This randomized clinical trial of Latino adults with poorly controlled type 2 diabetes compares the effect of a community health worker intervention vs enhanced usual care on blood pressure, LDL cholesterol, and hemoglobin A1c levels.
Key Points
Question
Can a community health worker intervention improve outcomes among Latinos with poorly controlled type 2 diabetes?
Finding
In this randomized clinical trial of 300 Latino adults, a community health worker intervention resulted in modest improvements in hemoglobin A1c levels. The effect on systolic blood pressure varied and did not meet the preplanned target, and no changes in low-density lipoprotein cholesterol levels were observed.
Meaning
The community health worker intervention showed improvement in only 1 of the 3 preplanned primary outcomes.
Abstract
Importance
Community health worker (CHW) intervention is a promising approach to address type 2 diabetes among Latinos. However, evidence from randomized clinical studies is limited.
Objective
To compare a CHW intervention with enhanced usual care.
Design, Setting, and Participants
This 52-week, single-blind, randomized clinical trial included 300 Latino adults aged 18 to 65 years who were treated in 2 public hospital outpatient clinics in Miami-Dade County, Florida, from July 1, 2010, through October 31, 2013. Eligible participants had a hemoglobin A1c (HbA1c) level of 8.0 or greater. Follow-up was completed January 31, 2015, and data were analyzed from March 10, 2015, to June 6, 2016.
Interventions
A 1-year CHW intervention consisted of home visits, telephone calls, and group-level activities.
Main Outcomes and Measures
Primary outcomes included systolic blood pressure (SBP), low-density lipoprotein cholesterol (LDLC) levels, and HbA1c levels. Secondary outcomes included body mass index, medication regimen intensification, and self-reported measures of diet, physical activity, and medication regimen adherence.
Results
Of the 300 participants randomized (135 men [45%] and 165 women [55%]; mean [SD] age, 55.2 [7.0] years), we obtained follow-up data on 215 (71.7%). Participants in the CHW group received a median of 4 home visits and 20 telephone calls. After adjusting for baseline values and covariates, participants in the CHW group had an HbA1c level that was 0.51% lower (95% CI, −0.94% to −0.08%) than that of participants in the enhanced usual care group. The reduction in SBP of 4.62 mm Hg (95% CI, −9.01 to −0.24 mm Hg) did not meet the preplanned target of 8 mm Hg and was not statistically significant in unadjusted models. No significant differences in LDLC levels (mean difference, −8.2 mg/dL; 95% CI, −18.8 to 2.3 mg/dL) or any of the preplanned secondary outcomes were observed. Post hoc analyses suggest that the intervention may be more beneficial among those with worse control of their type 2 diabetes at baseline.
Conclusions and Relevance
Among Latinos with poorly controlled type 2 diabetes, a 12-month CHW intervention lowered HbA1c levels by 0.51%. The intervention did not lead to improvements in LDLC levels, and the findings with respect to SBP were variable and half of what was targeted. Future studies should examine whether CHW interventions affect other measures, such as access to health care or social determinants of health.
Trial Registration
clinicaltrials.gov Identifier: NCT01152957
Introduction
In the United Sates, Latinos are almost twice as likely as non-Hispanic white individuals to be diagnosed with type 2 diabetes. Furthermore, nearly three-quarters of the Latino population 45 years and older has type 2 diabetes or prediabetes. Effective strategies for improving health outcomes among this group incorporate culturally tailored multifactorial interventions delivered for longer than 6 months. Most promising are individualized high-intensity interventions that incorporate community health workers (CHWs; also known as lay health workers).
A large body of data from nonexperimental studies supports the use of CHWs among Latinos with type 2 diabetes. However, the evidence from randomized clinical trials (RCTs) is limited. As recently reviewed, the few existing RCTs showing positive outcomes have had several limitations, including behavioral rather than physiologic outcomes, short follow-up, and/or focus on Latinos of Mexican origin. In addition, in most studies, CHWs served as part of a multidisciplinary intervention that included professional health care workers, such as nurse practitioners or pharmacists, managing medication regimens. This diversity makes evaluation of the independent effect of CHWs distinct from the broader intervention involving various types of health care workers difficult.
In this study, we present findings from the Miami Healthy Heart Initiative, an RCT of 300 Latinos with type 2 diabetes randomized to enhanced usual care (EUC) or a comprehensive 1-year CHW intervention. We tested the hypothesis that a CHW intervention would reduce systolic blood pressure (SBP) and low-density lipoprotein cholesterol (LDLC) levels, 2 of the most important and modifiable determinants of macrovascular complications in patients with type 2 diabetes, and enhance glycemic control (determined by hemoglobin A1c [HbA1c] level), an important modifiable determinant of diabetic microvascular complications.
