Abstract
The rodenticide tetramethylenedisulfotetramine (TETS) is a potent convulsant (lethal dose in humans 7–10 mg) that is listed as a possible threat agent by the United States Department of Homeland Security. TETS has previously been studied in vivo for toxicity and in vitro in binding assays, with the latter demonstrating it to be a non-competitive antagonist on GABAA receptors. To determine whether TETS exhibits subtype selectivity for a particular GABAA receptor combination, we used whole-cell patch-clamp to determine the potency of TETS on the major synaptic and extrasynaptic GABAA receptors associated with convulsant activity. The active component of picrotoxin, picrotoxinin, was used as a control. While picrotoxinin did not differentiate well between 13 GABAA receptors, TETS exhibited the highest activity on α2β3γ2 (IC50 480 nM, 95% CI 320–640 nM) and α6β3γ2 (IC50 400 nM, 95% CI 290–510 nM). Introducing β1 or β2 subunits into these receptor combinations reduced or abolished TETS sensitivity, suggesting that TETS preferentially affects receptors with α2/β3 or α6/β3 composition. Since α2β3γ2 receptors make up 15–20% of the GABAA receptors in the mammalian CNS, we suggest that α2β3γ2 is probably the most important GABAA receptor for the seizure-inducing activity of TETS.
Keywords: TETS, GABAA receptor, Electrophysiology, Picrotoxinin, Convulsant, Threat agent
Introduction
GABAA receptors are heteropentameric ligand-gated chloride channels that are activated by gamma-aminobutyric acid (GABA), the main inhibitory neurotransmitter in the adult CNS. GABAA receptors have a complex and often somewhat promiscuous pharmacology with numerous orthosteric and allosteric sites that modulate channel function (Krall et al. 2015; Olsen 2015). While GABAA receptor agonists and positive allosteric modulators reduce neuronal excitability and can be used as anxiolytics and anticonvulsants, compounds that inhibit GABAA receptor functions increase neuronal firing and promote seizures. TETS (tetramethylenedisulfotetramine) and picrotoxin are both potent convulsants (Haskell and Voss 1957; Zolkowska et al. 2012) that can cause severe tonic–clonic seizures and are, therefore, considered threat agents by the United States Department of Homeland Security. Both compounds are thought be to work through a similar mechanism; nonselective inhibition of GABAA receptors, yet TETS is 30–100-fold more potent as a convulsant and lethal toxin in the mouse than picrotoxin (Lamanna and Hart 1968; Shandra et al. 1996).
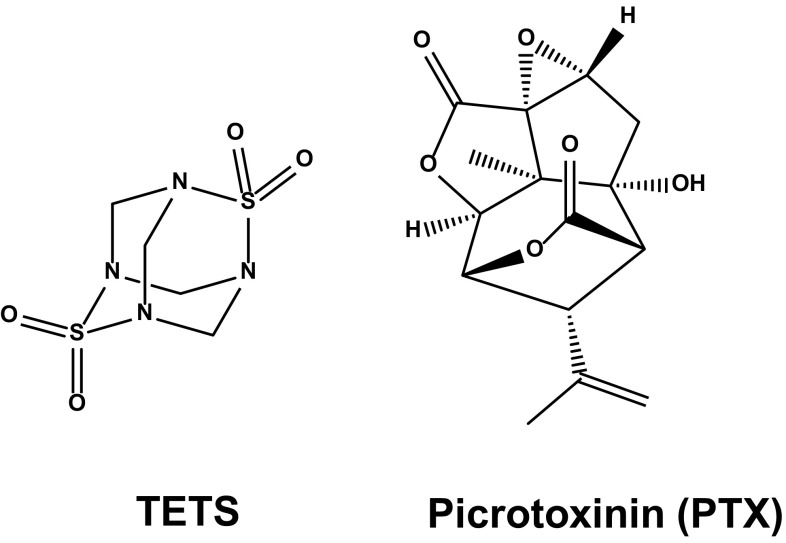
GABAA receptors exhibit a high degree of structural heterogeneity and exist in multiple subtypes (Olsen and Sieghart 2009), with each subtype being a pentamer assembled from a pool of 19 possible subunits, α1–α6, β1–β3, γ1–γ3, δ, ε, π, θ, and ρ1–ρ3. Based on the fact that TETS and picrotoxin are structurally somewhat similar but distinct (Fig. 1), we wondered if the two agents would exhibit different GABAA receptor subtype specificities. Picrotoxin can be isolated from seeds of the moonseed family and has an extremely bitter taste. It is an equimolar mixture of two tricyclic sesquiterpenes: picrotin and the active component picrotoxinin (Slater and Wilson 1951). TETS has similar physicochemical properties, but is easy to synthesize, tasteless and odorless, and stable in drinking water for months (Knaack et al. 2014). These characteristics make TETS a tangible threat.
Fig. 1.
Chemical structures of TETS and picrotoxinin
TETS was first synthesized in 1933 from sulfamide and formaldehyde (Wood and Battye 1933) and then used as an anti-mold agent for upholstery. Its severe toxicity first became apparent in a German furniture factory where workers accidentally exposed to TETS-impregnated wool suffered from disorientation and seizures (Hagen 1950). TETS was later resynthesized under laboratory conditions and found to be exceptionally poisonous with an extremely low parenteral LD50 of 0.1–0.3 mg/kg in rodents (Casida et al. 1976; Haskell and Voss 1957). The United States Forestry Department explored TETS as a rodenticide but eventually abandoned it due to its extreme toxicity, the lethal dose in adult humans being 7–10 mg (Guan et al. 1993), the lack of a viable rescue agent, and its persistence in the environment (Whitlow et al. 2005). TETS is currently banned worldwide, but continues to be easily obtainable and popular as a rodenticide in China, where several mass poisonings with malicious intent have occurred (Whitlow et al. 2005; Zhang et al. 2011). There have also been cases of reported TETS poisonings in the United States with material sourced from China as an indoor rodenticide (Barrueto et al. 2003; Whitlow et al. 2005). The first pharmacological information about TETS was generated by Alfred Haskell and Voss (1957), who tested TETS on organ preparations from frogs, rats, cats, and dogs and found that TETS acted exclusively on the brain without exhibiting any activity on peripheral nerves or muscle. Seizures only terminated with severance below the medulla. The fact that sub-lethal doses of TETS could reverse pentobarbital-induced decreases in blood pressure and respiration in dogs pointed towards a mechanism potentially involving GABAA receptors. TETS was later shown to displace [35S]t-butylbicyclophosphorothionate ([35S]TBPS) binding to rat brain membranes with an IC50 of 1 μM (Esser et al. 1991; Squires et al. 1983), and to prevent 36Cl− uptake (Ratra et al. 2001) or to inhibit chloride currents (Barnych et al. 2017) through α1β2γ2 GABAA receptors expressed in HEK293 cells with IC50 values of 1.3 or 8 μM, respectively. Interestingly, recent work from the Casida laboratory (Zhao et al. 2014) showed that “cold”-TETS displaces [14C]TETS from rat brain membranes with a much lower IC50 of 80 nM than it displaces another radiolabeled caged convulsant, 4′-ethynyl-4-n-[3H]propylbicycloorthobenzoate (EBOB), suggesting that TETS is binding to a site that is only partially overlapping with the EBOB or TBPS site on various GABAA receptors or that it might exhibit a specific GABAA receptor subtype selectivity. We here tested the later possibility using patch-clamp electrophysiology in an attempt to find an explanation for the discrepancy between the relatively low potency of TETS in inhibiting GABAA receptors and its high in vivo toxicity (Lamanna and Hart 1968; Zolkowska et al. 2012).
