Abstract
Antecollis is considered to be relatively rare in Parkinson's disease (PD). Few cases of dopamine agonist-induce antecollis in PD have been reported. We described literature review of 12 PD patients including our 2 cases with pramipexole (PPX)-induced antecollis. The patients were predominantly Japanese, women and above 3 of Hoehn and Yahr stage. PPX-induced antecollis in PD was considered a type of dystonia of flexor neck muscle, and was improved soon after cessation or reduction of PPX. Our two cases improved their antecollis by overnight changing from PPX to ropinirole without deteriorating motor functions. Overnight switching of DA was considered useful as one option in the treatment of antecollis.
Keywords: Parkinson's disease, Drop head, Dopamine agonist, Therapy, Pramipexole, Ropinirole
Highlights
-
•
We described literature review of 12 PD patients including our 2 cases with pramipexole (PPX)-induced antecollis.
-
•
The patients were predominantly Japanese, women and above 3 of Hoehn and Yahr stage.
-
•
To treatment of the antecollis, PPX were stopped in 10 patients or reduced in 2 patients.
-
•
Our two cases improved their antecollis by overnight changing from PPX to ropinirole without deteriorating motor functions.
-
•
Overnight switching of DA was considered useful as one option in the treatment of antecollis.
1. Introduction
Patients with Parkinson's disease (PD) often present with abnormal posture, such as camptocormia, antecollis, Pisa syndrome, and scoliosis [1]. Antecollis refers to forward flexion of the head and neck [2], [3]. It was first reported in patients with multiple system atrophy (MSA), and has been suggested as a useful clue for the diagnosis of multiple MSA [3]. Antecollis is considered to be relatively rare in PD, and its prevalence is as 5–6% in PD [1], [2], [4], [5], [6]. Reports of antecollis in PD have originated from Japan more frequently than from elsewhere [1], [4], [5], [6], [7], [8], [9], [10], [11], [12]. The pathophysiology of antecollis in PD is unclear, but various different central mechanisms (dystonia, rigidity, proprioceptive disintegration) and peripheral processes (myopathy, skeletal and soft-tissue changes) have been proposed [1]. Dopamine agonists (DA) are known to induce or aggravate antecollis in PD [1], [4], [5], [6], [7], [8], [9], [10], [11], [13], and it was found in 0.8% [4]. In addition, there were rare reports that amantadine and donepezil hydrochloride caused antecollis in Japanese patients with PD [12], [14]. Here, we describe the literature review of 12 PD patients including our 2 cases with pramipexole (PPX)-induced antecollis.
2. Present the two cases
Case 1 involved a 64-year-old woman with PD who had developed resting tremor and mild postural tremor of the right hand at 57 years old. At that time, marked orthostatic hypotension and dysuria were not observed, and her brain MRI was normal without abnormal signals of the putamen and the pons. The patient had started to take immediate-release pramipexole (PPX-IR) at 1.5 mg/day. After 2 years, resting tremors had expanded to all extremities, postural tremor appeared on both upper hands, and daily medication was PPX-IR 3 mg and levodopa/carbidopa 300 mg. At 62 years old, entacapone 300 mg and zonisamide 2.5 mg had been added because of wearing-off phenomenon. Antecollis appeared at 63 years old, and gradually worsened. Although PPX-IR had been decreased to 1.5 mg, no improvement in antecollis was seen. The patient complained of neck pain at 64 years old. Laboratory tests, including muscle enzymes, were normal. Needle electromyogram did not show myopathic pattern in the neck extensor muscles, but tonic muscle discharges during passive head up in the sternocleidomastoid muscles (SCM). We injected a total of 40 units botulinum A toxin to bilateral SCM. Injections relieved neck pain, but antecollis remained unchanged. We then changed her medication overnight from 1.5 mg PPX-IR to 6 mg of immediate-release ropinirole (ROP-IR). After 1 month, she was able to lift her head smoothly without deterioration of motor function (Fig. 1A, Video A and B).
