Summary
Background
Experience suggests that some physicians view obesity as a purely lifestyle condition rather than a chronic metabolic disease. Physicians may not be aware of the role of biological factors in causing weight regain after an initial weight loss.
Methods
A questionnaire was administered at continuing medical education conferences, both primary care and obesity‐specific. The questionnaire included items about biological and behavioral factors that predispose to weight regain and general items about treatment of obesity. The sample was separated into primary care physicians (PCPs) and physicians preparing for the obesity medicine (OMs) exam.
Results
Among all respondents, behavioral factors were given higher importance ratings, relative to biological factors in causing weight regain. Respondents rated behaviour modification as more effective, relative to medications or surgery to treat obesity. OMs gave higher importance ratings to biological factors, relative to PCPs. OMs also gave higher effectiveness ratings for medications and surgery, relative to PCPs. However, even OMs gave higher effectiveness ratings for behaviour modification, relative to medications or surgery. Respondents who reported a belief in the role of behavioral factors rated lifestyle modification as more effective. Respondents who reported a belief in both behavioral and biological factors rated medications as more effective.
Conclusions
Physicians rate biological factors as less important, relative to behavioral factors in causing weight regain. Physicians rate medications and surgery as less effective, relative to lifestyle modification alone. Belief in the importance of behavioral factors correlated with a higher effectiveness rating for lifestyle modification. A better understanding of the biological basis for weight regain may help to increase comfort with the use of biological treatments for obesity.
Keywords: Knowledge/attitudes, obesity, physicians, primary care physicians
Background
The biological basis for weight regain has been documented in the medical literature for over 20 years 1, 2, 3, 4, 5. Factors contributing to weight regain include lower 24 h energy expenditure (‘adaptive thermogenesis’), increased levels of ghrelin (a hormone closely linked to hunger), as well as increased brain sensitivity to food cues, reduced levels of leptin (a hormone linked to feeling full) and increased cellularity of adipose tissue 4, 5, 6, 7. Recent research conducted with participants from ‘The Biggest Loser’ television show has demonstrated that metabolic adaptations to weight loss persist out to at least 6 years, even when the majority of weight is regained 8.
Despite the clinical burden of obesity in daily practice and multiple advances in the treatment of obesity since 2012 9, 10, 11, 12, 13, 14, primary care physicians (PCPs) do not consistently address obesity in office visits 15, 16, even when more sophisticated methods are used to search electronic records for evidence of counselling 17. Reasons cited for this include inadequate time, lack of formal training in weight management, a perceived lack of effective treatments and low confidence in patients' ability to change behaviour 18, 19, 20.
An additional barrier to weight loss counseling in primary care may be a lack of understanding of why patients struggle to maintain weight loss over the longer term. Experience teaching PCPs about the treatment of obesity suggests that some clinicians do not understand the biological complexity of weight management. Specifically, after hearing talks on obesity treatment that include the metabolic adaptations to weight loss, physicians report that they have not been taught about the biological drivers of weight regain that occur after an initial weight loss.
The primary aim of this study was to examine physician perspectives about the relative importance that biology and behaviour play in weight control. A secondary aim was to compare differences between PCPs and physicians who practice obesity medicine (OMs). It was hypothesized that OMs would have greater awareness of biological factors, relative to PCPs.
Methods
A brief questionnaire was developed to address five biological factors and two behavioral factors implicated in weight regain. No validated instrument exists to ask about these factors. Therefore, five of the major biological mechanisms implicated in weight regain were included 5. The questionnaire also asked about satisfaction in treating obesity and about the perceived effectiveness of behavioral, pharmacologic and surgical treatment of obesity. All items were on a scale of 0–10, with 0 listed as ‘least important’ and 10 listed as ‘most important’. The questionnaire is included in Figure 1. A summary score was created of the five biological factors and of the two behavioral factors.
Figure 1.
