Abstract
Purpose:
The purpose of this study is to evaluate the effect of transfer of donor corneal tissue from McCarey–Kaufmann (MK) medium to Optisol-GS on corneal endothelium.
Methods:
This was a prospective, randomized comparative study. Twenty paired human donor corneal tissues of optical quality were retrieved. One tissue of the pair was preserved in Optisol-GS preservative medium (Group A) and other tissue of the pair in MK medium (Group B) at the time of corneoscleral disc excision. Within 12 h of retrieval, each cornea was evaluated using slit-lamp biomicroscopic examination and specular microscopic analysis. Group B corneas were transferred to Optisol-GS medium within 48–53 h of retrieval. Specular analysis of the paired corneas was repeated 3 h after transferring to Optisol-GS. On day 7 of storage, specular analysis of both the tissues was repeated.
Results:
The average age of the donor at the time of death was 29 years (16–68 years). The reduction in endothelial cell count, from baseline, in Groups A and B was 5.5% and 5.8% (P = 0.938) on the 3rd day and 8.2% and 12.6% (P = 0.025) on the 7th day, respectively, postretrieval. The coefficient of variation (CV) increased by 36% (P = 0.021) and hexagonality reduced by 19% (P = 0.007) on day 7. All tissues retained an endothelial cell density higher than the accepted critical level for penetrating keratoplasty.
Conclusion:
Significant endothelial cell loss was noted while transferring tissues from one medium to another, necessitating the need for reevaluation of transferred tissues before utilization.
Keywords: Corneal endothelium, McCarey Kaufmann medium, Optisol-GS
Worldwide, there are about 4.9 million bilaterally corneal blind persons.[1] Corneal transplantation can cause a significant impact on corneal blindness. Corneal tissues are preserved in tissue storage media after procuring from the deceased donor till they are utilized for surgery. Short-term storage media, such as McCarey–Kaufmann medium (MK medium), have been popular in developing countries, due to long waiting lists for surgery. Earlier, patients were always available for surgery within 24–48 h.[2,3,4,5,6,7] Intermediate-term storage media such as Optisol-GS[8,9,10] (Chiron Vision, Irvine, CA, USA), though relatively expensive, are gaining popularity. Donor corneal tissues can be preserved in MK medium and Optisol-GS for 4 and 14 days, respectively.[2,8,11,12] On an average, the reported endothelial cell loss is 9.5% for Optisol-GS medium stored corneas at the end of 1 week.[13]
In the recent past, in developing countries like India, there has been an exponential increase in corneal tissue collection by a few eye banks.[14] These eye banks collect more tissue for transplantation than the corneal surgeons in the area can utilize. MK medium (approximately 6$) is cheaper than Optisol-GS (approximately 85$). Thus, eye banks continue to place the procured corneal tissue in MK medium initially. The need for increasing the duration of tissue storage is felt when the tissue has to be transported to areas beyond the local area of tissue collection to increase the viability of the corneal tissue for a longer duration.
Previously, transfer of tissue from MK medium to organ culture is reported[15] and has not shown a deleterious effect on the endothelium by electron microscopy. To the best of our knowledge, this study is the first to provide us data for evaluating the effectiveness and safety of transferring corneal tissue from MK Medium to Optisol-GS medium.
Methods
A prospective, randomized study was conducted at a tertiary care eye hospital, New Delhi, India. The study protocol was approved by the institutional review board. The study period was from January 2015 to November 2015.
Twenty pairs of human cornea were retrieved from phakic donors between 3 years to 80 years of age within 6 h of death. The guidelines of Eyebank Association of India (EBAI) were followed during all cornea retrievals. In situ excision of corneoscleral disc was performed, and the procured tissue was placed in the preservative medium. This study comprised of two groups. Group A (Optisol-GS Group) contained corneal tissue collected in 20 ml Optisol-GS. Group B (MK medium group) contained corneal tissue collected in 20 ml MK medium. MK medium was procured from Ramayamma Eye Bank, Hyderabad. Optisol-GS was provided by Sightlife India[16] for the purpose of the study. Both tissues were stored at 4°C. Donor details included age, sex, cause of death, and death to preservation time. Seropositive donors for HIV, Hepatitis B, Hepatitis C, or VDRL were excluded from the study. Donor corneas with visible corneal pathologies, history of ocular disease or intraocular surgery, tissues with endothelial damage, unclear specular image, or any contraindications as per EBAI were also excluded from the study.
