Abstract
Purpose:
The purpose of the study was to evaluate tissue reaction to polycaprolactone (PCL) nanofiber patches in the cornea, conjunctiva, and anterior chamber (AC) in rabbit eyes and to assess their biocompatibility for use as patch grafts.
Methods:
Two 100 μ PCL patches were implanted under the conjunctiva and in the corneal stroma of one albino New Zealand rabbit, and pathologic evaluation was done after 3 weeks. In the next step, two PCL patches were implanted; one in the corneal stroma and the other in the AC of two rabbits followed by pathologic evaluation after 3 months.
Results:
On slit-lamp examination, there was minimum inflammation in all cases. Pathologic examination showed that the contact and probably merging between the host tissue and PCL fibers were achieved with minimal tissue reaction.
Conclusion:
As a biocompatible material, PCL nanofibers seem to be a promising modality for the repair of different tissue defects including melting, thinning, and perforation. They may also be a suitable material for manufacturing keratoprostheses.
Keywords: Anterior chamber, conjunctiva, cornea, inflammation, polycaprolactone nanofiber
Today, the cornea, sclera, and amniotic membrane are used for repairing sclera and corneal thinning, and perforation caused by trauma, infections, inflammation, and rheumatologic diseases. However, using them as patch grafts is not only associated with difficulties in production and maintenance but also they carry risks related to the use of biologic materials such as infection and tissue interactions.
Various synthetic materials such as Dacron, Gore-Tex soft-tissue patch, and MIRAgel have been evaluated as potential substitutes for biologic materials, but they have not been approved for use in ophthalmology due to lack of biocompatibility and failure to integrate with host tissue, untimely degradation, undesirable molding, and risk of toxicity or carcinogenicity.[1,2,3]
Polycaprolactone (PCL) is made of nanofibers for better merging and acceptable integrity with body tissues. Use of biocompatible, biodegradable, and nontoxic polymers instead of biologic materials not only has the advantage of better accessibility but also reduced risk of infections and tissue incompatibility. Furthermore, the nanofiber structure of this polymer and its lengthy degradation in the body as compared to the sclera and amnion can stimulate the growth of the adjacent tissue to provide ample time for the repair of the superficial ocular lesions.
Considering the white color of the PCL nanofiber and its staining properties, it may be used in cosmetic procedures such as treatment for ocular melanocytosis and scleral reinforcement to prevent the progression of myopia.[4,5,6,7,8]
In this study, we examined tissue reaction to PCL nanofiber patches and its biocompatibility for use as a patch graft.
Methods
Tehran University of Medical Sciences approved this study. The study adhered to the Association for Research in Vision and Ophthalmology Statement for the Use of Animals in Ophthalmic and Vision Research.
PCL nanofiber patches of mid-density and 100 μm thickness were implanted in the eyes of three albino New Zealand rabbits. The right eyes were treated as cases, and the left eyes were considered their controls.
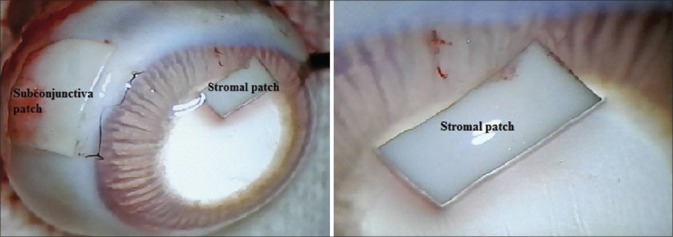
The study was done in two stages. In the first stage, two PCL patches were implanted in the right eye of rabbit A; one under the conjunctiva and one in the corneal stroma. For this purpose, we first created a limbal peritomy and a pocket at half the corneal thickness into which a 3 mm × 4 mm PCL patch was inserted. Then, Tenon's layer was dissected at the peritomy site, and a 5 mm × 7 mm patch was inserted under the conjunctiva. Finally, the limbal incision and the peritomy site were sutured with 10/0 nylon, and blepharorrhaphy was done. This rabbit was sacrificed 3 weeks after surgery, and the enucleated eyes were fixed immediately in 10% buffered formalin and submitted for routine histopathologic evaluation. Sections containing the implanted PCL in the cornea and conjunctiva were embedded. The dehydration process was performed using various concentrations of ethanol, followed by treatment with xylol. Paraffin blocks were prepared, and 3–5 μm sections were examined after hematoxylin and eosin (H and E) staining [Fig. 1].
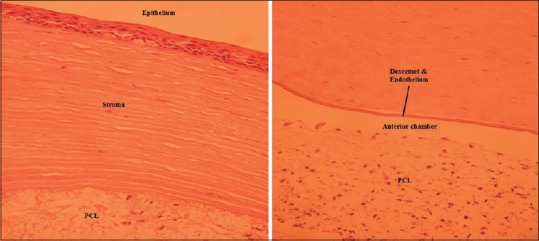
Figure 1.
