Summary
Objectives
To estimate the differences between individuals with and without obesity on healthcare resource utilization using two large electronic medical record databases.
Methods
Data from the UK Clinical Practice Research Datalink and US General Electric Centricity database of adults (≥18 years) with registration date before 01/01/2010. Differences between individuals with and without obesity on 5‐year rates of Primary Care Physician (PCP) contacts, prescriptions and hospitalizations were analysed.
Results
The study contained 1,878,017 UK and 4,414,883 US individuals. Compared with body mass index (BMI) (18.5–24.9 kg m−2), significant (p < 0.0001) increases in healthcare usage were observed with increasing BMI. Individuals with BMI 30–34.9 kg m−2 had higher PCP contact rate (rate ratios [RR] 1.27 and 1.28 for UK and USA, respectively), higher prescription rate (RR 1.61 and 1.51) and higher hospitalization rate (RR 1.10 and 1.13) than individuals with BMI 18.5–24.9 kg m−2. Individuals with BMI >40 kg m−2 also had higher PCP contact rate (RR 1.56 and 1.64), prescription rate (RR 2.48 and 2.14) and hospitalization rate (RR 1.27 and 1.30) than individuals with BMI 18.5–24.9 kg m−2.
Conclusions
The utilization of healthcare resources is significantly higher in individuals with obesity. A similar trend was observed in both the UK and US cohorts.
Keywords: Database study, Obesity, Public health
Introduction
A positive association between body mass index (BMI) and healthcare utilization has frequently been observed, particularly with increasing physical disability or chronic diseases such as type 2 diabetes (associated with increased BMI). A retrospective cohort study of the Humana Medicare Advantage (MA) claims data in America showed that a higher BMI category was associated with higher healthcare, medical and pharmacy total costs 1 and similar results were seen in an Australian database study 2. A recent meta‐analysis also showed a corresponding increase in healthcare costs for class I, II and III obesity 3.
Previous studies, however, often focus on a single country or are based on relatively small samples from insurance claims data 4, 5, 6. The use of new ‘big data’ technologies to perform advanced analytics on very large datasets has allowed researchers to gain insights into the behavior of real‐world populations that were previously time‐consuming, costly or infeasible 7.
The aim of this study is to analyse the impact of increasing BMI on healthcare utilization (hospitalizations, PCP contacts and prescriptions) using large population‐based electronic medical record (EMR) data from both the UK and the USA. This study is one of the first that combines EMR databases from both the UK and the USA, analysing both intra‐country and inter‐country differences in the impact of increasing BMI on healthcare utilization.
Methods
Data sources
This is an observational cohort study using data from two different EMR databases. The UK database, Clinical Practice Research Datalink (CPRD), is an EMR service administered by the Medicine and Healthcare Products Regulatory Agency and the National Health Service and contains information on more than 11 million patients (~17% of the UK population). The CPRD includes information on general practitioner (GP) contacts, prescriptions, laboratory tests and demographic and anthropometric measurements. It also contains data on admissions, discharge and inpatient procedures via linkage to Hospital Episodes Statistics. The CPRD is considered representative of the general population of the UK 8.
The US General Electric (GE) Centricity database for US physician practices contains information on more than 40 million patients (~12.5% of the US population). It captures a large variety of data such as basic patient demographics, primary care physician (PCP) contacts, specialist care, laboratory tests, anthropometric measurements, hospitalizations and prescriptions. The database covers all US states and different payment/insurance types to ensure that it is a representative of the population as a whole.
For this study, a separate cohort was created for each of the two databases (CPRD and GE) consisting of individuals with a current registration date before 01/01/2010. Each patient was followed from an individual baseline (latest date of BMI measurement 01/01/2008–01/01/2010) until end of follow‐up; defined as either the date of death, transfer out date (the date the patient leaves the system) or 30/09/2014. Inclusion criteria were individuals with acceptable data (defined by the individual database's standards) with a recorded BMI within the relevant time period and aged 18 or older. Individuals with BMI <18.5 kg m−2 or >70 kg m−2 were excluded, as a range of acceptable data is required for each variable for data cleaning purposes. Analyses were performed on the IBM BigInsights Platform using their version of the open source R (BigR) version 3.1.3 statistical computing.
Analysis
The objective of the study was to explore the relationship between BMI and healthcare resource utilization defined in three different ways:
Hospitalizations: total number of hospital admissions within the predefined time period. Mean values and individual rates (number of admissions divided by individual follow‐up time) were calculated. For CPRD, only the subpopulation with linkage to Hospital Episodes Statistics was included for this outcome (around half of the population).
PCP contacts: total number of PCP (in the USA) or GP (in the UK) contacts within the predefined time period. Mean values and individual rates (number of GP‐contacts divided by individual follow‐up time) were calculated.