One cornea from each pair was randomly assigned to Group A and the other one to Group B. Within 12 h of retrieval; each cornea was evaluated using slit-lamp biomicroscopy and specular microscopic analysis. Slit-lamp evaluation comprised an assessment of all layers of the donor cornea from anterior to posterior. Epithelium was assessed for defects, exposure, sloughing, and any debris. Stroma was evaluated for arcus, presence and location of edema, scars, striae and infiltrates. Severity and number of Descemet membrane folds were noted. Endothelium was evaluated on slit lamp on the basis of stress lines and areas of cell dropouts.
Specular microscopy gives a quantifiable assessment of the corneal endothelium. Cell density was recorded as the number of cells per square millimeter. The quantitative endothelial analysis from specular photographs was performed from the endothelial side by digitizing the apices of 100 cells per fixed frame with Konan eye bank specular microscope (Model EKA-10). Serial values of endothelial cell density (ECD), Coefficient of variation (CV), and percentage of hexagonal cells (HEX) was noted on each specular image. ECD was calculated as a mean of three fixed frame analysis of endothelial mosaic and expressed as number of cells per square millimeter area. Endothelial cell loss was calculated as the difference from baseline ECD expressed as a percentage of the baseline density. Coefficient of Variation (standard deviation divided by the mean cell area) was used as an index of the extent of variation in cell area (polymegethism). Pleomorphism, variation in cell shape, was determined by the percentage of HEX cells in the fixed frame (HEX). Baseline endothelial photographs were obtained for each corneal tissue using Konan eye bank specular microscope.
The donor corneas were graded as excellent, good, or fair based on the slit-lamp examination and specular microscopy.[17] MK medium stored corneal tissues were transferred to Optisol-GS medium within 48–53 h of retrieval. The upper time limit was decided to eliminate storage media induced endothelial cell loss in MK media.[15] The lower limit was chosen as 48 h because it is only by this time, that eye banks either utilize the tissue or feel the need to extend the storage life of the tissue by transferring to a longer-term storage medium.
The corneal tissue transfer from MK medium to Optisol-GS was done in an aseptic environment under laminar airflow by placing the tissue and MK medium into a sterile stainless steel bowl and holding the scleral rim of the corneoscleral disc with Castroviejo's forceps (IndoGerman Surgical Corporation, Mumbai, India) to place the tissue in a vial containing 20 ml Optisol-GS, epithelial side facing down. Endothelial evaluation on the 3rd day for both groups was repeated 3 h after transferring the Group B cornea to Optisol-GS, after warming it to room temperature for 1 h. On the 7th day of storage, the paired corneas were kept at room temperature for 1 h and then specular analysis was repeated.[18] To eliminate bias, all specular analysis was performed by the same evaluation technician.
Statistical Package for the Social Sciences software version 23 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. The difference between specular variables at different time interval was assessed using ANOVA. Post hoc analysis was done using Turkey's HSD method. To compare variables between the groups, paired t-test was applied. A probability of 0.05 or less was considered statistically significant.
Results
The mean age of the donors was 29 years (16–68 years). Causes of death in the enrolled group included hanging,[9] cardiorespiratory arrest,[6] and road traffic accidents.[5] The average death to preservation time was 215 min (90–345 min). Corneal tissues were retrieved from 6 males and 14 female donors. Due to a breach in the cold chain, one pair was excluded from the analysis from both study groups, and the remaining 19 donor tissues were analyzed. Morphologic assessment of the corneal tissues by slit-lamp examination included in the study was excellent on the 1st day and on the 7th day were either good or excellent.[17]
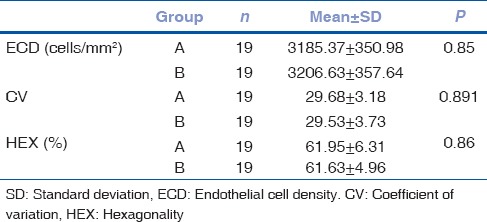
The average ECD in Group A and Group B was 3185 ± 350 cells/mm2 (range: 2551–3704) and 3206 ± 357 cells/mm2 (range: 2513–3831), respectively (P = 0.85). The mean CV in Group A and B was 29.7 and 29.5, respectively (P = 0.891). The average HEX of the corneas in Group A and B was 61.9% and 61.6%, respectively (P = 0.86). The tissues recruited for the study were matched at baseline for specular parameters [Table 1].