Materials and methods
Chemicals
Picrotoxinin (PTX), fipronil, bicuculline, propofol, salicylidene salicylhydrazide, zinc chloride, GABA, dexamethasone, zeocin, and geneticin were purchased from Sigma Aldrich (St. Louis, MO, United States). Diazepam, allopregnanolone, and DS2 (4-chloro-N-[2-(2-thienyl)imidazo[1,2-a]pyridin-3-yl]benzamide) were purchased from Tocris Bioscience (Bristol, United Kingdom). TETS was synthesized in the laboratory of Dr. Bruce Hammock, University of California, Davis, CA (Zhao et al. 2014). 10 mM stocks of GABA were made fresh daily using Ringer solution (see below for composition). 10 mM stocks of PTX and TETS were prepared in DMSO and diluted down into Ringer solution immediately before application onto the cell. Both TETS and PTX waste were treated with nitric acid and disposed of using the waste accumulation program at UC Davis.
Preparation of cells expressing the GABAA receptors
The human GABAA receptors α1, α2, α6, β1, β3, γ2L, and δ and the rat GABAA receptor β2 cloned into pcDNA3.1 expression vectors were a gift from Dr. Robert L. Macdonald, Vanderbilt University, Nashville, TN. The human GABAA receptor α4 cloned into a pcDNA3.1 expression vector was a gift from Dr. Richard Olson, University of California, Los Angeles, CA. The human GABAA receptor γ1 cloned into a pcDNA3.1 expression vector and a Lt-K cell line stably expressing α4β3δ (Mortensen et al. 2010) were gifts from Dr. Trevor Smart, University College London, United Kingdom. L929 cells, a mouse fibroblast cell line (CCL-1), were obtained from ATCC (American Type Culture Collection, Manassas, VA, United States), and were used for expressing all GABAA receptors with the exception of the receptor combination α6β3δ for which COS-7 cells (ATCC CRL-1651) were used to increase transfection efficacy and expression. L929, Lt-K, and COS-7 cells were cultured in Dulbecco’s modified Eagle’s medium (Lonza, Basel, Switzerland) supplemented with 10% fetal bovine serum, 100 U/mL penicillin and 100 mg/mL streptomycin (Invitrogen, ThermoFisher, Grand Island, NY, United States) and maintained in humidified 95% air and 5% CO2 air at 37 °C. The Lt-K cell line expressing α4β3δ was cultured with 1 mg/mL geneticin and 0.2 mg/mL of zeocin to maintain selection pressure. Two days before experiments, 1 μM dexamethasone was added to the media to induce α4 and β3 expressions (Mortensen et al. 2010). L929 or COS-7 cells were transfected using FuGENE 6 (ThermoFisher, Grand Island, NY, United States) transfection reagent in Opti-MEM® reduced serum medium (Life Technologies, Benicia, CA, United States) with an equal amount of each of the subunits (1:1:1) in combination with green fluorescent protein (GFP) expressed from the pEGFP-C1 vector (Invitrogen). The ratio of total cDNA to transfection reagent was 2:1. 48 h post-transfection, and cells were detached by trypsinization, washed, and plated onto poly-l-lysine-coated glass coverslips. Transfected cells were identified as GFP-expressing cells, using an epifluorescence microscope for electrophysiological whole-cell voltage-clamp studies. Correct subunit assembly was tested with a battery of GABAA receptor positive allosteric modulators and inhibitors (Table 1).
Table 1.
Pharmacological signature of expressed GABAA receptor isoforms
| GABAA isoform | Sensitivity to positive allosteric modulators | Sensitivity to inhibitors |
|---|---|---|
| α1β12γL | Diazepam+, Propofol+, Allopregnanolone+ | SAS+, Bicuculline+, Fipronil+ |
| α1β2γ2L | Diazepam+, Propofol+, Allopregnanolone+ | Fipronil+ |
| α1β3γ2L | Diazepam+, Propofol+, Allopregnanolone+ | Fipronil+ |
| α2β2γ2L | Diazepam+, Propofol+ | Fipronil+ |
| α2β3γ2L | Diazepam+, Propofol+, Allopregnanolone+ | SASneg, Bicuculline+, Fipronil+, Zn2+neg |
| α2β3 | Diazepamneg, Propofol+, | Fipronil+ |
| α4β3γ2L | Diazepamneg, Propofol+, | Fipronil+ |
| α4β3δ | Diazepamneg, Allopregnanolone+, DS2+ | Fipronil+ |
| α6β1γ2L | Diazepamneg | SAS+, Bicuculline+, Fipronil+ |
| α6β2γ2L | Diazepamneg, Propofol+ | Fipronil+ |
| α6β3γ2L | Diazepamneg, Propofol+, Allopregnanolone+ | SASneg, Bicuculline+, Fipronil+, Zn2+neg |
| α6β3 | ND | Zn2+ positive |
| α6β3γ1 | Diazepamneg, Propofol+ | Fipronil+ |
| α6β3δ | Diazepamneg, DS2+ | Fipronil+ |
Sensitivity to 10 μM diazepam, 250 nM Allopregnanolone, 100 μM Propofol, 50 μM DS2 (4-chloro-N-[2-(2-thienyl)imidazo[1,2-a]pyridin-3-yl]benzamide), 10 μM Fipronil, 100 μM Bicuculline, 10 μM SAS (salicylidene salicylhydrazide) and 10 μM ZnCl2 was tested on 3–10 cells per subunit combination
ND Not determined
Electrophysiological recordings
Whole-cell voltage-clamp experiments were performed at room temperature with an EPC-10 HEKA amplifier (HEKA Elektronik, Lambrecht, Germany). Cells were bathed in Ringer solution consisting of 160 mM NaCl, 4.5 mM KCl, 1 mM MgCl2, 2 mM CaCl2, 10 mM HEPES, pH 7.4, 311 mOsm. Recording electrodes were pulled from soda lime glass micro-haematocrit tubes (Kimble Chase, Rochester, NY, United States) and fire-polished to resistances of 1.8–2.8 MΩ for voltage-clamp. Electrodes were filled with an internal solution consisting of 154 mM KCl, 2 mM CaCl2, 1 mM MgCl2, 10 mM HEPES, and 10 mM EGTA with pH 7.2 and 305 mOsm. Cells were voltage-clamped at − 80 mV and control currents were recorded under the application of varying GABA concentrations for 5 s followed by a 55 s wash with external Ringer solution using a gravity-fed fast perfusion system (VC38 system, ALA Scientific, Farmingdale, NY, United States).
The GABA concentration–response relationships were determined by testing increasing concentrations of GABA and normalizing the GABA-induced peak currents to the peak currents induced by a maximal concentration of GABA. The normalized current responses were subsequently fitted using the Hill equation to determine EC50 and EC90.
For the TETS and PTX concentration–response curves, test solutions were freshly prepared immediately before application onto cells. A near maximal concentration of GABA (GABA EC90) was applied for 5 s and then washed out for 55 s. TETS or PTX was then perfused in a volume of 3–5 mL directly into the bath through a side port on the perfusion chamber and cells incubated with the inhibitor for 3 min before a 5 s pulse of GABA was applied to the patch-clamped cell. The convulsant was then washed out and another control GABA pulse applied. One cell was used per concentration of the convulsant. For analysis of receptor blockade, the area under the current curve (AUCMax) was determined for the control (EC90 GABA) and AUCEx after exposure:
For competition experiments, drug was applied for 5 s followed by 55 s of wash with Ringer. The cells were then exposed to GABA or GABA plus the convulsant (TETS or PTX) without any pre-incubation. GABA-induced responses in the presence and absence of convulsant were quantified by analyzing the peak response.
