cd68 +/ED1 + exsudative monocytes/macrophages (EM) and liver-resident cd163 +/ED2 + Kupffer cells (KC). The purities of cell fractions were determined to be: 98.4 ± 0.6 for HC, 99.9 ± 0.1 for MC, 80 ± 19.4 for KC/EM, and 94.5 ± 2.8 for EC. For details on culture conditions, procedures and purities of the cell fractions see Böhm et al. (2013). Stock solutions were prepared for PB and CPA and aliquots were added to the medium to provide final concentrations (Table S1). Treatment of cells commenced 2 h after plating (time point 0).
Determination of DNA replication
3H-thymidine was added 24 h before cell harvest. Autoradiography served to determine the percentage of nuclei with incorporated 3H-thymidine (LI %). In each of the experiments 2000 HC nuclei and 600 HCPREN nuclei were counted. Further details see Löw-Baselli et al. (2000).
Determination of apoptosis
HC were fixed with 4% formaldehyde for 60 min at room temperature and washed twice with PBS. DNA was stained with Hoechst (benzimide H33258; 8 μg/ml PBS) for 5 min. After washing steps and drying, cells were mounted in Kaiser´s glycerol gelatine. Apoptoses (evaluated by chromatin condensation and fragmentation) were counted by fluorescence microscopy. Overall, 1000 HC per dish were analyzed (Riegler et al. 2015).
Whole-genome gene expression analysis
To perform whole genome expression analyses, RNA was extracted. The quality of RNA was tested by the 2100 Bioanalyzer-System (Agilent, St.Clara, CA). Complementary RNA targets were prepared and hybridized according to the manufacturer’s procedures on high-density oligonucleotide microarrays (Affymetrix RAT 230 2.0 GeneChip). The microarrays were processed as described before (Riegler et al. 2015).
Following the import of Affymetrix raw data (CEL files) into the R programming language and environment for statistical computing, sufficient quality of the raw data was checked by various metrics and statistical analyses provided by the package ArrayQualityMetrics (Kauffmann et al. 2009). With the help of the RMA method data were normalized and probesets were mapped to gene symbols and Entrez IDs using the appropriate metadata packages of Bioconductor (Gentleman et al. 2004; Irizarry 2003). Open access to data is provided at http://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?token=qjyjgcqqxpavler&acc=GSE68111.
To detect differential gene expression, a moderated t test (implemented in LIMMA package for R/Bioconductor) was applied combined with subsequent Benjamini–Hochberg correction for multiple testing to ensure a false discovery rate of < 0.05 (Smyth 2004). Fold-change cutoffs of ≥ 2 and ≤ 0.5 determined upregulated and downregulated genes, respectively. For validation of transcriptome data by quantitative real-time PCR (RT-qPCR), see Fig. S1.
Gene expression analyses by RT-qPCR
The extracted mRNA was processed and measured by the ABI-Prism/7500 Sequence Detection System (Applied-Biosystems, Foster City/CA) using TaqMan-based assays (Applied-Biosystems). For primers and assays see Table S1.
Immunodetection
Antisera and ELISA-kits were used, see Table S1. ELISAs were performed according to the manufacturer´s instructions. Material not included in the kit: Tetramethylbenzidine-peroxidase-solution for colour development (Thermo-Scientific); microtiter plates (Costar, Corning, NY). For the protocol of the HBEGF-ELISA see electronic supplementary material.
Results
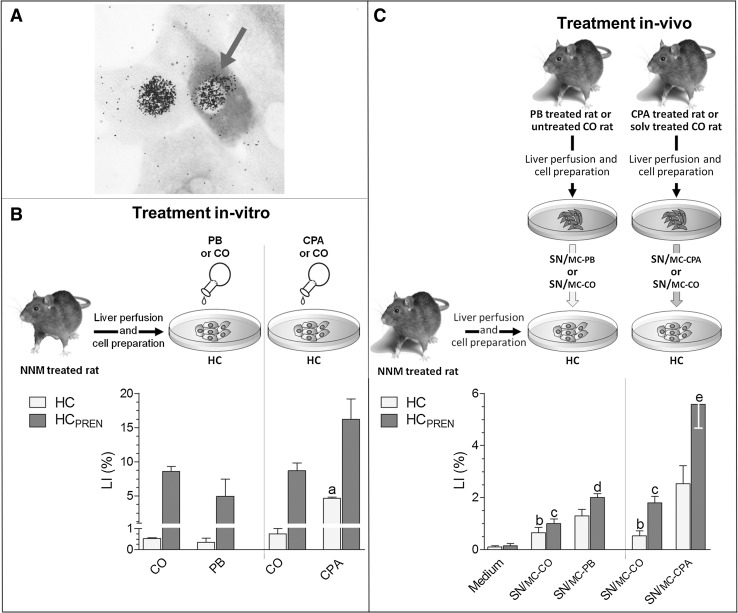
Effect of PB and CPA on replication of unaltered and preneoplastic hepatocytes in primary culture and the role of mesenchymal growth factors
According to our model, first stages of hepatocarcinogenesis were generated in rats by a single NNM application (Grasl-Kraupp et al. 2000). Twenty-one days later liver cells were isolated. Then, HCPREN and unaltered HC were co-cultured in the same system (Fig. 1A). HCPREN, identified by GSTp expression, showed a higher probability for DNA replication than normal appearing GSTp-negative HC, resulting in an inherent growth advantage of HCPREN, as described before (Fig. 1B: CO; Löw-Baselli et al. 2000).
Fig. 1.
Direct and/or indirect, MC-mediated effects of PB or CPA on cell replication of first stages of hepatocarcinogenesis. NNM was applied to induce the formation of HCPREN; 21 days later HC and HCPREN were isolated and cultured. A HCPREN (green arrow) in culture: 3H-thymidine incorporated into DNA is visualized by autoradiography as black spots over nucleus; magnification: ×200. B Direct effects of PB or CPA: cells were treated with 1 mM of PB or 10 µM of CPA; treatment was renewed at 48 h and lasted for 72 h. CO, solvent controls. C Indirect effects of PB or CPA: after a single dose of PB, CPA or solvent in vivo, MC were separated and cultured for 24 h to condition the supernatants, termed SN/MC-PB, SN/MC-CPA, or SN/MC-CO. Supernatants were added to cultured HC and HCPREN for 48 h. B, C 3H-thymidine was added 24 h before cell harvest; autoradiography served to determine LI. Data are mean ± SEM from 3 in B and 5 independent experiments in C. Statistics by unpaired t test in B for control vs. CPA: a) p < 0.01; in C for control medium vs. SN/MC-CO: b) p < 0.05; c) p < 0.01; for SN/MC-CO vs. SN/MC-PB: d) p < 0.01; for SN/MC-CO vs. SN/MC-CPA: e) p < 0.5
We tested whether PB or CPA elevate DNA replication in HC and HCPREN, when applied directly to the culture. Interestingly, PB treatment tended to lower the replication rate of HC and HCPREN (Fig. 1B). This was evident also at a lower dose of PB (Fig. S2). However, addition of CPA to the medium induced DNA synthesis considerably in HC and HCPREN (Fig. 1B). Due to the high basal frequency of replicating HCPREN, the additional stimulation by CPA caused that every sixth HCPREN started to cycle, which is remarkably high for HC in primary culture.
