Abstract
Background
Self-management education is critical to the development of successful health behavior changes related to chronic illness. However, people in high-risk groups attend less frequently or benefit less from patient education programs than do people with more socioeconomic advantages.
Aim
The aim was to test the feasibility of a participatory person-centered education approach and tool-kit targeting self-management of chronic illness in hardly reached people.
Methods
After participating in a training program, educators (n=77) tested the approach in practice. Data collection included online questionnaires for educators (n=65), observations of education sessions (n=7), and interviews with educators (n=11) and participants (n=22). Descriptive statistics were calculated. Transcripts of interviews and observations were analyzed using systematic text condensation. Feasibility was examined in terms of practicality, integration, suitability, and efficacy.
Results
Educators had a positive response to the approach and found that the tools supported involving participants in education and support. Participant satisfaction varied, depending on the ability of educators to integrate the tools into programs in a meaningful way. The tools provided time for reflection in the education process that benefited participants and educators alike. Educators found it challenging to allow participants to help set the agenda and to exchange experiences without educator control. Barriers to use reported by educators included lack of time for both training and preparation.
Limitations
The testing included varied groups of participants, some groups included members of hardly reached populations and others did not. Also, some tools were only tried in practice by a few educators.
Conclusion
The approach was feasible in terms of practicality, integration, acceptability, and efficacy and perceived by educators as suitable for both hardly reached participants and those who are less disadvantaged. Implementation of the approach requires time for training and preparation.
Keywords: health care educators, professional development, skills, vulnerable patients, support, participatory, dialogue tools, tool kit
Introduction
Chronic illnesses, such as diabetes, heart disease, and chronic obstructive pulmonary disease, are characterized by a large day-to-day self-management burden.1,2 Successful disease management often requires sustained behavior change and new skills to handle medication, undertake preventive actions, self-monitor, and cope with the emotional consequences of disease.2–4 Self-management education and support is critical to the development of successful health behavior changes related to a chronic illness like type 2 diabetes (T2D).3,5–8 Self-management education is beneficial for disease knowledge, self-management, self-efficacy, and health status.9,10 Patients also experience improved mood and less depressive symptoms when self-management education and support address psychological well-being.2
People with lower socioeconomic status experience more chronic illness and premature mortality than those in higher socioeconomic groups.11–15 People with lower income and less education are two to four times more likely to develop T2D than are more advantaged individuals, and income and education are important determinants of T2D complications and mortality.13,14 In addition, health-related behaviors are strongly influenced by social factors such as income, education, and employment.15
Consequently, it is critical to offer structured self-management education and support to people with chronic illness, including those in high-risk groups defined by socioeconomic disadvantages. However, people in high-risk groups are sometimes referred to as “hardly reached” because they attend patient education programs less frequently than do people with more socioeconomic advantages.16 As suggested by Fisher et al,17 the term “hardly reached” emphasizes that the problem lies in the frequent failure of interventions, health care systems, and providers to engage these individuals, rather than in their personal characteristics.
To address barriers to participation in education and support among members of disadvantaged groups, we developed a research-based, participatory, person-centered education approach and tool kit targeting self-management of chronic illness in hardly reached people (PEASCI).18–20 PEASCI was developed for use in individual and group-based patient education and support. The foundation of PEASCI is nine dialogue tools; its core purpose is to, 1) support participation of hardly reached people with chronic illness in patient education by enhancing self-reflection and dialogue among participants and between participants and educators; and 2) to inspire and support educators in providing person-centered education and support based on the individual needs and challenges of vulnerable participants with chronic illness.
Aim
The aim of this study was to investigate the feasibility of using PEASCI in patient education and support for hardly reached patients. Inspired by definitions formulated by Bowen et al,21 we examined four aspects of feasibility: practicality, integration, acceptability, and limited efficacy. We investigated four related questions: 1) to what extent can PEASCI be carried out and successfully delivered to intended participants using existing resources and circumstances?; 2) to what extent can PEASCI be integrated within an existing structured education program?; 3) how do educators and participants respond to PEASCI?; and 4) to what extent were the intended effects of PEASCI achieved in practice?
Methods
The self-management education approach and tool kit (PEASCI)
The first phase of PEASCI’s development consisted of a needs assessment among hardly reached people with diabetes and a study of educator challenges and needs related to working with hardly reached people with chronic illness.18–20 The theoretical framework for data collection and analysis consisted of two health education models, “The Balancing Person” and “The Health Education Juggler”.22,23 The Balancing Person describes challenges and education needs of people diagnosed with chronic illness. The Health Education Juggler describes four roles educators need to continuously juggle in group-based education to provide person-centered education and support for people with chronic illness. A refined model of The Balancing Person, which includes circumstances that may influence how vulnerable people participate in health education programs, emerged from these studies (Figure 1). In hardly reached people, individual circumstances include varying predisposing factors and behavioral characteristics that educators often find difficult to manage effectively.18–20
Figure 1.

“The Vulnerable Person” model.
Notes: The two outer circles represent “The Balancing Person” model, encompassing challenges and needs of patients with chronic illness in relation to health education.22 The two inner circles represent additional influences on participation and behavior in health education sessions.20 Predisposing factors include attitudes and skills such as acceptance of disease and the need to participate in patient education, literacy, learning disabilities, preferences for structure, capacity for self-reflection, and ability to think abstractly and verbalize needs and experiences. Varying behavior characteristics include reluctance, quiet, and shy behavior, or hyperactive, very talkative, and dominating behavior.19
Using design thinking methodology, we identified five design principles and five overall objectives guiding the development of PEASCI (Table 1).18,19,24 We focused on developing tools that facilitate an appreciative attitude, can be adapted to participants’ varying cognitive preferences and capacities, and foster positive group dynamics. PEASCI consists of two elements: nine patient education dialogue tools and a guidebook for educators.20 The guidebook introduces the overall approach, including a description of the theoretical background. It also provides general recommendations for structural frameworks, such as small group work, and initiatives to promote the inclusion and continuous participation of hardly reached people, for example, structures to support networking among participants. Finally, step-by-step guides suggest how to apply the dialogue tools in practice. Table 2 provides an overview of the dialogue tools, and Figure 2 provides two examples of tools. Dialogue tools and a guidebook are available online at no cost.20
Table 1.
Design principles and overall objectives guiding the development of PEASCI
| Design principles | Overall objectives |
|---|---|
| Flexibility in using the dialogue tools | Setting the scene – building safe environments for participation |
| Simplicity in structure | Support for achieving physical and mental well-being |
| Appreciative approach | Clarification of and support for strengthening relationships |
| Concrete expression | Generation of knowledge based on participants’ needs |
| Appealing to a broad target group | Promotion of motivation and action competence – goal setting and action planning |
Abbreviation: PEASCI, person-centered education approach and tool kit targeting self-management of chronic illness.
Table 2.