Enucleated eye of rabbit A, 3 weeks after patch implantation in the corneal stroma and subconjunctival (left) and the magnified view of the corneal stromal patch (right)
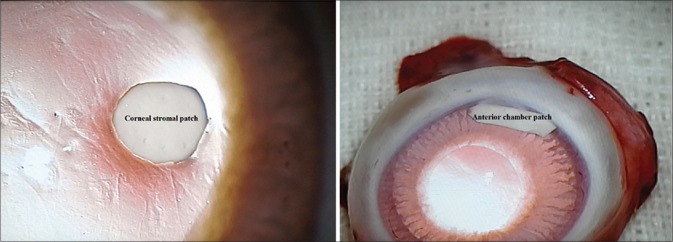
For the second stage, two rabbits (B and C) were chosen. The right eye of rabbit B was treated as the first stage and was implanted with a PCL patch at one-thirds of the corneal thickness. In the right eye of rabbit C, we placed a 2 mm × 4 mm PCL patch in the anterior chamber (AC) on the iris through a stab incision, and blepharorrhaphy was done after the incision was repaired with 10/0 nylon. The eyes of rabbits B and C were enucleated after 3 months and assessed by both frozen section and routine histopathologic methods [Fig. 2]. For frozen section study, specimens were cut immediately and frozen at −24°C. The prepared 5 μm slides were stained with H and E. Then, the remaining samples were fixed in 10% buffered formalin and submitted for routine histopathologic processing, as described for rabbit A. It should be noted that chloramphenicol drops were instilled every 6 h for 3 days after PCL implantation in all three rabbits, and no steroidal or nonsteroidal anti-inflammatory medications were used.
Figure 2.
The corneal stromal patch of rabbit B (left) and anterior chamber patch of rabbit C (right) 3 months after implantation with no signs of inflammatory reaction
To examine the effect of different tissue processing methods on PCL and compare possible changes in PCL fibers in the ocular tissue, samples of PCL were assessed using frozen section and also the routine histopathological methods. Eventually, stained slides of the right eyes of all three rabbits were separately examined by light microscopy. Furthermore, the paraffin block of the right eye of rabbit B underwent immunohistochemical (IHC) examination (EnVision, DAKO, Denmark) with CD45 and CD34 markers, and immunoperoxidase reaction was assessed through light microscopic examination.
Results
According to repeated examinations at the slit-lamp and a surgical microscope, all rabbit eyes were completely quiet with no evidence of reaction or inflammation in the conjunctiva, cornea, or AC. In the microscopic slides of rabbit A, no sign of PCL fibers was visible, and the PCL site appeared as an empty space around which a mild lymphocytic inflammatory reaction could be seen. The inflammatory reaction was slightly more severe with the conjunctival piece than the intracorneal one, but neither one showed any sign of epithelioid cell proliferation which is a typical reaction to foreign bodies. Furthermore, the tissue structure of the adjacent stroma was well preserved [Fig. 3].
Figure 3.
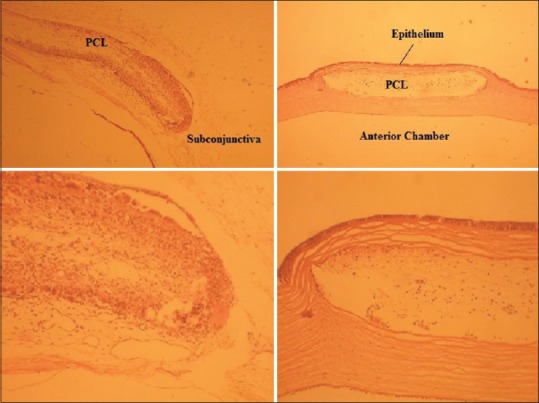
Routine histopathologic slides of the subconjunctival patch (upper left) and corneal stromal patch (upper right) in rabbit A and their magnified views (lower left and lower right, respectively). Images illustrate the infiltration of host cells through nanofibers
In case of rabbits B and C, PCL fibers were visible in microscopic slides prepared with the frozen section method, but there was no sign of these fibers in those prepared by the routine histopathologic process, and the PCL site appeared as an empty space. Inflammatory cell infiltration at the intracorneal PCL site of rabbit B and the adjacent stroma was similar to that seen in rabbit A. In rabbit C, the inflammatory reaction surrounding the PCL site in the AC was slightly greater than that with the intracorneal patch but seemed less than that seen with the subconjunctival patch in rabbit A. Similar to rabbit A, we observed no sign of foreign body reaction in rabbit B or C [Figs. 4 and 5].
Figure 4.
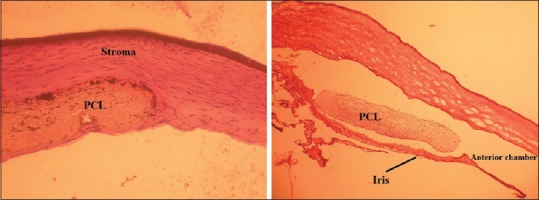
Frozen section slides of the corneal stromal patch in rabbit B (left) and anterior chamber patch in rabbit C (right)
Figure 5.
