Shields et al. described a series of 12 cases of retinal vascular mass with distinct clinical features but of unknown etiology in the early 1980s, which they hesitatingly called “Presumed Acquired Retinal Hemangioma.”[1] Baines et al. reported a similar entity and called it the “Peripheral Nodular Retinal Telangiectasia.”[2] Hiscott and Mudhar suspected that it may be a part of the spectrum of proliferative vitreoretinopathy and called it “Reactive Retinal Glioangiosis.”[3] Several authors have recognized the common clinical features of this benign, acquired vascular retinal lesion, which is now known as retinal vasoproliferative tumor (RVPT).[4,5,6,7,8] It is characterized by one or more globular vascular retinal mass lesions with or without feeder vessels and retinal telangiectasia, color varying from fiery red to intense pink to a more sedate dirty yellow, predominantly in preequatorial and inferotemporal location, with localized, diffuse, or remote macular intra- and subretinal exudates, macular edema, and epiretinal membranes.[4,5,6,7,8]
It is understood that RVPT is not a true tumor but represents reactive proliferation of blood vessels in response to some form of retinal ischemia, injury, or inflammation.[4,5,6,7,8] This unchecked localized proliferation of blood vessels in a loose glial matrix organizes itself into a vascular mass. Over time in a long-standing mass, or following treatment, reactive gliosis predominates over the vascular component, and in the end-stage, the color of the mass changes to yellow or white.[4,5,6,7,8] On histopathology, it shows glial cells interlaced with a fine capillary network and dilated, hyalinized partially occluded blood vessels, with exudates, macrophages, and foreign-body giant cells.[4,5,6,7,8,9] Histopathology does not support the presence of a “vasoproliferative” component in the lesion, and hence, the term RVPT is not universally accepted.[3,9] It is possible that the eyes that were enucleated and were available for histopathology had end-stage RVPT with predominant gliosis, thus skewing the findings.[3,9] While RVPT may indeed be a retinal mass composed of a reactive proliferation of blood vessels with a variable amount of gliosis, it is difficult to accept it as a tumor. It may be called a pseudotumor, analogous to exuberant granulation tissue (pyogenic granuloma) often found in the conjunctiva.
RVPTs can be classified as primary or secondary.[10] About three-fourths of RVPTs in the West are primary (idiopathic), while the remaining are associated with a coexisting ocular or a systemic disease such as retinitis pigmentosa, Coats' disease, retinopathy of prematurity, familial exudative vitreoretinopathy, retinal vasculitis, intermediate uveitis, choroiditis, histoplasmosis, toxoplasmosis, chronic retinal detachment of any etiology, prior laser photocoagulation or cryotherapy, and neurofibromatosis type 1.[10] Common denominators of these associated conditions seem to be retinal inflammation, ischemia, neovascularization, and exudation.[4,5,6,7,8,9,10]
In our series of 120 cases of RVPT in Indian population, only 40% were primary and 60% were secondary. Apart from the already known etiologies, the secondary RVPTs in our series were associated with regressed retinoblastoma status-post external beam radiotherapy, regressed melanoma status-post plaque brachytherapy, lasered diabetic retinopathy, scleral repair following trauma, vitrectomy for various conditions, pneumatic retinopexy, and Eales' disease. While the mean age of primary RVPTs was 48 years, the secondary RVPTs had a bimodal onset – in the first and second decade of life, and beyond the sixth decade. Only two cases of primary RVPT were bilateral. However, 20% of secondary RVPTs were bilateral. This issue of Indian Journal of Ophthalmology carries a series of cases of RVPT in Asian Indians, which supports the view that Indian spectrum of RVPT may be different from that in the West.[11]
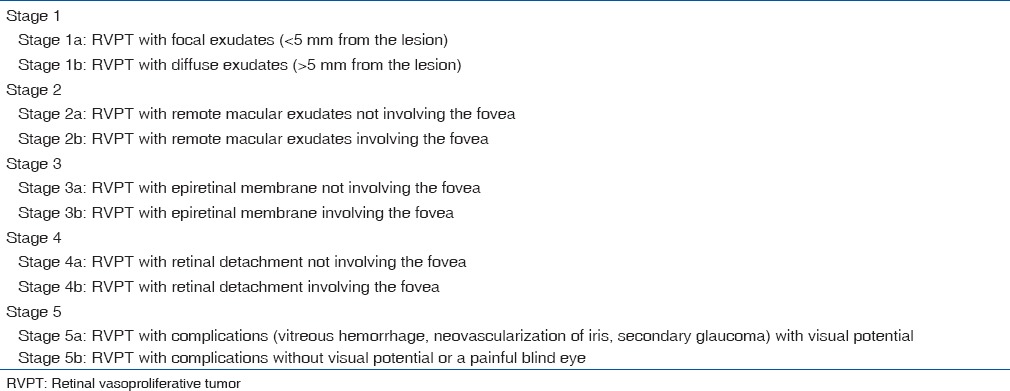
Clinical manifestations included globular vascular retinal mass with local or diffuse intra- and subretinal exudation, exudation at the macula, serous and tractional retinal detachment, dilated retinal vessels, retinal pigment epithelial alterations, macular edema, epiretinal membrane, vitreous hemorrhage, vitreous exudates, and neovascular glaucoma. Based on our clinical observations, a staging system has been proposed [Table 1], which is currently being validated for its relevance to management and outcome. This simple clinical staging can help guide treatment and assess prognosis.