Next we applied PB or CPA in vivo and studied the role of the hepatic mesenchyme. To be specific, rats received a single dose of either compound, and MC were isolated and kept in culture for 24 h. The supernatant (SN), conditioned by the MC (SN/MC-PB, SN/MC-CPA), was transferred to cultured HC and HCPREN from NNM-treated animals. MC-supernatants from solvent-treated rats (SN/MC-CO) served as control (Fig. 1C). SN/MC-CO elevated DNA replication in both, HC and HCPREN, indicating that even without treatment MC produce and release growth factors acting on unaltered HC as well as on first stages of hepatocarcinogenesis. Application of SN/MC-PB or SN/MC-CPA elevated DNA replication in HC and HCPREN even further, more pronounced with SN/MC-CPA than with SN/MC-PB (Fig. 1C).
These data suggest that in cultured HC and HCPREN (i) supernatant of untreated MC enhances cell replication, (ii) elevation of HC replication by PB needs mesenchymal growth factors and (iii) CPA exerts—in addition to its direct action—also an indirect effect, mediated by MC-derived factors.
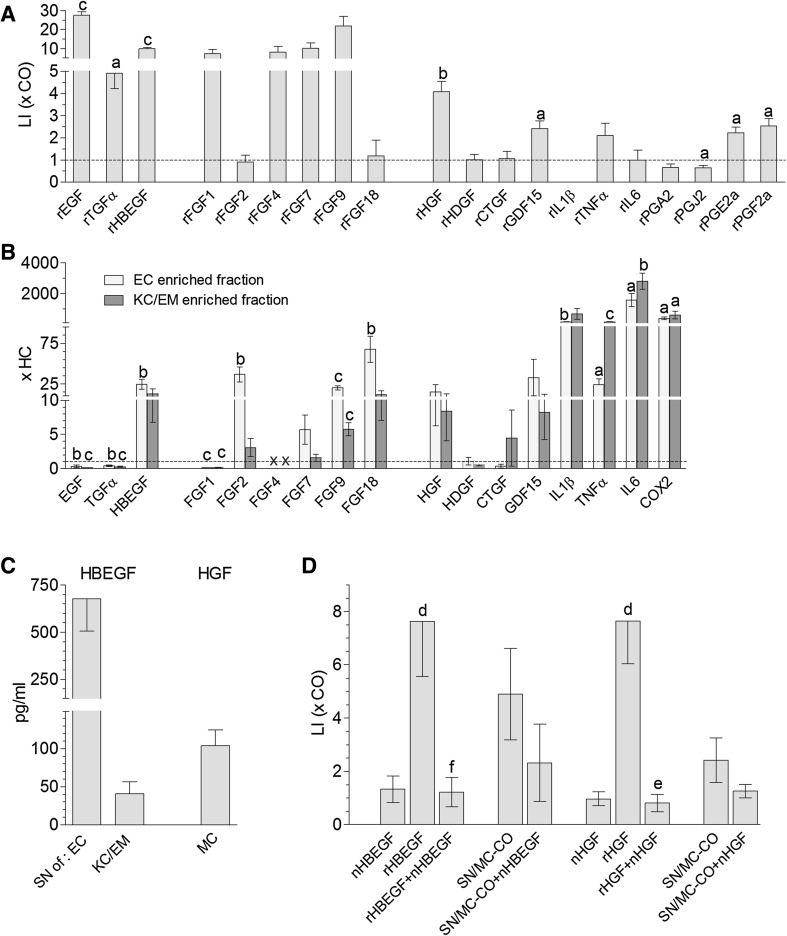
Identification of mesenchyme-derived growth factors supporting DNA replication of hepatocytes
To identify growth factors from untreated hepatic mesenchyme which enhance the replication of HC, we tested numerous candidates including the recombinant form of several erbb- or FGFR-ligands, HGF, some cytokines and also prostaglandins, and compared their DNA replication-inducing potential in HC. Most of the recombinant erbb- and FGFR-ligands, rHGF, rGDF15, and some prostaglandins elevated DNA replication (Fig. 2A).
Fig. 2.
MC, a rich source of growth factors for HC. A Effect of recombinant growth factors on LI of cultured HC. HC, from untreated animals were treated with recombinant proteins applied at 10 ng/ml (rEGF, rTGFα, rHBEGF, rFGF1, rFGF2, rFGF4, rFGF7, rFGF9, rFGF18, rHGF, rHDGF, rCTGF, rGDF15, rTNFα), 30 ng/ml (rIL6), 5 µg/ml (PGJ2), or 17.5 µg/ml medium (PGA2, PGE2a, PGF2a). Treatments were renewed at 48 h and lasted for 72 h. LI was determined by autoradiography and is expressed as fold solvent control. B Expression of growth factors in HC, EC and KC/EM from untreated animals. Transcript levels were determined by RT-qPCR and expressed as fold level in HC; x, transcripts were detected in EC- and KC/EM-enriched fractions but not in HC. C Concentration of HBEGF in supernatants of EC and KC/EM and of HGF in MC supernatants. EC, KC/EM and MC, obtained from untreated animals, were cultured; supernatants were collected after 24 h for ELISA. D Antibodies, neutralizing HBEGF or HGF, impair effect of SN/MC-CO. Medium and supernatants were pre-incubated with nHBEGF or nHGF at 37 °C for 60 min before addition to HC cultures; rHBEGF or rHGF served as positive control. LI was determined by autoradiography. A–D Data are mean ± SEM of ≥ 3 rats. Statistics by one sample t test in A for different treatment agents vs. control medium and in B for the expression level of genes of interest in EC- or KC/EM-enriched fractions vs. HC: a) p < 0.05, b) p < 0.01, c) p < 0.001; in D for rHBEGF or rHGF vs. CO: d) p < 0.05. Statistics by unpaired t test in D for treatment vs. treatment + treatment neutralizing antibodies: e) p < 0.05, f) p < 0.01
In parallel, we investigated the intrahepatic epithelial–mesenchymal distribution of the factors (Fig. 2B). Cells were isolated from the liver and separated into HC and MC. By selective cell adherence MC were further divided into an endothelial cell (EC)-enriched fraction and into a KC/EM-enriched fraction. HBEGF, FGF2, FGF4, FGF7, FGF18, IL1ß, TNFα, HGF, IL6 and COX2, the key enzyme of the prostaglandin biosynthesis, were expressed at higher levels in EC- and/or KC/EM-enriched fractions when compared to HC (Fig. 2B). Thus, the growth-inducing effect of SN/MC-CO might be due to a complex mixture of HBEGF, HGF, FGF7, GDF15, TNFα, IL6, prostaglandins and probably other factors.
We developed an ELISA for HBEGF and found that EC release considerably more HBEGF than KC/EM cells into the supernatant (Fig. 2C). For further clarification we added neutralizing anti-HBEGF (nHBEGF) to SN/MC-CO and found partial ablation of the growth stimulating effect of the supernatant on HC (Fig. 2D). Also HGF was secreted by MC into the supernatant and application of neutralizing anti-HGF (nHGF) largely blocked the stimulating effect of SN/MC-CO on DNA replication of HC (Fig. 2D). This indicates that HBEGF and HGF are the most important components in SN/MC-CO contributing to the paracrine growth stimulation of HC.