Data analysis was performed using the Excel (Microsoft) and Origin 9.1 (OriginLab Corporation, Northampton, MA, United States) software. Data fitting to the Hill equation to obtain EC50 or IC50 values were also performed using Origin 9.1. Individual data points are presented as mean ± SD from 3 to 8 independent recordings. EC50 and IC50 values are presented with 95% confidence intervals.
Results
GABA concentration responses
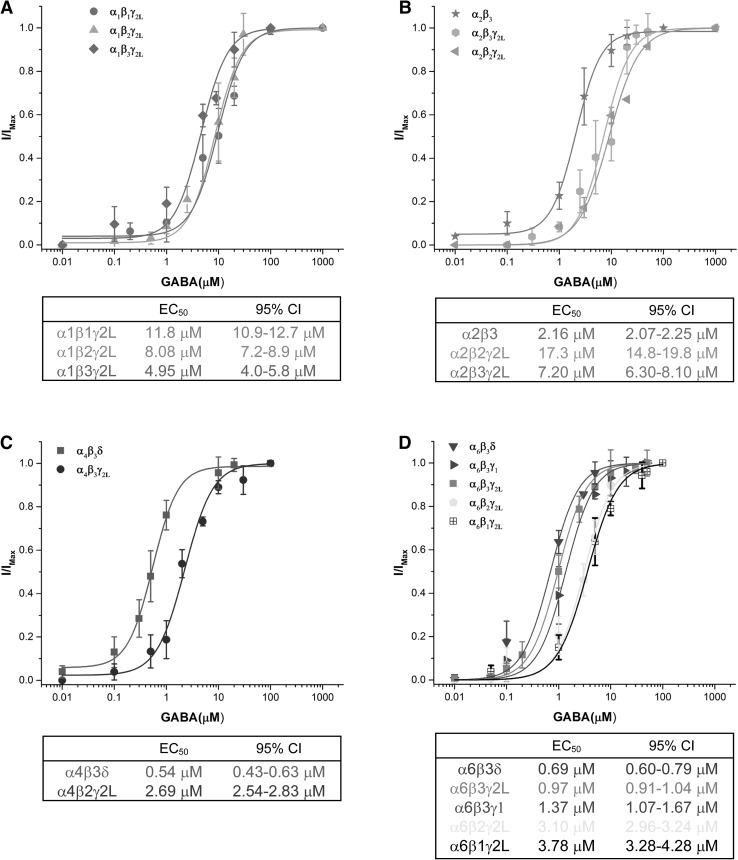
Before studying TETS activity, we first obtained GABA concentration–response curves for 13 synaptic and extrasynaptic GABAA receptor isoforms transiently or stably expressed in L929 cells, a mouse fibroblast cell line that has been used to express GABAA receptors since the early 1990s (Angelotti et al. 1993). Correct subunit assembly and γ2L or δ incorporation were confirmed with a battery of GABAA receptor probes consisting of the positive allosteric modulators diazepam, propofol, allopregnanolone, and DS2 and the inhibitors fibronil, bicuculline, salicylidene salicylhydrazide, and zinc chloride (Table 1). For both the exemplary synaptic GABAA receptors α1β1γ2L, α1β2γ2L, α1β3γ2L (Fig. 2a), α2β3, α2β2γ2L, and α2β3γ2L (Fig. 2b) and the exemplary extrasynaptic GABAA receptors α4β3δ, α4β3γ2L (Fig. 2c), α6β3δ, α6β3γ1, α6β2γ2L, α6β3γ2L, and α6β1γ2L (Fig. 2d), we determined GABA EC50 and EC90 values to choose the most appropriate GABA concentrations for subsequently evaluating TETS and PTX effects on each of these receptors. When comparing our EC50 values to the previous work in the field, we found that most of our results are in good agreement with data obtained by Mortson et al. (2011), who transiently expressed various synaptic and extrasynaptic GABAA receptors in HEK cells and reported a very similar overall ranking of GABA sensitivity. However, we observed a few differences. In our hands, α6 containing combinations were generally 2–3-fold less sensitive to GABA than previously reported. For example, we obtained an EC50 of 0.69 μM for α6β3δ (Fig. 2d), whereas Mortenson et al. reported EC50 of 0.17 μM for this same subunit combination (Mortensen et al. 2011). Despite this difference in sensitivity, we observed the expected pharmacological responses, specifically, no response to diazepam but a pronounced response to DS2 (Table 1).
Fig. 2.
GABA concentration–response curves for α1 (a), α2 (b), α4 (c), and α6 (d) containing GABAA receptor combinations. Individual data points are presented as mean ± SD from 7–20 independent recordings. EC50 values are presented with 95% confidence intervals
Importance of the β subunit in TETS activity
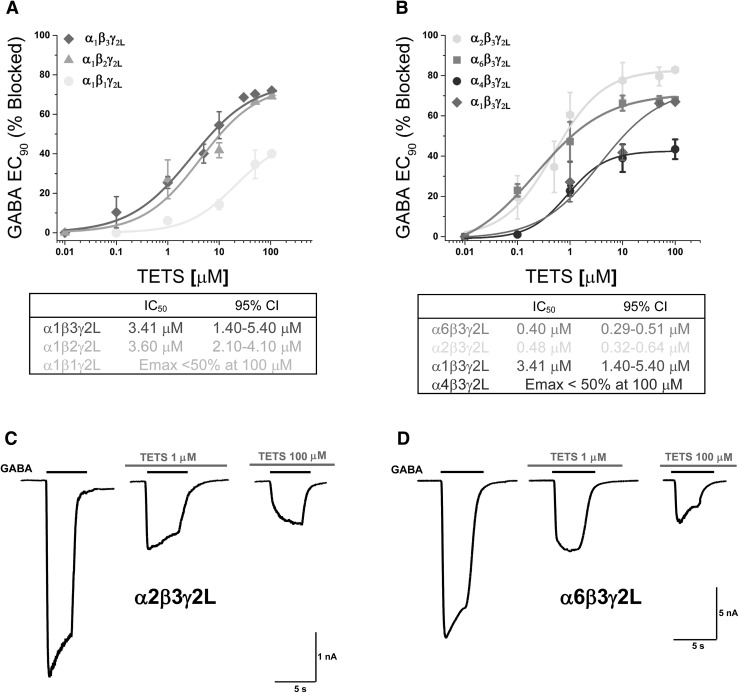
Based on molecular dynamics simulations using a homology model of the pore region of the α1β2γ2 GABAA receptor, TETS has been hypothesized to bind in the pore lumen by hydrogen bonding with two α1–M2 segments and one γ2–M2 segment without making any contacts with the β subunit (Zhao et al. 2014). In support of this hypothesis, the β3 homopentamer has been shown to not bind TETS even at concentrations greater than 10 μM (Ratra et al. 2001). To determine if the β subunit is really not important for TETS activity, as suggested by these studies, we tested all three β subunits, β1, β2, and β3, in combination with α1 and γ2 (Fig. 3a). We started with α1β2γ2, since it is the most abundant subunit combination, constituting ~ 60% of GABAA receptors in the mammalian brain (Rudolph and Knoflach 2011; Sur et al. 2001). GABA-induced chloride current at GABA EC90 through this subunit exhibited a moderate sensitivity to inhibition by TETS (IC50 3.6 μM). Following pre-incubation with different TETS concentrations, block developed quickly, and TETS inhibition was fully reversible on washout; however, even concentrations as high as 100 μM could not fully block the current and only achieved a maximal inhibition of ~ 70%. The remaining GABA-induced chloride current could be blocked by 100 μM of bicuculline or 10 μM of fipronil (data not shown). To determine the significance of changing the β subunit, we replaced it with both β1 and β3. While α1β1γ2 was not very sensitive to TETS (maximal block < 50% at 100 μM), α1β3γ2 was indistinguishable from the β2 containing subunit combination in terms of TETS potency and maximal efficacy (Fig. 3a). We, therefore, concluded that both β2 and β3 subunits can modulate TETS binding.