Overview of dialogue tools
| Tool name | Overall objective | Purpose | Idea |
|---|---|---|---|
| My Day | Safe environment, relationship development, knowledge, and motivation | To help participants feel acknowledged and allow the educator to gain valuable insights about the participants | Participants describe a typical day with their own focus and interests |
| Check-in | Setting the scene, well-being | To help participants settle in/get grounded in the course | In an exercise inspired by mindfulness, participants are invited to spend 5 minutes in mindful relaxation on arrival |
| Our Rules | Safe environment, relationships | To get participants actively engaged and responsible for education processes and a trustworthy environment | Participants use brainstorming to set common rules for teaching and social interaction |
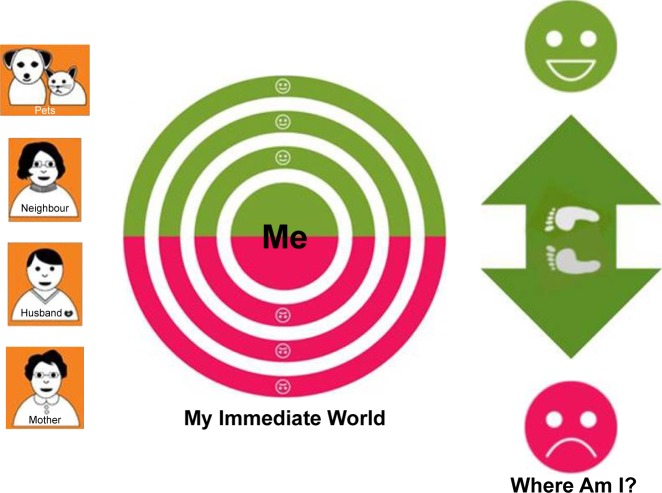
| My Immediate World | Relationships, knowledge, motivation, and action competence | To create an overview of help and support provided by family and friends and to discuss opportunities for change | Participants are invited to place relatives on a board based on whether the relationship is good or bad and how close it is |
| My Contact with Healthcare Professionals | Relationships, knowledge, motivation, and action competence | To get an overview of support and advice provided by health care providers and discuss opportunities for change | Participants are invited to place health care providers on a board based on whether the relationship is good or bad and how important it is |
| Fact or Fiction | Safe environment, knowledge | To facilitate discussion of knowledge and mutual learning among participants and to support educators in “sweet-spot” education | Participants discuss whether statements provided by educators are true or false |
| Where Am I? | Safe environment, motivation, and goals and plan | To help participants gain a body-based understanding of where they are and where they would like to be in relation to a specific topic | Participants are invited to place themselves between images of happy and frowning faces on the floor and to talk to other participants and/or educators about their present situation and desire for change |
| We’re on the Way | Safe environment, motivation, and goals and plan | To use a game framework to work in an informal way on own goals in an open process with focus on strengths and successes and provide participants with the opportunity to inspire each other | Participants take turns drawing cards inviting them to, 1) reflect back on something positive, 2) look ahead to desired change, and 3) reflect on what the first step could be. Includes a brainstorm process among participants about ways to achieve desired changes |
| Check-out | Well-being and motivation | Closure and reflection on what to take home from session | In an exercise inspired by mindfulness, participants are invited to spend 6 minutes in mindful relaxation at the end of a session |
Figure 2.
Examples of PEASCI dialogue tools.
Notes: My Immediate World consists of a red/green tablecloth and cards with icons of personal relationships. Participants are invited to arrange specific relevant relationships on the cloth in the red (bad or unhealthy) or green (good or healthy) area of the tablecloth while showing how close the relationship is by the distance to “Me”. The tool facilitates reflection on positive and negative experiences of support and addresses whether participants receive or reject support. It also enables discussion about opportunities for improving their social network. Where Am I? consists of a red frowning face representing dissatisfaction and a green smiling face representing satisfaction that are placed on the floor several feet apart. Participants are invited to stand between the two faces in a location that shows their current level of satisfaction and then to move to a spot that reflects their desired satisfaction in relation to a specific topic (eg, eating a healthy diet). The tool helps participants express their desire for change by using their body as well as their voice and provides an opportunity to talk to people in similar situations.
Abbreviation: PEASCI, person-centered education approach and tool kit targeting self-management of chronic illness.
Data collection and participants
Data on the feasibility of PEASCI were collected from April to June 2014 using a web-based questionnaire, observations of education sessions, and interviews with educators and participants. The primary study participants were educators in the Region of Southern Denmark providing education and support to individuals with chronic disease and low socioeconomic status.
Educators were recruited for the feasibility study if they signed up for a 1½-day professional development course on PEASCI. The course was developed in collaboration with, and conducted by, professional educators from University College Southern Denmark. They were invited to participate in the course by direct mail to the 22 municipalities and four hospitals in the Region of Southern Denmark and invitations posted on the region’s official websites. Four courses were conducted; 20 educators enrolled at each course, where they were introduced to PEASCI and trained to use the dialogue tools. Time allowed for training on five of the nine tools during the first day of the course. We asked educators to apply the dialogue tools in their own practices over the following 6 weeks. At the end of 6 weeks, a half-day session followed up on initial training and the application of the tools; we asked educators to complete a brief course evaluation on site.
Secondary study participants were individuals with chronic illness participating in programs led by educators who had enrolled in the courses about PEASCI; participants were referred to the programs by their general practitioners. Participants of the observed programs were invited onsite to take part in interviews about the program; those who volunteered were all interviewed. Written informed consent was obtained from all study participants.
Survey
Approximately 2 weeks after the second day of the course, a web-based questionnaire was emailed to all participating educators. Nonrespondents received two reminders. The questionnaire consisted of two sections: 1) general questions about professional background, experience as a patient educator, and experience with barriers to using the tools and with patient education approaches; and 2) questions specific to PEASCI, including experiences with each tool, details about the practice setting and use of tools, and the extent to which the design principles and the purpose of the dialogue tools were realized in practice. A five-point Likert scale was used for the section pertaining to PEASCI. Questions regarding application of the design principles in practice pertained to all tools, whereas most questions regarding the application of objectives and purpose were tool-specific.
Observations and interviews
During the 6-week interval between the first and second sessions of the professional development course, we observed educators as they applied the tools in practice and completed follow-up interviews with educators and participants. Observations and interviews were conducted in the practice settings of educators who agreed to participate in the study immediately after educational sessions. One or two authors (ARV and THA) observed patient education sessions, positioning themselves in the room as discreetly as possible. Observers took notes, augmented by complete video recordings that were reviewed and transcribed verbatim.
Interviews focused on educator and participant experiences with PEASCI, using a semistructured interview guide. Educators and participants were first asked for general reflections on the observed education session, followed by a set of questions about the dialogue tools applied in the session. All interviews were audio recorded and transcribed verbatim. The study was carried out in accordance with The Code of Ethics of the Declaration of Helsinki. In accordance with the policy on health research (section 1, part 4) the present study did not require an ethical approval from the Regional Committee, VEK (Capital Region of Denmark).
Data analysis
Data from observations and interviews were analyzed using systematic text condensation.25 The analysis was guided by a framework for feasibility studies from Bowen et al.21 We focused on data about four aspects of feasibility: practicality, integration, acceptability, and efficacy. However, throughout the data analysis, we were open to emerging themes not captured by these categories.
Descriptive statistics from the survey were generated using SurveyXact. After excluding “don’t know/not relevant” responses, we calculated mean values for educator ratings of each tool in terms of applying the design principles, objectives, and purpose in practice. Survey results were analyzed using the feasibility framework and linked to relevant themes emerging from the qualitative analysis, with the exception of efficacy. Efficacy refers to intended effects and, in our study, related to the way overall objectives and purposes of individual tools could be applied in practice. For three tools, Our Rules, My Immediate World, and Where Am I?, survey data were substantiated by data from interviews and observations.
Results
Educators, participants, and use of PEASCI
Of 80 educators from the Region of Southern Denmark who signed up for the professional development course, 77 (96%) completed the course and 66 (83%) completed the brief course evaluation. Most educators were satisfied with the course content and delivery (data not shown). They highlighted the importance of practicing the new approaches and tools before applying them in practice with patients. Although most educators were satisfied with the schedule of the professional development course, some felt that there was too little time to practice and discuss the approach during the course. Some would have preferred all nine tools to be introduced and practiced.