Table 1.
Baseline specular parameters in both groups
Within group A, the average endothelial cell loss from the baseline was 182 cells/mm2 (5.5%) on the 3rd day (P = 0.301) and 265 cells/mm2 (8.2%) on the 7th day (P = 0.079). CV increased from 29.7 at baseline to 32.8 on the 3rd day (P = 0.089) and increased from 29.7 at baseline to 36.4 on the 7th day (P < 0.001). HEX reduced from 61.9% at baseline to 57.4% on the 3rd day (P = 0.100) and from 61.9% at baseline to 56.1% on the 7th day (P = 0.029).
Within group B, the average endothelial cell loss from the baseline was 188 cells/mm2 (5.8%) on the 3rd day (P = 0.231) and 408 cells/mm2 (12.6%) on the 7th day (P < 0.001). CV increased from 29.5 at baseline to 34.4 on the 3rd day (P = 0.010) and increased from 29.5 at baseline to 40.1 on the 7th day (P < 0.001). HEX reduced from 61.6% at baseline to 54.2% on the 3rd day (P < 0.001) and from 61.6% at baseline to 49.7% on the 7th day (P < 0.001).
Comparing the tissues in group A with group B on the 3rd day, the reduction in endothelial cell count was 5.5% and 5.8%, respectively (P = 0.938). The coefficient of variation increased by 11.2% and 17.2% in groups A and B, respectively (P = 0.179). The HEX reduced by 7.3% and 11.6%, respectively, in Groups A and B (P = 0.091) [Table 2].
Table 2.
Comparative specular parameters between Groups A and B
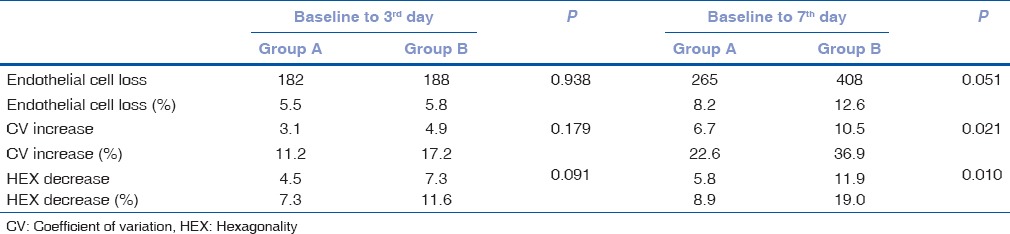
On comparing the tissues in Groups A and B on the 7th day, the reduction in endothelial cell count was 8.2% and 12.6%, respectively (P = 0.051). The coefficient of variation increased by 22.6% and 36.9% in Groups A and B, respectively (P = 0.021). The HEX reduced by 8.9% and 19.0%, respectively, in Groups A and B (P = 0.010) [Table 2].
The average ECD on the 7th day was 2870 cells/mm2 (range: 2427–3356) in Group A and 2734 cells/mm2 (range: 2227–3610) in Group B. All tissues retained a final cell count higher than 2200 cells/mm2 which is the critical acceptable count for penetrating keratoplasty.[19]
All tissues recruited in the study were utilized for penetrating keratoplasty. No adverse events or primary graft failure were noted with any of the above-studied tissues.
Discussion
Our study aimed to assess the effect of corneal tissue transfer from MK medium to Optisol-GS on the tissue endothelium. We noted that there was a reduction in endothelial cell count and worsening of morphological parameters with the passage of time in all study corneas. This was significant on the 7th-day assessment in the corneas transferred from MK medium to Optisol-GS in comparison to tissues that were initially stored in Optisol-GS media.
The endothelial cell loss in Group A corneas of 8.2% on the 7th day in our study is similar to earlier studies that report <10% ECD in Optisol-GS stored tissue.[13,20,21,22] We observed an endothelial cell loss of 5.8% in Group B corneas on the 3rd day. Van Horn et al.[23] have shown that corneas stored in MK medium have about 10% cell loss after 2–4 days of storage. The increase in cell size is due to the migration and spreading of surrounding endothelial cells to compensate for cell loss during storage. Endothelial cell loss in both the groups in our study compared well with other studies in having <10% cell loss in the storage period studied.[13,24] Optisol-GS scores over MK medium in being able to maintain endothelial cell viability for a longer duration.
