Key Points
Question
Is prehospital blood product transfusion among military combat casualties associated with improved acute and 30-day survival?
Findings
In this retrospective cohort study of 502 US military combat casualties undergoing medical evacuation, prehospital transfusion was associated with improved survival at 24 hours (adjusted hazard ratio for mortality, 0.26) and at 30 days (adjusted hazard ratio for mortality, 0.39).
Meaning
Prehospital transfusion of blood products in a military combat setting was associated with greater likelihood of survival.
Abstract
Importance
Prehospital blood product transfusion in trauma care remains controversial due to poor-quality evidence and cost. Sequential expansion of blood transfusion capability after 2012 to deployed military medical evacuation (MEDEVAC) units enabled a concurrent cohort study to focus on the timing as well as the location of the initial transfusion.
Objective
To examine the association of prehospital transfusion and time to initial transfusion with injury survival.
Design, Setting, and Participants
Retrospective cohort study of US military combat casualties in Afghanistan between April 1, 2012, and August 7, 2015. Eligible patients were rescued alive by MEDEVAC from point of injury with either (1) a traumatic limb amputation at or above the knee or elbow or (2) shock defined as a systolic blood pressure of less than 90 mm Hg or a heart rate greater than 120 beats per minute.
Exposures
Initiation of prehospital transfusion and time from MEDEVAC rescue to first transfusion, regardless of location (ie, prior to or during hospitalization). Transfusion recipients were compared with nonrecipients (unexposed) for whom transfusion was delayed or not given.
Main Outcomes and Measures
Mortality at 24 hours and 30 days after MEDEVAC rescue were coprimary outcomes. To balance injury severity, nonrecipients of prehospital transfusion were frequency matched to recipients by mechanism of injury, prehospital shock, severity of limb amputation, head injury, and torso hemorrhage. Cox regression was stratified by matched groups and also adjusted for age, injury year, transport team, tourniquet use, and time to MEDEVAC rescue.
Results
Of 502 patients (median age, 25 years [interquartile range, 22 to 29 years]; 98% male), 3 of 55 prehospital transfusion recipients (5%) and 85 of 447 nonrecipients (19%) died within 24 hours of MEDEVAC rescue (between-group difference, −14% [95% CI, −21% to −6%]; P = .01). By day 30, 6 recipients (11%) and 102 nonrecipients (23%) died (between-group difference, −12% [95% CI, −21% to −2%]; P = .04). For the 386 patients without missing covariate data among the 400 patients within the matched groups, the adjusted hazard ratio for mortality associated with prehospital transfusion was 0.26 (95% CI, 0.08 to 0.84, P = .02) over 24 hours (3 deaths among 54 recipients vs 67 deaths among 332 matched nonrecipients) and 0.39 (95% CI, 0.16 to 0.92, P = .03) over 30 days (6 vs 76 deaths, respectively). Time to initial transfusion, regardless of location (prehospital or during hospitalization), was associated with reduced 24-hour mortality only up to 15 minutes after MEDEVAC rescue (median, 36 minutes after injury; adjusted hazard ratio, 0.17 [95% CI, 0.04 to 0.73], P = .02; there were 2 deaths among 62 recipients vs 68 deaths among 324 delayed transfusion recipients or nonrecipients).
Conclusions and Relevance
Among medically evacuated US military combat causalities in Afghanistan, blood product transfusion prehospital or within minutes of injury was associated with greater 24-hour and 30-day survival than delayed transfusion or no transfusion. The findings support prehospital transfusion in this setting.
This cohort study examines associations between prehospital blood product transfusion and injury survival among US military combat casualties in Afghanistan.
Introduction
Hemorrhage is a leading cause of preventable death in both military and civilian trauma care. The National Academies of Sciences, Engineering, and Medicine have recommended integration of military and civilian trauma care into a national trauma system to achieve the aim of zero preventable deaths after injury, compelling advances in the treatment of life-threatening hemorrhage.
The evolution of the military trauma system in Afghanistan addressed factors contributing to hemorrhagic mortality through systematic improvements including tourniquet use; a mandate for rapid rotary wing medical evacuation (MEDEVAC); better management of hemorrhagic shock, blood loss, and coagulopathy; availability of critical care transport teams; and forward deployment of surgical facilities. Although prehospital transfusion for high-risk combat casualties began as early as the Franco-Prussian war of 1870, modern use of prehospital transfusion for US military casualties was limited before 2012.
Even though it is intuitive that early transfusion for hemorrhagic shock should improve survival, published data on prehospital transfusion to date do not demonstrate a survival advantage. A recent systematic review detailed limitations in prehospital transfusion trauma care research including significantly heterogeneous findings, lack of patient follow-up, flawed matching of recipient and nonrecipient cohorts, missing data, inadequate statistical adjustment to control for between-group differences, exposure misclassification (eg, transfusion initiated during interfacility transfer), selective exclusion of early deaths, and inadequate statistical power to detect mortality differences. A recent multicenter prospective observational study of prehospital transfusion among civilian trauma patients reported inconclusive findings. The goal of this study was to evaluate US military experience with prehospital blood product transfusion on MEDEVAC aircraft in Afghanistan, directly addressing the deficiencies in the literature.
Methods
Design and Study Setting
In 2012, prehospital transfusion capability for combat casualties in Afghanistan expanded in stages, starting with the highest-volume MEDEVAC site and gradually extending to serve all casualties in Afghanistan, allowing for the opportunity to retrospectively study concurrent cohorts. The study was deemed exempt from institutional review board approval by the Department of Defense Joint Trauma System.
Data Sources
Patients were identified from the Department of Defense trauma registry, the prehospital trauma registry, and the Armed Forces Medical Examiner System Database. Missing or questionable data values unresolved by electronic resources were supplemented or verified with data abstracted from original medical records.
Study Population
Casualties in Afghanistan between April 1, 2012, and August 7, 2015, were included if all of the following criteria were met: individual was a member of the US military, survived at least until MEDEVAC rescue from point of injury, and had at least 1 established criterion for prehospital transfusion for severe trauma (≥1 traumatic limb amputation with at least 1 located above the knee or elbow, or shock defined as a systolic blood pressure <90 mm Hg or a heart rate >120 beats per minute) documented on initial transport from point of injury.