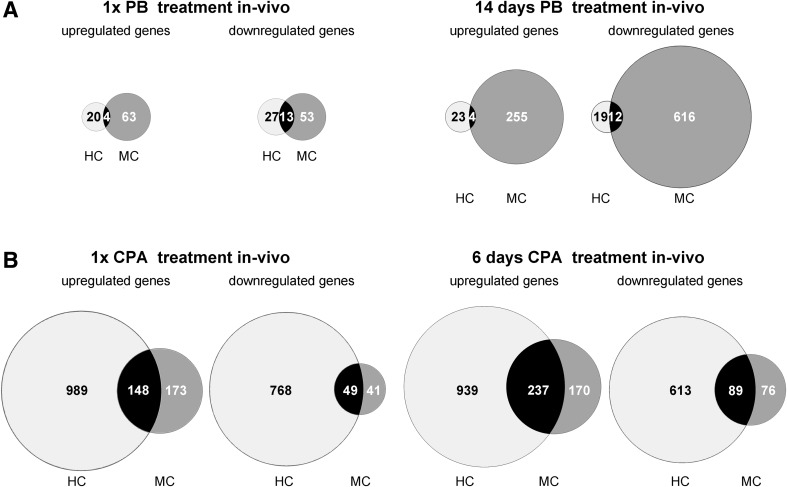
PB and CPA induce pronounced alterations in the transcriptome profile of mesenchymal liver cells
Next, we asked which mesenchymal factors mediate the growth-inducing capacity of PB or CPA on HC and HCPREN. Rats were treated with PB once or for 14 days or received CPA by gavage on 1 or on 6 consecutive days. Thereafter cells were isolated from the liver and separated into HC and MC. HC and MC from solvent-treated rats served as control. Oligonucleotide arrays revealed that a single dose of PB de-regulated considerably more genes in MC than in HC, an effect even more pronounced after 14 days of PB treatment (Fig. 3). In contrast, single and repeated treatment with CPA induced massive alterations in the gene expression profile of HC and less in MC. To conclude, the data provide clear evidence that the expression pattern of both, the parenchyma and mesenchyme, is altered considerably by both prototypical NGC.
Fig. 3.
PB alters the transcriptome profile rather in MC than in HC, while the opposite applies to CPA. Transcriptome profiles were determined by oligo-array analyses. Venn diagrams illustrate number of genes being up-/downregulated ≥ 2-fold in HC and/or MC after one application of PB or after 14 days of PB treatment in A or after one or 6 applications of CPA in B. Data are expressed as fold solvent controls and give means of ≥ 3 animals per treatment and time point
Transcriptome data were subjected to bio-informatic analyses to identify critical, cancer-related signal transduction pathways induced by the NGC. In general, many pathways were affected by PB and CPA in both, HC and MC (Table S2; Riegler et al. 2015). In HC, PB was found to be a potent inducer of drug metabolism, as expected, and of stress-induced pathways (MAPK-, NFkB-, TNFα-mediated signaling), while in MC there were profound upregulation of pathways involved in chemokine and cytokine signaling, as shown recently (Riegler et al. 2015). Genes driving the cell cycle or involved in caretaking of DNA stability and repair were induced by CPA in HC and MC (Table S2).
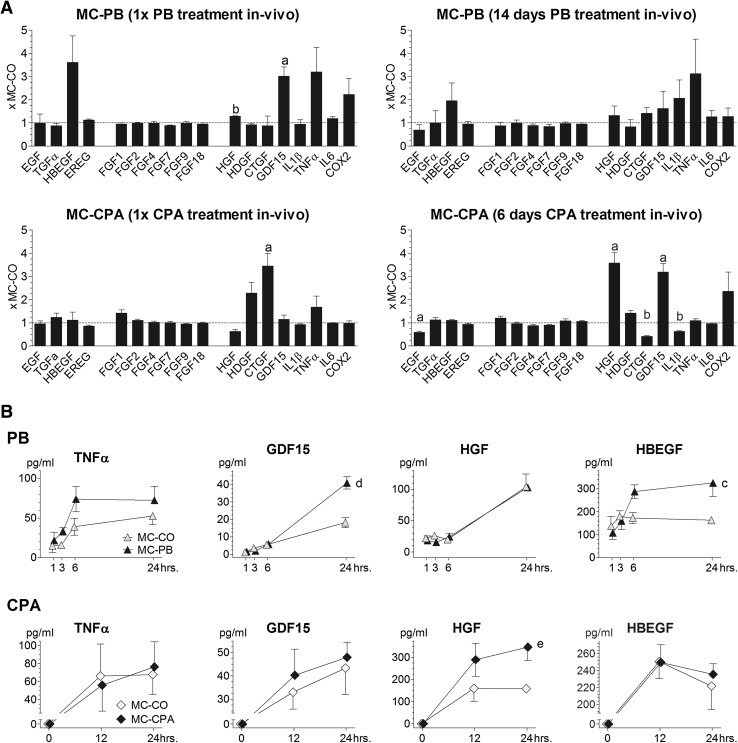
The hepatic mesenchyme secretes several growth factors following treatment with PB or CPA in vivo
We focused on the identification of growth factors for HC and HCPREN, produced and released by MC-PB or MC-CPA. Transcriptome data showed considerable upregulation of HBEGF, GDF15, TNFα, and COX2 in MC-PB (Fig. 4A). This was paralleled by elevated concentrations of HBEGF, GDF15 and TNFα in SN/MC-PB (Fig. 4B). MC-CPA showed pronounced elevations of HGF, CTGF, GDF15, and COX2 transcripts (Fig. 4A; for data validation see also Fig. S1). In SN/MC-CPA HGF occurred at concentrations of up to 300 ng/ml medium (Fig. 4B). For CTGF no rat-specific ELISA was available. PGE2 could not be detected in SN/MC-PB or SN/MC-CPA by the ELISA used (detection limit 31 pg/ml, data not shown).
Fig. 4.
Effect of PB or CPA in vivo on production and secretion of growth factors by MC in vitro. A Oligo-array analyses of growth factors in MC-PB and MC-CPA. No further growth factors were up-/downregulated ≥ 2-fold at any of the two time points than those given here. B Secretion of growth factors by MC-PB and MC-CPA. After a single dose of NGC or solvent in vivo, MC were separated and cultured. Aliquots of culture supernatant were collected at time points indicated and factor concentrations were determined by ELISA. A, B Data are mean ± SEM of ≥ 3 animals per treatment and time point. A Statistics by one sample t test for MC-CO vs. MC-PB or MC-CPA: a) p < 0.05, b) p < 0.01. B Statistics by unpaired t test for MC-CO vs. MC-PB at 24 h: c) p < 0.05, d) p < 0.01; for MC-CO vs. MC-CPA at 24 h: e) p < 0.05
Mesenchymal growth factors may mediate the anti-apoptotic and growth-inducing effects of NGC in hepatocytes and cancer prestages
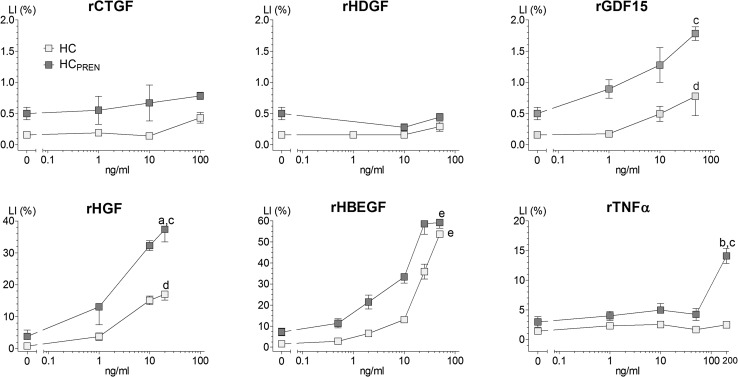
We addressed the question whether the growth factor concentrations, detected in SN/MC-PB or SN/MC-CPA, are sufficiently high to explain the supernatant effects. We tested these factors in recombinant form with regard to their potency to induce DNA replication in HC and HCPREN (Fig. 5). In SN/MC-PB GDF15 occurred at ~ 40 pg/ml, TNFα at ~ 70 pg/ml and HBEGF at ~ 350 pg/ml. At these concentrations rTNFα as well as rGDF15 were without any effect on DNA replication, while rHBEGF might become effective. In SN/MC-CPA HGF occurred at 0.35 ng/ml, which may elevate replication in HCPREN and to some extent also in HC, as shown by the recombinant form of this factor. rCTGF and rHDGF exerted no significant effects on hepatocellular DNA replication.
