Abstract
Purpose:
To study the time course of interface healing and its correlation with visual acuity, modulation transfer function (MTF), and aberrations after myopic small-incision lenticule extraction (SMILE) correction.
Methods:
Seventy-eight eyes of 78 patients (1 eye per patient) with a mean age of 25.7 years and mean spherical equivalent (SE) of −3.74D, undergoing bilateral SMILE procedure, were included in this study. On postoperative day 1, 2 weeks, and 3 months, dilated retroillumination photographs were taken and morphology of corneal interface was graded by comparing them with 5 standard templates representing 5 grades of interface roughness (IRG): IRG – 0 (clear), IRG – 1 (mild), IRG – 2 (moderate), IRG – 3 (severe), and IRG – 4 (severe IRG with Bowman's folds in visual axis). Pearson's correlations were computed to study correlation associations, and Wilcoxon signed-rank test was used for intragroup comparison of means. P ≤ 0.05 was considered statistically significant.
Results:
At 3 months, 90.70% eyes were Grade 0 while 9.30% eyes still had Grade 2 interface granularity. Mean IRG significantly improved from 2.47 ± 0.57 at day 1 to 0.62 ± 0.53 at 3 months (P = 0.00). At day 1, pre-SE showed a significant positive correlation with IRG; however, mean postoperative corrected distant visual acuity (CDVA, in decimal), corneal Strehl ratio (SR), and MTF showed weak but significant negative correlation with IRG (r2 = 0.28 for SE, −0.052 for CDVA, −0.017 for SR, and −0.39 for MTF, respectively, P < 0.05 for all correlations). At 2 weeks and 3 months, corneal MTF continued to show a significant negative correlation, whereas other parameters did not show any correlation with IRG.
Conclusion:
Visual quality and corneal MTF may be significantly affected by the IRG in the immediate postoperative period after SMILE and may take 3 months or more for complete recovery.
Keywords: Interface healing, optical quality, small-incision lenticule extraction
Refractive lenticule extraction through a small-incision lenticule extraction (ReLEx SMILE) has recently emerged as a preferred technique for correction of myopia, and various studies have established the long-term safety and efficacy of the procedure.[1,2,3] Comparison studies between laser in situ keratomileusis (LASIK) and SMILE have highlighted significant advantages of SMILE over LASIK such as no flap-related complications, less postoperative dry eye, and possibly better corneal biomechanics.[4,5,6] However, inability to treat hyperopia and mixed astigmatism, lack of iris registration software for cyclotorsion compensation, and slower visual recovery compared to LASIK are presently some limitations of this procedure.[7] Delayed visual recovery particularly has been highlighted as one of the main demerits due to various reasons such as suboptimal laser energy, poor surgical technique, the degree of tissue manipulation, and Bowman's membrane microdistortions.[8,9,10] However, interface healing as a cause of delayed visual recovery and its correlation with quality of vision has not been studied. The purpose of this work is to evaluate the interface healing following myopic SMILE procedure using serial clinical photography and study its correlation with uncorrected visual acuity, contrast sensitivity, Strehl ratio (SR), modular transfer function (MTF), and corneal aberrations in a 3-month, prospective clinical study.
Methods
This prospective, nonrandomized clinical study was approved by the Institutional Ethics Committee of our hospital and adhered to the tenets of the Declaration of Helsinki. Written informed consent was obtained from all patients participating in the study.
Seventy-eight eyes of 78 patients (1 eye from 1 patient) undergoing bilateral SMILE were included in the study. Inclusion criteria were as follows: age between 21 and 40 years, spherical equivalent (SE) ≤−10 D, myopic astigmatism ≤1 D, stable refraction (<0.5 D change in the past 12 months), corrected distant visual acuity (CDVA) of 20/20 or better, healthy ocular surface, absence of corneal ectatic diseases such as keratoconus, corneal scars, absence of any retinal pathology likely to affect visual outcomes, and assured follow-ups.
Eyes with thin corneas (central pachymetry <480 μm), diagnosed or suspicious cases of corneal ectatic conditions, moderate-to-severe dry eyes (Schirmer's 1 <15 mm), severe contact lens allergy, patients on systemic steroids, immunosuppressants, oral contraceptives, antidepressants, and pregnant females were excluded from the study.