Exposure
The exposures of interest were defined as (1) initiation of prehospital transfusion (red blood cells [RBCs], plasma, or both) en route from point of injury to a surgical hospital and (2) minutes from MEDEVAC rescue to first transfusion (regardless of location; ie, prior to or during hospitalization). Transfusion recipients were compared with nonrecipients for whom transfusion was delayed or not given. During the study period, prehospital transfusion-capable MEDEVAC teams carried at least 2 U of RBCs or 1 U each of RBCs and plasma.
Outcomes and Other Variables
Prespecified coprimary outcomes were 24-hour and 30-day survival after MEDEVAC rescue. Conditional 30-day survival among patients surviving the first 24 hours was a prespecified secondary analysis. The prevalence of shock (defined as a systolic blood pressure <90 mm Hg, a heart rate >120 beats per minute, or a shock index >0.9 [calculated as heart rate ÷ systolic blood pressure]) measured at hospital admission was the prespecified secondary end point.
Even though prehospital transfusion was well documented, the capability to transfuse was not known with certainty for transport teams serving nonrecipients. To balance the study groups based on injury severity, nonrecipients of prehospital transfusion were frequency matched on 5 documented factors likely to have been visible to the transport teams: (1) mechanism of injury (gunshot vs explosion), (2) positive indicator of prehospital shock defined as above, but measured prior to hospital admission (yes or no), (3) type and severity of traumatic limb amputation in 4 categories (none, 1 below knee or elbow, ≥2 below knee or elbow or 1 above knee or elbow, ≥2 above knee or elbow), (4) hemorrhagic torso injury assessed by Abbreviated Injury Scale (AIS) diagnostic code (yes or no), and (5) severity of head injury assessed by maximum head AIS score in 3 categories (0-1, 2, ≥3) (Figure 1). The AIS score designates severity of injury by body region (head, face, chest, abdomen, extremities, and external), ranging from 0 (no injury) to 6 (not survivable). Prehospital transfusion recipients were classified into 26 strata, each with a unique matching-factor profile. Nonrecipients of prehospital transfusion with a profile matching that of 1 or more recipients were selected into each stratum, allowing the ratio of nonrecipients to recipients to vary across strata.
Figure 1. Study Design.
aHemorrhagic torso injury assessed by Abbreviated Injury Scale (AIS) diagnostic code and severity of head injury assessed by maximum head AIS score.
Additional covariates for adjustment were age and minutes from injury occurrence to MEDEVAC rescue (continuous), injury year in 4 categories (for each calendar year during which the study took place), transport team (in 2 categories), and prehospital tourniquet use (yes or no). The varying matching ratios and additional covariates necessitated regression modeling to balance the study groups for potential confounders.
To examine the balance achieved by the matching and covariate-adjusted modeling, patient characteristics after hospital arrival were compared across study groups including elapsed time from injury occurrence to hospital arrival, MEDEVAC transport time, receipt of tranexamic acid, level of care available at the first surgical hospital, initial laboratory values, total units of RBCs or whole blood received from the time of MEDEVAC rescue to 24 hours after hospital admission, total hospital days among 30-day survivors, maximum AIS score, and Injury Severity Score (ISS). To compute ISS, the AIS scores for the 3 most severely injured body regions are each squared and then summed, or if any AIS score equals 6, the maximum ISS of 75 is assigned.
Statistical Analysis
Unadjusted associations were assessed using the χ2 test, the Wilcoxon rank sum test, and the Fisher exact test. One transfusion recipient and 13 nonrecipients (from various other strata) had missing data for the time from injury occurrence to MEDEVAC rescue; however, there were no missing data for the 4 other covariates included in the modeling, the 5 matching factors, or the prespecified outcomes. Adjusted analyses were performed only for complete cases without missing data. Balance across matched study groups was evaluated with median and multiple logistic regression adjusted for all 10 covariates simultaneously (including matching factors).
Initial Cox proportional hazards models were stratified by the matched groups and adjusted for the 5 other covariates. To generate survival curves, equivalent Cox models adjusted for all 10 covariates simultaneously and set each covariate at its median value. The delayed-entry approach adjusted all Cox models for left truncation (a source of potential immortal time bias) among transfusion recipients who were selected for analysis because they survived long enough to receive prehospital transfusions. Follow-up of matched and covariate-balanced nonrecipients was thus aligned to begin at the same minute after the MEDEVAC rescue that the prehospital transfusion started in the corresponding transfusion recipient with the shortest delay. Any matched and covariate-balanced nonrecipient who died on or before the earliest transfusion start time among corresponding transfusion recipients was not counted.
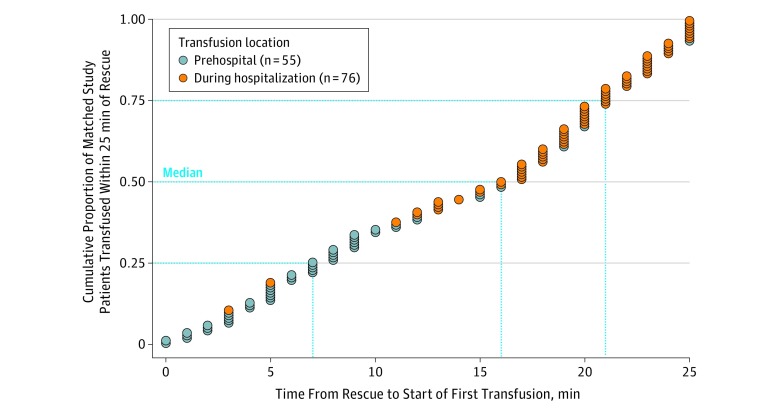
Time to initiation of transfusion (in minutes after MEDEVAC rescue), regardless of location (prior to or during hospitalization), was included in adjusted Cox models as a categorical variable. The times to the initial transfusion that overlapped between the prehospital transfusion recipients and nonrecipients who survived long enough to begin transfusion during hospitalization (≤25 minutes after MEDEVAC rescue) were examined in quartiles (Figure 2) and compared with longer delays. For a valid analysis consistent with Cox modeling for prehospital transfusion, a transfusion initiated during hospitalization (≤25 minutes after MEDEVAC rescue) among those who did not receive a prehospital transfusion was modeled as a time-dependent covariate, and the delayed-entry approach accounted for left truncation among prehospital transfusion recipients.