Improvement in eye banking practices in the recent past has resulted in exponential increase in availability of corneal tissue in some eye banks in India.[14] The need for intermediate-term storage is being felt as waiting lists for keratoplasty have shrunk, and tissues are being distributed beyond the local area of collection. Cost of Optisol-GS is more than ten times the cost of locally produced MK medium. Therefore, the practice of procuring the corneal tissue and initially placing in MK medium continues. Tissues are transferred to intermediate storage only when in the first 48 h a home to the tissue is not found in the local area of the eye bank. Group B corneas were transferred to Optisol-GS medium in 48–53 h to simulate the time at which tissues are normally transferred.
Our study demonstrated that Group B tissues after transfer from MK medium to Optisol-GS showed significant reduction in endothelial cell count and worsening of morphological parameters of CV and HEX. The greater cell loss in the corneas transferred from MK medium to Optisol-GS can be attributed to mechanical cell loss during transfer of tissue from one medium to another. Bending and folding of cornea also result in endothelial cell loss.[25] This “mechanical trauma” hypothesis could be tested by transferring corneas stored initially in Optisol-GS to fresh Optisol-GS. Transfer of corneas from MK medium to Optisol-GS to prolong their viability is followed in developing countries as a cost-saving measure. Our study questions the safety of the practice of tissue transfer from one medium to another.
All tissues in our study retained a final endothelial cell count higher than the critically accepted endothelial cell count for penetrating keratoplasty, despite significant reduction of the endothelial health of corneas being transferred from MK medium to Optisol-GS. No adverse events were reported with any patients after utilization of tissues for surgery. The good outcomes may be attributed to recruitment of cases with very good endothelium in both groups (average above 3000 cells/mm2).[26] Our study recommends need to reevaluate these corneal tissues before utilization for keratoplasty. A small number of corneas have been recruited for the study, and we would recommend a greater sample size to elucidate the results.
Conclusion
All tissues retained a cell count higher than the acceptable level for penetrating keratoplasty. The changes noted in the specular parameters indicate the need for reevaluation of transferred tissues before utilization.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Oliva MS, Schottman T, Gulati M. Turning the tide of corneal blindness. Indian J Ophthalmol. 2012;60:423–7. doi: 10.4103/0301-4738.100540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Van Horn DL, Schultz RO, DeBruin J. Endothelial survival in corneal tissue stored in M-K medium. Am J Ophthalmol. 1975;80:642–7. doi: 10.1016/0002-9394(75)90395-5. [DOI] [PubMed] [Google Scholar]
- 3.Maurice DM. The cornea and sclera. In: Davson H, editor. The Eye. 3rd ed. San Diego: Academic Press; 1984. pp. 75–89. [Google Scholar]
- 4.Kerr JF, Bishop CJ, Searle J. Apoptosis. Recent Adv Histopathol. 1984;12:1–15. [Google Scholar]
- 5.Bourne WM, Hodge DO, Nelson LR. Corneal endothelium five years after transplantation. Am J Ophthalmol. 1994;118:185–96. doi: 10.1016/s0002-9394(14)72898-3. [DOI] [PubMed] [Google Scholar]
- 6.Komuro A, Hodge DO, Gores GJ, Bourne WM. Cell death during corneal storage at 4 degrees C. Invest Ophthalmol Vis Sci. 1999;40:2827–32. [PubMed] [Google Scholar]
- 7.NPCB. Standards of Eye Banking in India. 2009 [Google Scholar]
- 8.Lindstrom RL, Kaufman HE, Skelnik DL, Laing RA, Lass JH, Musch DC, et al. Optisol corneal storage medium. Am J Ophthalmol. 1992;114:345–56. doi: 10.1016/s0002-9394(14)71803-3. [DOI] [PubMed] [Google Scholar]