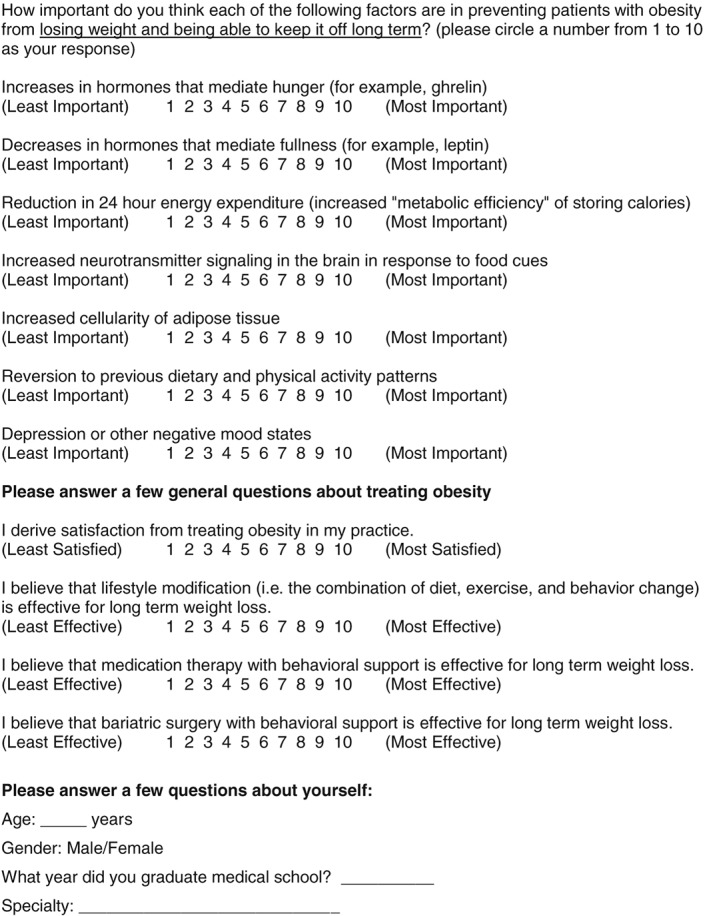
Questionnaire.
The questionnaire was administered at continuing medical education (CME) courses for physicians in which one of the authors (A. G. T., T. H. and W. T. D.) was a speaker. These included a Kaiser Permanente primary care CME course (n = 35) and a state‐level CME conference of the American College of Physicians (n = 126). The questionnaire was also given at 2 consecutive years of an OM course run by The Obesity Society (n = 111 total). Physicians who attend this course have a clinical practice in weight management and are preparing for the OMs board exam. The response rate was 63% across all conferences at which the questionnaire was given.
All data were de‐identified. No power calculation was performed, as the study was exploratory. Data were analysed by the first author using small Stata, version 12.1 (StataCorp LLC; College Station, TX, USA). Paired t‐tests were used to compare item scores and summary scores between PCPs and OMs. Within‐group t‐tests were used to compare scores within the same subgroup (e.g. to compare the summary score for biological factors and the summary score for behavioral factors within the OM group). Pairwise correlations were used to explore possible associations between the perceived importance of biological/behavioral factors and the perceived efficacy of treatment modalities. A p value of <0.05 was considered significant for all comparisons.
No financial support was received for the study. The study was considered exempt from full review by the Kaiser Permanente Colorado IRB (Protocol #CO‐14‐2156).
Results
Demographics are shown in Table 1. The average age of respondents was 47 ± 10.5 years. OMs were, on average, 3 years further out from their terminal degree, compared with PCPs, and 4.3 years older (p < 0.05 for both differences). Significantly, more OMs were female, compared with PCPs (56.1% vs. 46.8%, p < 0.05).
Table 1.
Respondent demographics
| Total (n = 272) | OMs (n = 161) | PCPs (n = 111) | |
|---|---|---|---|
| Age (years) | 47.1 ± 10.5 | a45.3 ± 9.8 | b49.6 ± 10.9 |
| Percent female | 52.3 | a56.1 | a46.8 |
| Years since degree | 19.6 ± 10.9 | a18.3 ± 9.7 | b21.3 ± 12.3 |
Superscripts with different letters are significantly different at p < 0.05. All values are mean ± standard deviation. OMs, obesity medicine; PCPs, primary care physicians.