Figure 2. Time to Start of First Transfusion Among US Military Combat Casualties Transfused Within 25 Minutes of Rescue.
First transfusion started within 25 minutes after medical evacuation (MEDEVAC) rescue for all 55 prehospital transfusion recipients and for 76 nonrecipients who received transfusion during hospitalization. Quartile bounds were determined by the points of intersection on the grid defined by the axes: x (time to the start of transfusion after MEDEVAC rescue in 5-minute increments from 0 to 25) and y (0, 0.25, 0.50, 0.75, 1.00). Time to start for the first transfusion was examined for each quartile relative to longer delays (>25 minutes or no transfusion received within 24 hours after hospital admission).
The sensitivity analysis omitted nonrecipients for whom prehospital transfusion may have been considered futile (loss of vital signs without response to cardiopulmonary resuscitation en route, vital signs remained undetectable after hospital arrival, and classified by Armed Forces Medical Examiner System as prehospital death). The final Cox models met the proportional hazards assumption based on Schoenfeld residuals and log-log plots.
The association between prehospital transfusion and prevalence of shock at hospital admission was adjusted for all 10 covariates using multiple logistic regression, and for the competing risk of prehospital death by using survivor average causal-effect modeling. Final logistic models satisfied Pearson and Hosmer-Lemeshow goodness-of-fit tests. All hypothesis tests were 2-sided, P values <.05 were considered significant. Analyses were performed using SAS version 9.4 (SAS Institute Inc) and Stata version 14 (StataCorp).
Results
Characteristics of Entire Study Population
Between April 1, 2012, and August 7, 2015, there were 502 US casualties (median age, 25 years [interquartile range, 22-29 years]; 98% male) that met the selection criteria (Figure 1) with 55 recipients of prehospital transfusion and 447 nonrecipients. Transfusion recipients had more severe injuries than nonrecipients (Table 1). Among prehospital transfusion recipients, 38 received only RBCs (1 patient received 2 U), 7 received only 1 U of plasma, and 10 received 1 U of RBCs and 1 U of plasma. All 7 prehospital transfusion recipients who received only 1 U of prehospital plasma went on to receive 1 U or more of RBCs during hospitalization. Within 24 hours of MEDEVAC rescue, 3 of 55 prehospital transfusion recipients (5%) and 85 of 447 nonrecipients (19%) died (between-group difference, −14% [95% CI, −21% to −6%]; P = .01). By day 30, 6 prehospital transfusion recipients (11%) and 102 nonrecipients (23%) died (between-group difference, −12% [95% CI, −21% to −2%]; P = .04).
Table 1. Characteristics of US Military Combat Casualties Who Met Study Inclusion Criteria.
| Prehospital Transfusion Recipients (n = 55) |
Nonrecipients (n = 447) |
P Valuea |
Matched Nonrecipients (n = 345)b |
P Valuea,c |
|
|---|---|---|---|---|---|
| Injury Characteristics | |||||
| Mechanism of injury, No. (%)d | |||||
| Explosives | 46 (84) | 303 (68) | .03 | 244 (71) | .05 |
| Gunshot wound | 9 (16) | 119 (26) | 101 (29) | ||
| Other (motor vehicle crash, fall, etc) | 0 | 25 (6) | 0 | ||
| Documented prehospital shock, No. (%)d,e | 51 (93) | 405 (91) | .81 | 330 (96) | .31 |
| Type and severity of traumatic limb amputation, No. (%)d | |||||
| None | 15 (27) | 331 (74) | <.001 | 251 (73) | <.001 |
| 1 Below knee or elbow | 12 (22) | 48 (11) | 38 (11) | ||
| ≥2 Below knee or elbow or 1 above knee or elbow | 12 (22) | 38 (8) | 31 (9) | ||
| ≥2 Above knee or elbow | 16 (29) | 30 (7) | 25 (7) | ||
| Hemorrhagic torso injury assessed by AIS diagnostic code, No. (%)d | 31 (56) | 164 (37) | .008 | 122 (35) | .004 |
| Severity of head injury assessed by maximum head AIS score, No. (%)d,f | |||||
| 0-1 | 26 (47) | 185 (41) | .60 | 163 (47) | .62 |
| 2 | 18 (33) | 176 (39) | 129 (37) | ||
| ≥3 | 11 (20) | 86 (19) | 53 (15) | ||
| Patient Demographics and Other Characteristics | |||||
| Age, median (IQR), yg | 26 (23-29) | 25 (22-29) | .31 | 25 (22-29) | .31 |
| Year of injury, median (IQR)g | 2012 (2012-2013) | 2012 (2012-2013) | .30 | 2012 (2012-2013) | .45 |
| Transport team, No. (%)g,h | |||||
| US Army DUSTOFF | 41 (74) | 362 (81) | .002 | 278 (81) | .008 |
| US Air Force Pedro or UK MERT | 13 (24) | 42 (9) | 36 (10) | ||
| Unknown | 1 (2) | 43 (10) | 31 (9) | ||
| Tourniquet used prior to hospitalization, No. (%)g | 46 (84) | 203 (45) | <.001 | 156 (45) | <.001 |
| Minutes from injury occurrence to MEDEVAC rescue from point of injuryg | |||||
| No. of patients without missing data | 54 | 427 | 332 | ||
| Median (IQR) | 29 (20-41) | 25 (17-38) | .11 | 25 (16-38) | .14 |
| Minutes from MEDEVAC rescue to start of first transfusion | |||||
| No. of patients without missing data | 55 | 238i | 181i | ||
| Median (IQR) | 7 (4-9) | 30 (22-61) | <.001 | 28 (21-51) | <.001 |
Abbreviations: AIS, Abbreviated Injury Scale; DUSTOFF, US Army medical evacuation; IQR, interquartile range; MEDEVAC, medical evacuation; MERT, Medical Emergency Response Team; Pedro, US Air Force Pararescue.
Calculated using the unadjusted Fisher exact test.