Methods
Detailed methods of the Miami Healthy Heart Initiative have been previously described, and a copy of the study protocol is available in Supplement 1. In brief, the study was a single-blind, parallel-group, pragmatic RCT in which patients were randomized to the CHW intervention or the EUC group in a 1:1 ratio stratified by sex. The study was conducted among patients receiving care at 1 of 2 safety-net clinics in Miami-Dade County, Florida. Both clinics were part of the county’s public hospital system. Care at both sites is provided by trainees (internal medicine or family medicine) under the supervision of attending physicians. The study was approved by the human subjects research office of the University of Miami, Miami, Florida. All patients provided written informed consent.
Participants were recruited from July 1, 2010, through October 31, 2013, and follow-up was completed on January 31, 2015. Eligible participants were Latino adults aged 18 to 65 years with at least 2 clinic visits and a last HbA1c level of 8.0% or greater (to convert to a proportion of total hemoglobin level, multiply by 0.01). With use of contact information from the electronic medical record, eligible patients were sent a letter describing the study and an opt-out option (by mail or telephone) if they did not wish to participate. A research assistant followed up by telephone with potential participants who did not opt out. Patients were excluded if they had been diagnosed with type 2 diabetes less than 6 months previously, self-reported having type 1 diabetes, were diagnosed with type 2 diabetes at younger than 25 years, were enrolled in other intervention studies, or planned to move from the county within the next year.
Eligible patients interested in participating were invited to a baseline evaluation at the University of Miami. After providing informed consent, participants underwent phlebotomy, and samples were analyzed for LDLC and HbA1c levels at the University of Miami Diabetes Research Institute. Systolic blood pressure was assessed using automated cuffs according to American Heart Association guidelines. Participants then completed a structured interview consisting of validated survey instruments assessing sociodemographic characteristics, depression, medication regimen adherence, physical activity, and nutritional intake. We also reviewed medication lists at baseline and 12 months to determine whether any intensification of the medication regimen (increased dosage or additional medication) used to treat blood pressure, type 2 diabetes, or hypercholesterolemia occurred. Patients were then randomized by the study statistician (H.L.) in a 1:1 ratio to 1 of 2 groups using an allocation sequence conducted before study commencement. At 12 months, participants were invited to a follow-up assessment using similar procedures. The research assistant conducting the follow-up interview was blinded to subject allocation.
EUC Group
Participants randomized to the EUC group continued to receive care from their primary health care clinician. Resources available at the clinics included social workers and nurse educators who could provide counseling on nutrition, physical activity, type 2 diabetes education, and medication regimen adherence. In addition to these existing services, our study team mailed EUC type 2 diabetes education materials to participants every 3 months. Follow-up telephone calls were conducted approximately 2 weeks after each mailing to confirm receipt of mailings and verify contact information.
CHW Intervention
Participants randomized to the CHW intervention continued to receive usual care from their health care clinicians. All needed tests, services, medications, and appointments were coordinated by the primary care clinician. Patients also received 12 months of a personalized CHW intervention. The CHWs providing the intervention completed a 75-hour training curriculum, including CHW-specific skills (35 hours); type 2 diabetes clinical and behavioral interventions (20 hours), including motivational interviewing training; and basic research methods, including training on human participants research (20 hours). The CHW trainees also shadowed 5 patient home visits with another CHW before receiving their initial cases. Ongoing periodic CHW training on issues such as CHW skills, clinic and insurance navigation, cardiovascular disease and type 2 diabetes care, and human participants occurred approximately every 2 months. The CHWs were not part of the health care system staff.
