Abstract
This study analyzes a newly released government survey examining Medicaid beneficiaries’ experiences with and opinions of the Medicaid program.
In the current debate over the Affordable Care Act (ACA), some policymakers have argued that Medicaid is a broken program that provides enrollees with inadequate access to physicians. While numerous studies demonstrate that Medicaid increases access to care,1,2 the literature has less frequently focused on patient satisfaction among Medicaid enrollees themselves. We analyzed a newly released government survey examining Medicaid beneficiaries’ experiences in the program.
Methods
We used the first-ever national Medicaid Consumer Assessment of Healthcare Providers and System (CAHPS) survey (n = 272 679), administered by the Centers for Medicare and Medicaid Services (CMS) in 46 states and Washington, DC.3 From December 2014 to July 2015, CMS sampled 4 groups of adults enrolled in Medicaid as of fall 2013: (1) people with disabilities, (2) individuals dually enrolled in Medicaid and Medicare, (3) nondisabled adults in managed care, and (4) nondisabled adults in fee-for-service medical care; the response rate was 23.6%. Our primary outcome was respondents’ overall health care rating, ranging from 0 for “the worst health care possible” to 10 for “the best health care possible.” Additional outcomes were (1) ability to get needed care in the last 6 months, and if not, why; and (2) whether respondents had a usual source of care other than the emergency department, and if not, why.
We calculated survey-weighted means or proportions for each outcome (item nonresponse rates ranged from 3.3%-7.7%). We stratified our primary outcome by age, race, sex, eligibility group, and state Medicaid expansion status. All results were estimated using CMS-designed survey weights to account for nonresponse and produce nationally representative estimates. This study was deemed non–human participants research and thus exempt from review by the Harvard T.H. Chan School of Public Health’s institutional review board.
Results
Medicaid enrollees gave their overall health care an average rating of 7.9 on a 0 to 10 scale (Figure). Forty-six percent gave their Medicaid coverage a score of 9 or 10, while only 7.6% gave scores under 5. Ratings were similar in Medicaid expansion and nonexpansion states (7.8 vs 7.9; P = .34). Ratings were slightly higher for older adults and dual-eligible beneficiaries, but similar in the fee-for-service and managed-care groups. Overall, ratings ranged from 7.6 to 8.3 across all demographic groups (Table).
Figure. Medicaid Enrollees’ Overall Health Care Satisfaction Ratings, 2014-2015.
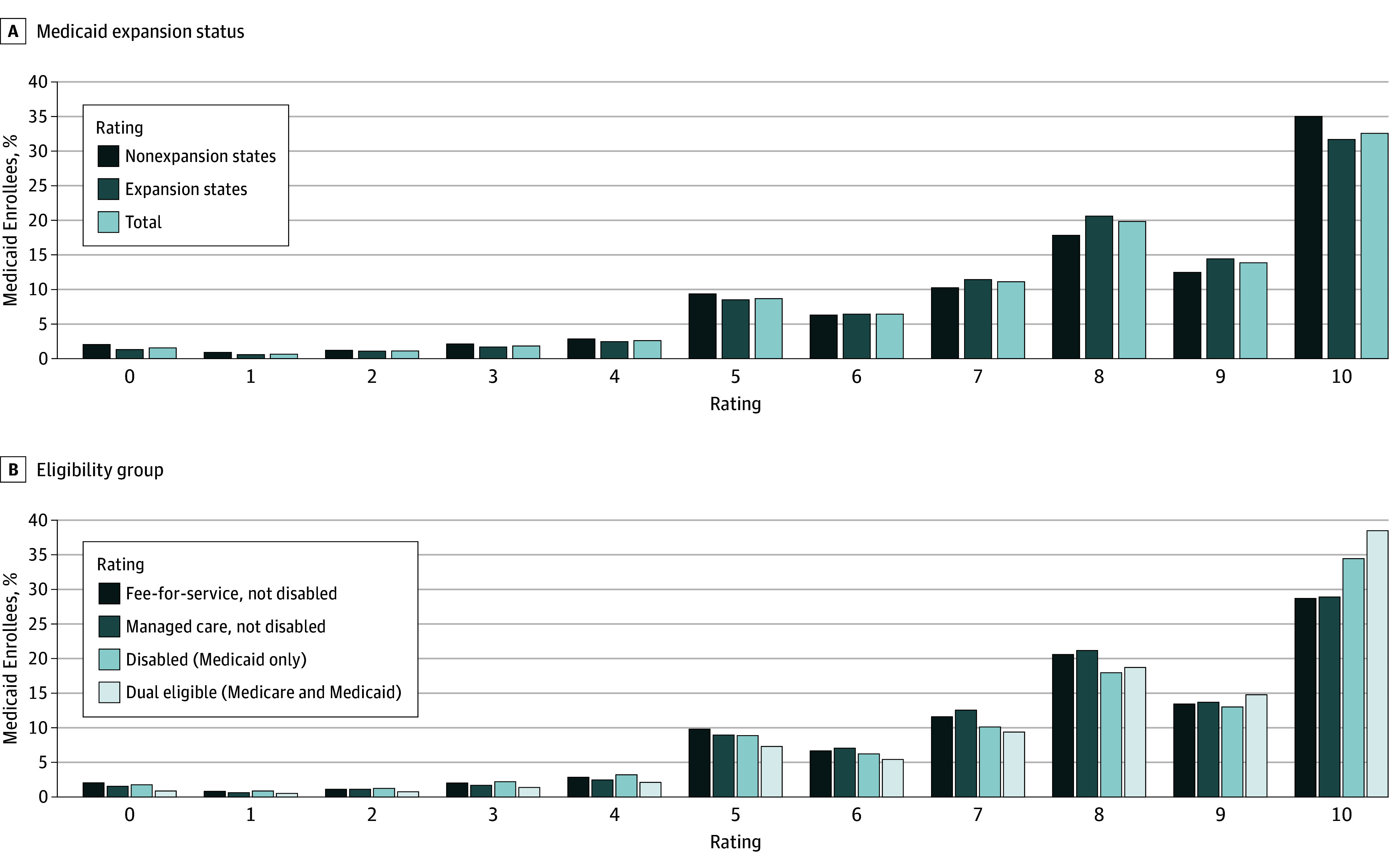