Preoperative evaluation
All patients underwent a thorough preoperative evaluation including anterior and posterior segment examination, uncorrected distance visual acuity (UDVA) and CDVA, corneal topography using Pentacam HR (Oculus Optikgeräte GmbH, Wetzlar, Germany) and Orbscan II (Bausch and Lomb, Rochester, NY, USA), contrast sensitivity using Functional Acuity Contrast Test (FACT, STEREO OPTICAL CO., INC. Chicago, USA), aberrometry (Hoya iTrace, surgical workstation, Japan), and dry eye evaluation with Schirmer 1, 2 and tear film breakup time. Ray-tracing technology (iTrace, Hoya) was used to measure the MTF, higher-order aberrations (HOA), and SR under scotopic conditions by covering the head of the patient with a black cloth. The patient was asked to blink the eye before capturing the measurement to enable uniform distribution of the tear film on the eye on all postoperative visits. Contrast sensitivity was evaluated using the FACT chart under standardized mesopic light conditions at 10 meters from the chart.
Patients wearing contact lenses were advised to discontinue contact lenses for a minimum period of 1 week for soft and 3 weeks for rigid contact lenses.
Surgical technique
All surgeries were performed by a single experienced refractive surgeon (S. G.) under topical anesthesia, using the VisuMax femtosecond laser (Carl Zeiss Meditec, Jena, Germany), with a pulse repetition rate of 500 KHz, cut energy of 160 nJ, 6.50 to 7.00 mm optical zone, cap thickness of 120 μm, and a 2-mm superior incision following the standard surgical technique.[9] The treatment was centered on the visual axis. Mean optical zone used was 6.5 ± 0.23 mm.
Postoperatively, patients were prescribed 0.3% ofloxacin eye drops (Exocin®, Allergan, Irvine, USA) 4 times for 3 days, 0.1% prednisolone acetate eye drops (Pred Forte®, Allergan, Irvine, USA) in tapering dosage for 4 weeks, and lubricants four times for 4 weeks or more.
Patients were followed up on postoperative day 1, 2 weeks, and 3 months. At every visit, slit-lamp examination for the corneal condition, noncontact tonometry, and UDVA and CDVA was evaluated.
On day 1, 2-week, and 3-month postoperative visits, after instillation of one drop of lubricant, dilated clinical photographs were taken in a retroillumination mode using the Haag-Streit photo slit-lamp camera (model BX 900, Rosengarten, Germany) using a fixed setting of ×16 magnification and level 3 illumination to ensure uniformity in all photographs. Photographs were taken for both eyes of each patient. However, only one eye of each patient was randomly selected for analysis to eliminate bias due to the inclusion of both eyes of the same individual with a similar healing response.
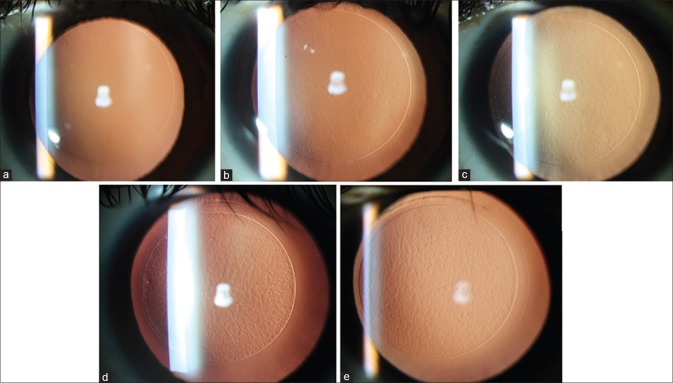
At the time of analysis, 5 standard templates, representing 5 grades of interface granularity/roughness, were created by an independent observer from a total of 234 postoperativephotographs of the 78 study eyes taken at 1st day, 2-week, and 3-month follow-up. The five IRGs used were as follows: IRG – 0 (clear), IRG – 1 (mild IRG), IRG – 2 (moderate IRG), IRG – 3 (severe IRG), and IRG – 4 (severe IRG with Bowman's folds in the visual axis) [Fig. 1].
Figure 1.
Retroillumination photographs after dilatation at ×16 magnification showing the five templates of interface roughness grade. (a) interface roughness grade – 0 (clear), (b) interface roughness grade – 1 (mild interface roughness), (c) interface roughness grade – 2 (moderate interface roughness), (d) interface roughness grade – 3 (severe interface roughness), (e) interface roughness grade – 4 (severe interface roughness with Bowman's folds in the visual axis)
All the 234 postoperative photographs were then jumbled up and presented to a second independent observer who matched the interface quality of each photograph with those of the five standard templates and thus assigned a grade corresponding to the template, to which the interface closely resembled. The observer was completely unaware of the timing of the postoperative visit at which these photographs were taken.
Apart from clinical photography, iTrace aberrometry was performed for corneal HOAs, MTF, and SR at all postoperative visits.