Biological vs. behavioral factors
These results are shown in Table 2. Among all respondents, behavioral factors were given higher importance ratings, relative to biological factors in causing weight regain (8.27 ± 1.29 vs. 6.65 ± 1.38 on a 10‐point scale; p < 0.001 for difference). OMs and PCPs gave similar ratings for the importance of behavioral factors in causing weight regain. OMs rated two of five biological factors as more important, relative to PCPs, and gave a significantly higher rating on a summary measure of behavioral factors.
Table 2.
Ratings for biological and behavioral factors causing weight regain
| Total | OMs | PCPs | |
|---|---|---|---|
| Summary score for biological factors | 6.65 ± 1.38 | a6.81 ± 1.37 | b6.41 ± 1.35 |
| Summary score for behavioral factors | 8.27 ± 1.29 | a8.28 ± 1.33 | a8.27 ± 1.24 |
| Increased levels of ghrelin (hunger) | 6.72 ± 2.10 | a7.05 ± 2.07 | b6.24 ± 2.05 |
| Decreased levels of leptin (fullness) | 6.52 ± 2.16 | a6.52 ± 2.31 | a6.52 ± 1.93 |
| Reduced 24 h energy expenditure | 7.09 ± 2.19 | a7.15 ± 2.13 | a7.0 ± 2.28 |
| Increased sensitivity of brain to food cues | 6.98 ± 1.86 | a7.19 ± 1.83 | b6.68 ± 1.87 |
| Increased cellularity of adipose tissue | 6.05 ± 2.19 | a6.23 ± 2.19 | a5.79 ± 2.18 |
| Reversion to previous dietary habits | 8.63 ± 1.62 | a8.78 ± 1.57 | a8.41 ± 1.66 |
| Depression or other negative mood states | 7.92 ± 1.55 | a7.79 ± 1.57 | a8.12 ± 1.50 |
Superscripts with different letters are significantly different at p < 0.05. All values are mean ± standard deviation. OMs, obesity medicine; PCPs, primary care physicians.
Belief in efficacy of treatment modalities
These data are shown in Figure 2. Among all respondents, medications were rated as significantly less effective, relative to lifestyle modification alone or bariatric surgery (p < 0.001 for both comparisons). Surgery was rated as less effective, relative to lifestyle modification (p = 0.002 for comparison). OMs and PCPs gave similar ratings for the effectiveness of lifestyle modification. OMs gave higher ratings relative to PCPs for the effectiveness of medications and surgery to treat obesity.
Figure 2.
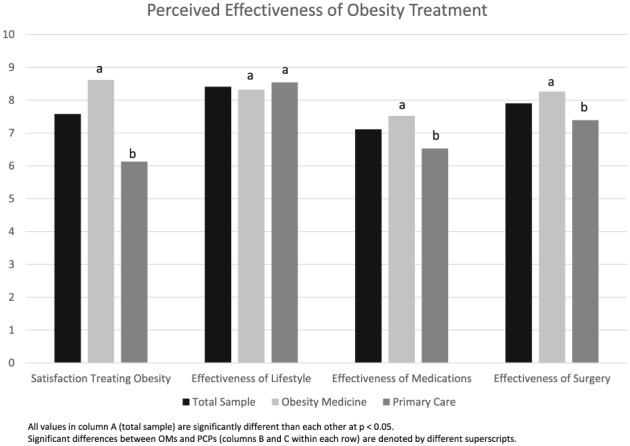
Perceived Effectiveness of Obesity Treatment Modalities.
Satisfaction in treating obesity
Average satisfaction with treating obesity was 8.62 ± 1.55 for OMs and 6.13 ± 2.34 for PCPs (p < 0.001 for difference).
Correlations
These data are shown in Table 3. Higher ratings for the importance of biological factors in weight regain were correlated with greater satisfaction in treating obesity. Higher ratings for biological factors also correlated with greater perceived efficacy of weight loss medications (but not weight loss surgery). Higher ratings for the importance of behavioral factors in causing weight regain correlated with greater perceived efficacy of behavioral treatment of obesity. Surprisingly, higher ratings for behavioral factors also correlated with greater perceived efficacy of weight loss medications.
Table 3.