Nonrecipients were matched to transfusion recipients by 5 matching factors that when taken together defined 26 unique strata for the 55 prehospital transfusion recipients and identified 345 matching nonrecipients. Each stratum contained 1 to 7 prehospital transfusion recipients (median, 2 patients) and 2 to 62 matched nonrecipients (median, 6 patients). The ratios of nonrecipients to recipients varied from 0.67 to 62.0 (median, 6 patients) per stratum. Matching did not balance the study groups in aggregate due to variation in the ratio of nonrecipients to recipients across strata, so the between-group differences for the posttreatment characteristics and the prespecified outcomes were assessed by regression models stratified by the matched groups or equivalently adjusted.
Comparison is prehospital transfusion recipients vs matched nonrecipients.
One of 5 matching factors by which nonrecipients were matched to prehospital transfusion recipients.
Defined as a systolic blood pressure of less than 90 mm Hg, a heart rate greater than 120, or a shock index greater than 0.9 (calculated as heart rate ÷ systolic blood pressure).
AIS scores range from 0 (no injury) to 6 (not survivable) for each of 6 body regions (head, face, chest, abdomen, extremities, and external).
Covariate included simultaneously with the other covariates in all regression models (along with statistical adjustment for matched groups).
Composed of at least 1 emergency medical technician for DUSTOFF; at least 2 paramedics for Pedro; and a physician-led resuscitation team for MERT.
Of 250 nonrecipients who received blood product transfusion during hospitalization, 186 were matched nonrecipients.
Characteristics of Matched Study Cohorts
The 5 matching factors classified the 55 recipients of prehospital transfusion into 26 unique strata, each containing from 1 to 7 patients (median, 2 patients). There were 345 matching nonrecipients identified, with the number of matched nonrecipients per stratum ranging from 2 to 62 (median, 6 patients) (Table 1). The ratio of matched nonrecipients to recipients per stratum ranged from 0.67 to 62.0 (median, 6 patients). Matching alone did not balance the study groups in aggregate because of the variable numbers of transfusion recipients and matched nonrecipients within each stratum.
By hour 24, 3 prehospital transfusion recipients died (5%) compared with 69 matched nonrecipients (20%) (between-group difference, −15% [95% CI, −22% to −7%]; P = .007). By day 30, 6 prehospital transfusion recipients died (11%) compared with 78 matched nonrecipients (23%) (between-group difference, −12% [95% CI, −21% to −2%]; P = .05). Regression modeling adjusted for frequency matching and additional covariates balanced the study groups with respect to evacuation and transport times, initial laboratory pH values, total hospital days among 30-day survivors, maximum AIS score, and ISS (Table 2). More prehospital transfusion recipients than nonrecipients received tranexamic acid (48/55 [87%] vs an estimated 45% of nonrecipients; P < .001). Tranexamic acid is an antifibrinolytic medication and potential confounder of the prehospital transfusion effects on survival. However, this medication was initiated during hospitalization for 150 (88%) of the 170 actual patients who received it; only 4 prehospital transfusion recipients (7%) received the initial dose before or concurrently with their initial transfusion.
Table 2. Characteristics After Hospital Arrival of US Military Combat Casualties Who Received or Did Not Receive Prehospital Transfusion.
| Characteristics | Prehospital Transfusion Recipients, Median (IQR) (n = 55)a |
Matched Nonrecipients, Median (95% CI) (n = 345)a,b |
P Value |
|---|---|---|---|
| Time from injury occurrence to arrival at first surgical hospital, min | |||
| No. of patients without missing data | 54 | 334 | |
| Value | 48 (37 to 59) | 46.9 (43.7 to 50.0) | .70 |
| MEDEVAC transport time, min | |||
| No. of patients without missing data | 55 | 333 | |
| Value | 17 (15 to 22) | 16.4 (13.2 to 19.5) | .70 |
| Received tranexamic acid, No. (%) [95% CI] | 48 (87) | 155 (45) [22 to 71] | <.001 |
| Initially transported to a role 3 surgical hospital, No. (%) [95% CI]c | 48 (87) | 192 (63) [39 to 81]d | .004 |
| Emergency department laboratory values | |||
| Base deficit, mEq/L | |||
| No. of patients without missing data | 52 | 249d | |
| Value | −7 (−11 to −4) | −6.2 (−7.9 to −4.4) | .37 |
| pH | |||
| No. of patients without missing data | 53 | 257d | |
| Value | 7.28 (7.17 to 7.38) | 7.29 (7.24 to 7.34) | .65 |
| Hemoglobin, g/dL | |||
| No. of patients without missing data | 51 | 261d | |
| Value | 12.4 (10.9 to 13.7) | 12.8 (11.4 to 13.4) | .24 |
| International normalized ratio | |||
| No. of patients without missing data | 34 | 210d | |
| Value | 1.4 (1.2 to 1.7) | 1.26 (1.16 to 1.36) | .008 |
| Total RBCs or whole blood by hour 24 after hospital admission, U | |||
| No. of patients without missing data | 55 | 186d,e | |
| Value | 15 (8 to 23) | 11.0 (8.5 to 13.5) | .002 |
| Total length of hospital stay among survivors at day 30, d | |||
| No. of patients without missing data | 48f | 265f | |
| Value | 30 (21 to 30) | 30 (27 to 33) | >.99 |
| Maximum Abbreviated Injury Scale (AIS) scoreg | 4 (3 to 5) | 4.0 (3.6 to 4.4) | .90 |
| Injury Severity Score (ISS)h | 29 (17 to 36) | 28.6 (24.0 to 33.2) | .88 |
Abbreviations: IQR, interquartile range; MEDEVAC, medical evacuation; RBCs, red blood cells.
Unless otherwise indicated.
Adjusted estimates from median and logistic regression adjusted simultaneously for the matching factors of (1) mechanism of injury, (2) prehospital shock, (3) type and severity of traumatic limb amputation, (4) hemorrhagic torso injury assessed by AIS diagnostic code, and (5) severity of head injury assessed by maximum head AIS score and for the 5 covariates of age, minutes from injury occurrence to MEDEVAC rescue, injury year, transport team, and prehospital tourniquet use.
Patients were transported to either a role 3 military hospital providing definitive theater support and advanced capabilities or a role 2 military surgical facility providing forward resuscitative care with limited resources.