Statistical analysis
SPSS software for Windows version 17.0.0 (IBM Corp., Armonk, NY, USA) was used for statistical analysis. All values were expressed as the mean ± standard deviation. Pearson's correlations were computed to study correlation associations between IRG scores and other variables such as CDVA, MTF, SR, and HOAs of the cornea. Data were studied for normality, and Wilcoxon signed-rank test was used for intragroup comparison of means. P = 0.05 or less was considered statistically significant.
Results
All surgeries were uneventful, and no intraoperative complications such as suction loss, black spots, difficult dissection, or incomplete separation of lenticule occurred in any of the eyes.
Visual and refractive outcomes
Compared to day 1, both mean UDVA and CDVA showed statistically significant improvement at 2 weeks (P = 0.00 for both UDVA and CDVA). At 3-month postoperative, the mean UDVA was −0.066 ± 0.09 logMAR which was significantly better compared to 2 weeks (P = 0.005) while the mean CDVA was −0.096 ± 0.08 logMAR which also showed statistically significant improvement from 2 weeks (P = 0.001) [Table 1].
Table 1.
Visual and refractive data of the study participants at pre-, day 1, 2-week, and 3-month postoperative visits
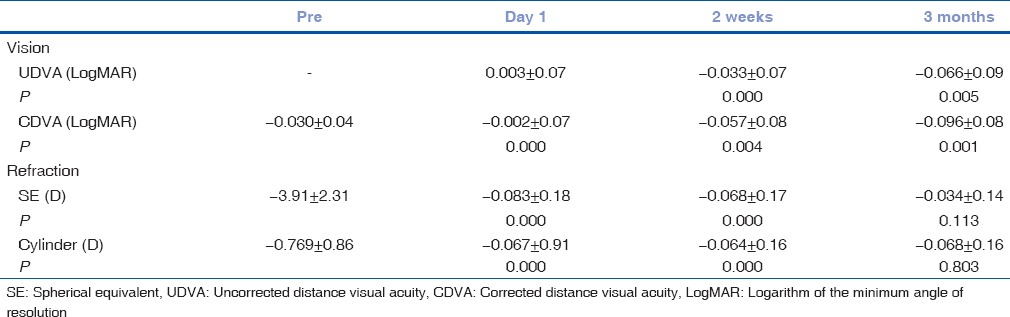
The mean SE reduced from −3.91 ± 2.31 D preoperatively to −0.068 ± 0.17 D at 2 weeks, which further reduced slightly to −0.034 ± 0.14 D at the end of 3-month follow-up (P = 0.000) [Table 1]. Nearly 95% eyes were within ± 0.50 D while all eyes were within ± 1.00D of SE correction. Similar changes were observed in the cylinder, which reduced significantly from the preoperative value of −0.769 ± 0.86 D to −0.064 ± 0.16 D at 2 weeks postoperatively (P = 0.00), with no significant change after that.
Corneal aberrations, modulation transfer function, Strehl ratio, and contrast sensitivity
Corneal HOAs increased significantly from RMS 0.129 ± 0.06 μ to 0.169 ± 0.08 μ at day 1, which however reduced significantly to 0.166 ± 0.08 μ at 2 weeks (P = 0.038). The aberrations did not show any significant change from 2 weeks to 3 months postoperative.
Both the MTF and SR, on the other hand, showed a statistically significant reduction at day 1, compared to preoperative mean values (P = 0.03 for both), with mild nonsignificant improvement over time [Table 2].
Table 2.
Comparison of corneal higher-order aberrations, modular transfer function, Strehl ratio, and contrast sensitivity (functional acuity contrast test) at pre-, day 1,2-week, and 3-month postoperative visits
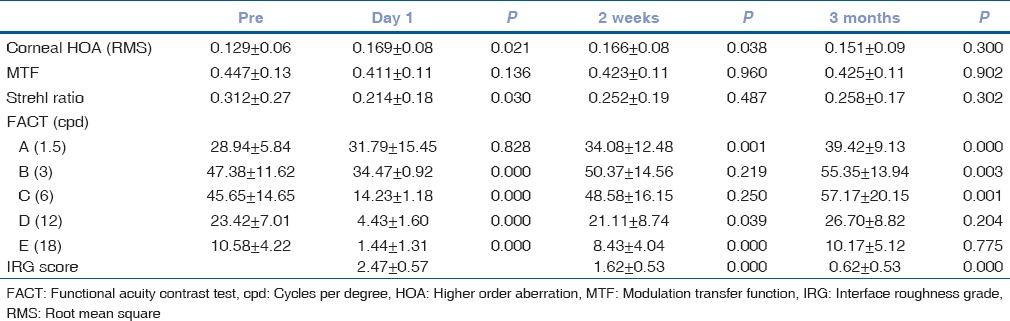
At day 1, compared to preoperative, the contrast sensitivity scores were nonsignificantly better for the spatial frequency of 1.5 cpd (P = 0.82) while the scores were significantly worse for higher spatial frequencies of 3, 6, 12, and 18 cpd (P < 0.05). At 3 months, the mean scores continued to improve from 2 weeks for spatial frequencies of 1.5, 3, and 6 (P < 0.05) while no significant change was observed for 12 and 18 spatial frequencies [Fig. 2 and Table 2].