Table 1.
Proposed staging of retinal vasoproliferative tumor
Management of RVPT can be simple observation if there is no threat to vision. For lesions with loss or threat to vision, management modalities used include laser photocoagulation or transpupillary thermotherapy (lesions ≤3 mm in diameter and thickness with no overlying subretinal fluid), cryotherapy (lesions ≤6 mm in diameter and ≤3 mm in thickness with or without subretinal fluid), plaque brachytherapy (lesions >3 mm in thickness with or without subretinal fluid), intravitreal triamcinolone (for patients with macular edema and predominant exudation), intravitreal anti-vascular endothelial growth factor (for patients with macular edema, exudation, and predominant vascularity of the lesion), and vitreoretinal surgery (tractional retinal detachment, unresolving vitreous hemorrhage, epiretinal membrane, etc.).
RVPT is not uncommon and has an impact on vision because of remote macular involvement. It needs to be specifically looked for and recognized when a patient presents with remote macular exudates. Prompt diagnosis and appropriate treatment may help maintain or improve vision.
References
- 1.Shields JA, Decker WL, Sanborn GE, Augsburger JJ, Goldberg RE. Presumed acquired retinal hemangiomas. Ophthalmology. 1983;90:1292–300. doi: 10.1016/s0161-6420(83)34389-x. [DOI] [PubMed] [Google Scholar]
- 2.Baines PS, Hiscott PS, McLeod D. Posterior non-vascularized proliferative extraretinopathy and peripheral nodular retinal telangiectasis. Trans Ophthalmol Soc U K. 1982;102(Pt 4):487–91. [PubMed] [Google Scholar]
- 3.Hiscott P, Mudhar H. Is vasoproliferative tumour (reactive retinal glioangiosis) part of the spectrum of proliferative vitreoretinopathy? Eye (Lond) 2009;23:1851–8. doi: 10.1038/eye.2008.351. [DOI] [PubMed] [Google Scholar]
- 4.Shields CL, Shields JA, Barrett J, De Potter P. Vasoproliferative tumors of the ocular fundus. Classification and clinical manifestations in 103 patients. Arch Ophthalmol. 1995;113:615–23. doi: 10.1001/archopht.1995.01100050083035. [DOI] [PubMed] [Google Scholar]
- 5.Jain K, Berger AR, Yucil YH, McGowan HD. Vasoproliferative tumours of the retina. Eye (Lond) 2003;17:364–8. doi: 10.1038/sj.eye.6700311. [DOI] [PubMed] [Google Scholar]
- 6.Heimann H, Bornfeld N, Vij O, Coupland SE, Bechrakis NE, Kellner U, et al. Vasoproliferative tumours of the retina. Br J Ophthalmol. 2000;84:1162–9. doi: 10.1136/bjo.84.10.1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smeets MH, Mooy CM, Baarsma GS, Mertens DE, Van Meurs JC. Histopathology of a vasoproliferative tumor of the ocular fundus. Retina. 1998;18:470–2. doi: 10.1097/00006982-199805000-00016. [DOI] [PubMed] [Google Scholar]
- 8.Irvine F, O'Donnell N, Kemp E, Lee WR. Retinal vasoproliferative tumors: Surgical management and histological findings. Arch Ophthalmol. 2000;118:563–9. doi: 10.1001/archopht.118.4.563. [DOI] [PubMed] [Google Scholar]
- 9.Poole Perry LJ, Jakobiec FA, Zakka FR, Reichel E, Herwig MC, Perry A, et al. Reactive retinal astrocytic tumors (so-called vasoproliferative tumors): Histopathologic, immunohistochemical, and genetic studies of four cases. Am J Ophthalmol. 2013;155:593–6080. doi: 10.1016/j.ajo.2012.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shields CL, Kaliki S, Al-Dahmash S, Rojanaporn D, Shukla SY, Reilly B, et al. Vasoproliferative tumors of the ocular fundus: Comparative clinical features of primary versus secondary tumors in 334 cases. Arch Ophthalmol. 2012;131:328–34. doi: 10.1001/2013.jamaophthalmol.524. [DOI] [PubMed] [Google Scholar]
- 11.Walinjkar JA, Sharma US, Rishi P, Rishi E, Gopal L, Sharma T. Clinical features and treatment outcomes of vasoproliferative tumors in Indian participants. Indian J Ophthalmol. 2018;66:246–51. doi: 10.4103/ijo.IJO_210_17. [DOI] [PMC free article] [PubMed] [Google Scholar]