The bulk of the CHW intervention was provided via tailored home visits and telephone calls. The frequency of visits and calls was tailored to each patient’s needs based on information gathered during the enactment phase. However, 4 home visits and 12 calls during the 12 months were considered a reasonable target. In addition, intervention participants were invited to monthly educational groups led by CHWs and bimonthly exercise groups in parks located within a convenient proximity to their homes. The CHW services included health education, patient navigation (help obtaining appointments, appointment reminders, appointment preparation checklists, medication refills, assistance with behavioral health linkages, communication with the clinician about patient care issues, and ≥1 clinic visit with the patient), and health coaching (helping patients to prioritize concerns before clinician visits, bringing all their medications, and ensuring they informed clinicians during the visit about elevated home blood pressure or glucose level readings). For long-term disease management, CHWs used culturally relevant resources, manuals, and tool kits. In addition, based on a framework of social determinants of health, CHWs assisted with nonmedical services, such as housing, employment, legal and financial assistance, food resources, and, when needed, linkages to existing community social service providers. On a weekly basis, a CHW supervisor (a master’s level social worker) reviewed all CHW case logs and discussed intervention plans for participants. Fidelity was also tracked by random monitoring of CHW telephone calls, accompanying CHWs to selected home visits, attending group sessions, and reviewing quantitative data on visits, calls, and group activities. Each CHW caseload was approximately 30 patients.
Statistical Analysis
Data were analyzed from March 10, 2015, to June 6, 2016. The 3 primary outcomes included changes in SBP, LDLC level, and HbA1c level, calculated by subtracting the follow-up values from the baseline values. Our sample size of 300 patients (150 in each arm) was designed to detect clinically meaningful changes in SBP of 8 mm Hg; in LDLC level, 10 mg/dL (to convert to millimoles per liter, multiply by 0.0259); and in HbA1c level, 0.5%, allowing up to 25% attrition. The primary analysis consisted of a difference-in-difference analysis for these continuous outcomes as measured at baseline and at 12 months using simple unpaired 2-tailed t tests. Analysis of covariance was used to estimate HbA1c level, SBP, and LDLC level at follow-up, adjusting for their corresponding baseline values and baseline potential confounders, such as age, sex, body mass index (BMI) (calculated as weight in kilograms divided by height in meters squared), educational attainment, depression, and comorbidity, that were selected a priori. We also report a subgroup analysis restricted to those participants who had an HbA1c level of at least 9.0% or an SBP of at least 140 mm Hg at study entry. Two sensitivity analyses were conducted to account for missing data among participants lost to or unavailable for follow-up. One was multiple imputation using 30 replication data sets with the previous observations as covariates and monotone missing data patterns. The other was imputation using the third-quartile scores of participants who completed the evaluation. This latter approach assumes that participants lost to attrition had worse outcomes than those who remained in the study. For binary secondary outcomes with preintervention and postintervention values, we used generalized estimating equation models. For those with values only at 12 months, such as medication regimen intensification, χ2 tests were used to compare differences between groups. We used SAS (version 9.2; SAS Institute, Inc) with an α value of .05 to test for significance.
Results
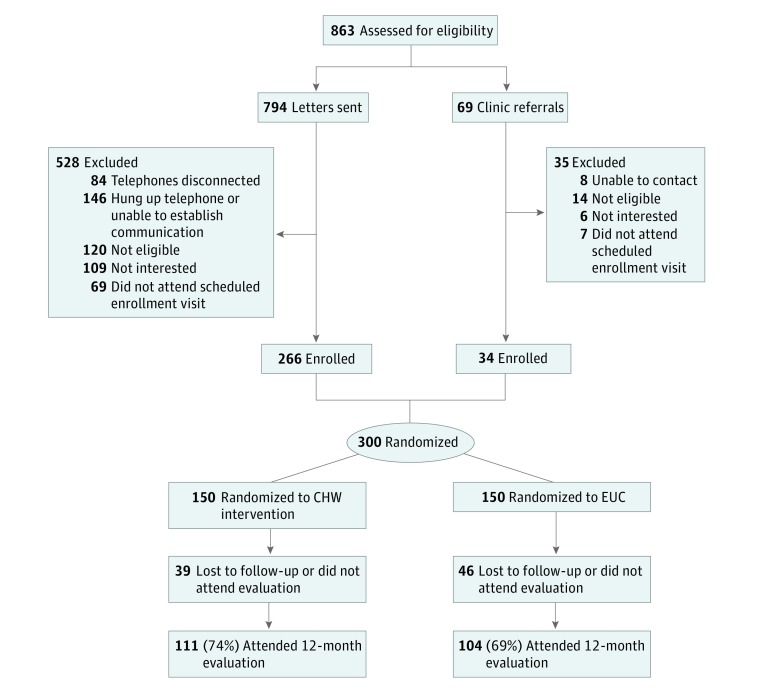
Our review of electronic medical record data identified 794 potentially eligible study participants. Clinicians referred 69 additional potential participants. We were able to contact 625 patients (72.4%) via telephone. Of these, 115 (18.4%) declined to participate, and 134 (21.4%) did not meet study eligibility criteria; 76 of 376 (20.2%) who had agreed to a baseline evaluation did not attend such a visit, despite multiple scheduling attempts (Figure). A total of 300 patients (135 men [45%] and 165 women [55%]; mean [SD] age, 55.2 [7.0] years) were enrolled.