Fig. 5.
rGDF15, rHGF and rHBEGF induce DNA replication of HC and HCPREN. HC and HCPREN were isolated from NNM-treated livers for culture. Treatments with recombinant factors started 2 h after seeding of cells, were renewed at 48 h and lasted for 72 h. The LI was determined by autoradiography. Data are mean ± SEM from ≥ 3 rats. Statistics by unpaired t test for HC vs. HCPREN at highest concentration: a) p < 0.05, b) p < 0.01. Statistics by Kruskal–Wallis test: c) p < 0.05, d) p < 0.01, e) p < 0.001
We pre-incubated SN/MC-PB with antibodies blocking HBEGF (nHBEGF), which failed to neutralize the effect of SN/MC-PB on DNA synthesis of HC (data not shown). Antibodies blocking rat GDF15 were not available. Thus, GDF15, an unidentified factor or a combination of some factors may be responsible for the weak effects of SN/MC-PB on HC replication (Fig. 1C).
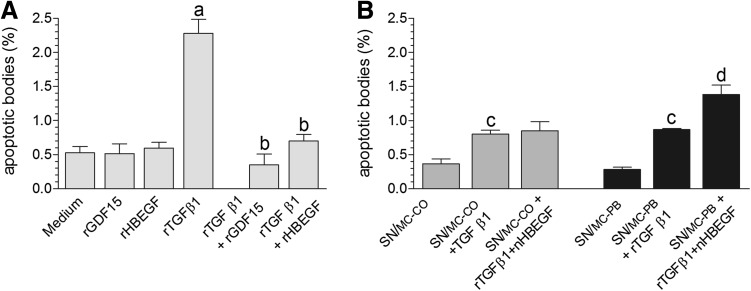
Recently, we described that MC-derived TNFα mediates the pronounced anti-apoptotic effects of SN/MC-PB in HC (Riegler et al. 2015). Therefore, we checked whether HBEGF or GDF15 may act also as survival factors for HC. Both factors, applied as recombinant form, exerted marginal effects on basal apoptotic activity. To induce a distinct apoptotic response, HC were treated with rTGFß1, which dramatically increased the incidence of apoptosis. Co-application of rHBEGF or rGDF15 antagonized the pro-apoptotic effects of TGFß1 (Fig. 6A). Interestingly, the apoptosis-inducing potency of rTGFß1 was also reduced dramatically by co-application of SN/MC-CO or SN/MC-PB. Obviously, the mesenchymal supernatants contain potent survival factors for HC. Pre-incubation of SN/MC-CO with nHBEGF had no effect on the apoptotic activity of HC. In contrast, pre-incubating SN/MC-PB with nHBEGF significantly elevated the apoptotic activity (Fig. 6B). This strongly suggests that the elevated HBEGF levels in SN/MC-PB inhibit apoptosis of HC. Due to lack of nGDF15-antibodies direct evidence for an anti-apoptotic effect of this factor in SN/MC-PB could not be obtained.
Fig. 6.
SN/MC-PB exerts anti-apoptotic effects in HC probably via GDF15 and HBEGF. A HC were kept in medium and were treated with rGDF15 (10 ng/ml), rHBEGF (10 ng/ml), and/or rTGFß1 (1 ng/ml). B HC were kept in SN/MC-CO or SN/MC-PB (with/without pre-incubation with nHBEGF; see also Fig. 2) and were treated with rTGFß1 (1 ng/ml). A, B 24 h after start of treatment HC were harvested to determine apoptoses. At least 2000 HC per experiment and treatment group were screened. Statistics by unpaired t test in A for TGFß1 vs. medium: a) p < 0.01; for TGFß1 vs. TGFß1 + treatment with recombinant factor: b) p < 0,01; in B for SN/MC-CO or SN/MC-PB vs. SN/MC-CO + TGFß1 or SN/MC-PB + TGFß1, respectively: c) p < 0.01; for treatment vs. treatment + nHBEGF: d) p < 0.05
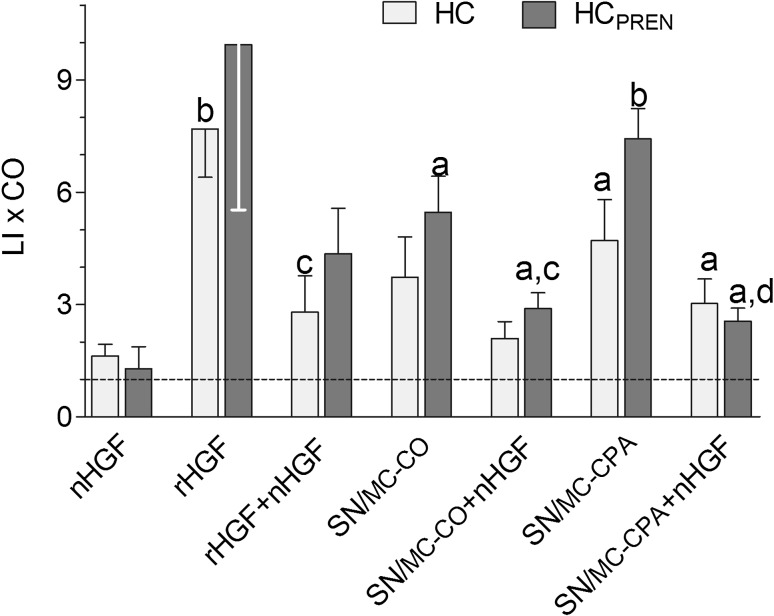
In contrast to SN/MC-PB, SN/MC-CPA strongly enhanced DNA replication of HC and HCPREN. Pre-incubation of SN/MC-CPA with antibodies neutralizing HGF (nHGF) largely abolished the stimulatory effect of SN/MC-CPA (Fig. 7). This implies that HGF may be the most important growth factor in SN/MC-CPA for normal HC and in particular for early cancer prestages and may thus be one of the key factors in CPA-driven hepatocarcinogenesis.
Fig. 7.
SN/MC-CPA induces replication of HC and HCPREN via HGF. Medium, SN/MC-CO or SN/MC-CPA were pre-incubated with nHGF before addition to HC cultures (see also Fig. 2). rHGF served as positive control. Cells were harvested 48 h after start of treatment; LI was determined by autoradiography. Data are expressed as fold medium control (CO) and are mean ± SEM from independent experiments on ≥ 3 rats. Statistics by one sample t test for treatment vs. CO: a) p < 0.05, b) p < 0.01; statistics by unpaired t test for treatment vs. treatment + nHGF: c) p < 0.05, d) p < 0.01
Discussion
Here, we show for the first time that two prototypical NGC increase the production and release of survival and growth factors from MC, which may promote outgrowth of first stages of carcinogenesis in rat liver. Such effects are considered causally involved in the tumor promoting and eventually carcinogenic action of these compounds, as discussed in the following.
The hepatic mesenchyme as source of growth factors for hepatocytes
In the liver and other organs the stroma is known to provide crucial signaling for control of tissue homeostasis. Accordingly, any deviation in signaling may cause not only destabilization of tissue homeostasis but also promotion of premalignant cells towards malignancy (Bissell and Hines 2011).
We tested the effect of the soluble factors, released by hepatic stroma cells surrounding unaltered HC as well as first stages of hepatocarcinogenesis. The overall outcome was slight induction of replication of HC and HCPREN by the supernatant of MC, isolated from untreated livers. This may be due to the fact that we used MC from 6–8 weeks old animals which were still growing. In addition, the disruption of the extracellular matrix may also create experimental conditions favoring cell replication.