Figure 2.
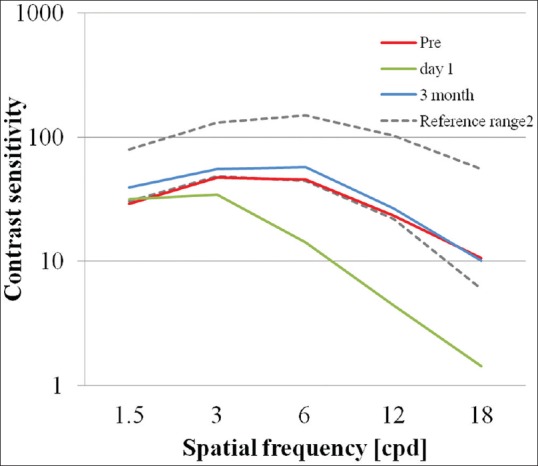
Contrast sensitivity (functional acuity contrast test) changes over time
Interface roughness grade
The mean IRG was 2.47 ± 0.86 on day 1, which reduced to 1.63 ± 0.62 at 2 weeks, and further reduced to 0.63 ± 0.27 at the end of 3 months. On day 1, majority (55.10%) of eyes were Grade 3, at 2 weeks, 57.70% eyes were Grade 2, while at 3 months, 90.70% eyes were Grade 0. Approximately 10% of eyes still had Grade1 or 2 at the end of 3 months [Fig. 3a].
Figure 3.
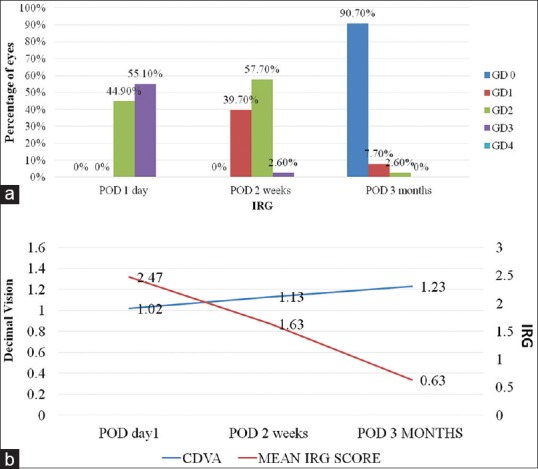
(a) Distribution of interface roughness grade at postoperative day 1, 2 weeks, and 3 months postoperative. (b) Correlation of corrected distant visual acuity with interface roughness grade score over time
The preoperative SE, at day 1, showed a weak but statistically significant positive correlation with IRG score (correlation coefficient (r2) = 0.282, P = 0.012). However, at 2 weeks and 3 months, the correlation was not statistically significant with IRG [Table 3].
Table 3.
Correlations of preoperative spherical equivalent and postoperative corrected distance visual acuity, corneal modulation transfer function, corneal Strehl ratio, and corneal higher-order aberration with interface roughness grade at day 1, 2-week, and 3-month postoperative visits
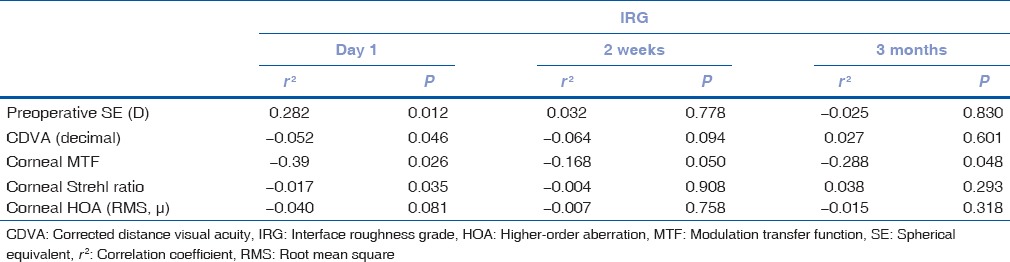
However, the mean postoperative CDVA (decimal) at day 1 showed a weak but statistically significant negative correlation with IRG score (correlation coefficient (r2) = −0.052, P = 0.04). However, at 2 weeks and 3 months, the CDVA did not show statistically significant correlation with IRG [Table 3 and Fig. 3b].