Fig. 3.
a Concentration–response curves comparing TETS inhibition of different β subunits in the α1βXγ2L combination. b Comparison of TETS inhibition of α1, α2, α4, and α6 subunits in αXβ3γ2L containing GABAA receptor combinations. Individual data points are presented as mean ± SD from 3–8 independent recordings. EC50 values are presented with 95% confidence intervals. Example traces showing TETS inhibition of α2β3γ2L (c) and α6β3γ2L (d) receptors. EC90 GABA was applied first alone as control and then in the presence of 1 or 100 μM of TETS
Understanding the significance of the α subunit in TETS activity on GABAA receptors
We next investigated the role of the α subunit in TETS activity by exchanging α1 for α2, α4, and α6 in the αXβ3γ2L combination (Fig. 3b). We chose this combination rather than the αXβ2γ2L combination, because the β3 we are using for this work is human, whereas β2 is a rat clone. We did not investigate α5, because this subunit is not thought to be involved in seizure generation, but rather plays a role in learning and memory (Collinson et al. 2002; Rudolph and Mohler 2004). Out of the tested subunit combinations, α2β3γ2L (IC50 = 480 nM with a maximal block of ~ 80%) and α6β3γ2L (IC50 = 400 nM with a maximal block of ~ 75%) showed the highest sensitivity to TETS (Fig. 3b), while α1β3γ2L was roughly tenfold less sensitive (α1β3γ2L: IC50 = 3.6 μM with a maximal block of ~ 75%). On the α4β3γ2L combination, even 100 μM of TETS could not achieve more than 45% of inhibition, making this subunit combination the least sensitive.
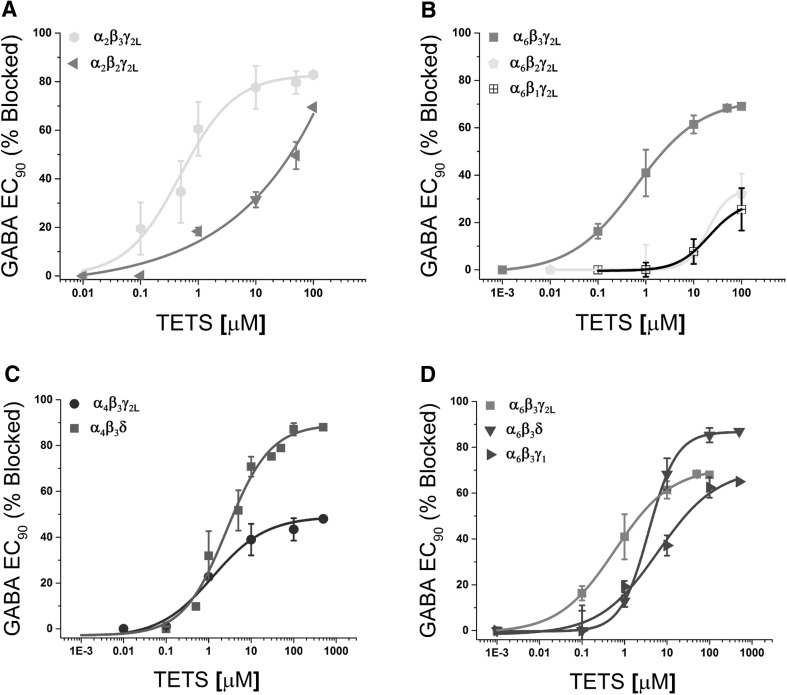
Does the β subunit affect the TETS sensitivity of α2 and α6?
We had seen that there was no difference in TETS sensitivity between β2 and β3 when these subunits were expressed with α1 (Fig. 3a). It was important to determine if this was also true for the more sensitive α2 and α6 subunits and we, therefore, next co-expressed these two subunits with β2 instead of β3. In both combinations, TETS clearly showed a preference for β3 containing subunit combinations over β2 containing combinations (Fig. 4a, b). For the α2βXγ2L combination, replacing β3 with β2 shifted the TETS concentration–response curve significantly to the right, and increased IC50 from 400 nM to 12.2 μM (Fig. 4a). For the α6βXγ2L combination, the effect was even more dramatic, and in the presence of β2, even 100 μM of TETS no longer achieved more than 40% inhibition of GABA-induced chloride current (Fig. 4b). Replacing β3 with β1 further reduced TETS activity with 100 μM of TETS only achieving 25% inhibition of current through α6β1γ2L (Fig. 4b). Based on these results, we conclude that the presence of an α2 or α6 subunit and a β3 subunit is necessary for TETS to inhibit chloride currents through GABAA receptors with high potency and efficacy.
Fig. 4.
a Concentration–response curves for TETS inhibition of currents evoked by EC90 GABA for α2βxγ2L receptors to determine the changes induced by exchanging β2 for β3. The concentration response curve of TETS for α2β2γ2L (IC50 12.2 μM, 95% CI 10.5–15.8 μM, E max ~ 65%) was right-shifted in comparison with α2β3γ2L (IC50 480 nM, 95% CI 10.5–15.8 nM, E max ~ 80%). b Both the α6β1γ2L receptor (IC50 > 20 μM, E max ~ 25%) and the α6β2γ2L receptor (IC50 20 μM, 95% CI 18.3–21.7 μM, E max ~ 35%) showed a significantly reduced response to TETS. The α6β3γ2L receptor (IC50 400 nM, 95% CI 290–510 nM, E max ~ 70%) is highly sensitive to TETS as shown previously in Fig. 3. c α4β3γ2L receptor (IC50 1.82 μM, 95% CI 1.02–2.62 μM, E max ~ 46%, n H = 0.7) showed a reduced E max for TETS inhibition, while the α4β3δ receptor (IC50 3 μM, 95% CI 1.36–3.96 μM, E max ~ 85%, n H = 1.2) showed an increased Hill coefficient. d In α6 containing receptors (α6β3γ2L: IC50 400 nM, 95% CI 0.29–0.51 nM E max ~ 70% as previously shown), introduction of a δ subunit increased E max and reduced potency (α6β3δ: IC50 3.69 μM, 95% CI 3.18–4.2 μM, E max ~ 85%), while replacement of γ2L with γ1 right-shifted the concentration response curve (α6β3γ1: IC50 6.81 μM, 95% CI 3.9–9.7 μM, E max ~ 65%). Individual data points are presented as mean ± SD from 3–9 independent recordings. EC50 values are presented with 95% confidence intervals. Please note that the α4β3δ receptor combination was stably expressed in Lt-K cells, while the α6β3δ combination was transiently expressed in COS-7 cells
Significance of the γ and δ subunits in TETS activity
We next tested if δ could possibly play a role in TETS activity, and, therefore, determined its potency for blocking currents through the extrasynaptic α4β3δ GABAA receptor stably expressed in Lt-K cells and the α6β3δ receptor transiently transfected into COS-7 cells. We used COS-7 cells for these experiments, because the α6β3δ combination did not express well in L929 cells (peak currents < 200 pA). We chose not to try and generate the α2β3δ GABAA receptor, since there seems to be no evidence for the existence of this subunit combination in the literature (Olsen and Sieghart 2008, 2009). Interestingly, in the two δ containing subunit combinations, we investigated the presence of a δ subunit increased the maximal efficacy of TETS inhibition when compared with the γ2L containing GABAA receptor combinations, and also changed the Hill coefficient (Fig. 4c, d). However, it should be noted here that the two δ containing subunit combinations in our study, α4β3δ and α6β3δ, were expressed in two different cell lines, Lt-K and COS-7, which could have impacted our results.