Sixty-five (84%) of 77 educators completing the course also completed the web-based questionnaire (Table S1). Use of each tool and contexts in which educators applied the tools are provided in Table S2. We observed seven education sessions in seven unique settings with a total of 42 participants and conducted eight interviews with 11 educators (individually or in pairs) and nine interviews with a total of 22 patients (two individual interviews and seven interviews in groups of two to six participants). Observations lasted an average of 67 minutes (range, 24–194), and interviews lasted an average of 31 minutes (range, 11–46) and 20 minutes (range, 8–45) with educators and participants, respectively.
Practicality
We examined the extent to which PEASCI could be successfully delivered using existing resources and circumstances. Qualitative data from interviews with educators revealed two themes related to practicality: educator competencies and issues related to time.
PEASCI was consistently useful to experienced and inexperienced educators in various contexts regardless of the composition of the staff group. One educator noted that she gained a great deal of knowledge by being introduced to PEASCI. Educators who introduced the tool to participants by role-playing or felt more comfortable having more resources to assist the group identified advantages to having two educators in the sessions. Educators also emphasized the importance of practicing with the tools before the education session; several mentioned that they had used the tools for training purposes with colleagues and family members.
Educators needed time to prepare for introducing the tools and planning the education session. They emphasized the importance of having time and support to discuss and practice using the tools with colleagues. Interviewed educators had these opportunities, but as reported in the survey, they often did not occur across all patient education settings. Barriers to using PEASCI most frequently reported by educators were lack of training for using tools (25, 39%), lack of time to prepare for education sessions incorporating the new tools (23, 35%), and poor fit between the tools and planned educational sessions (19, 29%). In addition, 20 respondents (15%) were unable to discuss using the tools with colleagues. Six (9%) educators reported no barriers.
Integration
Two themes related to the integration of PEASCI emerged from interviews with educators and participants: matching and plasticity.
In many circumstances, educators successfully matched dialogue tools to existing activities. They reported that PEASCI included tools with different purposes and topics that were relevant to their education activities. They used the tools to vary education styles, add more practice-oriented work, maintain a consistent thread throughout education sessions, and support working with difficult issues such as relationships, sleep, and changing maladaptive habits. However, in some situations, matching the dialogue tools to existing education was not successful for educators or participants. Participants did not consider the tool relevant, thought that educators spent too much time on it, or both; they became impatient. In general, educators emphasized that effectively applying new approaches and tools in existing activities requires familiarity with the approach, which necessitates time and resources. As noted earlier, 29% of surveyed educators did not think that the dialogue tools could fit into their education sessions during the 6-week application period.
In terms of plasticity, educators emphasized that the dialogue tools could be combined in different ways and adjusted for different settings and participants in terms of available time, space, number of participants, and level of knowledge. In some cases, educators only used parts of the dialogue tools, which worked well. Surveyed educators responded that the tools generally applied the design principle of flexibility to a high degree (Table 3). However, substantial variations among ratings for individual tools were observed.
Table 3.
Educator assessment of PEASCI tools
| My Day | Check-in | Our Rules | My Immediate World | My Contact with HCPs | Fact or Fiction | Where Am I? | We’re On the Way | Check-out | Mean | |
|---|---|---|---|---|---|---|---|---|---|---|
| Design principles | ||||||||||
| Flexibility of use | ||||||||||
| Useful for both individual and group sessions | 3.2 | 4.2 | 3.7 | 4.3 | 3.6 | 3.7 | 4.3 | 3.4 | 4.1 | 3.8 |
| Useful in different situations | 4.0 | 4.0 | 3.7 | 4.2 | 3.8 | 4.2 | 4.4 | 3.9 | 4.2 | 4.0 |
| Useful with different themes | 3.4 | 4.3 | 3.8 | 4.2 | 4.0 | 4.1 | 4.4 | 3.8 | 4.5 | 4.1 |
| Useful in situations of varying difficulty | 3.0 | 3.6 | 3.3 | 4.2 | 3.8 | 4.2 | 4.0 | 3.3 | 3.9 | 3.7 |
| Simplicity of structure | ||||||||||
| Easy to explain | 4.6 | 4.3 | 3.7 | 3.9 | 3.6 | 4.4 | 3.7 | 3.0 | 4.5 | 4.0 |
| Easy to understand | 4.3 | 4.4 | 3.9 | 3.9 | 3.6 | 4.2 | 3.9 | 3.0 | 4.4 | 4.0 |
| Has a clear objective | 4.0 | 4.3 | 4.4 | 4.2 | 3.8 | 4.2 | 4.0 | 3.3 | 4.3 | 4.1 |
| Concrete and specific | 4.3 | 4.3 | 3.7 | 4.1 | 3.8 | 4.3 | 3.5 | 3.1 | 4.1 | 3.9 |
| Reader friendly | 4.5 | 4.5 | 4.1 | 4.1 | 3.8 | 4.5 | 3.9 | 3.8 | 4.6 | 4.2 |
| Appreciative approach | ||||||||||
| Is supporting and affirmative | 3.7 | 3.7 | 3.8 | 3.9 | 3.8 | 4.3 | 3.8 | 4.0 | 4.0 | 3.9 |
| Is reliable and creates trust | 4.0 | 4.1 | 3.7 | 3.8 | 3.8 | 3.4 | 3.4 | 3.8 | 3.9 | 3.8 |
| Is humorous and creates hope | 2.4 | 2.3 | 3.4 | 3.5 | 3.2 | 3.4 | 3.6 | 3.7 | 3.2 | 3.2 |
| Focuses on success and is motivating | 3.3 | 2.8 | 3.2 | 3.8 | 3.6 | 3.4 | 3.8 | 4.1 | 3.5 | 3.5 |
| Concrete expression | ||||||||||
| Takes different learning styles into account | 3.0 | 2.6 | 3.0 | 3.8 | 3.6 | 3.4 | 3.8 | 4.0 | 3.2 | 3.4 |
| Provides visual, tactile, kinesthetic, and auditory stimulation | 3.2 | 3.2 | 3.1 | 3.9 | 3.4 | 2.6 | 4.0 | 4.0 | 3.7 | 3.5 |
| Focuses on practice | 2.8 | 3.6 | 3.4 | 4.1 | 3.6 | 2.9 | 4.1 | 3.9 | 3.8 | 3.6 |
| Tangible | 4.3 | 4.1 | 3.9 | 4.2 | 3.6 | 3.9 | 4.0 | 3.6 | 4.1 | 4.0 |
| Mean | 3.6 | 3.8 | 3.6 | 4.0 | 3.7 | 3.8 | 3.9 | 3.6 | 4.0 | 3.8 |
| Overall objective and purpose of tool | ||||||||||
| Safe environment | ||||||||||
| Supports creation of a trustworthy environment | 3.8 | 4.0 | 4.3 | – | – | – | – | – | – | 4.0 |
| Supports the educator’s contact with participants | 4.0 | 4.2 | 3.8 | – | – | – | – | – | – | 4.0 |
| Supports contact and trust between participants | – | – | 3.9 | 3.7 | 3.0 | 3.1 | 3.4 | 3.6 | – | 3.5 |
| Reflection, participation, and dialogue | ||||||||||
| Facilitates reflection | 4.2 | – | 3.8 | 4.2 | 4.2 | 4.2 | 4.5 | 4.0 | 4.0 | 4.1 |
| Creates dialogue | 4.3 | – | 3.9 | 4.1 | 4.2 | 4.3 | 4.2 | 4.3 | – | 4.2 |
| Creates participation | 4.3 | 3.5 | 4.0 | 4.2 | 4.2 | 4.1 | 4.3 | 4.0 | 3.7 | 4.0 |
| Supports articulation of individual participants’ needs and wishes | 3.8 | – | 3.8 | 3.8 | 4.2 | – | 4.3 | 4.0 | – | 4.0 |
| Stimulates sharing of experiences between participants | – | – | 3.5 | 3.9 | 4.5 | 3.8 | 3.9 | 4.0 | – | 3.9 |
| Relationships | ||||||||||
| Supports clarifying participants’ relationships | 3.3 | – | 2.6 | 4.7 | 4.4 | – | – | – | – | 3.8 |
| Supports improving participants’ relationships | – | – | – | 4.5 | 4.2 | – | – | – | – | 4.4 |
| Knowledge, motivation, and action competence | ||||||||||
| Supports knowledge sharing on participants’ premises | 2.8 | – | – | 3.8 | 3.3 | 4.1 | – | – | – | 3.5 |
| Facilitates development of action competence of individual participants | – | – | – | 3.6 | 3.8 | 3.2 | 3.8 | 3.8 | – | 3.6 |
| Helps motivate participants to set goals for change and actions | 3.7 | – | – | – | – | – | 4.1 | 4.0 | 3.3 | 3.8 |
| Facilitates identification of individual participants’ need for support for action | – | – | – | 3.9 | 4.0 | – | 3.8 | 3.8 | – | 3.9 |
| Is suitable for “hardly reached” participants | 4.2 | 4.0 | 3.6 | 3.9 | 4.0 | 3.6 | 3.4 | 3.7 | 3.9 | 3.8 |
| Is suitable for other participants than “hardly reached” | 3.5 | 4.1 | 3.8 | 4.1 | 4.3 | 4.0 | 4.2 | 3.8 | 4.3 | 4.0 |
| Mean | 3.8 | 4.0 | 3.7 | 4.0 | 4.0 | 3.8 | 4.0 | 3.9 | 3.8 | 3.9 |