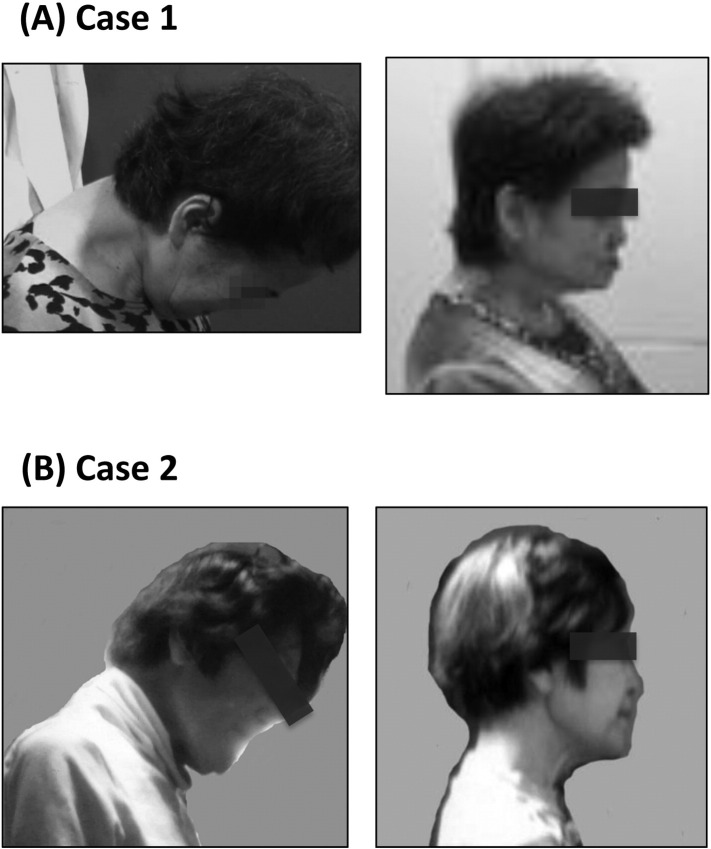
Fig. 1.
A) Case 1 shows marked antecollis during PRX-IR 1.5 mg, levodopa/carbidopa 300 mg, entacapone 300 mg and zonisamide 2.5 mg (left). One month after overnight switching from 1.5 mg PPX-IR to 6 mg ROP-IR (right).
B) Case 2 shows antecollis while taking PRX-IR 1.5 mg and levodopa/carbidopa 300 mg (left). Two weeks after overnight switching from 1.5 mg PPX-IR to 6 mg ROP-IR, antecollis has improved (right).
Case 2 involved a 71-year-old woman with PD who had developed mild resting tremor and postural tremor, cogwheel rigidity of the right hand, and mild orthostatic hypotension at 68 years old. There was not any abnormal signal in her brain MRI. Her motor symptoms were improved by taking PPX-IR 1.5 mg. Two years later, at Hoehn and Yahr stage II, levodopa/carbidopa had been added at 300 mg. The patient experienced neck pain during exercise, and antecollis appeared shortly thereafter, at 71 years old. Muscle tonus of the bilateral SCM increased. Laboratory tests including serum creatine kinase were normal. She was switched overnight from 1.5 mg PPX-IR to 6 mg ROP-IR. By 2 weeks later, she was able to lift her head smoothly (Fig. 1B). The improvements of their drop head were continuing after one year. Both patients did not undergo physiotherapy during one month after changing DA.
3. Literature review
Twelve PD patients with PPX-induced antecollis including two our patients were summarized in Table 1 [6], [7], [8], [9], [10], [12]. All patents were reported from Asia (11 patients were Japanese and 1 was Korean). Ten patients (2 patients of gender has not been described) were women. Hoehn and Yahr stage was above 3 in 7 patients of the described 8 patients. The disease durations were 3 to 17 years. Daily doses of PPX were from 1 to 3 mg. There were two types of intervals starting from PPX to the appearance of antecollis; the short interval of few weeks in 9 patients and the long interval of 2 to 4 years in 3 patients. To the treatment of the antecollis, PPX were stopped in 10 patients or reduced in 2 patients. Our cases were switched from pramipexole to ropinirole. The antecollis in all patients were improved in 1 to 4 weeks after cessation or reduction of PPX.
Table 1.