Overall, α4 containing receptors are not very sensitive to TETS (α4β3γ2L: IC50 = 1.82 μM, E max = 46%, n H = 0.7), as previously shown in Fig. 3, but TETS inhibited the δ containing α4β3δ receptor with an increased efficacy (IC50 = 2.66 μM, E max = 85%; Fig. 4c) and a steeper Hill coefficient (n H = 1.2). The same effect was observed in the more TETS-sensitive α6 combination (Fig. 4d). While α6β3δ was less sensitive (IC50 = 3.69 μM) to TETS inhibition than the α6β3γ2L receptor (IC50 = 400 nM, E max = 64%, n H = 0.7), TETS displayed a greater efficacy (E max = 85%) and a steeper Hill coefficient (n H = 1.3) for α6β3δ (Fig. 4d). In contrast, exchanging γ2 for γ1 “simply” shifted the TETS concentration–response curve to the right and reduced potency, but maintained efficacy (α6β3γ1: IC50 = 6.81 μM, E max = 60%). We further tested α2β3 to see how removing the γ subunit would change TETS sensitivity and found that the absence of a γ subunit in the receptor pentamer lowered both the potency and efficacy of TETS (Table 2).
Table 2.
IC50 values for TETS and PTX
| GABAA isoform | TETS (μM) | 95% CI | PTX (μM) | 95% CI |
|---|---|---|---|---|
| α1β1γ2L | > 20 | – | > 30 | – |
| α1β2γ2L | 3.60 | 2.1–4.1 | 7.98 | 6.58–9.38 |
| α1β3γ2L | 3.41 | 1.4–5.4 | 3.7 | 2.1–5.3 |
| α2β2γ2L | 12.2 | 10.5–15.8 | 11 | 8.6–13.5 |
| α2β3γ2L | 0.48 | 0.32–0.64 | 7.5 | 5.2–9.9 |
| α2β3 | 3.37 | 2.77–3.97 | 1.98 | 0.67–3.29 |
| α4β3γ2L | 1.82 | 1.02–2.62 | 3.0 | 1.7–4.3 |
| α4β3δ | 2.66 | 1.36–3.96 | ND | ND |
| α6β1γ2L | > 20 | – | ND | ND |
| α6β2γ2L | 20 | 18.3–21.7 | 26.9 | 20.3–33.2 |
| α6β3γ2L | 0.40 | 0.29–0.51 | 5.8 | 4.2–7.4 |
| α6β3γ1 | 6.81 | 3.9–9.7 | ND | ND |
| α6β3δ | 3.69 | 3.18–4.2 | ND | ND |
ND Not determined
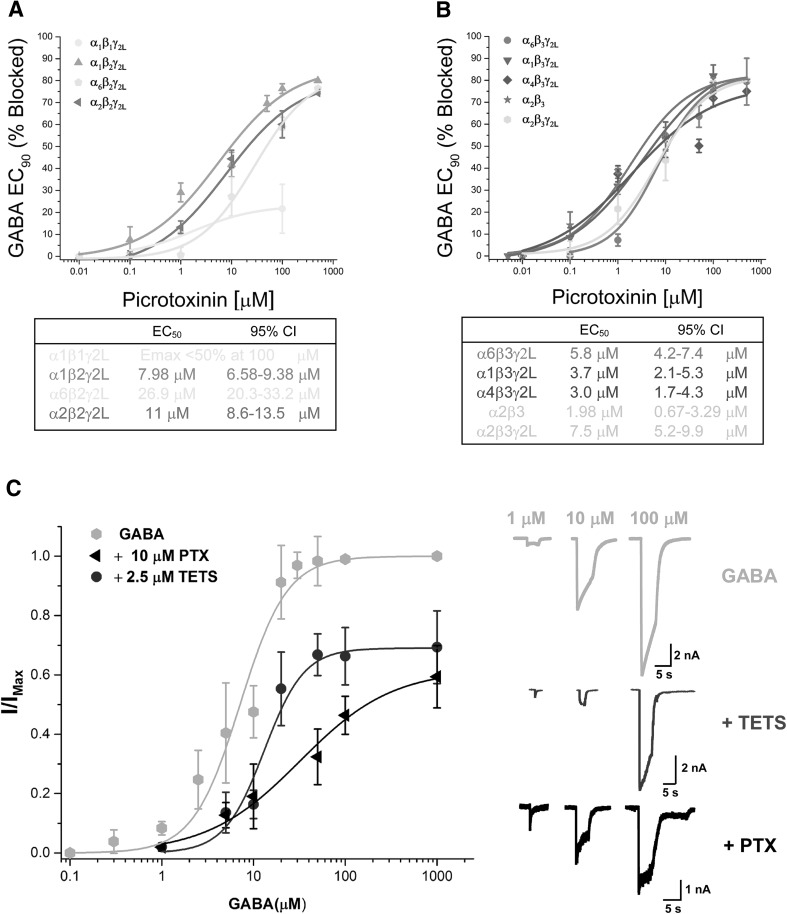
Picrotoxinin shows no GABAA receptor subtype selectivity
As a control, we tested picrotoxinin (PTX), which is a widely used GABAA receptor inhibitor also classified as a threat agent on the same receptor subtypes (Table 2 and Fig. 5). As expected based on data in the published literature, PTX is a relatively nonselective GABAA receptor inhibitor that blocks GABA-induced Cl− currents through most GABAA receptors with IC50s in 2–8 μM range and E max of ~ 80% current inhibition. Similar to TETS, the presence of a β1 subunit abolishes PTX sensitivity, since α1β1γ2L is insensitive to PTX, in contrast to various other β2 (Fig. 5a) or β3 (Fig. 5b) containing GABAA receptor combinations, which are all inhibited by PTX (Table 2).
Fig. 5.
Concentration-response curves for PTX inhibition of β1/β2 (a) and β3 (b) containing GABAA receptor combinations. c Effect of TETS and PTX are roughly IC80 concentrations on the GABA concentration response curve of the α2β3γ2L receptor. Individual data points are presented as mean ± SD 3–8 independent recordings. EC50 values are presented with 95% confidence intervals
TETS is a non-competitive GABAA receptor inhibitor
Finally, to start probing the mechanism of action of TETS on the α2β3γ2L receptor, we tested the effect of 2.5 μM TETS, which corresponds to IC80 on this receptor subtype, on the GABA concentration–response curve (Fig. 5c). As expected from the previously performed binding experiments (Zhao et al. 2014), TETS depressed the maximum GABA response elicited at 50 or 100 μM GABA and could not be competed off when the GABA concentration was increased to 1 mM, demonstrating that TETS is a non-competitive inhibitor similar to PTX, which was also tested at IC80 for comparison. PTX at 10 μM produced a similar depression of the GABA E max and was also not able to shift the GABA concentration–response curve fully to the right (Fig. 5c). Similar results were obtained with the other highly TETS-sensitive GABA receptor combination, α6β3γ2L (data not shown).