Figure. Study Recruitment Flow Diagram for the Miami Healthy Heart Initiative.
CHW indicates community health worker; EUC, enhanced usual care.
Baseline characteristics of participants are provided in Table 1. Additional characteristics have been previously published. With respect to Latino ancestry, 115 (38.3%) were born in Cuba; the rest were from more than a dozen different Latin American countries. Although more than 80% of participants had been living in the United States for longer than 10 years, only 140 (46.7%) had become citizens. Furthermore, nearly half (143 [47.7%]) scored the lowest possible score on the acculturation scale, but only 45 (15%) lacked adequate health literacy.
Table 1. Baseline Characteristics of Participants in the Miami Healthy Heart Initiativea.
| Characteristic | Participant Groupa | |
|---|---|---|
| EUC (n = 150) |
CHW (n = 150) |
|
| Age, mean (SD), y | 55.2 (6.1) | 55.3 (7.1) |
| Male | 67 (44.7) | 68 (45.3) |
| Uninsured | 122 (81.3) | 122 (81.3) |
| BMI, mean (SD) | 32.3 (7.9) | 32.2 (6.9) |
| Income level ≤$1000/mob | 62 (47.3) | 55 (42.3) |
| Educational attainment <12 y | 64 (42.7) | 61 (40.7) |
| US citizen | 71 (47.3) | 69 (46.0) |
| Active smoker | 24 (16.0) | 21 (14.0) |
| Duration of type 2 diabetes, mean (SD), y | 11.2 (8.4) | 11.7 (8.2) |
| Comorbidity score, mean (SD)c | 3.55(2.2) | 3.43 (2.4) |
| Depressiond | 103 (68.7) | 109 (72.7) |
| Low acculturatione | 76 (50.7) | 67 (44.7) |
| Inadequate health literacyf | 21 (14.0) | 24 (16.0) |
| SBP, mean (SD), mm Hg | 135 (20) | 131 (18)g |
| LDLC level, mean (SD), mg/dL | 107 (40) | 102 (40) |
| HbA1c level, mean (SD), % | 9.3 (1.9) | 9.3 (2.1) |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); CHW, community health worker; EUC, enhanced usual care; HbA1c, hemoglobin A1c; LDLC, low-density lipoprotein cholesterol.
SI conversion factors: To convert Hb A1c to a proportion of total hemoglobin, multiply by 0.01; LDLC to millimoles per liter, multiply by 0.0259.
Data are presented as number (percentage) of patients unless otherwise indicated. No statistically significant differences were found in the distribution of sociodemographic characteristics or LDLC and HbA1c levels between groups.
Thirty-nine participants (19 in the EUC and 20 in the CHW groups) declined to answer.
Measure described by Charlson et al.
Measure described by Prince et al.
Measure described by Marin et al.
Measure described by Lee et al.
P = .052 for the differences in baseline SBP between groups.
At study entry, the mean (SD) HbA1c level was 9.3% (2.0%) and the mean (SD) SBP was 133 (19) mm Hg, with 144 patients (48%) at the SBP target of less than 130 mm Hg (based on guidelines at the time of the study). Although the CHW and EUC groups had a similar distribution of sociodemographic characteristics, baseline SBP was higher in the EUC group (Table 1).
At 12 months, 215 participants (71.7%) completed the follow-up assessment. Forty-six patients (30.7%) in the EUC and 39 patients (26%) in the CHW groups were lost to attrition (P = .37). Review of medical records showed that most participants who were lost to attrition in the study were also no longer being followed up in the health care system. Those who did not complete the 12-month follow-up assessment had higher baseline mean HbA1c levels (9.8%) than did those who completed the 12-month assessment (9.1%).
Of the 150 participants randomized to the CHW intervention, the median number of home visits received was 5 (interquartile range [IQR], 2-7), the median number of CHW visits with the patient to the clinic was 1 (IQR, 0-2), and median number of telephone calls was 20 (IQR, 12-32). Most participants (126 [84%]) received at least 12 CHW contacts in the year. Participation with group activities was variable, with 93 (62%) of the sample not attending any such activities. Competing demands such as child-care responsibilities and work were cited as major reasons for nonparticipation. Among those who attended any group activity, the median number of group activities attended was 4 (IQR, 2-7).