Prescriptions: total number of prescriptions within the predefined time period. Mean values and individual rates (number of prescriptions divided by individual follow‐up time) were calculated.
Mean values for each healthcare resource outcome were calculated for individuals with healthy weight (BMI 18.5–<25 kg m−2), overweight (BMI 25–<30 kg m−2), class I obesity (BMI 30–<35 kg m−2), class II obesity (BMI 35–<40 kg m−2) and class III obesity (BMI 40–70 kg m−2). As the nature of the data and the underlying data infrastructure are different for each database, RR were calculated for each category to enable comparison between the databases, with healthy weight used as the reference point. The difference between individuals with obesity (BMI ≥30 kg m−2) and individuals without obesity (BMI 18.5–<30 kg m−2) in 5‐year rates of hospitalizations, PCP or GP contacts, and prescriptions were also calculated. All analyses used a Zero Inflated Poisson Regression model adjusted for sex and age. Complete case analyses were performed, with no imputation methods applied.
Results
Of the 15,639,136 UK individuals in the CPRD database, 5,564,918 had database‐determined acceptable data from the relevant time period; 4,441,041 were aged over 18, 1,923,100 had an available BMI and 1,878,017 fulfilled all inclusion/exclusion criteria to be included in the final analysis. Of the 40,096,604 US individuals in the GE Centricity database, 10,053,089 had database‐determined acceptable data from the relevant time period; 8,183,181 were aged over 18, 4,476,287 had an available BMI measurement (based on height and weight measured and reported by the healthcare providers) and 4,414,883 fulfilled all inclusion/exclusion criteria to be included in the final analysis. Baseline characteristics are shown in Table 1.
Table 1.
Baseline characteristics of eligible individuals from the UK CPRD cohort and the US GE Centricity cohort by BMI category.
| UK BMI (kg m−2) | US BMI (kg m−2) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Normal weight 18.5–<25 | Overweight 25–<30 | Class I Obesity 30–<35 | Class II Obesity 35–<40 | Class III Obesity 40–70 | Normal weight 18.5–<25 | Overweight 25–<30 | Class I Obesity 30–<35 | Class II Obesity 35–<40 | Class III Obesity 40–70 | |
| n (%) | 690,704 (36.8) | 656,219 (34.9) | 335,828 (17.9) | 127,675 (6.8) | 67,591 (3.6) | 1,239,819 (28.1) | 1,437,269 (32.6) | 929,329 (21.0) | 451,941 (10.2) | 356,525 (8.1) |
| Female, % | 65.3 | 50.6 | 53.6 | 62.6 | 70.9 | 72.9 | 54.2 | 54.8 | 62.5 | 70.5 |
| Start age, years | 47.5 | 53.3 | 53.5 | 51.4 | 49.0 | 43.8 | 48.5 | 49.2 | 48.2 | 46.7 |
| Mean BMI, kg m−2 | 22.3 | 27.3 | 32.1 | 37.0 | 44.6 | 22.5 | 27.4 | 32.2 | 37.2 | 45.8 |
| Mean study length, days | 1,746 | 1,871 | 1,881 | 1,869 | 1,843 | 1,509 | 1,563 | 1,583 | 1,584 | 1,565 |
Data are observed means or n numbers. BMI, body mass index.
A trend between increasing BMI and healthcare use was seen in both cohorts (Table 2).
Table 2.
Healthcare utilization in the UK from the CPRD cohort and the US from the GE centricity cohort, by BMI category.
| UK BMI (kg m−2) | US BMI (kg m−2) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Normal weight 18.5–<25 | Overweight 25–<30 | Class I Obesity 30–<35 | Class II Obesity 35–<40 | Class III Obesity 40–70 | Normal weight 18.5–<25 | Overweight 25–<30 | Class I Obesity 30–<35 | Class II Obesity 35–<40 | Class III Obesity 40–70 | |
| Prescriptions | 100.3 | 144.1 | 180.6 | 203.8 | 231.2 | 51.7 | 70.1 | 90.1 | 106.5 | 122.9 |
| Prescriptions per year | 23.7 | 30.2 | 37.2 | 41.9 | 48.2 | 18.3 | 21.2 | 25.0 | 28.3 | 32.0 |
| GP/PCP contacts | 78.3 | 97.5 | 112.2 | 121.1 | 130.7 | 35.1 | 44.9 | 53.7 | 60.4 | 66.7 |
| GP/PCP contacts per year | 18.2 | 20.3 | 23.0 | 24.5 | 26.8 | 17.3 | 17.0 | 17.5 | 18.0 | 18.9 |
| Hospital admissions | 1.51* | 1.76* | 1.91* | 2.04* | 2.22* | 0.06 | 0.07 | 0.09 | 0.10 | 0.11 |
| Hospital admissions per year | 0.39* | 0.40* | 0.42* | 0.44* | 0.50* | 0.01 | 0.02 | 0.02 | 0.02 | 0.02 |
Data are observed means. GP, general practitioner; PCP, primary care physician.