Note: Items were scored on a 5-point scale from 1 (not at all) to 5 (to a great extent).
Abbreviations: HCPs, health care professionals; PEASCI, person-centered education approach and tool kit targeting self-management of chronic illness.
Acceptability
Two themes related to acceptability emerged from interviews and our observations of educator and participant responses to PEASCI: odd or childish characteristics of tools and “leaving the stage”.
Some educators expressed uncertainty as to whether patients would find the dialogue tools too childish or odd because they were very colorful and tangible. However, most participants valued the colorful materials. Participants also found it helpful that the tools stimulated different learning styles, such as visual and tactile (eg, My Immediate World) and kinesthetic (eg, Where Am I?). One participant mentioned that she liked to metaphorically “move her relatives around” on the table (My Immediate World). Participants felt that time passed quickly during the sessions when they were actively involved. Although their preferences varied, participants were generally open to using the new tools if the purpose made sense. Educator ratings of the degree to which individual tools reflected the design principle of concrete expression were generally in the mid-range of possible scores (Table 3).
“Leaving the stage” refers to the patient-centered focus of PEASCI. In general, educators aimed to get new perspectives on the education process and engage participants more actively. However, interviews and observations revealed that they were ambivalent about allowing participants to actually take the center stage in patient education. Although educators reported that the tools facilitated their objective of involving participants more, some also expressed insecurity about the process of doing so. One educator was uncomfortable with not knowing what participants talked about in smaller groups: “I feel that it is out of my hands when I use the new tools.” Another educator mentioned that she had difficulty conveying knowledge while using the tools to the same extent as she did while using her previous processes. However, participants generally valued being involved and engaged and talking in groups or pairs as long as the activity felt relevant to them.
During observations, we noted that educators often seemed excited or nervous when introducing the tools to participants, and these introductions were frequently unclear and unstructured. However, in most cases, participants seemed to understand what to do or chose to engage in the activity and address questions and uncertainties as they arose. We did not observe participants being unwilling to use the tools, and only a few participants were not actively engaged in sessions in which tools were applied. Surveyed educators reported that most of the tools had a clear objective and were easy to understand and to explain (Table 3).
Efficacy
We examined efficacy in terms of the extent to which the intended effects (ie, intermediate outcomes) of PEASCI were achieved. This was done by evaluating the extent to which the overall objectives and purposes of the individual tools were realized in practice. Mean survey scores for general features like “facilitation of reflection”, “creation of dialogue”, “creation of participation”, “suitability for hardly reached”, and “suitability for other than hardly reached participants” were 3.8–4.2 (Table 3). Other features were dependent on the objective and purpose of the individual tool.
Table 4 presents outcomes from different perspectives in relation to Our Rules, My Immediate World, and Where Am I? Educator ratings of all three tools on features that were relevant to an individual tool’s objective and purpose ranged from 3.4 to 4.7, with a single exception, and average educator ratings of features that were relevant to objective and purpose of these tools were 3.7–4.0. In general, interviews with educators supported these positive ratings. However, interviews with participants and observations provided a more nuanced picture. Even though many positive views were expressed, a few participants found that some of the tools were not appropriate or useful (Table 4).
Table 4.
Efficacy of Our Rules, My Immediate World, and Where Am I?
| Interviews | Observations | Participant interview quotes | Tool-specific survey ratings |
|---|---|---|---|
| Our Rules | |||
| Educators reported that this tool supported a friendly tone during education sessions, an open approach, room for everybody, and a relaxed atmosphere Participants emphasized that too much time was spent on this tool, but they also valued getting to know each other and being involved in formulating rules for their education sessions |
A participant expressed difficulty in participating in education sessions requiring too much of her, eg, to speak up in the group. This was then formulated as a rule: All participants should feel OK with education activities Sessions using Our Rules gave rise to participation and dialogue, but many participants were initially reluctant |
“Well, the point is more like that you are involved in formulating (the rules), so you take part.” “So, you are on a par when you take part … that’s what I think.” | Supports creation of a trustworthy environment: 4.3 Supports educator’s contact with participants: 3.8 Supports creation of contact and trust between participants: 3.9 Supports articulation of individual participants’ needs and wishes: 3.8 |
| My Immediate World | |||
| Educators reported that the tool supported participants in feeling respected and being taken seriously, that it was helpful for them to talk to other peers and mirror one another, and that important perspectives emerged on their support from, for example, their general practitioner Participants liked to get together in pairs and talk about relatives. Most participants described the tool as very useful for reflecting on support from relatives and how they valued the educators One participant did not find it relevant at all and another participant found it difficult to talk about “changing roles at home” at an education session |
Moments occurred in which participants were emotionally touched Some participants took photos of the tool with their relatives in place |
“It was something like an eye opener afterwards …” “Using the tool made you think about relationships in a new way” |
Supports clarifying relationships: 4.7 Supports improving relationships: 4.5 Stimulates sharing of experiences between participants: 3.9 |
| Where Am I? | |||
| Educators reported that the tool promoted a lot of dialogue very quickly and that participants reflected on barriers and capabilities in relation to what they wanted to achieve One educator thought that moving around on the floor may cause increased commitment A participant found the tool interactive, engaging, and more participating. Another participant described the tool as prompting him to reflect on his own limitations and to be realistic regarding his desired achievements |
Some participants found the tool helpful and obtained new perspectives, but others did not get support to do things differently One educator ended the session by asking how participants experienced the tool. One participant mentioned that it facilitated reflection, and another described getting a guilty conscience because she wanted to do more than she had |
“… and then I can see where I want to go. I would like to go just halfway (towards the smiling face) in terms of getting to the swimming bath again …” | “Support articulation of needs and wishes”: 4.3 “Facilitate development of action competence of individual participants”: 3.8 “Help motivate participants to set goals for change”: 4.1 “Facilitate identification of individual participants’ need of support for action”: 3.8 |
Discussion
PEASCI was feasible in terms of practicality, integration, acceptability, and efficacy when investigated among educators and people with or at risk of developing chronic illness in a variety of settings. Educators generally viewed the approach positively and found that the tools supported involving participants in group education or individual consultations.