Of the 304 nonrecipients who survived to receive treatment in the emergency department of the first surgical hospital.
There were 186 nonrecipients who received an initial transfusion during hospitalization.
Of the 49 recipients and 267 nonrecipients who were discharged alive or survived through hospital day 30.
Ranges from 0 (no injury) to 6 (not survivable) for each of 6 body regions (head, face, chest, abdomen, extremities, and external).
Computed as the sum of the squares of each AIS score for the 3 most severely injured body regions. If any AIS score is 6, the maximum ISS of 75 is assigned.
A greater percentage of prehospital transfusion recipients arrived alive at a role 3 vs a role 2 hospital (48/55 [87%] vs an adjusted 63% of surviving nonrecipients; P = .004). A role 3 hospital provides definitive theater support and advanced capabilities compared with a role 2 hospital, which provides forward resuscitative care with limited resources. Prehospital transfusion recipients also had higher international normalized ratios (1.40 vs 1.26 for matched nonrecipients; P = .008), suggesting a higher prevalence of coagulopathy, and more RBC or whole blood transfusions by hour 24 after hospital admission (15 U vs 11 U, respectively; P = .002).
Primary Survival Analysis
Exposure Defined as Prehospital Transfusion
In adjusted survival analyses among the 386 matched study patients with complete covariate data (97%), the association of survival with prehospital transfusion remained significant at both 24 hours and 30 days (Figure 3A, B). The adjusted hazard ratio (HR) for mortality was 0.26 (95% CI, 0.08-0.84; P = .02) over 24 hours (3 deaths among 54 prehospital transfusion recipients vs 67 deaths among 332 matched nonrecipients) and 0.39 (95% CI, 0.16-0.92; P = .03) over 30 days (6 deaths among 54 prehospital transfusion recipients vs 76 deaths among 332 matched nonrecipients). In adjusted Cox models that also included interaction terms to assess whether selected covariates modified the association of prehospital transfusion with survival, there were no significant variations across 24 hours (P = .14) or 30 days (P = .44) of follow-up, calendar year of injury occurrence (P = .93 at 24 hours and P = .77 at 30 days), or type of transport team (P = .53 at 24 hours and P = .76 at 30 days).
Figure 3. Mortality of Prehospital Transfusion Recipients vs Matched Nonrecipients.
Adjusted mortality curves were estimated by Cox proportional hazards modeling at the median value of each covariate. The median values for the matching factors were set as follows: (1) 0, explosives for mechanism of injury; (2) 1, yes for documented prehospital shock; (3) 2, two or more traumatic limb amputations below the knee or elbow, or 1 above the knee or elbow; (4) 1, Abbreviated Injury Scale score for head injury of 2; and (5) 1, yes for hemorrhagic torso injuries. The median values for the additional covariates were set as follows: age of 26 years, injury year of 2012, US Army DUSTOFF transport team, yes for prehospital tourniquet, and 29 minutes from injury occurrence to medical evacuation rescue. There were no patients lost to follow-up and the median survival times were 1440 minutes (24 hours) for the 24-hour survival analysis and 30 days for the 30-day survival analysis. HR indicates hazard ratio.
Among all patients in the matched groups who died within 30 days, 59 of the 84 deaths (70%) occurred within the first hour after MEDEVAC rescue or prior to hospital arrival, including 58 of 78 deaths (74%) among nonrecipients and 1 of 6 deaths (17%) among prehospital transfusion recipients. Deaths among nonrecipients early after MEDEVAC rescue contributed the most to the between-group difference in survival (Figure 3A, B). In adjusted Cox analyses focused on survival to 30 days conditional on 24-hour survival, the association with prehospital transfusion was not statistically significant (adjusted HR, 0.84 [95% CI, 0.18-4.00], P = .83; there were 3 deaths among 51 transfusion recipients vs 9 deaths among 265 nonrecipients; Figure 3C).
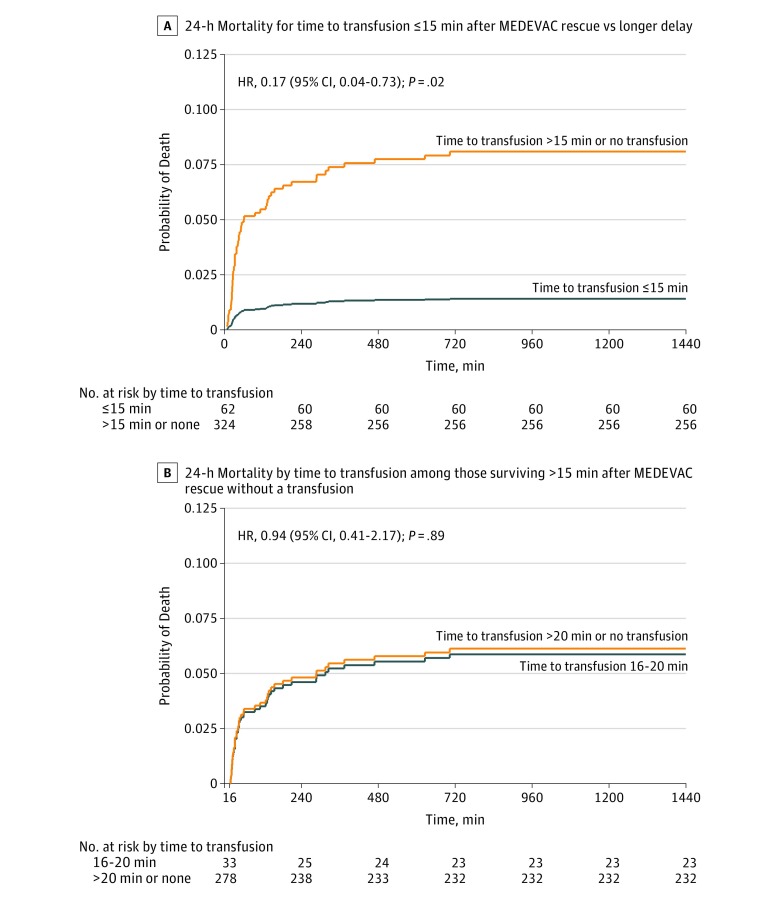
Exposure Defined as Time to First Transfusion
For 47 prehospital transfusion recipients and 76 nonrecipients who survived long enough to receive a transfusion during hospitalization, the times to initiate transfusion (regardless of location) overlapped (Figure 2). In the adjusted Cox models, only transfusions initiated within 15 minutes of MEDEVAC rescue (median, 36 minutes after injury) were associated with reduced 24-hour mortality (HR, 0.17 [95% CI, 0.04-0.73], P = .02; Figure 4A; there were 2 deaths among 62 recipients of transfusion within 15 minutes of MEDEVAC rescue vs 68 deaths among 324 matched patients with delayed treatment). For delays of only 1 to 5 minutes longer (16-20 minutes after MEDEVAC rescue), there was no significant association with survival at 24 hours (adjusted HR, 0.94 [95% CI, 0.41-2.17], P = .89; there were 10 deaths among 33 recipients of transfusion within 16-20 minutes of rescue vs 46 deaths among 278 matched patients with delayed treatment; Figure 4B). Prehospital deaths occurred only among nonrecipients, and after removing 21 of the total 41 in the sensitivity analysis to allow for possible transfusion futility, a reduced 24-hour mortality rate persisted for transfusions started within 15 minutes of MEDEVAC rescue (adjusted HR, 0.23 [95% CI, 0.06-0.96], P = .04; there were 2 deaths among 62 recipients of transfusion within 15 minutes of MEDEVAC rescue vs 47 deaths among 303 with delayed treatment).