Pairwise correlations between perceived efficacy of obesity treatment and belief in strength of biological and behavioral factors causing weight regain
| Summary score of biological factors | Summary score of behavioral factors | |
|---|---|---|
| Satisfaction in treating obesity | 0.22 (p = 0.0004) | 0.08 (p = 0.20) |
| Effectiveness of lifestyle modification | 0.08 (p = 0.20) | 0.31 (p < 0.0001) |
| Effectiveness of medications | 0.17 (p = 0.006) | 0.14 (p = 0.018) |
| Effectiveness of weight loss surgery | 0.06 (p = 0.29) | 0.02 (p = 0.70) |
Demographic factors
Female and male physicians gave similar ratings for the importance of biological factors. Female physicians gave a slightly higher rating, relative to male physicians, for the importance of behavioral factors. Years since medical school graduation was not associated with ratings for biological factors. Years since graduation was associated with lower ratings for behavioral factors, but the association did not reach statistical significance (p = 0.054). Age was not associated with ratings for biological or behavioral factors. In multivariable regression, no demographic variables were significantly associated with ratings for biological or behavioral factors.
Discussion
In this study, physicians gave a higher importance rating to behavioral factors than to biological factors in causing weight regain after an initial weight loss. OM physicians rated biological factors as more important, relative to PCPs, a finding that would be expected given that OMs are more likely to read the literature in this area. Whether behavioral or biological factors are the most important remains open to debate. A recent study suggests that, in addition to the decreases in energy expenditure that occur with weight loss, automatic increases in calorie intake accompany weight loss 21, strengthening the argument for the role of biological factors.
The most striking finding of this survey is that physicians rate weight loss medications and surgery as less effective, relative to lifestyle modification alone. This finding clearly contradicts the medical literature, which shows that weight loss medications and surgery produce additional and more durable weight loss compared with lifestyle modification alone. OMs gave higher effectiveness ratings for medications and surgery, relative to PCPs. However, even OMs gave lower ratings for medications, relative to lifestyle modification alone. Thus, both groups of physicians have incorrect impressions regarding the efficacy of treatment, highlighting the need for more physician education.
Respondents who expressed a greater belief in the role of behaviour were more likely to state that lifestyle modification is effective for treatment of obesity. Respondents who expressed a greater belief in the role of both behaviour and biology were more likely to state that medications are effective. Belief in the importance of behaviour or biological factors did not correlate with the perceived effectiveness of surgery. It is possible that once a physician accepts that biology plays an important role in weight regain, he or she then realizes that behaviour, while a critical component of long‐term success, is not a sustainable treatment on its own for many patients with obesity. In this context, the treatment modality, rather than the patient, becomes the limiting factor in long‐term maintenance of weight loss.
If the medical community is expected to treat obesity as a chronic disease, then physicians must understand both the behavioural and the biological underpinnings of managing weight on a chronic basis. A recent paper highlighted the need for better physician education on obesity. Specifically, in the United States Medical Licensing Exam (USMLE) step exams, very few items directly addressed obesity; rather, most items on obesity were in the context of weight‐related comorbidities 22. Physicians who better understand the biological challenge of achieving and maintaining weight loss might be more likely to effectively counsel patients on appropriate weight loss goals 7; patients who are more satisfied with their physician's weight loss counselling are likely to lose more weight 23. Physicians who better understand the biology also might be more open to using ‘biologic’ tools (medications and surgery) to help patients maintain their weight losses. Studies from the literature on depression support the idea that physicians who believe more in the biological causes of the condition are more likely to prescribe medication 24, 25. Physicians clearly recognize the role they have in encouraging weight loss as a means to improve health 26. Improved training into the biologic basis of weight regulation will further improve physicians' ability to treat obesity as a chronic disease. Physicians have been shown to demonstrate weight bias 27, 28; it is possible that improved education could mitigate this bias.
Limitations of this study include the convenience nature of the sample and the fact that this is a questionnaire and does reflect actual office practice or management of obesity. An additional limitation is the structure of the questionnaire, which did not allow us to directly compare responses among the items. Strengths of the study include the high response rate to the questionnaire, participation of physicians from several states and multiple practice settings, and the comparison between a general sample of PCPs and a sample of physicians preparing for the OM board exam.