The overall purpose of PEASCI to support participation by enhancing reflection and dialogue was achieved. Other studies also emphasize the importance of involving participants in education and support sessions and the ability of dialogue tools and other interactive methods, such as storytelling and teach back, to enhance the involvement of participants.6,22,26–31 It may be especially critical that vulnerable or hardly reached participants are involved and engaged to receive the benefits of education and support programs.6,18,19,31
Educator skills at conducting participatory education and support also have an essential impact on outcomes.6,18,19,32,33 During interviews, participants expressed different views of PEASCI from enthusiastically positive to quite negative. When the tools made sense, the approach became a natural part of the education and participants liked it. However, on some occasions, the tools were incorporated into existing education in ways that participants did not find relevant. In addition, some educators had difficulty allowing participants to take the center stage. They felt uncertain about working in new ways, a challenge inherent in implementing any new approach. This may relate to educators’ lack of training and preparation time for using PEASCI, which were the biggest barriers to implementation: however, we note again that educators had only 6 weeks to practice, plan, and conduct sessions using PEASCI.
Observations revealed that educators often used the tools in highly planned ways, leaving little room to experiment with more patient-centered methods. During training courses and interviews, some educators wanted very specific instructions for using the tools and reported struggling with remaining flexible and open and adapting tools to participants, topics, and context. Studies highlight the importance of flexibility and tailoring in education approaches with hardly reached participants.17–19,30 Additionally, trusting relationships, peer support, and family and social support are important focus points in education and support for vulnerable people.17–19,30,33,34 These elements were included in PEASCI.18–20 Family support and social support were addressed in particular by the tool “My Immediate World” and gave rise to discussions of good and less good support. Earlier studies have identified family involvement to include both supportive and nonsupportive behaviors.35,36 The more resourceful participants (in terms of income) were more likely to report that their family members provided supportive behaviors.35 The study recommends health care providers assist patients in developing strategies to address nonsupportive family member behaviors, and for this purpose “My Immediate World” could be supportive. Furthermore, family members should be included in intervention studies in order to improve the diabetes-specific interaction with the person with diabetes and become more supportive. Also, family members’ challenges and needs should be investigated and addressed in self-management education. Finally, more research on the impact of diabetes on the family dynamics and function is needed.37
Using PEASCI, peer support can be facilitated by interactive group work for example by sharing reflections and experiences. The tools can also assist in creating trusting relationships among participants. Some Chronic Disease Self-Management Programs have used trained peers to conduct the education programs enabling provision of education sessions with the patient voice.38 That approach might also be interesting to apply in PEASCI; however, the importance of flexibility in using PEASCI might make the training of peers challenging as high professional skills are required to adapt the program individually. A combination of peers and professionals as educators might be a more innovative and effective way of conducting self-management education and should be considered in future studies.
Education sessions often involved a mixture of hardly reached and less disadvantaged participants. Consequently, PEASCI should be useful with both groups of participants. The education sessions we observed included participants with a range of characteristics, and educators generally reported that the tools were suitable for hardly reached and less disadvantaged participants. However, their ratings differed substantially across tools, which may reflect difficulty adapting some tools for use with groups comprising highly varying participants. Each tool was designed to address different learning styles, but that does not ensure that each tool is attractive to all participants. Education processes per se should be subject to attention in order to be an active part of learning for participants and, moreover, to enable the educators to adjust education to fit participants’ different preferences and individual processes.
Harrison et al39 identify the importance of balancing process and content in education. Educators must be able to juggle different roles (facilitator, translator, embracer, and initiator), as described in The Health Education Juggler model.23 However, juggling roles pose many challenges for educators, which was also the case in this study, emphasizing the need for professional development for educators.40
Study strengths include triangulation of data from survey, observations, and interviews with participants and educators. Observations and interviews with participants added many crucial insights to survey results and to ensuing discussions about how to involve hardly reached people in patient education. Another strength is the fact that the tools and training program are based on thorough studies of needs and challenges of hardly reached people with chronic illness and educator needs for training.18,19 In addition, the study included a variety of different settings and educators.
Limitations
A limitation of the study was that some tools were only used in practice by a few educators. An obvious reason for this could be educator preferences for using only tools they had been introduced to or practiced during the professional development course. Another limitation was that the testing of PEASCI included varied groups of participants. Some groups included or consisted exclusively of members of hardly reached populations and others did not include hardly reached participants. Thus, the results are more generalizable to mixed groups of participants than to hardly reached participants alone, which is more representative of real-life patient education. However, it should be highlighted that the results of this study are based on participants, who showed up for self-management education after referral from general practitioners. Participants may thus represent more resourceful members of hardly reached groups. Finally, the assessment of PEASCI did not include structural or organizational frameworks.20,31,34
Conclusion
PEASCI promoted interactive patient education involving hardly reached and less disadvantaged participants. Educators generally responded positively to PEASCI after implementing it in practice, while participants’ assessments varied. Key barriers to use for educators were lack of training and preparation time. Participant satisfaction was highly dependent on educators’ ability to integrate the tools into the existing education program in a meaningful way, that is, to create coherence between educational content and tools. Main challenges for educators were juggling roles and integrating attention to group dynamics into education sessions. In addition, many educators found it difficult to use the tools flexibly, to allow participants to help set the agenda, and to allow participants to exchange experiences without educator control. Finally, the tools provided time for reflection in the education process that greatly benefited participants and educators alike.
Implications for practice
Few effective methods and tools for education and support target hardly reached people with chronic illness. The patient-centered approach of PEASCI is feasible when training and supervision of educators is provided. However, implementing the approach in a way that is consistent with its objectives of facilitating involvement, respect, and simplicity requires time and training. Managerial support for time for training, preparation, and reflection is crucial. Future research should explore the effects of implementing PEASCI using patient-reported outcomes such as health behavior change and quality of life as well as motivation for engaging in self-management education. This could be addressed in a larger randomized controlled trial. Future research should also address methods for effectively recruiting hardly reached people for patient education programs.
Supplementary materials
Table S1.