We found that compared with participants in the EUC group, participants in the CHW intervention had statistically significant improvements in HbA1c level (Table 2). For example, after adjusting for differences in baseline values and potential covariates, the HbA1c level in participants in the CHW group was 0.51% lower (95% CI, −0.94% to −0.08%). In addition, at study conclusion, the proportion of patients with type 2 diabetes under moderate control (HbA1c level ≤8.0%) was 42 (37.8%) in the CHW group vs 26 (25%) in the EUC group (P = .03). Furthermore, in a post hoc analysis limited to the 101 study completers who entered the study with an HbA1c level of at least 9.0%, the HbA1c level was 1.36% lower (95% CI, −0.59% to 22.1%) in the CHW vs the EUC group.
Table 2. Differences in Primary Outcomes at 12 Months Between the CHW and EUC Groupsa.
| Analysis | Primary Outcome, Mean Difference (95% CI) | ||
|---|---|---|---|
| HbA1c Level, % | SBP, mm Hg | LDLC Level, mg/dL | |
| Unadjusted | −0.59 (−1.1 to −0.11)b | −2.03 (−6.93 to 2.87) | −3.54 (−15.28 to 8.19) |
| Adjusted for baseline value | −0.52 (−0.94 to −0.09)b | −3.91 (−8.28 to 0.46) | −8.13 (−18.57 to 2.30) |
| Adjusted for baseline values and covariatesc | −0.51 (−0.94 to −0.08)b | −4.62 (−9.01 to −0.24)b | −8.21 (−18.74 to 2.32) |
Abbreviations: CHW, community health worker; EUC, enhanced usual care; HbA1c, hemoglobin A1c; LDLC, low-density lipoprotein cholesterol.
SI conversion factors: To convert HbA1c to a proportion of total hemoglobin, multiply by 0.01; LDLC to millimoles per liter, multiply by 0.0259.
Includes 215 participants with 12-month follow-up data.
The 95% CIs for these measures do not include zero.
Adjusted for age, body mass index, sex, comorbidity, educational attainment, and depression.
When we examined SBP, we found that reductions in SBP were only statistically significant in the multivariate models (−4.62 mm Hg; 95% CI, −9.01 to −0.24 mm Hg), and the observed reductions in SBP were lower than our planned target of 8 mm Hg. In a subgroup analysis limited to the 65 study completers who entered the study with an SBP of at least 140 mm Hg, at 1 year the SBP was 13.6 mm Hg lower in the CHW vs EUC group (95% CI, −2.0 to −25.1 mm Hg), which we consider as an exploratory post hoc finding. In all analyses, the differences in LDLC levels were not statistically significant (mean difference in the multivariate model, −8.2 mg/dL; 95% CI, −18.8 to 2.3 mg/dL).
In sensitivity analysis using multiple imputation to account for missing outcome data for all 300 patients, the effects were nearly identical to those in the multivariate analysis based only on the 215 cases with complete data. Imputation using third-quartile scores showed smaller effects. In all sensitivity analyses, the 95% CIs for HbA1c levels remained statistically significant, whereas they varied for SBP based on the approach used (eTable in Supplement 2).
Last, to examine potential pathways through which the CHW intervention may have improved HbA1c level, we examined differences in changes in BMI, self-reported physical activity, and fruit and vegetable intake among participants in the CHW and EUC groups. At baseline, 134 participants (58%) were obese (BMI>30.0), 156 (52%) were sedentary, and the mean (SD) fruit and vegetable intake was only 2.6 (1.6) servings per day. We did not find any significant differences in these measures between the CHW and EUC groups. Although medication regimen intensification was slightly greater in the CHW than EUC groups for medications to lower lipid levels (29 [26.4%] vs 16 [15.5%]) and to treat type 2 diabetes (48 [43.6%] vs 33 [31.7%]), this difference did not meet our criteria for statistical significance (P = .053 and P = .08, respectively). We also did not find any significant changes in self-reported medication regimen adherence score between the 2 groups (Table 3).