The postoperative corneal SR also depicted a statistically significant negative correlation with IRG on day 1 (correlation coefficient (r2) = −0.017, P = 0.035) and no significant correlation with IRG after that [Table 3 and Fig. 4a].
Figure 4.
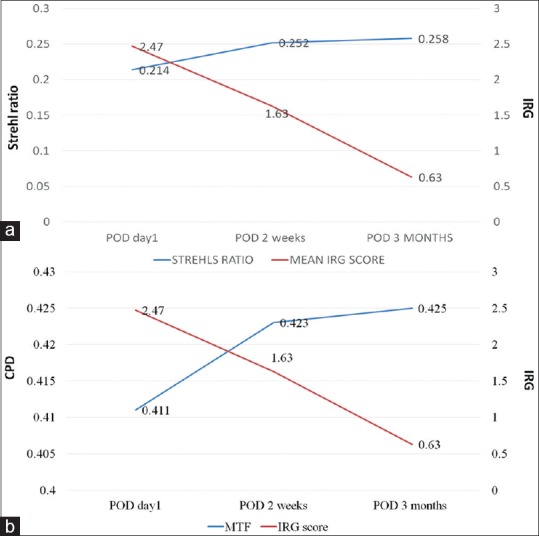
Correlation of (a) corneal Strehl ratio and (b) corneal modulation transfer function with interface roughness grade score over time
The mean postoperative corneal MTF, although followed a similar trend on day 1 as CDVA and corneal SR, i.e. showed a significant negative correlation with IRG scores (correlation coefficient (r2) = −0.39, P = 0.026), on the subsequent visits at 2 weeks and 3 months, however, continued to show a significant negative correlation with the IRG [Table 3 and Fig. 4b].
The mean postoperative corneal HOAs were not found to show any correlation with IRG at any postoperative visit [Table 3].
Discussion
Recent literature showed that the optical quality and visual recovery after SMILE were attributed to microdistortions in the Bowman's membrane which were observed to be dependent upon the refractive error and thickness of the lenticule removed.[11,12] It was also observed that these microdistortions peaked at 1 week and remained stable after that and had no impact on the long-term visual performance.[11] Shetty et al. suggested intraoperative ironing of the cap as a useful maneuver to reduce these microdistortions, to hasten postoperative visual recovery.[13] In another study, they defined a Bowman's roughness index (BRI) for quantitative evaluation of these microdistorsions and found that BRI increased after SMILE from preoperative levels possibly due to mechanical stress, changes in corneal biomechanics, mismatch between the surface areas of anterior and posterior surface of the lenticule, and relaxation of the lamellae due to severance of the transverse fibers in the anterior stroma. This increase in the BRI was related to the slow visual recovery after SMILE, which peaked at 1 week after surgery and stabilized in the further course of time.[14] However, when postoperatively does the BRI normalize has not been documented or speculated. This could be attributable to their short study period of 1 month.
According to the results of both these studies, the bowmans membrane (BM) microdistortions and BRI peaked at 1 week postoperative and remained stable after that, suggesting that visual disturbances after SMILE surgery may be expected more in the 1st week after SMILE surgery, and should settle after that. However, it is often observed that some patients complain of persistent blurness/fluctuation in vision and night glare in the absence of clinically significant dry eye disease, as long as up to 3 months after the surgery.
Furthermore, it was shown by Luo et al. that the BM microdistortions did not occur in low myopia of < −three-dimensional SE.[12] Hence, if BM microdistortions were the only reason, then patients undergoing SMILE for low myopia should be expected to have a better quality of vision compared to those for high myopia, as the latter must be associated with more BM microdistortions. On the contrary, patients with low myopia usually report lesser satisfaction compared to high myopia immediately post-SMILE surgery.
It may be suggested that the BM microdistortions may not alone contribute to the slow visual recovery after SMILE since it has been shown that structurally, the Bowman's membrane is not smooth and has some amount of microdistortions inherently,[13] possibly due to the ongoing wear and tear processes. Surgical trauma and manipulation of the Bowman's membrane during lenticule dissection may lead to an increase in these microdistortions.