Figure 4. Mortality by Time From Medical Evacuation (MEDEVAC) Rescue to Start of Transfusion.
Adjusted mortality curves by Cox proportional hazards modeling at the median value of each covariate. The median time to start of transfusion was 36 minutes after injury (interquartile range, 27-46 minutes). The median values for the matching factors were set as follows: (1) 0, explosives for mechanism of injury; (2) 1, yes for documented prehospital shock; (3) 2, two or more traumatic limb amputations below the knee or elbow, or 1 above the knee or elbow; (4) 1, Abbreviated Injury Scale score for head injury of 2; and (5) 1, yes for hemorrhagic torso injuries. The median values for the additional covariates were set as follows: age of 26 years, injury year of 2012, US Army DUSTOFF transport team, yes for prehospital tourniquet, and 29 minutes from injury occurrence to medical evacuation rescue. There were no patients lost to follow-up and the median survival times were 1440 minutes (24 hours) for the 24-hour survival analysis and 30 days for the 30-day survival analysis. HR indicates hazard ratio.
Secondary End Point Analysis
Of the 55 prehospital transfusion recipients, 42 (76%) had documented shock measured at arrival to the first surgical hospital compared with an estimated 206 of the 299 surviving matched nonrecipients (69%) (adjusted for all 10 covariates including documented prehospital shock measured during transport). Adjusting also for competing risk of prehospital death, prehospital transfusion had no statistically significant association with shock at hospital admission (adjusted odds ratio, 1.01 [95% CI, 0.86-1.18]; P = .94).
Discussion
In this retrospective cohort study of US military casualties transported on MEDEVAC helicopters in Afghanistan, prehospital transfusion within minutes of injury was associated with significantly reduced 24-hour and 30-day mortality. Concurrent cohorts in this retrospective study minimized the potential confounding inherent to historical comparisons of preintervention vs postintervention outcomes. Findings were consistent regardless of whether they were derived from (1) the unadjusted analyses of all 502 casualties; (2) the survival analysis adjusted for matching, other covariates, and immortal time bias; or (3) the sensitivity analysis for possible transfusion futility, which removed more than half (21) of the 41 prehospital deaths among nonrecipients of prehospital transfusion.
The results of this study must be interpreted within the context of the military trauma system in which the transfusions were given. First, during the time frame of this study, the “golden hour rule” was in effect, which had been mandated by the US Secretary of Defense. This policy prescribed that injured service members designated as urgent evacuation casualties arrive at a location equipped with surgical capability within 1 hour from the time of initial MEDEVAC request. The golden hour rule fueled expansion of the MEDEVAC service and forward-deployed surgical resources, resulting in the median total evacuation time of 47 minutes for patients in this study population.
Second, military casualties receive prompt life-saving treatment at the point of injury from trained medical and nonmedical first responders with an initial emphasis on control of massive external hemorrhage. This is an advantage not currently available to most civilian trauma patients.
Third, all deaths in this military population were captured with complete autopsy examinations, including prehospital deaths. Early hemorrhagic deaths constitute a large proportion of patients predicted to benefit from prehospital transfusion. Thus, to fully understand the effect of prehospital transfusion, inclusion of prehospital deaths is critical. Civilian trauma centers have been reported to vary significantly in their detection of early deaths, especially prehospital deaths. In addition, unlike previous studies, the US military study population allowed capture of complete 30-day follow-up.
The increase in survival observed in this study is significant, consistent with a UK study of military casualties, but distinct from civilian studies. The conditional 30-day survival analysis among 24-hour survivors revealed how an approach used in some previous studies may be flawed. Excluding prehospital and early deaths within 24 hours of hospital admission, which are primarily due to hemorrhage, may introduce survival bias, rendering the true association between injury mortality and early transfusion undetectable.
Because the time to initiate transfusion during hospitalization may in some cases be shorter than the time to prehospital transfusion, it is important to evaluate time to first transfusion without regard to location. Transfusion is a critical intervention in the treatment of hemorrhagic shock, however, the exact length of time to hemorrhagic death will vary for each individual patient depending on injury pattern and available hemorrhage-control capabilities. It may be challenging for civilian and immature military trauma systems to deliver transfusion resources in time to prevent exsanguination, especially with a tolerance margin as narrow as these results suggest.
Four recent prospective studies of prehospital transfusion in civilian trauma settings may be able to further address the issues of transfusion timing, inclusion of early deaths, and other limitations of previous studies. Two of these 4 studies were designed to evaluate prehospital RBC and plasma transfusion, including the first randomized trial under way and another that reported inconclusive findings. The remaining 2 studies were designed to examine prehospital transfusion of plasma only; one is under way, and the other was terminated for futility.