Considering the mesenchymal expression profile of growth factors and the ELISA data of the secretomes, MC produce and release a complex mixture of TNFα, HBEGF, HGF, GDF15, and probably other factors, not identified so far. TNFα is secreted mainly by KC to bind to TNFR1/2, which transiently activates NFkB and increases the proliferative response of HC to growth factors in vivo (Michalopoulos 2014). This priming effect of TNFα was also evident in cultured HC, e.g., peroxisome proliferators stimulate DNA synthesis of cultured HC only in the presence of TNFα or TNFα-producing KC (Parzefall et al. 2001). In the present study, TNFα was not a growth stimulator of unaltered HC, but at concentrations of > 50 ng/ml medium it induced replication of HCPREN. This indicates an altered response of the very first stages of hepatocarcinogenesis towards paracrine stimuli. We found that mainly EC produce HBEGF, which binds to erbb1 and erbb4 for signaling. HBEGF is one of the key factors in liver growth and promotes the transition of HC from the G1 into the S-phase (Michalopoulos 2014). HGF transcripts are produced by both, EC and KC, at more or less equal amounts. When released, HGF acts as a multi-functional cytokine on HC via the hepatocyte growth factor receptor to regulate hepatocellular growth, motility and morphogenesis (Michalopoulos 2014). GDF15, a member of the transforming growth factor-β family, is also known as macrophage inhibitory cytokine-1. A specific receptor for GDF15 has not been identified so far. Recently, it was shown that GDF15 enhances the phosphorylation of Erk and Akt, components of growth and survival pathways (Urakawa et al. 2015). Here, we show for the first time that this factor supports survival and replication of HC and HCPREN.
Considering the presence of ~ 0.05 ng of TNFα, ~ 0.1 ng of HGF and ~ 0.2 ng of HBEGF per ml SN/MC-CO, rHBEGF and rHGF required five–tenfold higher concentrations to elevate hepatocellular DNA replication in purified HC, being depleted from TNFα-producing KC. It appears possible that the efficacy of the natural factors in SN/MC-CO was increased by the presence of TNFα, known to prime HC to enter the cell cycle. Also IL6 is occurring in the MC supernatant at ~ 70 pg/ml and is also a priming factor for HC (Michalopoulos 2014; Riegler et al. 2015). This may explain, that neutralization of only 0.2 ng of HBEGF or 0.1 ng of HGF in SN/MC-CO by blocking antibodies abolished greatly the replication-inducing effect of the supernatant. These observations provide strong evidence that HBEGF and HGF are the main mesenchymal factors driving hepatocellular replication.
PB-treatment in vivo stimulates mesenchymal liver cells to release growth/survival factors for hepatocytes and early cancer prestages
In the present study, DNA replication of HC and HCPREN was suppressed when PB was applied directly to cultures but was stimulated by SN/MC-PB. We considered the possibility of a direct growth-suppressing PB effect due to blockade of Erbb1 activity, as was described recently in cultured primary murine HC (Mutoh et al. 2013). In this system, 2.5 mM PB binds directly to Erbb1 to block phosphorylation and signalling of the receptor and to prevent phosphorylation also of the receptor for activated C kinase 1 (RACK1). De-phosphorylated RACK1 interacts with constitutive androstan receptor (CAR) and protein phosphatase 2A to elicit de-phosphorylation and subsequent translocation of CAR to the nucleus for transcription of PB-target genes (Mutoh et al. 2013). However, in HC of the currently used rat model, 1 mM PB did affect neither rEGF-induced Erbb1-phosphorylation nor rEGF-induced DNA replication (Fig. S3). The reason underlying the apparent discrepancy between murine and rat HC is presently unclear.
In the hepatic mesenchyme PB induced profound alterations of the transcriptome profiles, including growth regulatory genes, such as GDF15. The ~ twofold elevated transcript levels of GDF15 in MC-PB was reflected by a ~ twofold enhanced secretion of this cytokine. HBEGF transcripts were elevated ~ 3-fold in MC-PB resulting in ~ twofold enhanced secretion of this cytokine. HBEGF is a ligand of Erbb1 and Erbb4. PB did not affect DNA replication, if induced by HBEGF (Fig. S3). This indicates that the activity not only of Erbb1 but also of Erbb4 was not affected by PB in HC. HBEGF tended to stimulate growth of HC at ~ 1 ng/ml medium and of HCPREN already at 0.5 ng/ml, a concentration coming close to levels measured in the supernatant of PB-treated MC. However, nHBEGF failed to block the effects of SN/MC-PB on replication of HC and HCPREN indicating a function of HBEGF in PB-driven hepatocarcinogenesis being different from induction of DNA replication.
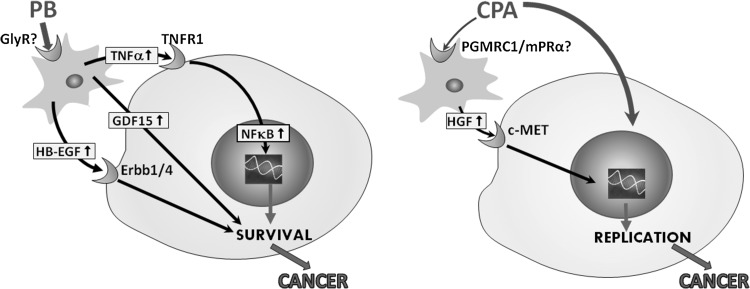
As reported previously, PB slightly elevated DNA replication but suppressed distinctly the elimination of cells by apoptosis in unaltered tissue and preneoplastic lesions of rat liver in vivo (Schulte-Hermann et al. 1990). This led to liver hypertrophy/hyperplasia and to outgrowth of tumors. Withdrawal of PB increased dramatically the apoptotic activity in the liver, which reversed liver hyperplasia and dramatically reduced the size of preneoplastic lesions, indicating a dependence of unaltered and preneoplastic HC on this NGC. This PB-elicited shift from death towards replication of preneoplastic cells was found to be crucial for the tumor promoting effect of this compound (Schulte-Hermann et al. 1990). We described recently that PB-treated MC secrete elevated levels of TNFα, which antagonizes apoptosis in HC via activation of NFkB and down-stream survival pathways (Riegler et al. 2015). Therefore, we checked whether HBEGF and GDF15 exert anti-apoptotic activity as well. In fact, rGDF15 and rHBEGF completely blocked rTGFß1-induced HC apoptosis. Interestingly, the pro-apoptotic effect of rTGFß1 remained unaffected when pre-incubating SN/MC-CO with nHBEGF but was elevated significantly when pre-incubating SN/MC-PB with nHBEGF. These observations provide indirect but compelling evidence that the elevated HBEGF levels in SN/MC-PB may mediate the pro-survival effects of PB in HC (Fig. 8).
Fig. 8.