Antecollis induced by pramipexole in patients with Parkinson's disease.
| Authors | Age (year)/sex | HY stage | Duration (year) | PPX dosed (mg/d) | Interval from starting PPX to appearance of antecollis | Treatment | Combined drugs/d |
|---|---|---|---|---|---|---|---|
| Suzuki et al. 8) | 80/F | 4 | 3 | 3 | Few weeks | Cessation of PPX | l-dopa/carbidopa 200 mg |
| Oyama et al. 9) | 75/F | 3 | 6 | UD | 8 weeks | Reduction | UD |
| 64/F | 3 | 9 | UD | 4 weeks | Reduction of PPX | UD | |
| 79/F | 3 | 17 | UD | 4 weeks | Cessation of PPX | UD | |
| Taguchi et al. 10) | 80/F | UD | 3 | 1 | 1.5 years | Cessation of PPX Increase dose of l-dopa |
none |
| Uzawa et al. 11) | 64/F | 4 | 6 | 2.5 | Few weeks | Cessation of PPX | l-dopa/benserazid 450 mg |
| 47/F | 4 | 5 | 1 | 2 weeks | Cessation of PPX |
l-dopa/carbidopa 50 mg, Cabergoline 3 mg |
|
| Kashihara et al. 6) | UD | UD | UD | UD | Few weeks | Cessation of PPX | UD |
| UD | UD | UD | UD | Few weeks | Cessation of PPX | UD | |
| Kim et al. 13) | 80/F | UD | 3 | 1 | 6 weeks | Cessation of PPX | l-dopa/benserazid 450 mg |
| Our patient 1 | 64/F | 3 | 7 | 3 | 4 years | Reduction of PPX 1.5 mg, and Overnight switched from PPX to ROP 6 mg |
l-dopa/carbidopa 300 mg, Entacapone 300 mg, Zonisamide 2.5 mg |
| patient 2 | 71/F | 2 | 4 | 1.5 | 3 years | Overnight switched from PPX to ROP 6 mg | l-dopa/carbidopa 300 mg, |
HY stage; Hoehn and Yahr stage, UD; undescribed, PPX; pramipexole, ROP; ropinirole.
4. Discussion
We describe the literature review of 12 PD patients with PPX-induced antecollis. The patients were predominantly Japanese, women and above 3 of Hoehn and Yahr stage. PPX-induced antecollis was considered dystonia, rather than myopathy, based on their disproportionate tonus of the neck muscles, laboratory data, and EMG findings. Kashihara et al. [6] reported that the frequency of antecollis in PD was 0% at Hoehn and Yahr 1, 1.4% at 2, 4.7% at 3, and 9.1% at 4. Thus the incidence of antecollis increases as the disease progress. Regarding to the gender differences of deformities in PD, female are predominant in antecollis [6], [7], [9], [11] and in anterior flexion of the trunk [6], however male are predominant or gender difference was not shown in camptocormia [6], [15], [16].
Ergot DAs, cabergoline and perdolide, also induced antecollis [5], [9], [11], [18]. It is not statistically different in the appearance of antecollis between ergot DAs and non-ergot DAs [6]. Deformity developing after DA treatment usually resolves after discontinuing the offending drug [1], [5], [6], [7], [8], [9], [10], [11], [13]. However, we sometimes have experienced patients with DA induced antecollis whom motor symptoms were worsened after stopping DA. In our cases, overnight switching from PPX-IR to ROP-IR successfully resolved antecollis without deterioration of motor symptoms. The cause in this response was unclear. One proposed mechanism for antecollis is an imbalance between dopamine and norepinephrine, serotonin, acetylcholine, or glutamine levels, and the ways in which these neurotransmitters regulate axial muscle tone [1]. The binding profile at multiple classes of dopaminergic and serotonergic receptors differs somewhat between PPX and ROP, and affinity at the 5HT2B receptor was much stronger for ROP than for PPX [19]. In our patients, a dopaminergic–serotonergic imbalance in the striatum by PPX might be improved by changing ROP.
In conclusion, PPX-induced antecollis are rare, but should be considered in female and advanced PD patients treated with PPX. Switching to DA was successful in early and advanced PD patients with antecollis, and it appears useful as one option in the treatment of antecollis.
The following are the supplementary data related to this article.
Case 1 shows marked antecollis. She was not able to raise up her head.
One month after overnight switching from 1.5 mg PPX-IR to 6 mg ROP-IR, the patient can raise her head smoothly.
Disclosure
The authors declare that they have no conflicts of interest.
We obtained the permission for the publication of the video material by the patient.