Limitations
This study has several limitations. Retrospective studies cannot overcome unmeasured confounding. Although receipt of prehospital transfusion was well documented in medical records, the prehospital transfusion capability of MEDEVAC teams transporting nonrecipients was not. To enhance between-group comparability, nonrecipients were matched to prehospital transfusion recipients. Because stratification on posttreatment surrogates for severity (eg, massive transfusion, ISS) has introduced bias into both randomized and observational studies of prehospital trauma care, the current study used only matching and additional covariate adjustment based on documented injury characteristics that prehospital transport teams would likely observe.
Compared with nonrecipients, prehospital transfusion recipients had more casualties transported by the US Air Force Pararescue (call sign Pedro) and the UK Medical Emergency Response Teams, which are aircraft platforms equipped with higher levels of care that could confer survival advantages vs the more common US Army MEDEVAC (call sign DUSTOFF) aircraft platforms. However, the potential for varying MEDEVAC capabilities to modify or confound results was systematically evaluated. Regardless of different patient selection, matching, or statistical adjustment strategies, the association of prehospital transfusion with reduced mortality was consistent without significant variation for follow-up time, injury year, or transport team capabilities. Moreover, in-hospital care (regardless of complexity or intensity) had little opportunity to influence the observed associations because transfusion initiated within 15 minutes and deaths prior to hospital arrival or within 1 hour of MEDEVAC rescue contributed most to the observed between-group differences in mortality.
A sensitivity analysis was applied as a mitigation strategy for potential transfusion futility among nonrecipients reported as unresponsive to resuscitation efforts after the loss of vital signs en route. Because prehospital transfusion may have been considered futile for at least some moribund casualties, the sensitivity analysis omitted all of them to reduce mortality to the lowest extreme among nonrecipients. Despite removing more than 50% of prehospital deaths, 24-hour mortality was still significantly decreased for recipients of transfusions started within about 36 minutes after injury. In addition, although all of the 55 prehospital transfusion recipients received at least 1 U of additional blood product after hospital arrival, 112 matched nonrecipients (32%) survived longer than 24 hours without receiving any transfusion, which could cast doubt on their eligibility for prehospital transfusion. If these casualties were excluded, a higher mortality rate among the nonrecipients would further strengthen the association of prehospital transfusion with survival, but would also further reduce statistical power and precision. Alongside consistently favorable and statistically significant associations of prehospital and early transfusion with survival, the study’s modest sample size of only 55 prehospital transfusion recipients generated broad 95% CIs with upper bounds close to null, especially for 30-day survival.
Early deaths prior to MEDEVAC arrival were excluded from the study to focus on casualties who could possibly have received transfusions. During this study, capability for transfusion prior to MEDEVAC arrival was nominal and no recipients were identified. It is possible that even earlier transfusion (ie, prior to the estimated 36 minutes shown in this study) may be associated with a greater likelihood of survival. More research in this area is needed.
Conclusions
Among medically evacuated US military combat causalities in Afghanistan, blood product transfusion prehospital or within minutes of injury was associated with greater 24-hour and 30-day survival than delayed transfusion or no transfusion. The findings support prehospital transfusion in this setting.
References
- 1.Eastridge BJ, Mabry RL, Seguin P, et al. Death on the battlefield (2001-2011): implications for the future of combat casualty care [published correction appears in J Trauma Acute Care Surg. 2013;74(2):706]. J Trauma Acute Care Surg. 2012;73(6)(suppl 5):S431-S437. [DOI] [PubMed] [Google Scholar]
- 2.Davis JS, Satahoo SS, Butler FK, et al. An analysis of prehospital deaths: who can we save? J Trauma Acute Care Surg. 2014;77(2):213-218. [DOI] [PubMed] [Google Scholar]
- 3.National Academies of Sciences, Engineering, and Medicine A National Trauma Care System: Integrating Military and Civilian Trauma Systems to Achieve Zero Preventable Deaths after Injury. Washington, DC: National Academies Press; 2016. [PubMed] [Google Scholar]
- 4.Kragh JF Jr, Walters TJ, Baer DG, et al. Survival with emergency tourniquet use to stop bleeding in major limb trauma. Ann Surg. 2009;249(1):1-7. [DOI] [PubMed] [Google Scholar]
- 5.Kotwal RS, Howard JT, Orman JA, et al. The effect of a golden hour policy on the morbidity and mortality of combat casualties. JAMA Surg. 2016;151(1):15-24. [DOI] [PubMed] [Google Scholar]
- 6.Butler FK, Holcomb JB, Kotwal RS, et al. Fluid resuscitation for hemorrhagic shock in tactical combat casualty care: TCCC guidelines proposed change 14-01. J Spec Oper Med. 2014;14(3):13-38. [DOI] [PubMed] [Google Scholar]
- 7.Borgman MA, Spinella PC, Perkins JG, et al. The ratio of blood products transfused affects mortality in patients receiving massive transfusions at a combat support hospital. J Trauma. 2007;63(4):805-813. [DOI] [PubMed] [Google Scholar]
- 8.Morrison JJ, Dubose JJ, Rasmussen TE, Midwinter MJ. Military Application of Tranexamic Acid in Trauma Emergency Resuscitation study (MATTERs). Arch Surg. 2012;147(2):113-119. [DOI] [PubMed] [Google Scholar]
- 9.Carrick MM, Leonard J, Slone DS, Mains CW, Bar-Or D. Hypotensive resuscitation among trauma patients [published online August 9, 2016]. Biomed Res Int. doi: 10.1155/2016/8901938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Butler FK, Giebner SD, McSwain N, Pons P, eds. Prehospital Trauma Life Support Manual. 8th ed Burlington, MA: Jones and Bartlett Learning; 2014. [Google Scholar]