Hypothesis on PB/CPA-induced alterations in epithelial–mesenchymal interactions supporting tumor promotion in rat liver. Left panel, after treatment of MC by PB, TNFα is released and binds to TNFR1 exposed on HC. This leads to activation of NFκB and nuclear translocation of this transcription factor, activating pro-survival pathways (Riegler et al. 2015). PB also may induce the release of HBEGF and GDF15 from MC. Subsequently HC are protected from pro-apoptotic stimuli. As a consequence, enhanced survival of HCPREN may support indirectly growth of preneoplasia and enhances the probability for development of cancer. Right panel, in contrast with PB, CPA elicits more direct effects on DNA replication of HCPREN. In addition, CPA may also act via PGMRC1 and/or mPRα on MC, which produce and release HGF to support the growth-inducing and tumor promoting effect of CPA in cancer prestages
The direct hepatomitogen CPA recruits mesenchymal HGF for paracrine growth stimulation of hepatocytes and cancer prestages
In rats CPA acts as a strong hepatomitogen inducing pronounced hyperplasia of the liver (Kasper 2001). This considerable intrahepatic growth pressure is considered to be essential for the outgrowth of preneoplasia to malignancy. In cultured HC and HCPREN CPA exerted a direct growth inducing effect but also a considerable indirect one, mediated by factors released from CPA-treated MC. Similar to PB, CPA elicited multiple alterations in the hepatic mesenchyme, which is reflected by elevated transcript levels of growth factors, like CTGF, HDGF and HGF, and enhanced secretion of some of these factors. CTGF and HDGF appear not to interfere with hepatocellular growth regulation, since in recombinant forms they neither induced replication of HC or HCPREN (Fig. 5) nor affected the apoptotic activity of HC (data not shown). SN/MC-CPA contained about 0.35 ng HGF/ml; this concentration induced DNA replication of HCPREN, as confirmed by the HGF-blocking antibodies abrogating completely the SN/MC-CPA effect. Array data showed that the expression of HGF remained elevated in the hepatic mesenchyme also after 6 days of CPA treatment. Taken together, these findings indicate that HGF may be one of the key growth factors in CPA-driven rat hepatocarcinogenesis (Fig. 8).
We described recently that MC express glycine receptors, which may mediate the PB effects (Riegler et al. 2015). In analogy, we raised the question which receptors in the hepatic mesenchyme might transmit the CPA effects. CPA inhibits competitively androgen and glucocorticoid receptors, exerts progestational and mineralocorticoid effects, acts as pregnane-X-receptor (PXR) agonist, and interferes also with CAR (Honer et al. 2003; Kasper 2001; Schuetz et al. 1998). On HC the hepatomitogenic effect appears to be largely mediated by PXR and CAR (Shizu et al. 2013). However, in EC or KC we could not detect significant levels of PXR or CAR (Riegler et al. 2015). The same holds true for the androgen or mineralocorticoid receptors (Fig. S4). The glucocorticoid receptor showed the highest expression level in liver cell-types, when compared to the other receptors investigated. Since CPA antagonizes the effects of the glucocorticoid receptor, the relatively high expression level appears not to be significant for the CPA-mediated effects in MC, as seen in this study. Considering that CPA acts mainly as progestin, it was surprising not to detect any signal for progesterone receptor transcripts, neither in HC nor in any MC type.
The recent discovery of membrane-located progesterone receptors (mPR) and progesterone-receptor-membrane-component 1 (PGRMC1) in mammalians suggests that there are alternatives to mediate progesterone effects particularly in tissues lacking the classical progesterone receptor. mPR belong to the progestin-adipoQ-receptor-family and are coupled to an inhibitory G-protein. Progesterone is the most important ligand, indicating regulatory functions in reproductive tissues (Tokumoto et al. 2016). mPR appear to be involved in the inhibition of apoptosis via MAP-kinase and Akt (Dressing et al. 2012). PGRMC1, a member of the membrane-associated progesterone receptor family, is highly expressed in the liver, and shows high affinity for progesterone, but also testosterone and glucocorticoids are possible ligands (Cahill et al. 2016). PGRMC1 interacts with Erbb1 and binds and activates also cytochrome P450 proteins, facilitating cancer proliferation and chemoresistance (Kabe et al. 2016). In the present study, we found transcripts of mPRa and PGMRC1 in HC and all MC types studied, at levels being comparable to those in uterus or ovar (Fig. S4). This might indicate that the progestin CPA acts on all liver cell types via the membrane-anchored progesterone receptors.
PB and CPA may also interfere with human MC—putative implications for risk assessment
Much effort has been spent to assess putative health risks for humans being continuously treated with barbiturates or CPA. When exposed to barbiturates an altered functional status of macrophages/monocytes became evident, similar to observations in rats (Park and Brody 1971; Ploppa et al. 2008; Rossano et al. 1992). The elevated secretion of TNFα by PB-treated rat KC suppressed apoptosis of HC and acted as survival factor (Riegler et al. 2015). In human liver, however, enhanced intrahepatic TNFα secretion may lead rather to the development of drug-induced liver injury, as observed occasionally during treatment with anti-epileptic barbiturates (Shapiro et al. 1980). It remains to be elucidated whether barbiturates can enhance the production of HBEGF and GDF15 in liver mesenchyme not only of rats but of humans as well. Species comparisons with regard to the functional reactivity of the hepatic mesenchyme towards PB or other barbiturates would greatly support the estimation of health risks by this class of compounds.
In humans CPA is widely applied for contraception and treatment of androgen-related diseases, such as acne, hirsutism, prostate cancer, or pubertas praecox (Azziz 2007; Bastide et al. 2013). Conflicting data exist with regard to the carcinogenic potency. Most studies do not report an increased incidence of hepatic tumors under therapeutic use of CPA in adults (Kasper 2001). However, in 1552 children and adolescents, suffering from pubertas praecox or other diseases and receiving CPA for 2.7 years on average, there was a tendency towards an elevated occurrence of malignant hepatoma (Watanabe et al. 1997). With regard to the mode of carcinogenic action in rats, CPA is sex-specifically activated to pro-mutagenic adducts in the liver of females only. In a long-term rat carcinogenicity study very high, hepatotoxic doses of CPA elevated the incidence of tumors in the liver with a somewhat higher incidence in females than in males (Schuppler and Günzel 1979). At lower dose levels no tumorigenic effect became evident in both sexes (Kasper 2001). Schulte-Hermann et al. (1981) showed that in the intact liver CPA induced proliferation dramatically in HCPREN and only slightly in HC indicating that HCPREN are more susceptible to the growth stimulus of CPA than their unaltered counterparts. Consequently, rodent liver tumor formation was considered to depend largely on the mitogenic effects of the compound and a predominantly non-genotoxic and non-linear mode of action has been anticipated. It has not been excluded so far that CPA may act as tumor promoter also in human livers. In previous and the present study CPA was found to enhance the proliferation of rat HC and HCPREN in vitro, as observed in vivo. However, cultured human primary HC were non-responsive to direct mitogenic stimulation by CPA (Parzefall et al. 1991). It is presently unclear whether these cultures were depleted from MC and whether CPA requires the presence of MC to elicit a growth reaction in human HC. Similar to PB, data on the functional reactivity of human MC towards CPA would greatly help to better understand the health risk of exposed humans.
To conclude, homeostasis of liver tissue is dependent on the continuous integration of intra- and extracellular signals controlling growth, survival, and death of the cells. Any disturbances may trigger the outgrowth of cancer. While factors released from MC after PB-treatment appear to interfere mainly with cell survival pathways, CPA-treated MC secrete HGF to stimulate cell replication. Both effects may contribute to the outgrowth of liver tumors (Fig. 8). Thus, our data suggest that the carcinogenic activity of NGC results not solely from effects on the parenchyma as frequently anticipated. However, direct effects on the hepatic mesenchyme may be of high significance in NGC-driven carcinogenesis. This new concept requires testing with other NGC in other organs and species and may improve greatly strategies in risk assessment of NGC.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
Open access funding provided by Medical University of Vienna. The technical assistance of Elisabeth Haslinger, Helga Koudelka and Birgit Mir-Karner is gratefully acknowledged. Venn diagrams were drawn with the program “Venn Diagram Plotter” kindly provided by PNNL and the OMICS.PNL.GOV website. This project (“MARCAR”) received funding under European Union Innovative Medicine Initiative (IMI JU) under grant agreement no. 115001 and by the Herzfelder´sche Familienstiftung.