Table 3. Secondary Outcomes at Baseline and 12 Months Among the CHW and EUC Groupsa.
| Secondary Outcome | Participant Group | |||
|---|---|---|---|---|
| EUC (n = 104) |
CHW (n = 111) |
|||
| Baseline | 12 Months | Baseline | 12 Months | |
| BMI, mean (SD) | 32.8 (8.0) | 32.7 (7.7) | 32.4 (7.1) | 32.1 (6.7) |
| Fruit and vegetable intake, mean (SD), servings/db | 2.6 (1.6) | 3.3 (2.1) | 2.5 (1.6) | 2.7 (1.6) |
| Sedentary, No. (%)c | 56 (53.9) | 58 (55.8) | 56 (50.5) | 57 (51.4) |
| Medication adherence score, mean (SD)d | 5.5 (1.9) | 5.4 (1.9) | 5.8 (1.6) | 5.4 (1.7) |
| Medication regimen intensification, No. (%)e | ||||
| Blood pressure | NA | 24 (23.3) | NA | 24 (21.8) |
| Type 2 diabetesf | NA | 33 (31.7) | NA | 48 (43.6) |
| Lowering of lipid levelsg | NA | 16 (15.5) | NA | 29 (26.4) |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); CHW, community health worker; EUC, enhanced usual care; NA, not applicable.
We did not find any significant differences between baseline and 12-month changes and no difference-in-differences across groups.
Measured using the Centers for Disease Control and Prevention Fruit and Vegetable Consumption Questionnaire.
Measured by the International Physical Activity Questionnaire.
One patient was missing in each group. Measure described by Morisky et al. Scores range from 1 to 8, with higher scores indicating greater adherence.
Measure described by Carrasquillo et al. For EUC, n = 103; for CHW, n = 110.
P = .053.
P = .08.
Discussion
We found that among Latinos with poorly controlled type 2 diabetes, a 12-month CHW intervention resulted in modest improvements in HbA1c levels. This change was robust in all the sensitivity analyses. The findings with respect to SBP were statistically significant only in multivariate analysis and did not meet our preplanned target. Post hoc analyses suggest that for HbA1c level and SBP, the CHW intervention may have a greater effect among those with poorer glycemic and SBP control at baseline. The intervention did not result in measurable improvements in LDLC levels.
Our findings are consistent with those of other RCTs among Latinos, which have found that CHW interventions can result in a similar magnitude of reduction in HbA1c level but not SBP. In most such studies, CHWs were integrated as part of a broader intervention that included medication management by health care professionals. The few prior studies in which the CHW intervention was examined independently have reported conflicting results. One study in New York found that CHW intervention did not lead to improvements in any measures. However, intervention fidelity was a limitation in that study. In another recent RCT, CHW intervention resulted in improvements in behavioral outcomes but not in physiologic measures. In contrast, another study among Mexicans found similar improvements in HbA1c level and not in SBP. However, that study had much greater service intensity consisting of 36 home visits during 2 years.
Unfortunately, our study does not provide conclusive information on which aspects of the CHW intervention led to the observed improvements in HbA1c level. We did not find any change in BMI or self-reported measures of diet, physical activity, or medication regimen adherence. Differences in medication regimen intensification were of borderline statistical significance. For patients with home blood pressure readings or blood glucose levels that were repeatedly elevated, CHWs would call clinicians or schedule urgent appointments. This process could have resulted in clinicians intensifying medication regimens.
Although the findings on HbA1c levels were modest, such reductions are similar to the effect of diabetes medications on glycemic control. In our study, in a low-income population that is medically indigent, the CHW intervention achieved similar reductions without medication management. Furthermore, even small changes in HbA1c level have considerable clinical significance. In 1 large study, a 0.8% reduction in HbA1c level was associated with a 10% lower risk of macrovascular and microvascular outcomes.
In addition, 212 participants, or 70.7% of our population, had positive findings on screening for depression. Helping a predominantly uninsured population find high-quality culturally acceptable behavioral and mental health services was a major challenge. The CHWs were trained to screen for depression by using standardized instruments and on the processes and procedures to link patients with the mental health resources that exist in the community. However, uptake of such referrals was low owing to limited availability of such services, and patients often were reluctant to pursue such care. Training CHWs in cognitive behavioral therapy should be considered for future CHW-led diabetes interventions.
Dissemination of CHW programs is also a challenge. To this end, we have published an implementation guide that includes more detail on specific components of the intervention and case studies by CHWs as examples of ways that they helped address many of the social and health systems barriers encountered. Lack of reimbursement is also a major barrier to CHW uptake. We estimate that with a caseload of 30 patients, the cost for a CHW and supervising case manager would be approximately $2300 annually per patient. This cost is similar to that of newer diabetes medications. Furthermore, in 2012, median US health expenditures for individuals with diabetes were nearly $14 000 per year. Thus, from a societal perspective, the costs of such a program may not seem unreasonable. However, because CHW services are not routinely covered by most insurance plans, health care systems may lack sufficient resources on their own to invest in such programs.