In summary, this study found that (1) physicians gave higher importance ratings for behavioural factors relative to biological factors in causing weight regain and that (2) physicians (incorrectly) rated behaviour modification alone as more effective, relative to medications or surgery to treat obesity. Not surprisingly, OM physicians reported a greater awareness of biological factors and gave higher effectiveness ratings for medications and surgery, relative to a general sample of PCPs. The results of this study highlight the need for greater education of physicians in the management of obesity.
Conflict of Interest Statement
Dr. Kyle reports consulting fees from Novo Nordisk, Enteromedics and Nutrisystem.
Tsai, A. G. , Histon, T. , Kyle, T. K. , Rubenstein, N. , and Donahoo, W. T. (2018) Evidence of a gap in understanding obesity among physicians. Obesity Science & Practice, 4: 46–51. doi: 10.1002/osp4.146.
References
- 1. Leibel RL, Rosenbaum M, Hirsch J. Changes in energy expenditure resulting from altered body weight. N Engl J Med 1995; 332: 621–628. https://doi.org/10.1056/NEJM199503093321001. [DOI] [PubMed] [Google Scholar]
- 2. Sumithran P, Prendergast LA, Delbridge E, et al. Long‐term persistence of hormonal adaptations to weight loss. N Engl J Med 2011; 365: 1597–1604. https://doi.org/10.1056/NEJMoa1105816. [DOI] [PubMed] [Google Scholar]
- 3. Rosenbaum M, Hirsch J, Gallagher DA, Leibel RL. Long‐term persistence of adaptive thermogenesis in subjects who have maintained a reduced body weight. Am J Clin Nutr 2008; 88: 906–912. [DOI] [PubMed] [Google Scholar]
- 4. Sumithran P, Proietto J. The defence of body weight: physiological basis for weight regain after weight loss. Clin Sci 2013; 124: 231–241. https://doi.org/10.1042/CS20120223. [DOI] [PubMed] [Google Scholar]
- 5. Ochner CN, Barrios DM, Lee CD, Pi‐Sunyer FX. Biological mechanisms that promote weight regain following weight loss in obese humans. Physiol Behav 2013; 120: 106–113. https://doi.org/10.1016/j.physbeh.2013.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. MacLean PS, Wing RR, Davidson T, et al. NIH working group report: innovative research to improve maintenance of weight loss. Obesity 2015; 23: 7–15. https://doi.org/10.1002/oby.20967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ochner CN, Tsai AG, Kushner RF, Wadden TA. Treating obesity seriously: when recommendations for lifestyle change confront biological adaptations. Lancet Diabetes Endocrinol 2015; 3: 232–234. https://doi.org/10.1016/S2213‐8587(15)00009‐1. [DOI] [PubMed] [Google Scholar]
- 8. Fothergill E, Guo J, Howard L, et al. Persistent metabolic adaptation 6 years after ‘The Biggest Loser’ competition. Obesity 2016; 24: 1612–1619. https://doi.org/10.1002/oby.21538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tsai AG, Abbo ED, Ogden LG. The time burden of overweight and obesity in primary care. BMC Health Serv Res 2011; 11: 191 https://doi.org/10.1186/1472‐6963‐11‐191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wadden TA, Butryn ML, Hong PS, Tsai AG. Behavioral treatment of obesity in patients encountered in primary care settings: a systematic review. JAMA 2014; 312: 1779–1791. https://doi.org/10.1001/jama.2014.14173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. American Medical Association (2013). Business of the American Medical Association host of delegates 2013 annual meeting. Annotated reference committee reports. Reference Committee D. http://www.ama‐assn.org/ama/pub/news/news/2013/2013‐06‐18‐new‐ama‐policies‐annual‐meeting.page. Accessed on July 15, 2014.
- 12. Centers for Medicare & Medicaid Services (2011). Decision memo for intensive behavioral therapy for obesity (CAG‐00423N). Available at http://http%3A%2F%2Fwww.cms.gov%2Fmedicare-coverage-database%2Fdetails%2Fnca-decision-memo.aspx%3F%26amp%3BNcaName%3DIntensive%20Behavioral%20Therapy%20forObesity&bc=ACAAAAAAIAAA&NCAId=253&. Accessed on December 14, 2013.