Only calculated within the 2,693,267 individuals of the CPRD eligible for linkage with Hospital Episodes Statistics.
Compared with individuals with healthy weight, statistically significant (all p < 0.0001) increases in PCP contacts, prescriptions and hospitalizations were observed with higher BMI after controlling for sex and age (Figure 1a,b). Individuals with class I obesity (BMI 30–<35 kg m−2) had higher prescription rates (RR 1.61 and 1.51 for the UK and USA, respectively), PCP contact rates (RR 1.27 and 1.28, respectively) and hospitalization rates (RR 1.10 and 1.13, respectively) than for healthy weight individuals. Similarly, individuals with class II (BMI 35–<40 kg m−2) and class III obesity (BMI 40–70 kg m−2) had higher prescription rates (class II RR 1.95 and 1.78; class III RR 2.48 and 2.14, for the UK and USA, respectively), PCP contact rates (class II RR 1.39 and 1.43; class III RR 1.56 and 1.64, respectively) and hospitalization rates (class II RR 1.18 and 1.16; class III RR 1.27 and 1.30, respectively) than healthy weight individuals.
Figure 1.
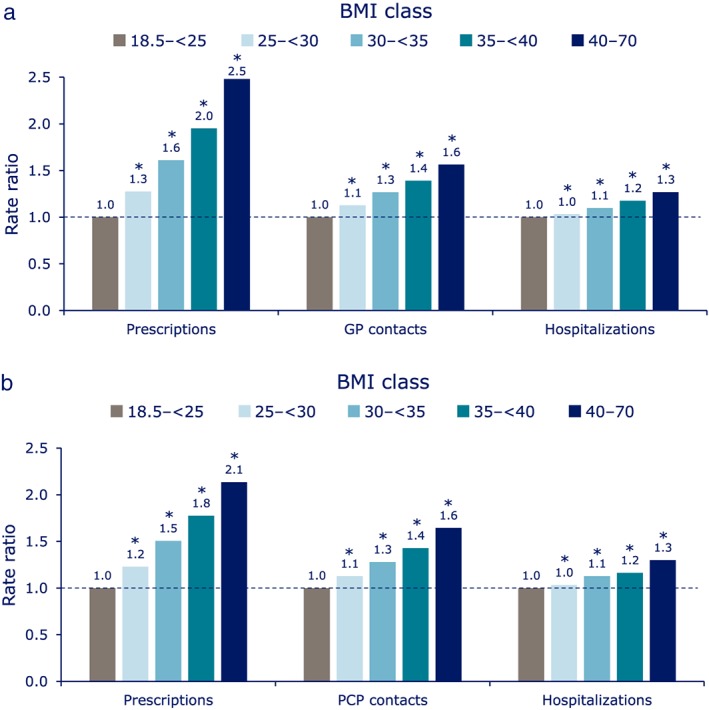
(a) Rate of healthcare resource utilization from the UK CPRD cohort. (b) Rate of healthcare resource utilization from the US GE Centricity cohort. Data are rate ratios estimated using a Zero Inflated Poisson Regression model adjusted for sex and age. Reference category is the 18.5–<25 BMI class. BMI, body mass index; CPRD, Clinical Practice Research Datalink; GE, General Electric; GP, general practitioner; PCP, primary care physician
The study examined the relationship between BMI and healthcare resource utilization and found a linear positive relationship. Each single‐point increment in BMI over the reference range (18.5–<25 kg m−2) was associated with a mean increase in the rate ratio for prescriptions, PCP contacts and hospitalizations over a 5‐year period of 4.2% (p < 0.0001), 2.1% (p < 0.0001) and 0.9% (p < 0.0001), respectively, in the UK cohort; and 3.1% (p < 0.0001), 2.1% (p < 0.0001) and 1.1% (p < 0.0001), respectively, in the US cohort.
Compared with individuals without obesity (BMI 18.5–<30 kg m−2), individuals with obesity (BMI ≥30–70 kg m−2) had higher mean rates of prescriptions, PCP contacts and hospitalizations of 61% (p < 0.0001), 27% (p < 0.0001) and 21% (p < 0.0001), respectively, in the UK; and 55% (p < 0.0001), 32% (p < 0.0001) and 16% (p < 0.0001), respectively, in the USA.
Discussion
The study observed increased healthcare resource utilization in individuals with higher BMIs compared with individuals of healthy BMI, after adjusting for sex and age, in a large representative sample of UK and US individuals. Despite the differences in healthcare systems and patient population, the same trend was identified in both the UK and US cohorts with rate ratio estimates of similar directions and magnitude.