- 9.Walkenbach RJ, Boney F, Ye G. Corneal function after storage in Dexsol or Optisol-GS. Invest Ophthalmol Vis Sci. 1992;33:2454–8. [PubMed] [Google Scholar]
- 10.Lass JH, Bourne WM, Musch DC, Sugar A, Gordon JF, Reinhart WJ, et al. A randomized, prospective, double-masked clinical trial of Optisol-GS vs. DexSol corneal storage media. Arch Ophthalmol. 1992;110:1404–8. doi: 10.1001/archopht.1992.01080220066022. [DOI] [PubMed] [Google Scholar]
- 11.Basu PK. A review of methods for storage of corneas for keratoplasty. Indian J Ophthalmol. 1995;43:55–8. [PubMed] [Google Scholar]
- 12.Kaufman HE, Beuerman RW, Steinemann TL, Thompson HW, Varnell ED. Optisol corneal storage medium. Arch Ophthalmol. 1991;109:864–8. doi: 10.1001/archopht.1991.01080060128040. [DOI] [PubMed] [Google Scholar]
- 13.Means TL, Geroski DH, Hadley A, Lynn MJ, Edelhauser HF. Viability of human corneal endothelium following Optisol-GS storage. Arch Ophthalmol. 1995;113:805–9. doi: 10.1001/archopht.1995.01100060131047. [DOI] [PubMed] [Google Scholar]
- 14.Sangwan VS, Gopinathan U, Garg P. Eye banking in India: A road ahead. JIMSA. 2010;23:197–200. [Google Scholar]
- 15.Nelson JD, Lange DB, Lindstrom RL, Doughman DJ, Hatchell DL. McCarey-Kaufman (MK) organ culture and MK medium-shifted corneas. Arch Ophthalmol. 1984;102:308–11. doi: 10.1001/archopht.1984.01040030252036. [DOI] [PubMed] [Google Scholar]
- 16.SightLife. [Last accessed on 2017 Jul 31]. Available from: https://www.sightlife.org/
- 17.Joshi SA, Jagdale SS, More PD, Deshpande M. Outcome of optical penetrating keratoplasties at a tertiary care eye institute in Western India. Indian J Ophthalmol. 2012;60:15–21. doi: 10.4103/0301-4738.91337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rootman DS, Hasany SM, Basu PK. A morphometric study of endothelial cells of human corneas stored in McCarey-Kaufman media and warmed at 37°C. Br J Ophthalmol. 1988;72:545–9. doi: 10.1136/bjo.72.7.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wakefield MJ, Armitage WJ, Jones MN, Kaye SB, Larkin DF, Tole D, et al. The impact of donor age and endothelial cell density on graft survival following penetrating keratoplasty. Br J Ophthalmol. 2016;100:986–9. doi: 10.1136/bjophthalmol-2015-306871. [DOI] [PubMed] [Google Scholar]
- 20.Sibayan SA, Garcia-Arenal CP, Corpus KD, Manlongat RG, Ibanez MB, Padilla DB, et al. Serial endothelial cell count of donor corneal buttons in Optisol-GS-GS. Procedia Chem. 2015;14:394–7. [Google Scholar]
- 21.Chen CH, Rama P, Chen AH, Franch A, Sulewski M, Orlin S, et al. Efficacy of media enriched with nonlactate-generating substrate for organ preservation: In vitro and clinical studies using the cornea model. Transplantation. 1999;67:800–8. doi: 10.1097/00007890-199903270-00004. [DOI] [PubMed] [Google Scholar]
- 22.Basak S, Prajna NV. A prospective, in vitro, randomized study to compare two media for donor corneal storage. Cornea. 2016;35:1151–5. doi: 10.1097/ICO.0000000000000912. [DOI] [PubMed] [Google Scholar]
- 23.Van Horn DL, Schultz RO, De Bruin J. Endothelial survival in corneal tissue stored in Mc Carey-Kaufman media. Am J Ophthalmol. 1975;80:642–7. doi: 10.1016/0002-9394(75)90395-5. [DOI] [PubMed] [Google Scholar]
- 24.Nelson LR, Hodge DO, Bourne WM. In vitro comparison of Chen medium and Optisol-GS medium for human corneal storage. Cornea. 2000;19:782–7. doi: 10.1097/00003226-200011000-00005. [DOI] [PubMed] [Google Scholar]
- 25.Halberstadt M, Athmann S, Winter R, Hagenah M. Impact of transportation on short-term preserved corneas preserved in Optisol-GS, Likorol, Likorol-DX, and MK-medium. Cornea. 2000;19:788–91. doi: 10.1097/00003226-200011000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Gal RL, Dontchev M, Beck RW, Mannis MJ, Holland EJ, et al. Cornea Donor Study Investigator Group. The effect of donor age on corneal transplantation outcome results of the cornea donor study. Ophthalmology. 2008;115:620–6. doi: 10.1016/j.ophtha.2008.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]