Educators, participants, and settings
| Surveyed educators | Number (%) N=65 |
| Gender | |
| Female | 65 (100) |
| Professional backgrounda | |
| Nurse | 17 (26.2) |
| Physiotherapist | 31 (47.7) |
| Dietitian | 11 (16.9) |
| Other | 10 (15.4) |
| Work place | |
| Municipality | 61 (93.8) |
| Hospital | 3 (4.6) |
| General practice | 1 (1.5) |
| Years of experience as patient educator | |
| None | 8 (12.3) |
| 0–1 | 12 (18.5) |
| 1–2 | 5 (7.7) |
| 2–5 | 20 (30.8) |
| >5 | 20 (30.8) |
| Experience with a similar person-centered education programb | |
| To a large extent | 4 (6.2) |
| To some extent | 30 (46.2) |
| Observational experience | 14 (215) |
| Theoretical experience | 9 (13.8) |
| No knowledge | 8 (12.3) |
|
| |
| Observed patient education settings | Number (%) N=7 |
| Organizational setting | |
| Municipality | 5 (71.4) |
| Hospital | 1 (14.3) |
| General practice | 1 (14.3) |
| Dialogue tools appliedc | |
| My Day | 0 |
| Check-in | 0 |
| Our Rules | 2 (28.6) |
| My Immediate World | 2 (28.6) |
| My Contact with Healthcare Professionals | 0d |
| Fact or Fiction | 1 (14.3) |
| Where Am I? | 3 (42.9) |
| We’re on the Way | 0 |
| Check-out | 1 (14.3) |
| Education theme | |
| T2D | 3 (42.9) |
| Physical activity | 3 (42.9) |
| Other | 1 (14.3) |
| Target group for education | |
| People with T2D | 4 (57.1) |
| People with chronic illness of different kinds or CVD only | 2 (28.6) |
| Other | 1 (14.3) |
| Number of participants | |
| 1 | 2 (28.6) |
| 6–7 | 3 (42.9) |
| 10 | 2 (28.6) |
|
| |
| Participant gender | |
| Male only | 2 (28.6) |
| Female only | 1 (14.3) |
| Mixed (30%–60% men) | 4 (57.1) |
|
| |
| All program participants | N=42 |
| Age in years, average (range) | |
| Male | 60.1 (32–86) |
| Female | 55.5 (25–80) |
|
| |
| Interviewed program participants | Number (%) N=22 |
| Gender | |
| Male | 9 (41) |
| Female | 13 (59) |
| Total | 22 (100) |
| Age | |
| <51 years | 6 (27.3) |
| 51–65 years | 7 (31.8) |
| >65 years | 9 (40.9) |
| Chronic illness | |
| Diabetes | 12 (54.5) |
| CVD | 3 (13.6) |
| COLD | 3 (13.6) |
| None | 4 (18.2) |
| Duration of chronic illness | |
| <1 year | 3 (16.7) |
| 1–5 years | 4 (22.2) |
| >5 years | 7 (38.9) |
| Unknown | 4 (22.2) |
|
| |
| Interviewed educators | Number (%) N=11 |
| Gender | |
| Female | 11 (100) |
| Professional background | |
| Nurse | 4 (36.4) |
| Physiotherapist | 3 (27.3) |
| Dietitian | 2 (18.2) |
| Other | 2 (18.2) |
| Work place | |
| Municipality | 7 (63.6) |
| Hospital | 2 (18.2) |
| General practice | 2 (18.2) |
| Years of experience as patient educator | |
| <5 years | 4 (36.4) |
| >5 years | 7 (63.6) |
Notes:
Some educators had more than one professional background.
A patient-centered general chronic illness education program NEED (Next Education) is widely applied in patient education settings in the southern region of Denmark.1–3
In two settings, more than one dialogue tool was applied.
Included as part of another tool (My Immediate World) on one occasion.
Abbreviations: CVD, cardiovascular disease; COLD, chronic obstructive lung disease; T2D, type 2 diabetes.
Table S2.
Use of each tool and contexts in which 65 educators tested tools
| Tools | Educators using the tool, N | Times used, N | Average duration, minutes | Themes addressed, Na | Target groups testing the tool, Nb | Used more than once, N | Used at individual consultations, N | Used in group sessions with 2–4 participants, N | Used in group sessions with 5–10 participants, N | Used in group sessions with >10 participants, N | Participants included hardly reached individuals, N |
|---|---|---|---|---|---|---|---|---|---|---|---|
| My Day | 6 | 11 | 28 | 9 | 4 | 4 | 6 | 0 | 0 | 0 | 3 |
| Check-in | 10 | 20 | 116 | 7 | 5 | 7 | 2 | 0 | 6 | 2 | 10 |
| Our Rules | 15 | 20 | 25 | 10 | 5 | 4 | 0 | 1c | 10c | 5c | 9 |
| My Immediate World | 13 | 18 | 32 | 9 | 4 | 4 | 2c | 0 | 11c | 1c | 11 |
| My Contact with HCPs | 5 | 6 | 30 | 8 | 3 | 1 | 3 | 0 | 2 | 0 | 5 |
| Fact or Fiction | 10 | 12 | 26 | 8 | 3 | 2 | 1 | 5 | 1 | 3 | 8 |
| Where Am I? | 25 | 42 | 23 | 10 | 5 | 12 | 9c | 2c | 8c | 7c | 19 |
| We’re On the Way | 9 | 13 | 40 | 8 | 4 | 3 | 0 | 2 | 7 | 0 | 7 |
| Check-out | 24 | 47 | 14 | 7 | 5 | 15 | 1c | 5c | 19c | 1c | 21 |
Notes:
Themes: knowledge, illness, and symptoms; medicine; nutrition; physical activity; smoking/alcohol use; social relations; relationship with HCPs; emotional relationships; stress management; others.
Target groups: participants with T2D, chronic obstructive lung disease, cardiovascular disease, cancer, and other.
Total exceeds number of educators who used the tool because some used it with groups of more than one size.
Abbreviations: HCPs, health care professionals; T2D, type 2 diabetes.