Discussion
The rodenticide TETS has previously been primarily studied in animal models to assess its convulsant activity and toxicity or in binding assays, which demonstrated that TETS acts as a non-competitive GABAA receptor inhibitor. However, so far, only very limited electrophysiological information is available for this highly toxic threat agent. In 1975, Bowery et al. demonstrated that TETS could reverse the effects of GABA on isolated superior cervical rat ganglions at concentrations between 10 and 100 μM (Bowery et al. 1975), while a group in the former Soviet Union showed in 1989 that 5 μM of TETS increased the excitability of hippocampal slices (Pervukhin et al. 1989). A more recent paper from our own group describing the synthesis of TETS-related haptens for the development of an ELISA assay to detect TETS (Vasylieva et al. 2017) reported that TETS inhibited chloride currents through α1β2γ2 GABAA receptors expressed in HEK293 cells with IC50 of 8 μM (Barnych et al. 2017). Since we were somewhat surprised by this relatively low potency in electrophysiological assays considering TETS has a reported LD50 of 0.1 mg/kg (Casida et al. 1976; Haskell and Voss 1957), we here investigated the GABAA receptor subtype selectivity of TETS using whole-cell patch-clamp electrophysiology. One observation that made us suspect that TETS might exhibit subtype selectivity was a report from the Casida laboratory that unlabeled TETS displaced [14C]TETS from rat brain membranes with IC50 of 80 nM (Zhao et al. 2014), which is much lower than IC50s usually reported for TETS displacement of other radiolabeled GABAA receptor antagonists such as EBOB (Zhao et al. 2014) or TBPS (Esser et al. 1991; Squires et al. 1983). Another report suggests that the possibility of a higher affinity target was Ca2+ dynamics measurements in mouse hippocampal neuronal cultures which develop spontaneous network activity after about 2 weeks in culture (Cao et al. 2012). TETS visibly altered Ca2+ dynamics in these networks at submicromolar concentrations, although the reported EC50s for altering the frequency and amplitude of the Ca2+-induced fluorescence changes in the assay were the 1–2 μM range (Cao et al. 2012).
Here, we identified two GABAA receptor subtypes that are sensitive to TETS at submicromolar concentrations: α2β3γ2 with IC50 of 480 nM and α6β3γ2 with IC50 of 400 nM. Of these two receptor subtypes, both of which are among the 11 GABAA receptors conclusively identified as native receptors (Olsen and Sieghart 2008), α2β3γ2 is probably the more important receptor for the seizure-inducing activity of TETS, since α2β3γ2 receptors make up 15–20% of the GABAA receptors in the mammalian CNS (Fritschy and Mohler 1995; Pirker et al. 2000; Rudolph and Knoflach 2011) and α2 containing GABAA receptors have been shown to significantly contribute to the anticonvulsant actions of diazepam (Fradley et al. 2007). In contrast, receptors with the α6β2/3γ2 composition constitute less than 5% of the GABAA receptors (Mohler et al. 2002; Rudolph and Knoflach 2011) and are largely restricted to the cerebellum (Jones et al. 1997). One short coming of our study is that we only used the long splice variant of the γ2 subunit, γ2L, and not the short γ2s subunit, which is known to be expressed throughout the mammalian CNS in similar proportions and often co-localizes with γ2L in the same receptor complexes (Khan et al. 1994).
TETS differs from the less selective PTX in showing preference for α2 and α6 over α1 and α4 when expressed in combination with β3 and γ2. Introducing a β1 subunit into the GABAA receptor heteropentamer dramatically decreases both TETS and PTX potency and efficacy, suggesting that the presence of an α/β1 interface disrupts binding for both compounds. In contrast, exchanging β3 for β2 or γ2 for the less commonly found γ1 reduces TETS activity by roughly tenfold (Table 2). However, β3 alone is not sufficient to generate a TETS binding site, since homopentameric β3 GABAA receptors have been shown to not bind TETS at concentrations of up to 10 μM, while they bind PTX with an affinity of 32 nM (Ratra et al. 2001). It is interesting that the presence of a β3 subunit in the preferred α2/β3 or α6/β3 combination plays such a large role in TETS action on the GABAA receptor. Of these two β subunits, β2 and β3, that are able to participate in TETS binding, the more sensitive β3 subunit is probably more important for the proconvulsant activity of TETS. Mice lacking the β3 subunit display features reminiscent of Angelman syndrome in humans including abnormal EEG with interictal spikes and slowing, seizures, hyperactivity, impaired learning, and memory and repetitive behavior (DeLorey et al. 1998; Handforth et al. 2005). In contrast, mice lacking β2 do not exhibit spontaneous seizures, but are less susceptible to the hypnotic actions of ethanol and the effects of benzodiazepines (Blednov et al. 2003; Sur et al. 2001).
While TETS and PTX thus differ in their GABAA receptor subtype selectivity, with TETS most likely exerting its major action on α2β3γ2 receptors and while PTX does not demonstrate any significant receptor selectivity, we hesitate to use this selectivity as an explanation for the greater in vivo toxicity of TETS, since the differences in potency could possibly also be pharmacokinetic in nature. When administered intraperitoneally in mice, TETS induces clonic seizures with ED50 of 0.14 mg/kg and is lethal at a dose of 0.3 mg/kg, which is roughly 40 times more potent than picrotoxin (Zolkowska et al. 2012). However, when TETS and picrotoxin (which in this case contained only 50% of the active picrotoxinin) were administered intraventricularly, they were found to be equipotent in their ability to induce convulsions (Zolkowska et al. 2012), suggesting that the higher potency of TETS when administered systemically could be due to brain penetration or brain uptake than PTX. Another possibility is of course that TETS has additional actions on other receptors than GABAA receptors that promote seizures and convulsions.
Both TETS and PTX failed to fully block GABA-induced chloride currents through all tested GABAA receptor subunit combinations under our experimental conditions in which we elicited near maximal currents using GABA EC90 concentrations for each receptor, and could typically only achieve 70–85% of block. It is of course possible that we could have achieved some additional block by applying millimolar TETS or PTX concentrations, but we chose to not test concentrations higher than 100 μM of TETS on most receptors, since we regard these high concentrations as physiologically unrealistic. However, it should be mentioned here that the remaining current could be blocked by bicuculline (100 μM) or fipronil (10 μM). Out of these two compounds, bicuculline is known to competitively inhibit GABA binding at the orthosteric site, although it also seems to have additional allosteric actions (Johnston 2013), while the phenylpyrazole fipronil has been shown to bind to the same site as picrotoxinin and several polychlorocycloalkane insecticides in radioligand binding assays on the homopentameric β3 receptor (Chen et al. 2006). This of course raises the question of the TETS binding site, which based on the non-competitive nature of its inhibition, and the observations that TETS displaces pore blockers like [35S]TBPS (Esser et al. 1991; Squires et al. 1983) and the cage convulsant EBOB (Ratra et al. 2001; Zhao et al. 2014) is most likely located in the pore region of the channel, where TETS has been predicted by molecular dynamics simulations to hydrogen bond with two α1–M2 segments and one γ2–M2 segment in a homology model of the α1β2γ2 GABAA receptor. This model (Zhao et al. 2014), which was based on the crystal structure of the homopentameric Caenorhabditis elegans glutamate-gated chloride channel (Hibbs and Gouaux 2011), and which has never been probed by mutagenesis, showed TETS making no contacts with the β subunit, thus, apparently providing an explanation for why the α1β2γ2 GABAA receptor is sensitive to TETS, while the β3 homopentamer is not (Ratra et al. 2001). This molecular model should be re-examined in light of our findings that TETS shows the highest potency for blocking chloride current through GABAA receptors containing α2 or α6 as well as β3 subunits. Ideally, the TETS binding site should be mapped through a combination of site-directed mutagenesis and molecular modeling using new homology models of the α2β3γ2, α2β2γ2 and the α1β2γ2 GABAA receptors based on the more recently crystallized human β3 homopentamer (Miller and Aricescu 2014).