- 13. Khera R, Murad MH, Chandar AK, et al. Association of pharmacological treatments for obesity with weight loss and adverse events: a systematic review and meta‐analysis. JAMA 2016; 315: 2424–2434. https://doi.org/10.1001/jama.2016.7602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chang SH, Stoll CR, Song J, et al. The effectiveness and risks of bariatric surgery. JAMA Surg 2014; 149: 275–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jackson JE, Doescher MP, Saver BG, Hart LG. Trends in professional advice to lose weight among obese adults, 1994 to 2000. J Gen Intern Med 2005; 20: 814–818. https://doi.org/10.1111/j.1525‐1497.2005.0172.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Stafford RS, Farhat JH, Misra B, Schoenfeld DA. National patterns of physician activities related to obesity management. Arch Fam Med 2000; 9: 631–638. https://doi.org/10.1001/archfami.9.7.631. [DOI] [PubMed] [Google Scholar]
- 17. Hazlehurst BL, Lawrence JM, Donahoo WT, et al. Automating assessment of lifestyle counseling in electronic health records. Am J Prev Med 2014; 46: 457–464. https://doi.org/10.1016/j.amepre.2014.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kushner RF. Barriers to providing nutrition counseling by physicians: a survey of primary care practitioners. Prev Med 1995; 24: 546–552. https://doi.org/10.1006/pmed.1995.1087. [DOI] [PubMed] [Google Scholar]
- 19. Leverence RR, Williams RL, Sussman A. Crabtree BF; RIOS Net Clinicians. Obesity counseling and guidelines in primary care: a qualitative study. Am J Prev Med 2007; 32: 334–339. [DOI] [PubMed] [Google Scholar]
- 20. Huang J, Yu H, Marin E, Brock S, Carden D, Davis T. Physicians' weight loss counseling in two public hospital primary care clinics. Acad Med 2004. Feb; 79: 156–161. [DOI] [PubMed] [Google Scholar]
- 21. Polidori D, Sanghvi A, Seeley RJ, Hall KD. How strongly does appetite counter weight loss? Quantification of the feedback control of human energy intake. Obesity 2016; 24: 2289–2295. https://doi.org/10.1002/oby.21653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kushner RF, Butsch WS, Kahan S, Machineni S, Cook S, Aronne LJ. Obesity coverage on medical licensing examinations in the United States. What is being tested? Teach Learn Med 2016: 1–6. https://doi.org/10.1080/10401334.2016.1250641. [DOI] [PubMed] [Google Scholar]
- 23. Bennett WL, Wang NY, Gudzune KA, et al. Satisfaction with primary care provider involvement is associated with greater weight loss: results from the practice‐based POWER trial. Patient Educ Couns 2015; 98: 1099–1105. https://doi.org/10.1016/j.pec.2015.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ross S, Moffat K, McConnachie A, Gordon J, Wilson P. Sex and attitude: a randomized vignette study of the management of depression by general practitioners. Br J Gen Pract 1999; 49: 17–21. [PMC free article] [PubMed] [Google Scholar]
- 25. Liu SI, Lu RB, Lee MB. Non‐psychiatric physicians' knowledge, attitudes and behavior toward depression. J Formos Med Assoc 2008; 107: 921–931. [DOI] [PubMed] [Google Scholar]
- 26. Bennett WL, Gudzune KA, Appel LJ, Clark JM. Insights from the POWER practice‐based weight loss trial: a focus group study on the PCP's role in weight management. J Gen Intern Med 2014; 29: 50–58. https://doi.org/10.1007/s11606‐013‐2562‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hebl MR, Xu J. Weighing the care: physicians' reactions to the size of a patient. Int J Obes Relat Metab Disord 2001; 25: 1246–1252. [DOI] [PubMed] [Google Scholar]
- 28. Huizinga MM, Cooper LA, Bleich SN, Clark JM, Beach MC. Physician respect for patients with obesity. J Gen Intern Med 2009; 24: 1236–1239. https://doi.org/10.1007/s11606‐009‐1104‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]