References
- 1.Steno Health Promotion Center . In balance with chronic illness. Tools for patient education; Gentofte, Denmark: 2011. [Google Scholar]
- 2.Torenholt R, Engelund G, Willaing I. Bringing person-centeredness and active involvement into reality: the feasibility of a participatory concept for patient education. Health Educ. 2015;115:518–533. [Google Scholar]
- 3.Pals RAS, Olesen K, Willaing I. What does theory-driven evaluation add to the analysis of self-reported outcomes of diabetes education? A comparative realist evaluation of a participatory patient education approach. Patient Educ Couns. 2016;99:995–1001. doi: 10.1016/j.pec.2016.01.006. [DOI] [PubMed] [Google Scholar]
Acknowledgments
The authors would like to thank Gitte Engelund, Susanne Vestergaard, and Kurt Æbelø, as well as all educators and participants for their contributions. The authors acknowledge Jennifer Green, Caduceus Strategies for proofreading and editing the manuscript. This work was supported by the Danish Health and Medicines Authority.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Corbin JM, Strauss A. Unending Work and Care: Managing Chronic Illness at Home. San Francisco: Jossey-Bass; 1988. [Google Scholar]
- 2.Newman S, Steed L, Mulligan K. Self-management interventions for chronic illness. Lancet. 2004;364(9444):1523–1537. doi: 10.1016/S0140-6736(04)17277-2. [DOI] [PubMed] [Google Scholar]
- 3.Jarvis J, Skinner TC, Carey ME, Davies MJ. How can structured self-management patient education improve outcomes in people with type 2 diabetes? Diabetes Obes Metab. 2010;12(1):12–19. doi: 10.1111/j.1463-1326.2009.01098.x. [DOI] [PubMed] [Google Scholar]
- 4.Holman H, Lorig K. Patient self-management: a key to effectiveness and efficiency in care of chronic disease. Public Health Rep. 2004;119(3):239–243. doi: 10.1016/j.phr.2004.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chrvala CA, Sherr D, Lipman RD. Diabetes self-management education for adults with type 2 diabetes mellitus: a systematic review of the effect on glycemic control. Patient Educ Couns. 2016;99(6):926–943. doi: 10.1016/j.pec.2015.11.003. [DOI] [PubMed] [Google Scholar]
- 6.Coppola A, Sasso L, Bagnasco A, Giustina A, Gazzaruso C. The role of patient education in the prevention and management of type 2 diabetes: an overview. Endocrine. 2016;53(1):18–27. doi: 10.1007/s12020-015-0775-7. [DOI] [PubMed] [Google Scholar]
- 7.Powers MA, Bardsley J, Cypress M, et al. Diabetes self-management education and support in type 2 diabetes: a joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. Diabetes Educ. 2017;43(1):40–53. doi: 10.1177/0145721716689694. [DOI] [PubMed] [Google Scholar]
- 8.American Diabetes Association Lifestyle management. Diabetes Care. 2017;40(Suppl 1):S33–S43. doi: 10.2337/dc17-S007. [DOI] [PubMed] [Google Scholar]
- 9.Barlow J, Wright C, Sheasby J, Turner A, Hainsworth J. Self-management approaches for people with chronic conditions: a review. Patient Educ Couns. 2002;48(2):177–187. doi: 10.1016/s0738-3991(02)00032-0. [DOI] [PubMed] [Google Scholar]
- 10.Bodenheimer T, Lorig K. Patient self-management of chronic disease in primary care. JAMA. 2002;288(19):2469–2475. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- 11.Mackenbach JP, Kulhánová I, Menvielle G, et al. Eurothine and EURO-GBD-SE consortiums Trends in inequalities in premature mortality: a study of 3.2 million deaths in 13 European countries. J Epidemiol Community Health. 2015;69(3):207–217. doi: 10.1136/jech-2014-204319. [DOI] [PubMed] [Google Scholar]
- 12.Mackenbach JP, Kunst AE, Cavelaars AE, Groenhof F, Geurts JJ. Socioeconomic inequalities in morbidity and mortality in western Europe. Lancet. 1997;349(9066):1655–1659. doi: 10.1016/s0140-6736(96)07226-1. [DOI] [PubMed] [Google Scholar]
- 13.Hill J, Nielsen M, Fox MH. Understanding the social Factors that contribute to diabetes: a means to informing health care and social policies for the chronically ill. Perm J. 2013;17(2):67–72. doi: 10.7812/TPP/12-099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saydah S, Lochner K. Socioeconomic status and risk of diabetes-related mortality in the U.S. Public Health Rep. 2010;125(3):377–388. doi: 10.1177/003335491012500306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stringhini S, Sabia S, Shipley M, et al. Association of socioeconomic position with health behaviors and mortality. JAMA. 2010;303(12):1159–1166. doi: 10.1001/jama.2010.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Freimuth VS, Mettger W. Is there a hard-to-reach audience? Public Health Rep. 1990;105(3):232–238. [PMC free article] [PubMed] [Google Scholar]
- 17.Fisher EB, Coufal MM, Parada H, et al. Peer support in health care and prevention: cultural, organizational, and dissemination issues. Annu Rev Public Health. 2014;35:363–383. doi: 10.1146/annurev-publhealth-032013-182450. [DOI] [PubMed] [Google Scholar]
- 18.Torenholt R, Varming AR, Engelund G, et al. Simplicity, flexibility and respect: preferences related to diabetes education in hardly reached people with type 2 diabetes. Patient Prefer Adherence. 2015;9:1581–1586. doi: 10.2147/PPA.S91408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Varming AR, Torenholt R, Møller BL, Vestergaard S, Engelund G. Addressing challenges and needs in patient education targeting hardly reached patients with chronic diseases. Indian J Endocrinol Metab. 2015;19(2):292–295. doi: 10.4103/2230-8210.149324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Danish Diabetes Association, Region of Southern Denmark, Steno Diabetes Center Guide to health education tools. Educating vulnerable people with chronic illness. 2015. [Accessed September 2017]. Available from: https://www.sdcc.dk/english/educational-materials/dialouge-tools/Sider/Inequity-in-health.aspx.
- 21.Bowen DJ, Kreuter M, Spring B, et al. How we design feasibility studies. Am J Prev Med. 2010;36(5):452–457. doi: 10.1016/j.amepre.2009.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hansen UM, Engelund G, Rogvi SA, Willaing I. The Balancing Person: an innovative approach to person-centered education in chronic illness. Eur J Pers Cent Healthc. 2014;2(3):290–302. [Google Scholar]
- 23.Engelund G, Hansen UM, Willaing I. ‘The Health Education Juggler’: development of a model describing educator roles in participatory, group-based patient education. Health Educ. 2014;114(5):398–412. [Google Scholar]
- 24.Brown T, Wyatt J. Design thinking for social innovation. 2010. [Accessed September 2017]. (Stanford Social Innovation Review). Available: http://www.ssireview.org/articles/entry/design_thinking_for_social_innovation.
- 25.Malterud K. Systematic text condensation: a strategy for qualitative analysis. Scand J Public Health. 2012;40(8):795–805. doi: 10.1177/1403494812465030. [DOI] [PubMed] [Google Scholar]
- 26.Steno Health Promotion Center . In balance with chronic illness. Tools for patient education. Gentofte: Steno Diabetes Center; 2011. [Google Scholar]
- 27.Torenholt R, Engelund G, Willaing I. Bringing person-centeredness and active involvement into reality: the feasibility of a participatory concept for patient education. Health Educ. 2015;115(6):518–533. [Google Scholar]
- 28.Pals RAS, Olesen K, Willaing I. What does theory-driven evaluation add to the analysis of self-reported outcomes of diabetes education? A comparative realist evaluation of a participatory patient education approach. Patient Educ Couns. 2016;99(6):995–1001. doi: 10.1016/j.pec.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 29.Grande SW, Faber MJ, Durand MA, Thompson R, Elwyn G. A classification model of patient engagement methods and assessment of their feasibility in real-world settings. Patient Educ Couns. 2014;95(2):281–287. doi: 10.1016/j.pec.2014.01.016. [DOI] [PubMed] [Google Scholar]
- 30.Millan-Ferro A, Caballero E. Cultural approaches to diabetes self-management programs for the latino community. Curr Diab Rep. 2007;7(5):391–397. doi: 10.1007/s11892-007-0064-9. [DOI] [PubMed] [Google Scholar]
- 31.Saunders MM, Hale DL, Harris K. Clinical nurse specialists’ perceptions of care for vulnerable patients. Holist Nurs Pract. 2016;30(2):64–69. doi: 10.1097/HNP.0000000000000132. [DOI] [PubMed] [Google Scholar]
- 32.Deakin T, McShane CE, Cade JE, Williams RD. Group based training for self-management strategies in people with type 2 diabetes mellitus. Cochrane Database Syst Rev. 2005;2:CD003417. doi: 10.1002/14651858.CD003417.pub2. [DOI] [PubMed] [Google Scholar]
- 33.Des Jardins T, Drone SA, Hashisaka S, et al. Patient engagement and activation in three underserved Beacon Communities. J Health Care Poor Underserved. 2015;26(3):777–783. doi: 10.1353/hpu.2015.0084. [DOI] [PubMed] [Google Scholar]
- 34.Kauffman KS, dosReis S, Ross M, Barnet B, Onukwugha E, Mullins CD. Engaging hard-to-reach patients in patient-centered outcomes research. J Comp Eff Res. 2013;2(3):313–324. doi: 10.2217/cer.13.11. [DOI] [PubMed] [Google Scholar]
- 35.Mayberry LS, Osborn CY. Family support, medication adherence, and glycemic control among adults with type 2 diabetes. Diabetes Care. 2012;35(6):1239–1245. doi: 10.2337/dc11-2103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Khan CM, Stephens MAP, Franks MM, et al. Influences of spousal support and control on diabetes management through physical activity. Health Psychol. 2013;32(7):739–747. doi: 10.1037/a0028609. [DOI] [PubMed] [Google Scholar]
- 37.Grabowski D, Andersen TH, Varming A, Ommundsen C, Willaing I. Involvement of family members in life with type 2 diabetes: Six interconnected problem domains of significance for family health identity and healthcare authenticity. SAGE Open Med. 2017;5:1–9. doi: 10.1177/2050312117728654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lorig KR, Ritter PL, Gonzales VM. Hispanic chronic disease self-development: a randomized community-based outcome trial. Nurs Res. 2003;52(6):361–369. doi: 10.1097/00006199-200311000-00003. [DOI] [PubMed] [Google Scholar]
- 39.Harrison M, Fullwood C, Bower P, Kennedy A, Rogers A, Reeves D. Exploring the mechanisms of change in the chronic disease self-management program: secondary analysis of data from a randomized controlled trial. Patient Educ Couns. 2011;85(2):e39–e47. doi: 10.1016/j.pec.2010.10.026. [DOI] [PubMed] [Google Scholar]
- 40.Andersen TH, Hempler NF, Willaing I. Educator challenges using participatory methods in group-based patient education. Health Educ. 2014;114(2):152–165. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1.