Abbreviations
- BW
Body weight
- CAR
Constitutive androstane receptor
- CO
Untreated or solvent treated control rats or cells
- COX2
Cyclooxygenase 2
- CPA
Cyproterone acetate
- CTGF
Connective tissue growth factor
- EC
Endothelial cell
- EM
Exsudative monocyte
- GDF15
Growth and differentiation factor 15
- (r)HBEGF
(recombinant) heparin-binding EGF-like growth factor
- HC
Hepatocyte
- HCPREN
Initiated/preneoplastic hepatocyte
- HGF
Hepatocyte growth factor
- IL6
Interleukin 6
- KC
Kupffer cells
- LI
Labeling index
- MC
Mesenchymal liver cells
- MC-CO
MC obtained from a solvent-treated or untreated control rat
- MC-CPA
MC obtained from of a CPA-treated rat
- MC-PB
MC obtained from a PB-treated rat
- mPR
Membrane located progesterone receptor
- NGC
Non-genotoxic carcinogen
- nHBEGF
HBEGF-neutralizing antibodies
- nHGF
HGF-neutralizing antibodies
- NNM
N-nitrosomorpholine
- NOS2
Nitric oxide synthase 2
- PB
Phenobarbital
- PBS
Phosphate-buffered saline
- PPAR-alpha
Peroxisome proliferator-activated receptor alpha
- PGRMC1
Progesterone receptor membrane component 1
- PXR
Pregnane X receptor
- SN
Supernatant
- SN/MC-CO
Supernatant of MC obtained from untreated or solvent-treated rats
- SN/MC-CPA
Supernatant of MC obtained from CPA treated rats
- SN/MC-PB
Supernatant of MC obtained from PB-treated rats
- LI labelling index
% Cells replicating DNA
Footnotes
Marzieh Nejabat and Teresa Riegler contributed equally.
Electronic supplementary material
The online version of this article (doi:10.1007/s00204-017-2080-0) contains supplementary material, which is available to authorized users.
References
- Azziz R. Clinical and hormonal evaluation of androgen excess. In: Azziz R, editor. Androgen excess disorders in women. New York: Springer; 2007. pp. 365–375. [Google Scholar]
- Bastide C, Bruyère F, Karsenty G, Guy L, Rozet F. Hormonal treatment in prostate cancer. Prog Urol. 2013;23:1246–1257. doi: 10.1016/j.purol.2013.08.325. [DOI] [PubMed] [Google Scholar]
- Bissell MJ, Hines WC. Why don’t we get more cancer? A proposed role of the microenvironment in restraining cancer progression. Nat Med. 2011;17:320–329. doi: 10.1038/nm.2328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Böhm T, Berger H, Nejabat M, Riegler T, Kellner F, Kuttke M, Sagmeister S, Bazanella M, Stolze K, Daryabeigi A, Bintner N, Murkovic M, Wagner KH, Schulte-Hermann R, Rohr-Udilova N, Huber W, Grasl-Kraupp B. Food-derived peroxidized fatty acids may trigger hepatic inflammation: a novel hypothesis to explain steatohepatitis. J Hepatol. 2013;59:563–570. doi: 10.1016/j.jhep.2013.04.025. [DOI] [PubMed] [Google Scholar]
- Cahill MA, Jazayeri JA, Catalano SM, Toyokuni S, Kovacevic Z, Richardson DR. The emerging role of progesterone receptor membrane component 1 (PGRMC1) in cancer biology. Biochim Biophys Acta. 2016;1866:339–349. doi: 10.1016/j.bbcan.2016.07.004. [DOI] [PubMed] [Google Scholar]
- Dressing GE, Alyea R, Pang Y, Thomas P. Membrane progesterone receptors (mPRs) mediate progestin induced antimorbidity in breast cancer cells and are expressed in human breast tumors. Horm Cancer. 2012;3:101–112. doi: 10.1007/s12672-012-0106-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elcombe CR, Peffer RC, Wolf DC, Bailey J, Bars R, Bell D, Cattley RC, Ferguson SS, Geter D, Goetz A, Goodman JI, Hester S, Jacobs A, Omiecinski CJ, Schoeny R, Xie W, Lake BG. Mode of action and human relevance analysis for nuclear receptor-mediated liver toxicity: a case study with phenobarbital as a model constitutive androstane receptor (CAR) activator. Crit Rev Toxicol. 2014;44:64–82. doi: 10.3109/10408444.2013.835786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellinger-Ziegelbauer H, Gmuender H, Bandenburg A, Ahr HJ. Prediction of a carcinogenic potential of rat hepatocarcinogens using toxicogenomics analysis of short-term in vivo studies. Mutat Res. 2008;637:23–39. doi: 10.1016/j.mrfmmm.2007.06.010. [DOI] [PubMed] [Google Scholar]
- Gentleman RC, Carey VJ, Bates DM, Bolstad B, Dettling M, Dudoit S, Ellis B, Gautier L, Ge Y, Gentry J, Hornik K, Hothorn T, Huber W, Iacus S, Irizarry R, Leisch F, Li C, Maechler M, Rossini AJ, Sawitzki G, Smith C, Smyth G, Tierney L, Yang JY, Zhang J. Bioconductor: open software development for computational biology and bioinformatics. Genome Biol. 2004;5:R80. doi: 10.1186/gb-2004-5-10-r80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grasl-Kraupp B, Ruttkay-Nedecky B, Müllauer L, Taper H, Huber W, Bursch W, Schulte-Hermann R. Inherent increase of apoptosis in liver tumors: implications for carcinogenesis and tumor regression. Hepatology. 1997;25:906–912. doi: 10.1002/hep.510250420. [DOI] [PubMed] [Google Scholar]
- Grasl-Kraupp B, Luebeck G, Wagner A, Löw-Baselli A, de Gunst M, Waldhör T, Moolgavkar S, Schulte-Hermann R. Quantitative analysis of tumor initiation in rat liver: role of cell replication and cell death (apoptosis) Carcinogenesis. 2000;21:1411–1421. doi: 10.1093/carcin/21.7.1411. [DOI] [PubMed] [Google Scholar]
- Honer C, Nam K, Fink C, Marshall P, Ksander G, Chatelain RE, Cornell W, Steele R, Schweitzer R, Schumacher C. Glucocorticoid receptor antagonism by cyproterone acetate and RU486. Mol Pharmacol. 2003;63:1012–1020. doi: 10.1124/mol.63.5.1012. [DOI] [PubMed] [Google Scholar]
- Irizarry RA. Summaries of Affymetrix GeneChip probe level data. Nucleic Acids Res. 2003;31:e15. doi: 10.1093/nar/gng015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs MN, Colacci A, Louekari K, Luijten M, Hakkert BC, Paparella M, Vasseur P. International regulatory needs for development of an IATA for non-genotoxic carcinogenic chemical substances. Altex. 2016;33:359–392. doi: 10.14573/altex.1601201. [DOI] [PubMed] [Google Scholar]
- Kabe Y, Nakane T, Koike I, Yamamoto T, Sugiura Y, Harada E, Sugase K, Shimamura T, Ohmura M, Muraoka K, Yamamoto A, Uchida T, Iwata S, Yamaguchi Y, Krayukhina E, Noda M, Handa H, Ishimori K, Uchiyama S, Kobayashi T, Suematsu M. Haem-dependent dimerization of PGRMC1/Sigma-2 receptor facilitates cancer proliferation and chemoresistance. Nature Communications. 2016;7:11030. doi: 10.1038/ncomms11030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasper P. Cyproterone acetate: a genotoxic carcinogen? Pharmacol Toxicol. 2001;88:223–231. doi: 10.1034/j.1600-0773.2001.d01-108.x. [DOI] [PubMed] [Google Scholar]