Since SMILE interface is much deeper (120 μ) compared to the BM (55–60μ) and all the surgical manipulations occur at the level of interface, we believe that interface healing may also play a role in the visual recovery after SMILE; this aspect, however, has not received much attention earlier.
In the present study, we evaluated the morphology of the interface after SMILE, after dilatation of the pupil in the retroillumination mode using clinical photography at all postoperative visits through 3 months. Interestingly, we observed that the interface was visibly rough and showed severe granularity immediately postoperative and gradually cleared in due course of time, and this was significantly correlated with the CDVA, corneal MTF, and SR. This may suggest that interface healing may play a role in the visual recovery and quality of vision after SMILE.
Our observations may be supported by previous studies which showed that refractive femtosecond lenticule extraction (FLEx) induced transiently and enhanced the visibility of the interface due to mild interface haze formation which may potentially cause a delay in early visual recovery.[15,16,17] Later, Kamiya et al. confirmed these findings using a double-pass system and observed that FLEx was associated with an increase in intraocular scattering in the early postoperative period, possibly due to mild interface haze formation, but gradually recovered with time.[8]
We believe that the reason for the IRG could be the activation of keratocytes and increased reflectivity from the extracellular matrix, as recently identified by Agca et al.[18] They compared the interface backscatter between SMILE and FemtoLASIK using in vivo confocal microscopy (IVCM) and showed that SMILE resulted in significantly increased backscatter in the anterior stroma at 1 week, 1 month, and 3 months compared to FemtoLASIK; however, differences were not significant at 6 months between the two groups. They observed a network of activated keratocytes and increased reflectivity from the extracellular matrix which could be easily identified in SMILE eyes and occupied the anterior one-third of the corneal stroma in the first postoperative week.
Furthermore, it is known that the structure of the cornea is not uniform, the anterior one-third stroma being more compact, and the deeper two-third stroma being relatively loose.[18,19] Hence, the superimposition of both the superficial and deeper interfaces created in SMILE at variable depths may lead to a granular appearance when seen in retroillumination mode.
de Medeiros et al. reported that higher energy levels might induce more cell death and inflammatory response when a femtosecond laser is used for the creation of corneal flaps.[20] A study by Riau et al. showed that ReLEx induced a lower degree of keratocyte apoptosis, proliferation, and inflammation compared with FS-LASIK in rabbit eyes.[20] However, in this study, an overall comparison between the two groups was not performed, and statistics may be misleading due to small sample size. Moreover, rabbit eyes may behave differently compared to human eyes.
However, Agca et al. emphasized that the total energy applied to the corneal stroma in SMILE is higher than that in FemtoLASIK performed with the same platform. In a contralateral eye study, they compared the interface backscatter by IVCM between SMILE and FemtoLASIK using the same femtosecond platform and showed that SMILE resulted in significantly increased backscatter in the anterior stroma at 1 week, 1 month, and 3 months. However, differences were not significant at 6 months between the two groups. This was attributed to the addition of a second lamellar cut at a deeper level and the increased number of surgical steps required for blunt dissection of the planes above and below the lenticule in the SMILE group.[18]
The energy intensity of the VisuMax femtosecond laser used in SMILE is generally in the range of 120–175 nJ, and it was 160 nJ in the present study for both the lenticule and flap at a repetition rate of 500 kHz. Nevertheless, despite the low energy, some degree of keratocyte apoptosis, corneal inflammation, and edema are expected, especially in the early postoperative period. Nevertheless, despite the low energy, some degree of keratocyte apoptosis, corneal inflammation, and edema are expected, especially in the early postoperative period.[21]
In our study, IRG positively correlated with preoperative SE at day 1, suggesting that higher the amount of tissue removed, higher the amount of IRG seen. However, it negatively correlated with the postoperative CDVA, MTF, and SR at day, suggesting that immediate visual results may be influenced by the quality of interface after surgery. However, at 3 months, there was no correlation of SE, CDVA, and SR with IRG, suggesting that once the interface clears completely, it may not have bearing on these parameters. On the other hand, MTF continued to show a significant negative correlation until 3 months, indicating that the visual quality in terms of MTF may take a longer time to recover completely. This may be indirectly correlated with the results of contrast sensitivity, which had still not recovered fully for higher spatial frequencies by the end of 3 months in our study.
The HOA, however, did not seem to have any correlation with the interface healing as they are predominantly thought to occur as a result of a change in the asphericity of the cornea rather than a function of the interface.[22]
Previous studies on the optical quality and objective scatter after SMILE were performed using the optical quality analysis system, results of which may be significantly affected by ocular dryness.[23,24] This limitation is overcome when interface healing is assessed with dilated clinical photography immediately after instillation of lubricating drops.