A difference was observed in the actual numbers of individuals using healthcare resources, which were much higher in the UK compared with the USA. It is most likely that these observed differences between the UK and USA are rooted in the different structures of the underlying databases and healthcare differences between countries. For example, prescriptions in the USA are often longer than the UK, which would alter the number of prescriptions given. Furthermore, in the UK, specialist referral is via the GP and therefore captured in the CPRD, while in the US patients can refer themselves to specialists outside of the GE database. This study does not conclude the setting or country in which obesity is associated with the highest increase in healthcare resource utilization.
Clinical implications and future research directions
The findings of this study concur with data from other international database studies, in showing BMI weight categories experience increasing healthcare utilization compared with BMI 18.5–24.9 kg m−2. This suggests that there is a real need to increase the availability and effectiveness of current obesity treatments in order to drive down the current increase in healthcare utilization, with bariatric surgery currently recommended for individuals with BMI ≥40 kg m−2 and pharmacotherapy for individuals with BMI ≥30 kg m−2 or ≥27 kg m−2 with comorbidities such as hypertension and dyslipidemia. Further explorations of how increasing BMI affects the cost of healthcare within these databases would provide even more valuable information to aid discussions of healthcare delivery in the treatment of obesity. It might also be interesting to analyse the trend using ‘big data’ for other countries to ascertain the global impact associated with obesity.
Study limitations
As this study is based on electronic data from the CPRD and GE Centricity databases, the results should be interpreted in the light of the limitations typical to these types of datasets and analyses. Of note, socio‐economic status could not be controlled for because of the nature of the data available in the databases. The difference between the databases also does not allow for comparisons between the absolute number of patients utilizing UK and US healthcare. Many individuals, in both databases, were also missing BMI values or did not have data from the relevant time period that fell within the database standards of ‘acceptable data’. While there do not seem to be any biases that would make these samples non‐representative, they nevertheless represent a subset of the full UK and US databases.
Conclusions
In the UK and US, the number of pharmaceutical prescriptions, primary care physician contacts and hospital admissions increase consistently with higher BMI categories. This is the first time that these associations have been described in two large EMR datasets utilizing identical methods. The results illuminate striking consistency in the impact of obesity on healthcare utilization across two very different healthcare systems.
Clinical trial registration
N/A (this is not a clinical trial and not registered anywhere).
Declarations
EN, BC and AB are all employees of Novo Nordisk A/S. EN and BC are shareholders of Novo Nordisk A/S..
Medical writing assistance was provided by Shuna Gould, and editing and submission support was provided by Grant Womack, both of Watermeadow Medical, an Ashfield Company. This was funded by Novo Nordisk A/S.
Funding
The development of this article was funded by Novo Nordisk A/S.
Conflict of Interest Statement
No conflict of interest was declared.
Nørtoft, E. , Chubb, B. , and Borglykke, A. (2018) Obesity and healthcare resource utilization: comparative results from the UK and the USA. Obesity Science & Practice, 4: 41–45. doi: 10.1002/osp4.148.
References
- 1. Suehs BT, Kamble P, Huang J, et al. Association of obesity with healthcare utilization and costs in a Medicare population. Current Medical Research and Opinion 2017: 1–8. [DOI] [PubMed] [Google Scholar]
- 2. Korda RJ, Joshy G, Paige E, et al. The relationship between body mass index and hospitalisation rates, days in hospital and costs: findings from a large prospective linked data study. PLoS One 2015; 10: e0118599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kent S, Fusco F, Gray A, Jebb SA, Cairns BJ, Mihaylova B. Body mass index and healthcare costs: a systematic literature review of individual participant data studies. Obesity Reviews 2017; 18: 869–879. [DOI] [PubMed] [Google Scholar]
- 4. Buchmueller TC, Johar M. Obesity and health expenditures: evidence from Australia. Economics and Human Biology 2015; 17: 42–58. [DOI] [PubMed] [Google Scholar]
- 5. Peterson MD, Mahmoudi E. Healthcare utilization associated with obesity and physical disabilities. American Journal of Preventive Medicine 2015; 48: 426–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Li Q, Blume SW, Huang JC, Hammer M, Ganz ML. Prevalence and healthcare costs of obesity‐related comorbidities: evidence from an electronic medical records system in the United States. Journal of Medical Economics 2015; 18: 1020–1028. [DOI] [PubMed] [Google Scholar]
- 7. Cook JA, Collins GS. The rise of big clinical databases. The British Journal of Surgery 2015; 102: e93–e101. [DOI] [PubMed] [Google Scholar]
- 8. Herrett E, Gallagher AM, Bhaskaran K, et al. Data resource profile: clinical practice research datalink (CPRD). International Journal of Epidemiology 2015; 44: 827–836. [DOI] [PMC free article] [PubMed] [Google Scholar]