Data are from the National Medicaid CAHPS survey administered by the Centers for Medicare and Medicaid Services (CMS) to Medicaid enrollees in 46 states and Washington, DC3 (n = 108 645 in nonexpansion states, and n = 164 034 in expansion states, excluding item nonresponse). Ratings ranged from 0 to 10 for the question, “Using any number from 0 to 10, where 0 is the worst health care possible and 10 is the best health care possible, what number would you use to rate all your health care in the last 6 months?” All estimates use CMS survey weights to account for the sampling design of the CAHPS survey.
Table. Medicaid Beneficiaries’ Health Care Satisfaction Ratings and Physician Access by Demographic Subgroup, 2014-2015a.
| Group | Sample Proportion, Weighted % | Health Care Rating, 0-10, Mean (SE)b | Able to Get All Needed Care in Past 6 Months, % (SE)b | Has a Usual Source of Care, % (SE)b |
|---|---|---|---|---|
| Full sample | 100 | 7.9 (0.0) | 84.2 (0.5) | 83.4 (0.9) |
| Eligibility group | ||||
| Fee-for-service, not disabled | 19.8 | 7.7 (0.1) | 83.8 (1.0) | 77.5 (1.8) |
| Managed care, not disabled | 34.8 | 7.8 (0.1) | 84.6 (0.9) | 81.7 (1.6) |
| Disabled (Medicaid only) | 18.8 | 7.8 (0.1) | 80.2 (0.5) | 85.3 (0.7) |
| Dual eligible (Medicare and Medicaid) | 26.6 | 8.2 (0.0) | 86.9 (0.2) | 88.9 (0.3) |
| Between-groups P value | NA | <.001 | <.001 | <.001 |
| Medicaid expansion status, as of 2015 | ||||
| Nonexpansion state | 26.5 | 7.8 (0.1) | 81.5 (0.7) | 81.1 (1.6) |
| Expansion state | 73.5 | 7.9 (0.0) | 85.2 (0.5) | 84.2 (1.1) |
| Between-groups P value | NA | .34 | <.001 | .11 |
| Age, y | ||||
| 18-24 | 13.1 | 7.7 (0.1) | 86.7 (0.8) | 76.1 (1.8) |
| 25-34 | 18.2 | 7.7 (0.0) | 84.2 (0.9) | 80.9 (1.0) |
| 35-44 | 19.7 | 7.7 (0.0) | 82.8 (0.7) | 82.5 (1.2) |
| 45-54 | 14.6 | 7.8 (0.0) | 81.6 (0.7) | 84.9 (0.8) |
| 55-64 | 14.3 | 8.0 (0.0) | 82.1 (0.6) | 87.7 (0.5) |
| 65-74 | 8.9 | 8.3 (0.0) | 86.7 (0.5) | 88.2 (0.6) |
| ≥75 | 8.6 | 8.3 (0.0) | 89.7 (0.4) | 89.2 (0.4) |
| Unknown/refused | 2.6 | 7.7 (0.1) | 80.9 (1.0) | 75.9 (1.9) |
| Between-groups P value | NA | <.001 | <.001 | <.001 |
| Race/ethnicity | ||||
| White, non-Latino | 40.7 | 7.9 (0.0) | 84.1 (0.6) | 86.7 (0.6) |
| Black, non-Latino | 18.3 | 7.9 (0.0) | 83.7 (0.5) | 79.9 (0.9) |
| Latino | 24.1 | 8.0 (0.1) | 85.1 (0.7) | 80.8 (1.9) |
| Asian, non-Latino | 6.9 | 7.8 (0.1) | 88.7 (0.4) | 85.7 (1.5) |
| Other | 9.9 | 7.6 (0.0) | 79.9 (0.8) | 80.6 (1.2) |
| Between-groups P value | NA | <.001 | <.001 | <.001 |
| Sex | ||||
| Male | 35.0 | 7.9 (0.0) | 83.5 (0.6) | 84.3 (0.9) |
| Female | 62.9 | 7.9 (0.0) | 85.7 (0.5) | 82.1 (1.0) |
| Unknown/refused | 2.1 | 7.7 (0.1) | 80.2 (1.6) | 74.9 (2.1) |
| Between groups P value | NA | .27 | <.001 | <.001 |
Abbreviations: NA, not applicable; SE, standard error.