Limitations
Our findings include several caveats. First, our findings for SBP were variable based on the method of analysis, and we found no effect on LDLC levels. At study entry, nearly half the patients were already at the targeted SBP and LDLC level. As suggested by our post hoc analyses, this finding and the loss of statistical power owing to attrition may have limited our ability to detect a more robust effect on SBP. In addition, the intervention was designed as a 1-year program, with the last 2 months serving to wean participants off the intervention. To have a more definitive effect on outcomes, CHW interventions may need to be ongoing.
Conclusions
A CHW intervention among Latinos with type 2 diabetes in South Florida resulted in improvements in only 1 of the 3 primary outcomes. Additional studies will need to examine whether CHW interventions affect other important measures such as access to or satisfaction with care. Furthermore, when our findings were presented to community groups, they noted our outcomes focused on physiologic and behavioral measures and did not include measures that may be more important to patients, such as immigration, housing, and employment. With increased recognition that social determinants of health have a major effect on population health, future studies evaluating CHW interventions should also include such outcomes.
Trial Protocol
eTable. Sensitivity Analysis to Account for Missing Data
References
- 1.Centers for Disease Control and Prevention Tables of Summary Health Statistics. Summary Health Statistics National Health Interview Survey: 2014. Table A-4. https://www.cdc.gov/nchs/nhis/shs/tables.htm Updated January 24, 2017. Accessed February 4, 2017.
- 2.National Heart, Lung, and Blood Institute Hispanic Community Health Study Data Book: A Report to the Communities. Bethesda, MD: National Institutes of Health; 2013:13-7951. [Google Scholar]
- 3.Peek ME, Cargill A, Huang ES. Diabetes health disparities: a systematic review of health care interventions. Med Care Res Rev. 2007;64(5)(suppl):101S-156S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Community Preventive Services Task Force Diabetes Prevention: Interventions Engaging Community Health Workers. 2017 Centers For Disease Prevention and Control. https://www.thecommunityguide.org/sites/default/files/assets/Diabetes-Prevention-Community-Health-Workers.pdf. Updated January 25, 2017. Accessed February 4, 2017.
- 5.Carrasquillo O, Patberg E, Alonzo Y, Li H, Kenya S. Rationale and design of the Miami Healthy Heart Initiative: a randomized controlled study of a community health worker intervention among Latino patients with poorly controlled diabetes. Int J Gen Med. 2014;7:115-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Palmas W, March D, Darakjy S, et al. . Community health worker interventions to improve glycemic control in people with diabetes: a systematic review and meta-analysis. J Gen Intern Med. 2015;30(7):1004-1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Emdin CA, Rahimi K, Neal B, Callender T, Perkovic V, Patel A. Blood pressure lowering in type 2 diabetes: a systematic review and meta-analysis. JAMA. 2015;313(6):603-615. [DOI] [PubMed] [Google Scholar]
- 8.Kearney PM, Blackwell L, Collins R, et al. ; Cholesterol Treatment Trialists’ (CTT) Collaborators . Efficacy of cholesterol-lowering therapy in 18,686 people with diabetes in 14 randomised trials of statins: a meta-analysis. Lancet. 2008;371(9607):117-125. [DOI] [PubMed] [Google Scholar]
- 9.Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359(15):1577-1589. [DOI] [PubMed] [Google Scholar]
- 10.Patel A, MacMahon S, Chalmers J, et al. ; ADVANCE Collaborative Group . Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358(24):2560-2572. [DOI] [PubMed] [Google Scholar]
- 11.Perloff D, Grim C, Flack J, et al. . Human blood pressure determination by sphygmomanometry. Circulation. 1993;88(5, pt 1):2460-2470. [DOI] [PubMed] [Google Scholar]
- 12.Prince MJ, Reischies F, Beekman AT, et al. . Development of the EURO-D Scale—a European, Union initiative to compare symptoms of depression in 14 European centres. Br J Psychiatry. 1999;174:330-338. [DOI] [PubMed] [Google Scholar]
- 13.Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich). 2008;10(5):348-354. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 14.International Physical Activity Questionnaire Web site. Guidelines for the data processing and analysis of the international physical activity questionnaire. https://sites.google.com/site/theipaq/ Updated July 30. 2016. Accessed July 1, 2013.