- Kauffmann A, Gentleman R, Huber W. ArrayQualityMetrics—a bioconductor package for quality assessment of microarray data. Bioinformatics. 2009;25:415–416. doi: 10.1093/bioinformatics/btn647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Llovet JM, Zucman-Rossi J, Pikarsky E, Sangro B, Schwartz M, Sherman M, Gores G. Hepatocellular carcinoma. Nat Rev Dis Primers. 2016;2:16018. doi: 10.1038/nrdp.2016.18. [DOI] [PubMed] [Google Scholar]
- Löw-Baselli A, Hufnagl K, Parzefall W, Schulte-Hermann R, Grasl-Kraupp B. Initiated rat hepatocytes in primary culture: a novel tool to study alterations in growth control during the first stage of carcinogenesis. Carcinogenesis. 2000;21(1):79–86. doi: 10.1093/carcin/21.1.79. [DOI] [PubMed] [Google Scholar]
- Luch A. Nature and nurture-lessons from chemical carcinogenesis. Nat Rev Cancer. 2005;5:113–125. doi: 10.1038/nrc1546. [DOI] [PubMed] [Google Scholar]
- Michalopoulos GK. Advances in liver regeneration. Expert Rev Gastroenterol Hepatol. 2014;8:897–907. doi: 10.1586/17474124.2014.934358. [DOI] [PubMed] [Google Scholar]
- Mutoh S, Sobhany M, Moore R, Perera L, Pedersen L, Sueyoshi T, Negishi M. Phenobarbital indirectly activates the constitutive active androstane receptor (CAR) by inhibition of epidermal growth factor receptor signaling. Sci Signal. 2013;6:31. doi: 10.1126/scisignal.2003705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park SK, Brody JI. Suppression of immunity by phenobarbital. Nat New Biol. 1971;233:181–182. doi: 10.1038/newbio233181a0. [DOI] [PubMed] [Google Scholar]
- Parzefall W, Erber E, Sedivy R, Schulte-Hermann R. Testing for induction of DNA synthesis in human hepatocyte primary cultures by rat liver tumor promoters. Cancer Res. 1991;51:1143–1147. [PubMed] [Google Scholar]
- Parzefall W, Berger W, Kainzbauer E, Teufelhofer O, Schulte-Hermann R, Thurman RG. Peroxisome proliferators do not increase DNA synthesis in purified rat hepatocytes. Carcinogenesis. 2001;22:519–523. doi: 10.1093/carcin/22.3.519. [DOI] [PubMed] [Google Scholar]
- Ploppa A, Kiefer RT, Nohé B, Haeberle HA, Dieterich HJ, Unertl KE, Durieux ME, Krueger WA. Monocyte phagocytosis of viable Staphylococcus aureus is impaired by barbiturates, but not by propofol. Infection. 2008;36:220–225. doi: 10.1007/s15010-007-7240-3. [DOI] [PubMed] [Google Scholar]
- Pogribny IP, Rusyn I. Environmental toxicants, epigenetics, and cancer. Adv Exp Med Biol. 2013;754:215–232. doi: 10.1007/978-1-4419-9967-2_11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riegler T, Nejabat M, Eichner J, Stiebellehner M, Subosits S, Bilban M, Zell A, Huber WW, Schulte-Hermann R, Grasl-Kraupp B. Proinflammatory mesenchymal effects of the non-genotoxic hepatocarcinogen phenobarbital: a novel mechanism of antiapoptosis and tumor promotion. Carcinogenesis. 2015;36:1521–1530. doi: 10.1093/carcin/bgv135. [DOI] [PubMed] [Google Scholar]
- Roberts RA, Ganey PE, Ju C, Kamendulis LM, Rusyn I, Klaunig JE. Role of the Kupffer cell in mediating hepatic toxicity and carcinogenesis. Toxicol Sci. 2007;96:2–15. doi: 10.1093/toxsci/kfl173. [DOI] [PubMed] [Google Scholar]
- Rossano F, Tufano R, Cipollaro de L’Ero G, Servillo G, Baroni A, Tufano MA. Anesthetic agents induce human mononuclear leucocytes to release cytokines. Immunopharmacol Immunotoxicol. 1992;14:439–450. doi: 10.3109/08923979209005403. [DOI] [PubMed] [Google Scholar]
- Schuetz EG, Brimer C, Schuetz J. Environmental xenobiotics and the antihormones cyproterone acetate and spironolactone use the nuclear hormone pregnenolone X receptor to activate the CYP3A23 hormone response element. Mol Pharmacol. 1998;54:1113–1117. doi: 10.1124/mol.54.6.1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulte-Hermann R, Ohde G, Schuppler J, Timmermann-Trosiener I. Enhanced proliferation of putative preneoplastic cells in rat liver following treatment with the tumor promoters phenobarbital, hexachlorocyclohexane, steroid compounds, and nafenopin. Cancer Res. 1981;41:2556–2562. [PubMed] [Google Scholar]
- Schulte-Hermann R, Timmermann-Trosiener I, Barthel G, Bursch W. DNA synthesis, apoptosis, and phenotypic expression as determinants of growth of altered foci in rat liver during phenobarbital promotion. Cancer Res. 1990;50:5127–5135. [PubMed] [Google Scholar]
- Schuppler J, Günzel P. Liver tumours and steroid hormones in rats and mice. Arch Toxicol. 1979;2:181–195. doi: 10.1007/978-3-642-67265-1_16. [DOI] [PubMed] [Google Scholar]
- Shapiro PA, Antonioli DA, Peppercorn MA. Barbiturate-induced submassive hepatic necrosis. Report of a case and review of the literature. Am J Gastroenterol. 1980;74:270–273. [PubMed] [Google Scholar]
- Shizu R, Benoki S, Numakura Y, Kodama S, Miyata M, Yamazoe Y, Yoshinari K. Xenobiotic-induced hepatocyte proliferation associated with constitutive active/androstane receptor (CAR) or peroxisome proliferator-activated receptor α (PPARα) is enhanced by pregnane X receptor (PXR) activation in mice. PLoS ONE. 2013;8:e61802. doi: 10.1371/journal.pone.0061802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smyth GK. Linear models and empirical bayes methods for assessing differential expression in microarray experiments. Stat Appl Genet Mol Biol. 2004;3:1–25. doi: 10.2202/1544-6115.1027. [DOI] [PubMed] [Google Scholar]
- Tokumoto T, Hossain MB, Wang J. Establishment of procedures for studying mPR-interacting agents and physiological roles of mPR. Steroids. 2016;111:79–83. doi: 10.1016/j.steroids.2016.02.015. [DOI] [PubMed] [Google Scholar]
- Trinka E, Kälviäinen R. 25 years of advances in the definition, classification and treatment of status epilepticus. Seizure. 2017;44:65–73. doi: 10.1016/j.seizure.2016.11.001. [DOI] [PubMed] [Google Scholar]
- Urakawa N, Utsunomiya S, Nishio M, Shigeoka M, Takase N, Arai N, Kakeji Y, Koma Y, Yokozaki H. GDF15 derived from both tumor-associated macrophages and esophageal squamous cell carcinomas contributes to tumor progression via Akt and Erk pathways. Lab Invest. 2015;95:491–503. doi: 10.1038/labinvest.2015.36. [DOI] [PubMed] [Google Scholar]
- Watanabe S, Cui Y, Tanae A, Tanaka T, Fujimoto M, Matsuo Y, Tachibana K, Yamasaki S. Follow-up study of children with precocious puberty treated with cyproterone acetate. Ad hoc Committee for CPA. J Epidemiol. 1997;7:173–178. doi: 10.2188/jea.7.173. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.