Data are from the National Medicaid Consumer Assessment of Healthcare Providers and System (CAHPS) survey administered to Medicaid beneficiaries in 46 states and Washington, DC (N = 272 679), minus item nonresponse for each outcome. All estimates use CAHPS survey weights. All P values in the table are from survey-weighted Wald tests of whether the subgroup means in each category are equal.
Standard errors were clustered by state and eligibility grouping.
For physician access, 84% of enrollees reported that they had been able to get all the care that they or their physician believed was necessary in the past 6 months, and 83% reported having a usual source of care. The mean percentage of beneficiaries able to get all needed care was significantly higher in Medicaid expansion states than in nonexpansion states (85.2% vs 81.5%; P < .001). Overall, only 3% of enrollees reported not being able to get care because of waiting times or physicians not accepting their insurance. Two percent reported lacking a usual source of care because “no doctors take my insurance.”
Discussion
We found that Medicaid enrollees are generally satisfied with their coverage across multiple demographic groups and state expansion choices. Overall health care satisfaction in Medicaid was in a similar range, though slightly lower, than benchmarks from 2013 CAHPS surveys in other populations, including those with commercial insurance (50.9% with ratings of 9 or 10)4 and Medicare (8.6 mean satisfaction score).5 We are unaware of any CAHPS data for uninsured patients. We also found little evidence that low physician participation rates are a key barrier to care for most Medicaid enrollees, consistent with prior studies of access to care in Medicaid.1,2
While limited by its response rate and use of pre-ACA enrollment to define the sample, this data set offers important advantages. First, its sample was drawn from official Medicaid enrollment files, so it does not rely on often inaccurate self-reporting of insurance coverage as in other surveys.6 Second, it has a much larger sample size of Medicaid enrollees than many similar surveys.
In summary, we found that Medicaid enrollees are largely satisfied with their care, and that few perceive their insurance as a major barrier to care. Changes to Medicaid that would result in millions of beneficiaries losing coverage could have major adverse effects.
References
- 1.Sommers BD, Blendon RJ, Orav EJ, Epstein AM. Changes in utilization and health among low-income adults after Medicaid expansion or expanded private insurance. JAMA Intern Med. 2016;176(10):1501-1509. [DOI] [PubMed] [Google Scholar]
- 2.Baicker K, Taubman SL, Allen HL, et al. ; Oregon Health Study Group . The Oregon experiment: effects of Medicaid on clinical outcomes. N Engl J Med. 2013;368(18):1713-1722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.NORC at the University of Chicago . Nationwide Adult Medicaid CAHPS. http://www.norc.org/Research/Projects/Pages/nationwide-adult-medicaid-cahps.aspx. Accessed May 7, 2017.
- 4.Onstad K, Khan A, Hart A, et al. Final report: benchmarks for Medicaid adult health care quality measures. 2014. https://www.medicaid.gov/medicaid/quality-of-care/downloads/adultbenchmarkreport.pdf. Accessed May 23, 2017.
- 5.McWilliams JM, Landon BE, Chernew ME, Zaslavsky AM. Changes in patients’ experiences in Medicare Accountable Care Organizations. N Engl J Med. 2014;371(18):1715-1724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pascale J, Call KT, Fertig A, Oellerich D. Validating self-reported health insurance coverage: preliminary results on CPS and ACS. US Census Bureau. https://www.census.gov/newsroom/blogs/research-matters/2016/05/validating-self-reported-health-insurance-coverage-preliminary-results-on-cps-and-acs.html. Accessed May 8, 2017.