- 15.Centers for Disease Control and Prevention (CDC) State-specific trends in fruit and vegetable consumption among adults—United States, 2000-2009. MMWR Morb Mortal Wkly Rep. 2010;59(35):1125-1130. [PubMed] [Google Scholar]
- 16.Lebron C, Alonzo Y, Castillo A, et al. From one CHW to another: a community health worker's guide. http://www.ces4health.info/find-products/view-product.aspx?code=K6GJYM8G. Published November 14, 2015. Accessed July 12, 2016.
- 17.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373-383. [DOI] [PubMed] [Google Scholar]
- 18.National Research Council ; Panel on Handling Missing Data in Clinical Trials; Committee on National Statistics, Division of Behavioral and Social Sciences and Education. The Prevention and Treatment of Missing Data in Clinical Trials. Washington, DC: National Academies Press; 2010. [Google Scholar]
- 19.De Waal T, Pannekoek J, Scholtus S. Handbook of Statistical Data Editing and Imputation. Hoboken, NJ: John Wiley & Sons; 2011. [Google Scholar]
- 20.Marin G, Sabogal F, Marin BV. Development of a short acculturation scale for Hispanics. Hisp J Behav Sci. 1987;9:183-205. [Google Scholar]
- 21.Lee SY, Stucky BD, Lee JY, Rozier RG, Bender DE. Short Assessment of Health Literacy–Spanish and English: a comparable test of health literacy for Spanish and English speakers. Health Serv Res. 2010;45(4):1105-1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kenya S, Lebron CN, Chang AYH, Li H, Alonzo YA, Carrasquillo O. A profile of Latinos with poorly controlled diabetes in South Florida. J Community Hosp Intern Med Perspect. 2015;5(2):26586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.American Diabetes Association Standards of medical care in diabetes–2012. Diabetes Care. 2012;35(suppl 1):S11-S63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pérez-Escamilla R, Damio G, Chhabra J, et al. . Impact of a community health workers–led structured program on blood glucose control among Latinos with type 2 diabetes: the DIALBEST trial. Diabetes Care. 2015;38(2):197-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Palmas W, Findley SE, Mejia M, et al. . Results of the northern Manhattan diabetes community outreach project: a randomized trial studying a community health worker intervention to improve diabetes care in Hispanic adults. Diabetes Care. 2014;37(4):963-969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Baig AA, Benitez A, Locklin CA, et al. ; Little Village Community Advisory Board . Picture good health: a church-based self-management intervention among Latino adults with diabetes. J Gen Intern Med. 2015;30(10):1481-1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rothschild SK, Martin MA, Swider SM, et al. . Mexican American trial of community health workers: a randomized controlled trial of a community health worker intervention for Mexican Americans with type 2 diabetes mellitus. Am J Public Health. 2014;104(8):1540-1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Duckworth W, Davis SN. Comparison of insulin glargine and NPH insulin in the treatment of type 2 diabetes: a review of clinical studies. J Diabetes Complications. 2007;21(3):196-204. [DOI] [PubMed] [Google Scholar]
- 29.Stratton IM, Adler AI, Neil HA, et al. . Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321(7258):405-412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lebron CN, Reyes-Arrechea E, Castillo A, Carrasquillo O, Kenya S. Tales from the Miami Healthy Heart Initiative: the experiences of two community health workers. J Health Care Poor Underserved. 2015;26(2):453-462. [DOI] [PubMed] [Google Scholar]
- 31.Mutamba BB, van Ginneken N, Smith Paintain L, Wandiembe S, Schellenberg D. Roles and effectiveness of lay community health workers in the prevention of mental, neurological and substance use disorders in low and middle income countries: a systematic review. BMC Health Serv Res. 2013;13:412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Institute for Clinical and Economic Review Controversies in the management of patients with type 2 diabetes. http://icer-review.org/wp-content/uploads/2014/08/CEPAC-T2D-Final-Report-December-22.pdf Published December 2014. Accessed July 12, 2016.
- 33.American Diabetes Association Economic costs of diabetes in the U.S. in 2012. Diabetes Care. 2013;36(4):1033-1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Adler NE, Cutler DM, Jonathan JE, et al. . Addressing Social Determinants of Health and Health Disparities. Discussion Paper, Vital Directions for Health and Health Care Series. Washington, DC: National Academy of Medicine; September 19, 2006. https://nam.edu/addressing-social-determinants-of-health-and-health-disparities-a-vital-direction-for-health-and-health-care/. Accessed February 28, 2017. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
eTable. Sensitivity Analysis to Account for Missing Data