Abbreviations
- AUC
Area under the curve
- CI
Confidence interval
- DMSO
Dimethylsulfoxide
- EBOB
4′-Ethynyl-4-n-propylbicycloorthobenzoate
- EC50
Concentration producing 50% effect
- Emax
Maximal effect
- GABA
Gamma-aminobutyric acid
- GFP
Green fluorescent protein
- IC50
Concentration producing 50% inhibition
- nH
Hill coefficient
- PTX
Picrotoxinin
- SD
Standard deviation
- TETS
Tetramethylenedisulfotetramine
- TBPS
t-Butylbicyclophosphorothionate
Compliance with ethical standards
Funding
This work was supported by the CounterACT Program, National Institutes of Health Office of the Director, and the National Institute of Neurological Disorders and Stroke [U54NS079202]. Brandon Pressly was supported by a National Institute of General Medical Sciences funded Pharmacology Training Program [T32GM099608].
References
- Angelotti TP, Uhler MD, Macdonald RL. Assembly of GABAA receptor subunits: analysis of transient single-cell expression utilizing a fluorescent substrate/marker gene technique. J Neurosci. 1993;13(4):1418–1428. doi: 10.1523/JNEUROSCI.13-04-01418.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnych B, Vasylieva N, Joseph T, Hulsizer S, Nguyen H, Cajka T, Pessah I, Wulff H, Gee S, Hammock B. Development of tetramethylenedisulfotetramine (TETS) hapten library: synthesis, electrophysiological studies and immune response in rabbits. Chemistry. 2017 doi: 10.1002/chem.201700783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrueto F, Jr, Furdyna PM, Hoffman RS, Hoffman RJ, Nelson LS. Status epilepticus from an illegally imported Chinese rodenticide: “tetramine”. J Toxicol Clin Toxicol. 2003;41(7):991–994. doi: 10.1081/CLT-120026523. [DOI] [PubMed] [Google Scholar]
- Blednov YA, Jung S, Alva H, Wallace D, Rosahl T, Whiting PJ, Harris RA. Deletion of the alpha1 or beta2 subunit of GABAA receptors reduces actions of alcohol and other drugs. J Pharmacol Exp Ther. 2003;304(1):30–36. doi: 10.1124/jpet.102.042960. [DOI] [PubMed] [Google Scholar]
- Bowery NG, Brown DA, Collins JF. Tetramethylenedisulphotetramine: an inhibitor of gamma-aminobutyric acid induced depolarization of the isolated superior cervical ganglion of the rat. Br J Pharmacol. 1975;53(3):422–424. doi: 10.1111/j.1476-5381.1975.tb07379.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao Z, Hammock BD, McCoy M, Rogawski MA, Lein PJ, Pessah IN. Tetramethylenedisulfotetramine alters Ca2+ dynamics in cultured hippocampal neurons: mitigation by NMDA receptor blockade and GABA(A) receptor-positive modulation. Toxicol Sci. 2012;130(2):362–372. doi: 10.1093/toxsci/kfs244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casida JE, Eto M, Moscioni AD, Engel JL, Milbrath DS, Verkade JG. Structure-toxicity relationships of 2,6,7-trioxabicyclo(2.2.2)octanes and related compounds. Toxicol Appl Pharmacol. 1976;36(2):261–279. doi: 10.1016/0041-008X(76)90006-5. [DOI] [PubMed] [Google Scholar]
- Chen L, Durkin KA, Casida JE. Structural model for gamma-aminobutyric acid receptor noncompetitive antagonist binding: widely diverse structures fit the same site. Proc Natl Acad Sci USA. 2006;103(13):5185–5190. doi: 10.1073/pnas.0600370103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collinson N, Kuenzi FM, Jarolimek W, Maubach KA, Cothliff R, Sur C, Smith A, Otu FM, Howell O, Atack JR, McKernan RM, Seabrook GR, Dawson GR, Whiting PJ, Rosahl TW. Enhanced learning and memory and altered GABAergic synaptic transmission in mice lacking the alpha 5 subunit of the GABAA receptor. J Neurosci. 2002;22(13):5572–5580. doi: 10.1523/JNEUROSCI.22-13-05572.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeLorey TM, Handforth A, Anagnostaras SG, Homanics GE, Minassian BA, Asatourian A, Fanselow MS, Delgado-Escueta A, Ellison GD, Olsen RW. Mice lacking the beta3 subunit of the GABAA receptor have the epilepsy phenotype and many of the behavioral characteristics of Angelman syndrome. J Neurosci. 1998;18(20):8505–8514. doi: 10.1523/JNEUROSCI.18-20-08505.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esser T, Karu AE, Toia RF, Casida JE. Recognition of tetramethylenedisulfotetramine and related sulfamides by the brain GABA-gated chloride channel and a cyclodiene-sensitive monoclonal antibody. Chem Res Toxicol. 1991;4(2):162–167. doi: 10.1021/tx00020a007. [DOI] [PubMed] [Google Scholar]
- Fradley RL, Guscott MR, Bull S, Hallett DJ, Goodacre SC, Wafford KA, Garrett EM, Newman RJ, O’Meara GF, Whiting PJ, Rosahl TW, Dawson GR, Reynolds DS, Atack JR. Differential contribution of GABA(A) receptor subtypes to the anticonvulsant efficacy of benzodiazepine site ligands. J Psychopharmacol. 2007;21(4):384–391. doi: 10.1177/0269881106067255. [DOI] [PubMed] [Google Scholar]
- Fritschy JM, Mohler H. GABAA-receptor heterogeneity in the adult rat brain: differential regional and cellular distribution of seven major subunits. J Comp Neurol. 1995;359(1):154–194. doi: 10.1002/cne.903590111. [DOI] [PubMed] [Google Scholar]
- Guan FY, Liu YT, Luo Y, Hu XY, Liu F, Li QY, Kang ZW. GC/MS identification of tetramine in samples from human alimentary intoxication and evaluation of artificial carbonic kidneys for the treatment of the victims. J Anal Toxicol. 1993;17(4):199–201. doi: 10.1093/jat/17.4.199. [DOI] [PubMed] [Google Scholar]
- Hagen J. Schwere Vergiftungen in Liner Polstermöbelfabrik durch einen neuartigen hoch toxischen Giftstoff (Tetramethylendisulfotetramin) Dtsch Med Wochenschr. 1950;75:183–184. doi: 10.1055/s-0028-1117825. [DOI] [Google Scholar]
- Handforth A, Delorey TM, Homanics GE, Olsen RW. Pharmacologic evidence for abnormal thalamocortical functioning in GABA receptor beta3 subunit-deficient mice, a model of Angelman syndrome. Epilepsia. 2005;46(12):1860–1870. doi: 10.1111/j.1528-1167.2005.00287.x. [DOI] [PubMed] [Google Scholar]
- Haskell AR, Voss E. The pharmacology of tetramine (tetraethylenedisulfotetramine) J Am Pharm Assoc Am Pharm Assoc. 1957;46(4):239–242. doi: 10.1002/jps.3030460412. [DOI] [PubMed] [Google Scholar]
- Hibbs RE, Gouaux E. Principles of activation and permeation in an anion-selective Cys-loop receptor. Nature. 2011;474(7349):54–60. doi: 10.1038/nature10139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston GA. Advantages of an antagonist: bicuculline and other GABA antagonists. Br J Pharmacol. 2013;169(2):328–336. doi: 10.1111/bph.12127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones A, Korpi ER, McKernan RM, Pelz R, Nusser Z, Makela R, Mellor JR, Pollard S, Bahn S, Stephenson FA, Randall AD, Sieghart W, Somogyi P, Smith AJ, Wisden W. Ligand-gated ion channel subunit partnerships: GABAA receptor alpha6 subunit gene inactivation inhibits delta subunit expression. J Neurosci. 1997;17(4):1350–1362. doi: 10.1523/JNEUROSCI.17-04-01350.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan ZU, Gutiérrez A, De Blas AL. Short and long form gamma 2 subunits of the GABAA/benzodiazepine receptors. J Neurochem. 1994;63(4):1466–1476. doi: 10.1046/j.1471-4159.1994.63041466.x. [DOI] [PubMed] [Google Scholar]