References
- 1.Doherty K.M., van de Warrenburg B.P., Peralta M.C. Postural deformities in Parkinson's disease. Lancet Neurol. 2011;10:538–549. doi: 10.1016/S1474-4422(11)70067-9. [DOI] [PubMed] [Google Scholar]
- 2.Ashour R., Jankovic J. Joint and skeletal deformities in Parkinson's disease, multiple system atrophy, and progressive supranuclear palsy. Mov. Disord. 2006;21:1856–1863. doi: 10.1002/mds.21058. [DOI] [PubMed] [Google Scholar]
- 3.Quinn N. Disproportionate antecollis in multiple system atrophy. Lancet. 1989;1:844. doi: 10.1016/s0140-6736(89)92300-3. [DOI] [PubMed] [Google Scholar]
- 4.Kashihara K., Ohno M., Tomita S. Dropped head syndrome in Parkinson's disease. Mov. Disord. 2006;21:1213–1216. doi: 10.1002/mds.20948. [DOI] [PubMed] [Google Scholar]
- 5.Fujimoto K. Dropped head in Parkinson's disease. J. Neurol. 2006;253 doi: 10.1007/s00415-006-7006-3. (VII 21–26) [DOI] [PubMed] [Google Scholar]
- 6.Kashihara K., Imanura T. Clinical correlates of anterior and lateral flexion of the thoracolumbar spine and dropped head in patients with Parkinson's disease. Parkinsonism Relat. Disord. 2012;18:30–34. doi: 10.1016/j.parkreldis.2011.11.012. [DOI] [PubMed] [Google Scholar]
- 7.Yoshiyama Y., Takama J., Hattori T. The drop head sign in parkinsonism. J. Neurol. Sci. 1999;167:22–25. doi: 10.1016/s0022-510x(99)00129-x. [DOI] [PubMed] [Google Scholar]
- 8.Suzuki M., Hirai T., Ito Y. Pramipexole-induced antecollis in Parkinson's disease. J. Neurol. Sci. 2008;264:195–197. doi: 10.1016/j.jns.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 9.Oyama G., Hayashi A., Mizuno Y. Mechanism and treatment of dropped head syndrome associated with parkinsonism. Parkinsonism Relat. Disord. 2009;15:181–186. doi: 10.1016/j.parkreldis.2008.04.040. [DOI] [PubMed] [Google Scholar]
- 10.Taguchi Y., Takashima S., Tanaka K. Pramipexole-induced dropped head syndrome in Parkinson's disease. Intern. Med. 2008;47:2011–2012. doi: 10.2169/internalmedicine.47.1579. [DOI] [PubMed] [Google Scholar]
- 11.Uzawa A., Mori M., Kojima S. Dopamine agonist-induced antecollis in Parkinson's disease. Mov. Disord. 2009;24:2408–2411. doi: 10.1002/mds.22779. [DOI] [PubMed] [Google Scholar]
- 12.Kataoka H., Ueno S. Dropped head associated with amantadine in Parkinson's disease. Clin. Neuropharmacol. 2011;34:48–49. doi: 10.1097/WNF.0b013e318204d35c. [DOI] [PubMed] [Google Scholar]
- 13.Kim H.J., Jeon B.S., Kim S.H. Reversible antecollis associated with pramipexole in a patient with Parkinson's disease. J. Clin. Neurosci. 2012;19:903–904. doi: 10.1016/j.jocn.2011.09.015. [DOI] [PubMed] [Google Scholar]
- 14.Oh Y.S., Kim J.S., Ryu D.W. Donepezil induced antecollis in a patient with Parkinson's disease dementia. Neurol. Sci. 2013;34:1685–1686. doi: 10.1007/s10072-012-1242-3. [DOI] [PubMed] [Google Scholar]
- 15.Lepoutre A.C., Devos D., Blanchard-Dauphin A. A specific clinical pattern of camptocormia in Parkinson's disease. J. Neurol. Neurosurg. Psychiatry. 2006;77:1229–1234. doi: 10.1136/jnnp.2005.083998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tiple D., Fabbrini G., Colosimo C. Camptocormia in Parkinsons disease: an epidemiological and clinical study. J. Neurol. Neurosurg. Psychiatry. 2009;80:145–148. doi: 10.1136/jnnp.2008.150011. [DOI] [PubMed] [Google Scholar]
- 18.Matsui H., Udaka F., Kubori T. Parkinson disease with kubisagari. Neurol. Med. (Tokyo) 2004;61:94–98. [Google Scholar]
- 19.Millam M.J. From the cell to the clinic: a comparative review of the partial D2/D3 receptor agonist and α2-adrenoceptor antagonist, piribedil, in the treatment of Parkinson's disease. Pharmacol. Ther. 2010;128:229–273. doi: 10.1016/j.pharmthera.2010.06.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Case 1 shows marked antecollis. She was not able to raise up her head.
One month after overnight switching from 1.5 mg PPX-IR to 6 mg ROP-IR, the patient can raise her head smoothly.