Abstract
This study assess the association between the elements of the patient-centered medical home model and clinical quality in the Veterans Health Administration’s Patient Aligned Care Team program.
Despite widespread adoption of the patient-centered medical home (PCMH) model, it is unknown which components are most related to clinical quality. We sought to assess the association between elements of the PCMH model and clinical quality in the Veterans Health Administration’s (VHA’s) national PCMH initiative, the Patient Aligned Care Team (PACT) program.
Methods
In a patient-level observational study, we included veterans who received primary care from fiscal year 2012 to 2014 and had their medical records abstracted by an independent, external contractor for the External Peer Review Program (n = 422 125). We used External Peer Review Program data for 48 clinical quality measures for chronic disease management and disease prevention that are comparable to Healthcare Effectiveness Data and Information Set measures. We gauged clinic-level PCMH implementation in 2012 for 909 clinics using the PACT implementation Progress Index (Pi2), which includes 8 core components (access, continuity, care coordination, comprehensiveness, self-management support, patient-centered care and communication, shared decision making, and team-based care). We modeled the association between quartile of the Pi2 component and the 48 clinical quality indicators using generalized estimating equations for binary outcomes (modeled jointly), accounting for within-patient correlation across quality measures and adjusting for multiple comparisons. We calculated mean marginal effects to report differences in the probability of meeting clinical quality between the highest- and lowest-quartile Pi2 component scores. To estimate the full adoption of PACT throughout the VHA, we calculated the number of patients who would have met each quality measure if they had been cared for in high-Pi2 clinics, given model results, and the number of patients in the VHA primary care population eligible for each measure in the low- and medium-Pi2 clinics in 2014. The evaluation efforts are part of an going quality improvement effort at the VHA and are not considered research activity; they are thus not subject to institutional review board review or waiver.
Results
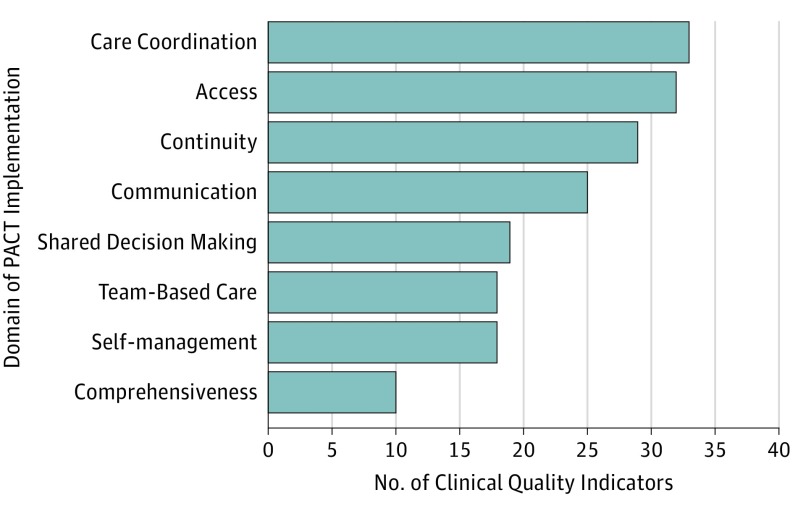
Overall, higher scores on each of the 8 components of Pi2 were associated with better performance on clinical quality indicators (Figure). The Pi2 components that were most strongly associated with a clinic meeting the most clinical quality indicators were care coordination, access, continuity, and communication. Clinics with high care coordination performed significantly better on 33 (69%) of 48 quality measures compared with clinics with lower scores. Similar results were noted for access (32 [67%]), continuity (29 [60%]), and communication (25 [52%]) (Figure). When extrapolated to the entire VHA primary care population of 5.4 million patients, 310 468 additional high-quality care services could have been delivered if all clinics performed similarly to high-quartile clinics for care coordination. We calculated similar potential effects on quality metrics for access (n = 258 999), continuity (n = 253 816), and communication (n = 285 193).
Figure. Percentage of 48 Quality Indicators Associated With Significantly Better Performance in Highest-Quartile Clinics Compared With Lowest-Quartile Clinics (N = 909 Clinics).
PACT indicates Patient Aligned Care Team.
Discussion
Although all components of the PCMH model contributed to better performance on clinical quality indicators, those with the strongest association were care coordination, continuity, access, and communication. When we applied the probabilities to the full primary care population, substantially more high-quality care services would have been delivered if adoption of PACT at all clinics was commensurate with the high-quartile clinics. If these differences were sustained over time, the health benefits accruing to the population would be sizable. The strengths of our study include a broad range of process and outcome clinical quality measures for a large and diverse patient population served by primary care clinics varying in size and geographic location.
Limitations
This study has several limitations. This was an associational study that does not permit causal inference, and confounding cannot be excluded. Clinical quality at baseline was high, potentially obscuring improvements attributable to PCMH components.
Conclusions
We found that higher performance on each Pi2 component favored improved clinical quality. This was especially true for continuity, access, care coordination, and communication, which are hallmarks of effective primary care practice. Initiatives to improve primary care should focus on these important domains.
References
- 1.Jackson GL, Powers BJ, Chatterjee R, et al. Improving patient care: the patient centered medical home: a systematic review. Ann Intern Med. 2013;158(3):169-178. [DOI] [PubMed] [Google Scholar]
- 2.Shi L, Lock DC, Lee DC, et al. Patient-centered medical home capability and clinical performance in HRSA-supported health centers. Med Care. 2015;53(5):389-395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goulet JL, Erdos J, Kancir S, et al. Measuring performance directly using the Veterans Health Administration electronic medical record: a comparison with external peer review. Med Care. 2007;45(1):73-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nelson KM, Helfrich C, Sun H, et al. Implementation of the patient-centered medical home in the Veterans Health Administration: associations with patient satisfaction, quality of care, staff burnout, and hospital and emergency department use. JAMA Intern Med. 2014;174(8):1350-1358. [DOI] [PubMed] [Google Scholar]
- 5.Das A, Poole WK, Bada HS. A repeated measures approach for simultaneous modeling of multiple neurobehavioral outcomes in newborns exposed to cocaine in utero. Am J Epidemiol. 2004;159(9):891-899. [DOI] [PubMed] [Google Scholar]
- 6.Liang K-Y, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73(1):13-22. [Google Scholar]