- 11.Morrison JJ, Oh J, DuBose JJ, et al. En-route care capability from point of injury impacts mortality after severe wartime injury. Ann Surg. 2013;257(2):330-334. [DOI] [PubMed] [Google Scholar]
- 12.Brewer HF, Ellis R, Greaves RIN, et al. Blood Transfusion. London, England: Simpkin Marshall; 1949. [Google Scholar]
- 13.Powell-Dunford N, Quesada JF, Malsby RF, et al. Risk management analysis of air ambulance blood product administration in combat operations. Aviat Space Environ Med. 2014;85(11):1130-1135. [DOI] [PubMed] [Google Scholar]
- 14.Smith IM, James RH, Dretzke J, Midwinter MJ. Prehospital blood product resuscitation for trauma: a systematic review. Shock. 2016;46(1):3-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Holcomb JB, Swartz MD, DeSantis SM, et al. ; PROHS Study Group . Multicenter observational prehospital resuscitation on helicopter study. J Trauma Acute Care Surg. 2017;83(1)(suppl 1):S83-S91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stannard A, Morrison JJ, Scott DJ, Ivatury RA, Ross JD, Rasmussen TE. The epidemiology of noncompressible torso hemorrhage in the wars in Iraq and Afghanistan. J Trauma Acute Care Surg. 2013;74(3):830-834. [DOI] [PubMed] [Google Scholar]
- 17.Sjölander A, Greenland S. Ignoring the matching variables in cohort studies—when is it valid and why? Stat Med. 2013;32(27):4696-4708. [DOI] [PubMed] [Google Scholar]
- 18.Keiding N. Delayed entry In: Armitage P, Colton T, eds. Encyclopedia of Biostatistics: 2. New York, NY: John Wiley & Sons; 2005:1-5. [Google Scholar]
- 19.Klein JP, Moeschberger MI. Survival Analysis: Techniques for Censored and Truncated Data. 2nd ed New York, NY: Springer; 2005. [Google Scholar]
- 20.Kalbfleisch JD, Prentice RL. The Statistical Analysis of Failure Time Data. 2nd ed New York, NY: John Wiley & Sons; 2002. [Google Scholar]
- 21.Azzato EM, Greenberg D, Shah M, et al. Prevalent cases in observational studies of cancer survival: do they bias hazard ratio estimates? Br J Cancer. 2009;100(11):1806-1811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ho AM-H, Dion PW, Ng CS, Karmakar MK. Understanding immortal time bias in observational cohort studies. Anaesthesia. 2013;68(2):126-130. [DOI] [PubMed] [Google Scholar]
- 23.Mackenzie EJ, Rivara FP, Jurkovich GJ, et al. The impact of trauma-center care on functional outcomes following major lower-limb trauma. J Bone Joint Surg Am. 2008;90(1):101-109. [DOI] [PubMed] [Google Scholar]
- 24.Tchetgen Tchetgen EJ, Phiri K, Shapiro R. A simple regression-based approach to account for survival bias in birth outcomes research. Epidemiology. 2015;26(4):473-480. [DOI] [PubMed] [Google Scholar]
- 25.Shakur H, Roberts I, Bautista R, et al. ; CRASH-2 Trial Collaborators . Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): a randomised, placebo-controlled trial. Lancet. 2010;376(9734):23-32. [DOI] [PubMed] [Google Scholar]
- 26.Handley MA, Schillinger D, Shiboski S. Quasi-experimental designs in practice-based research settings: design and implementation considerations. J Am Board Fam Med. 2011;24(5):589-596. [DOI] [PubMed] [Google Scholar]
- 27.O’Reilly DJ, Morrison JJ, Jansen JO, Apodaca AN, Rasmussen TE, Midwinter MJ. Prehospital blood transfusion in the en route management of severe combat trauma: a matched cohort study. J Trauma Acute Care Surg. 2014;77(3)(suppl 2):S114-S120. [DOI] [PubMed] [Google Scholar]
- 28.Tisherman SA, Schmicker RH, Brasel KJ, et al. Detailed description of all deaths in both the shock and traumatic brain injury hypertonic saline trials of the Resuscitation Outcomes Consortium. Ann Surg. 2015;261(3):586-590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gomez D, Xiong W, Haas B, Goble S, Ahmed N, Nathens AB. The missing dead: the problem of case ascertainment in the assessment of trauma center performance. J Trauma. 2009;66(4):1218-1224. [DOI] [PubMed] [Google Scholar]
- 30.Holcomb JB, Tilley BC, Baraniuk S, et al. ; PROPPR Study Group . Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial. JAMA. 2015;313(5):471-482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.del Junco DJ, Fox EE, Camp EA, Rahbar MH, Holcomb JB; PROMMTT Study Group . Seven deadly sins in trauma outcomes research: an epidemiologic post mortem for major causes of bias. J Trauma Acute Care Surg. 2013;75(1)(suppl 1):S97-S103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Powell EK, Hinckley WR, Gottula A, Hart KW, Lindsell CJ, McMullan JT. Shorter times to packed red blood cell transfusion are associated with decreased risk of death in traumatically injured patients. J Trauma Acute Care Surg. 2016;81(3):458-462. [DOI] [PubMed] [Google Scholar]
- 33.UK Clinical Trials Gateway Resuscitation with Pre-hospital Blood Products (RePHILL). https://ukctg.nihr.ac.uk/trials/trial-details/trial-details?trialNumber=ISRCTN62326938. Accessed April 20, 2017.
- 34.Clinical Trials.gov Prehospital Air Medical Plasma Trial (PAMPer). https://clinicaltrials.gov/show/NCT01818427. Accessed April 20, 2017.
- 35.Clinical Trials.gov Control of Major Bleeding After Trauma Study (COMBAT). https://clinicaltrials.gov/show/NCT01838863. Accessed April 20, 2017.
- 36.del Junco DJ, Bulger EM, Fox EE, et al. ; ROC Investigators . Collider bias in trauma comparative effectiveness research: the stratification blues for systematic reviews. Injury. 2015;46(5):775-780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Apodaca A, Olson CM Jr, Bailey J, Butler F, Eastridge BJ, Kuncir E. Performance improvement evaluation of forward aeromedical evacuation platforms in Operation Enduring Freedom. J Trauma Acute Care Surg. 2013;75(2)(suppl 2):S157-S163. [DOI] [PubMed] [Google Scholar]
- 38.Mabry RL, Apodaca A, Penrod J, Orman JA, Gerhardt RT, Dorlac WC. Impact of critical care-trained flight paramedics on casualty survival during helicopter evacuation in the current war in Afghanistan. J Trauma Acute Care Surg. 2012;73(2)(suppl 1):S32-S37. [DOI] [PubMed] [Google Scholar]