It was observed that approximately 10% eyes still had an IRG score between 1 and 2 at the end of 3 months, suggesting that it may take 3 months or more for the healing of the interface and hence complete stabilization of vision after SMILE. This could be a potential limitation of our study that our follow-up was relatively short. However, it was found in recent studies that most of the visual quality parameters such as point spread function and corneal MTF had returned to the preoperative values by 3–6 months after refractive lenticule extraction.[7,8] Another the limitation could be that the method of evaluation of interface healing was based on subjective assessment of the observer.
Conclusion
To our knowledge, interface healing and its correlation with the visual quality of SMILE using clinical photography have not been studied. This may be used as a simple and inexpensive tool to monitor changes in healing patterns and reassure apprehensive patients in the first 3 months, during which visual fluctuations may be expected. Furthermore, it may be ideal to study the correlation of clinical grading described in our study with corresponding changes in the interface using IVCM in future prospective studies.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Blum M, Kunert KS, Engelbrecht C, Dawczynski J, Sekundo W. Femtosecond lenticule extraction (FLEx) – Results after 12 months in myopic astigmatism. Klin Monbl Augenheilkd. 2010;227:961–5. doi: 10.1055/s-0029-1245894. [DOI] [PubMed] [Google Scholar]
- 2.Lazaridis A, Droutsas K, Sekundo W. Topographic analysis of the centration of the treatment zone after SMILE for myopia and comparison to FS-LASIK: Subjective versus objective alignment. J Refract Surg. 2014;30:680–6. doi: 10.3928/1081597X-20140903-04. [DOI] [PubMed] [Google Scholar]
- 3.Sekundo W, Kunert KS, Blum M. Small incision corneal refractive surgery using the small incision lenticule extraction (SMILE) procedure for the correction of myopia and myopic astigmatism: Results of a 6 month prospective study. Br J Ophthalmol. 2011;95:335–9. doi: 10.1136/bjo.2009.174284. [DOI] [PubMed] [Google Scholar]
- 4.Ivarsen A, Asp S, Hjortdal J. Safety and complications of more than 1500 small-incision lenticule extraction procedures. Ophthalmology. 2014;121:822–8. doi: 10.1016/j.ophtha.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 5.Ganesh S, Gupta R. Comparison of visual and refractive outcomes following femtosecond laser- assisted lasik with smile in patients with myopia or myopic astigmatism. J Refract Surg. 2014;30:590–6. doi: 10.3928/1081597X-20140814-02. [DOI] [PubMed] [Google Scholar]
- 6.Miao H, Tian M, Xu Y, Chen Y, Zhou X. Visual outcomes and optical quality after femtosecond laser small incision lenticule extraction: An 18-month prospective study. J Refract Surg. 2015;31:726–31. doi: 10.3928/1081597X-20151021-01. [DOI] [PubMed] [Google Scholar]
- 7.Jin Y, Wang Y, Xu L, Zuo T, Li H, Dou R, et al. Comparison of the optical quality between small incision lenticule extraction and femtosecond laser LASIK. J Ophthalmol. 2016;2016:2507973. doi: 10.1155/2016/2507973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kamiya K, Shimizu K, Igarashi A, Kobashi H. Time course of optical quality and intraocular scattering after refractive lenticule extraction. PLoS One. 2013;8:e76738. doi: 10.1371/journal.pone.0076738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kamiya K, Shimizu K, Igarashi A, Kobashi H. Effect of femtosecond laser setting on visual performance after small-incision lenticule extraction for myopia. Br J Ophthalmol. 2015;99:1381–7. doi: 10.1136/bjophthalmol-2015-306717. [DOI] [PubMed] [Google Scholar]
- 10.Miao H, He L, Shen Y, Li M, Yu Y, Zhou X, et al. Optical quality and intraocular scattering after femtosecond laser small incision lenticule extraction. J Refract Surg. 2014;30:296–302. doi: 10.3928/1081597X-20140415-02. [DOI] [PubMed] [Google Scholar]