Educators, participants, and settings
| Surveyed educators | Number (%) N=65 |
| Gender | |
| Female | 65 (100) |
| Professional backgrounda | |
| Nurse | 17 (26.2) |
| Physiotherapist | 31 (47.7) |
| Dietitian | 11 (16.9) |
| Other | 10 (15.4) |
| Work place | |
| Municipality | 61 (93.8) |
| Hospital | 3 (4.6) |
| General practice | 1 (1.5) |
| Years of experience as patient educator | |
| None | 8 (12.3) |
| 0–1 | 12 (18.5) |
| 1–2 | 5 (7.7) |
| 2–5 | 20 (30.8) |
| >5 | 20 (30.8) |
| Experience with a similar person-centered education programb | |
| To a large extent | 4 (6.2) |
| To some extent | 30 (46.2) |
| Observational experience | 14 (215) |
| Theoretical experience | 9 (13.8) |
| No knowledge | 8 (12.3) |
|
| |
| Observed patient education settings | Number (%) N=7 |
| Organizational setting | |
| Municipality | 5 (71.4) |
| Hospital | 1 (14.3) |
| General practice | 1 (14.3) |
| Dialogue tools appliedc | |
| My Day | 0 |
| Check-in | 0 |
| Our Rules | 2 (28.6) |
| My Immediate World | 2 (28.6) |
| My Contact with Healthcare Professionals | 0d |
| Fact or Fiction | 1 (14.3) |
| Where Am I? | 3 (42.9) |
| We’re on the Way | 0 |
| Check-out | 1 (14.3) |
| Education theme | |
| T2D | 3 (42.9) |
| Physical activity | 3 (42.9) |
| Other | 1 (14.3) |
| Target group for education | |
| People with T2D | 4 (57.1) |
| People with chronic illness of different kinds or CVD only | 2 (28.6) |
| Other | 1 (14.3) |
| Number of participants | |
| 1 | 2 (28.6) |
| 6–7 | 3 (42.9) |
| 10 | 2 (28.6) |
|
| |
| Participant gender | |
| Male only | 2 (28.6) |
| Female only | 1 (14.3) |
| Mixed (30%–60% men) | 4 (57.1) |
|
| |
| All program participants | N=42 |
| Age in years, average (range) | |
| Male | 60.1 (32–86) |
| Female | 55.5 (25–80) |
|
| |
| Interviewed program participants | Number (%) N=22 |
| Gender | |
| Male | 9 (41) |
| Female | 13 (59) |
| Total | 22 (100) |
| Age | |
| <51 years | 6 (27.3) |
| 51–65 years | 7 (31.8) |
| >65 years | 9 (40.9) |
| Chronic illness | |
| Diabetes | 12 (54.5) |
| CVD | 3 (13.6) |
| COLD | 3 (13.6) |
| None | 4 (18.2) |
| Duration of chronic illness | |
| <1 year | 3 (16.7) |
| 1–5 years | 4 (22.2) |
| >5 years | 7 (38.9) |
| Unknown | 4 (22.2) |
|
| |
| Interviewed educators | Number (%) N=11 |
| Gender | |
| Female | 11 (100) |
| Professional background | |
| Nurse | 4 (36.4) |
| Physiotherapist | 3 (27.3) |
| Dietitian | 2 (18.2) |
| Other | 2 (18.2) |
| Work place | |
| Municipality | 7 (63.6) |
| Hospital | 2 (18.2) |
| General practice | 2 (18.2) |
| Years of experience as patient educator | |
| <5 years | 4 (36.4) |
| >5 years | 7 (63.6) |
Notes:
Some educators had more than one professional background.
A patient-centered general chronic illness education program NEED (Next Education) is widely applied in patient education settings in the southern region of Denmark.1–3
In two settings, more than one dialogue tool was applied.
Included as part of another tool (My Immediate World) on one occasion.
Abbreviations: CVD, cardiovascular disease; COLD, chronic obstructive lung disease; T2D, type 2 diabetes.
Table S2.
Use of each tool and contexts in which 65 educators tested tools
| Tools | Educators using the tool, N | Times used, N | Average duration, minutes | Themes addressed, Na | Target groups testing the tool, Nb | Used more than once, N | Used at individual consultations, N | Used in group sessions with 2–4 participants, N | Used in group sessions with 5–10 participants, N | Used in group sessions with >10 participants, N | Participants included hardly reached individuals, N |
|---|---|---|---|---|---|---|---|---|---|---|---|
| My Day | 6 | 11 | 28 | 9 | 4 | 4 | 6 | 0 | 0 | 0 | 3 |
| Check-in | 10 | 20 | 116 | 7 | 5 | 7 | 2 | 0 | 6 | 2 | 10 |
| Our Rules | 15 | 20 | 25 | 10 | 5 | 4 | 0 | 1c | 10c | 5c | 9 |
| My Immediate World | 13 | 18 | 32 | 9 | 4 | 4 | 2c | 0 | 11c | 1c | 11 |
| My Contact with HCPs | 5 | 6 | 30 | 8 | 3 | 1 | 3 | 0 | 2 | 0 | 5 |
| Fact or Fiction | 10 | 12 | 26 | 8 | 3 | 2 | 1 | 5 | 1 | 3 | 8 |
| Where Am I? | 25 | 42 | 23 | 10 | 5 | 12 | 9c | 2c | 8c | 7c | 19 |
| We’re On the Way | 9 | 13 | 40 | 8 | 4 | 3 | 0 | 2 | 7 | 0 | 7 |
| Check-out | 24 | 47 | 14 | 7 | 5 | 15 | 1c | 5c | 19c | 1c | 21 |
Notes:
Themes: knowledge, illness, and symptoms; medicine; nutrition; physical activity; smoking/alcohol use; social relations; relationship with HCPs; emotional relationships; stress management; others.
Target groups: participants with T2D, chronic obstructive lung disease, cardiovascular disease, cancer, and other.
Total exceeds number of educators who used the tool because some used it with groups of more than one size.
Abbreviations: HCPs, health care professionals; T2D, type 2 diabetes.