- Knaack JS, Hamelin EI, Magnuson M, Silvestri E, Ash D, Johnson RC. Quantitative analysis and stability of the rodenticide TETS (tetramine) in finished tap water. Anal Methods UK. 2014;6(8):2780–2784. doi: 10.1039/c3ay41912f. [DOI] [Google Scholar]
- Krall J, Balle T, Krogsgaard-Larsen N, Sorensen TE, Krogsgaard-Larsen P, Kristiansen U, Frolund B. GABAA receptor partial agonists and antagonists: structure, binding mode, and pharmacology. Adv Pharmacol. 2015;72:201–227. doi: 10.1016/bs.apha.2014.10.003. [DOI] [PubMed] [Google Scholar]
- Lamanna C, Hart ER. Relationship of lethal toxic dose to body weight of the mouse. Toxicol Appl Pharmacol. 1968;13(3):307–315. doi: 10.1016/0041-008X(68)90104-X. [DOI] [PubMed] [Google Scholar]
- Miller PS, Aricescu AR. Crystal structure of a human GABAA receptor. Nature. 2014;512(7514):270–275. doi: 10.1038/nature13293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohler H, Fritschy JM, Rudolph U. A new benzodiazepine pharmacology. J Pharmacol Exp Ther. 2002;300(1):2–8. doi: 10.1124/jpet.300.1.2. [DOI] [PubMed] [Google Scholar]
- Mortensen M, Ebert B, Wafford K, Smart TG. Distinct activities of GABA agonists at synaptic- and extrasynaptic-type GABAA receptors. J Physiol. 2010;588(Pt 8):1251–1268. doi: 10.1113/jphysiol.2009.182444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mortensen M, Patel B, Smart TG. GABA potency at GABA(A) receptors found in synaptic and extrasynaptic zones. Front Cell Neurosci. 2011;6:1. doi: 10.3389/fncel.2012.00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsen RW. Allosteric ligands and their binding sites define gamma-aminobutyric acid (GABA) type A receptor subtypes. Adv Pharmacol. 2015;73:167–202. doi: 10.1016/bs.apha.2014.11.005. [DOI] [PubMed] [Google Scholar]
- Olsen RW, Sieghart W. International Union of pharmacology. LXX. Subtypes of gamma-aminobutyric acid(A) receptors: classification on the basis of subunit composition, pharmacology, and function. Update. Pharmacol Rev. 2008;60(3):243–260. doi: 10.1124/pr.108.00505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsen RW, Sieghart W. GABA A receptors: subtypes provide diversity of function and pharmacology. Neuropharmacology. 2009;56(1):141–148. doi: 10.1016/j.neuropharm.2008.07.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pervukhin G, Sharonova IN, Prokof’ev SE, Fedorov NB, Kotel’nikov SA. Effect of the gamma-aminobutyric acid antagonist disulfotetraazaadamantane on the evoked responses of neurons in hippocampal slices. Neirofiziologiia. 1989;21(1):66–70. [PubMed] [Google Scholar]
- Pirker S, Schwarzer C, Wieselthaler A, Sieghart W, Sperk G. GABA(A) receptors: immunocytochemical distribution of 13 subunits in the adult rat brain. Neuroscience. 2000;101(4):815–850. doi: 10.1016/S0306-4522(00)00442-5. [DOI] [PubMed] [Google Scholar]
- Ratra GS, Kamita SG, Casida JE. Role of human GABA(A) receptor beta3 subunit in insecticide toxicity. Toxicol Appl Pharmacol. 2001;172(3):233–240. doi: 10.1006/taap.2001.9154. [DOI] [PubMed] [Google Scholar]
- Rudolph U, Knoflach F. Beyond classical benzodiazepines: novel therapeutic potential of GABAA receptor subtypes. Nat Rev Drug Discov. 2011;10(9):685–697. doi: 10.1038/nrd3502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudolph U, Mohler H. Analysis of GABAA receptor function and dissection of the pharmacology of benzodiazepines and general anesthetics through mouse genetics. Annu Rev Pharmacol Toxicol. 2004;44:475–498. doi: 10.1146/annurev.pharmtox.44.101802.121429. [DOI] [PubMed] [Google Scholar]
- Shandra AA, Mazarati AM, Godlevsky LS, Vastyanov RS. Chemical kindling: implications for antiepileptic drugs—sensitive and resistant epilepsy models. Epilepsia. 1996;37(3):269–274. doi: 10.1111/j.1528-1157.1996.tb00024.x. [DOI] [PubMed] [Google Scholar]
- Slater SN, Wilson AT. Relationship between picrotin and picrotoxinin. Nature. 1951;167(4243):324–325. doi: 10.1038/167324a0. [DOI] [PubMed] [Google Scholar]
- Squires RF, Casida JE, Richardson M, Saederup E. [35S]t-butylbicyclophosphorothionate binds with high affinity to brain-specific sites coupled to gamma-aminobutyric acid-A and ion recognition sites. Mol Pharmacol. 1983;23(2):326–336. [PubMed] [Google Scholar]
- Sur C, Wafford KA, Reynolds DS, Hadingham KL, Bromidge F, Macaulay A, Collinson N, O’Meara G, Howell O, Newman R, Myers J, Atack JR, Dawson GR, McKernan RM, Whiting PJ, Rosahl TW. Loss of the major GABA(A) receptor subtype in the brain is not lethal in mice. J Neurosci. 2001;21(10):3409–3418. doi: 10.1523/JNEUROSCI.21-10-03409.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasylieva N, Barnych B, Rand A, Inceoglu B, Gee SJ, Hammock BD. Sensitive immunoassay for detection and quantification of the neurotoxin, tetramethylenedisulfotetramine. Anal Chem. 2017;89(10):5612–5619. doi: 10.1021/acs.analchem.7b00846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitlow KS, Belson M, Barrueto F, Nelson L, Henderson AK. Tetramethylenedisulfotetramine: old agent and new terror. Ann Emerg Med. 2005;45(6):609–613. doi: 10.1016/j.annemergmed.2004.09.009. [DOI] [PubMed] [Google Scholar]
- Wood FC, Battye AE. The condensation of sulphamide, dimethylsulphamide, and aniline-p-sulphonamide with formaldehyde. J Soc Chem Ind. 1933;56:346–349. [Google Scholar]
- Zhang Y, Su M, Tian DP. Tetramine poisoning: a case report and review of the literature. Forensic Sci Int. 2011;204(1–3):e24–e27. doi: 10.1016/j.forsciint.2010.06.025. [DOI] [PubMed] [Google Scholar]
- Zhao C, Hwang SH, Buchholz BA, Carpenter TS, Lightstone FC, Yang J, Hammock BD, Casida JE. GABAA receptor target of tetramethylenedisulfotetramine. Proc Natl Acad Sci USA. 2014;111(23):8607–8612. doi: 10.1073/pnas.1407379111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zolkowska D, Banks CN, Dhir A, Inceoglu B, Sanborn JR, McCoy MR, Bruun DA, Hammock BD, Lein PJ, Rogawski MA. Characterization of seizures induced by acute and repeated exposure to tetramethylenedisulfotetramine. J Pharmacol Exp Ther. 2012;341(2):435–446. doi: 10.1124/jpet.111.190579. [DOI] [PMC free article] [PubMed] [Google Scholar]