- 11.Yao P, Zhao J, Li M, Shen Y, Dong Z, Zhou X, et al. Microdistortions in bowman's layer following femtosecond laser small incision lenticule extraction observed by fourier-domain OCT. J Refract Surg. 2013;29:668–74. doi: 10.3928/1081597X-20130806-01. [DOI] [PubMed] [Google Scholar]
- 12.Luo J, Yao P, Li M, Xu G, Zhao J, Tian M, et al. Quantitative analysis of microdistortions in bowman's layer using optical coherence tomography after SMILE among different myopic corrections. J Refract Surg. 2015;31:104–9. doi: 10.3928/1081597X-20150122-05. [DOI] [PubMed] [Google Scholar]
- 13.Shetty R, Shroff R, Kaweri L, Jayadev C, Kummelil MK, Sinha Roy A, et al. Intra-operative cap repositioning in small incision lenticule extraction (SMILE) for enhanced visual recovery. Curr Eye Res. 2016;41:1532–8. doi: 10.3109/02713683.2016.1168848. [DOI] [PubMed] [Google Scholar]
- 14.Shroff R, Francis M, Pahuja N, Veeboy L, Shetty R, Sinha Roy A, et al. Quantitative evaluation of microdistortions in Bowman's layer and corneal deformation after small incision lenticule extraction. Transl Vis Sci Technol. 2016;5:12. doi: 10.1167/tvst.5.5.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Blum M, Kunert K, Schröder M, Sekundo W. Femtosecond lenticule extraction for the correction of myopia: Preliminary 6-month results. Graefes Arch Clin Exp Ophthalmol. 2010;248:1019–27. doi: 10.1007/s00417-009-1293-1. [DOI] [PubMed] [Google Scholar]
- 16.Vestergaard A, Ivarsen A, Asp S, Hjortdal JØ. Femtosecond (FS) laser vision correction procedure for moderate to high myopia: A prospective study of ReLEx(®) flex and comparison with a retrospective study of FS-laser in situ keratomileusis. Acta Ophthalmol. 2013;91:355–62. doi: 10.1111/j.1755-3768.2012.02406.x. [DOI] [PubMed] [Google Scholar]
- 17.Sekundo W, Kunert K, Russmann C, Gille A, Bissmann W, Stobrawa G, et al. First efficacy and safety study of femtosecond lenticule extraction for the correction of myopia: Six-month results. J Cataract Refract Surg. 2008;34:1513–20. doi: 10.1016/j.jcrs.2008.05.033. [DOI] [PubMed] [Google Scholar]
- 18.Agca A, Ozgurhan EB, Yildirim Y, Cankaya KI, Guleryuz NB, Alkin Z, et al. Corneal backscatter analysis by in vivo confocal microscopy: Fellow eye comparison of small incision lenticule extraction and femtosecond laser-assisted LASIK. J Ophthalmol. 2014;2014:265012. doi: 10.1155/2014/265012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Knox Cartwright NE, Tyrer JR, Jaycock PD, Marshall J. Effects of variation in depth and side cut angulations in LASIK and thin-flap LASIK using a femtosecond laser: A biomechanical study. J Refract Surg. 2012;28:419–25. doi: 10.3928/1081597X-20120518-07. [DOI] [PubMed] [Google Scholar]
- 20.de Medeiros FW, Kaur H, Agrawal V, Chaurasia SS, Hammel J, Dupps WJ, Jr, et al. Effect of femtosecond laser energy level on corneal stromal cell death and inflammation. J Refract Surg. 2009;25:869–74. doi: 10.3928/1081597X-20090917-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Riau AK, Angunawela RI, Chaurasia SS, Lee WS, Tan DT, Mehta JS, et al. Early corneal wound healing and inflammatory responses after refractive lenticule extraction (ReLEx) Invest Ophthalmol Vis Sci. 2011;52:6213–21. doi: 10.1167/iovs.11-7439. [DOI] [PubMed] [Google Scholar]
- 22.Bottos KM, Leite MT, Aventura-Isidro M, Bernabe-Ko J, Wongpitoonpiya N, Ong-Camara NH, et al. Corneal asphericity and spherical aberration after refractive surgery. J Cataract Refract Surg. 2011;37:1109–15. doi: 10.1016/j.jcrs.2010.12.058. [DOI] [PubMed] [Google Scholar]
- 23.Güell JL, Pujol J, Arjona M, Diaz-Douton F, Artal P. Optical quality analysis system; instrument for objective clinical evaluation of ocular optical quality. J Cataract Refract Surg. 2004;30:1598–9. doi: 10.1016/j.jcrs.2004.04.031. [DOI] [PubMed] [Google Scholar]
- 24.Kobashi H, Kamiya K, Yanome K, Igarashi A, Shimizu K. Longitudinal assessment of optical quality and intraocular scattering using the double-pass instrument in normal eyes and eyes with short tear breakup time. PLoS One. 2013;8:e82427. doi: 10.1371/journal.pone.0082427. [DOI] [PMC free article] [PubMed] [Google Scholar]