Histopathologic slides of the corneal stromal patch in rabbit B (left) and anterior chamber patch in rabbit C (right)
In the assessment of the unimplanted pieces of PCL, the sample processed by the routine procedure completely dissolved in xylol and no trace was left. Comparison of structural changes of unimplanted PCL with those implanted in rabbits B and C (observed with frozen section method) did not show any remarkable difference at the level of light microscopy. In the assessment of the slides prepared by IHC staining, all immigrated cells in between PCL fibers demonstrated nonspecific staining with both CD45 and CD34 markers [Fig. 6].
Figure 6.
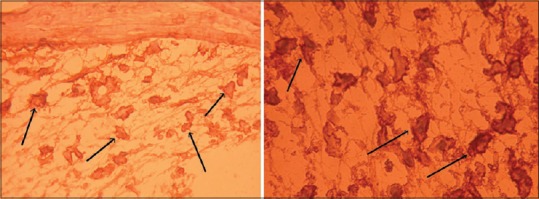
Immunohistochemical staining with CD45 (left) and CD34 (right) markers showing nonspecific staining of immigrated cells in between polycaprolactone fibers (corneal stromal patch of rabbit B)
Discussion
Review of the clinical and pathological findings of this study indicates the induction of weak antigenic properties and minimum stimulation of tissue reaction and inflammation (mostly lymphocytic) by PCL. Even in the subconjunctival sample in rabbit A which showed the worst reaction in the form of a moderate histiocytic reaction with accumulations of inflammatory giant cells, the classical foreign body reaction with epithelioid histiocytes was not seen, and the inflammatory reaction was far milder than a chalazion.
Our assessment of PCL fibers in frozen samples and their comparison with 3-week and 3-month implanted samples indicated that the immune system was unable to degrade and remove this material and that there was no sign of rapid hydrolysis in the short term.
Theoretically speaking, PCL nanofibers can imitate the structure of the extracellular matrix as a scaffold, promote adhesion, proliferation, and migration, and stimulate regeneration in damaged tissue. The weak inflammatory reaction and slow degradation of PCL on the one hand and the stimulation of regeneration on the other hand provide the opportunity for damaged cells of the ocular surface to heal tissue defects.[5,6,9] To discover the nature of cells among PCL fibers, we performed IHC staining with CD34 and CD45 markers which differentiate inflammatory cells and corneal keratocytes, respectively. However, there was no case of specific staining, and all cells had nonspecific staining. This is most probably due to the chemical properties induced by PCL, which interferes with proper staining of cells using a sensitive method such as IHC. Use of other diagnostic methods such as electron microscopy might help establish the possible migration of keratocytes among PCL fibers and the concept of tissue regeneration.
Conclusion
Preliminary results with PCL nanofibers in the eye seem to promise the emergence of a biocompatible matter with several applications including repair of different tissue defects caused by trauma, inflammation, infection, etc.; however, further research on its long-term effects and changes is necessary.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Tarutta EP, Andreeva LD, Markosian GA, Iomdina EN, Lazuk AV, Kruzhkova GV, et al. Reinforcement of the sclera with new types of synthetic materials in progressive myopia. Vestn Oftalmol. 1999;115:8–10. [PubMed] [Google Scholar]
- 2.Karesh JW, Fabrega MA, Rodrigues MM. Interpositional polytetrafluoroethylene grafts. Conjunctival biocompatibility. Ophthal Plast Reconstr Surg. 1991;7:278–83. doi: 10.1097/00002341-199112000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Whitmore WG, Harrison W, Curtin BJ. Scleral reinforcement in rabbits using synthetic graft materials. Ophthalmic Surg. 1990;21:327–30. [PubMed] [Google Scholar]
- 4.Reed CR, Han L, Andrady A, Caballero M, Jack MC, Collins JB, et al. Composite tissue engineering on polycaprolactone nanofiber scaffolds. Ann Plast Surg. 2009;62:505–12. doi: 10.1097/SAP.0b013e31818e48bf. [DOI] [PubMed] [Google Scholar]
- 5.Tiaw KS, Teoh SH, Chen R, Hong MH. Processing methods of ultrathin poly (epsilon-caprolactone) films for tissue engineering applications. Biomacromolecules. 2007;8:807–16. doi: 10.1021/bm060832a. [DOI] [PubMed] [Google Scholar]
- 6.Srouji S, Kizhner T, Suss-Tobi E, Livne E, Zussman E. 3-D nanofibrous electrospun multilayered construct is an alternative ECM mimicking scaffold. J Mater Sci Mater Med. 2008;19:1249–55. doi: 10.1007/s10856-007-3218-z. [DOI] [PubMed] [Google Scholar]
- 7.Kumbar SG, James R, Nukavarapu SP, Laurencin CT. Electrospun nanofiber scaffolds: Engineering soft tissues. Biomed Mater. 2008;3:034002. doi: 10.1088/1748-6041/3/3/034002. [DOI] [PubMed] [Google Scholar]
- 8.Más Estellés J, Vidaurre A, Meseguer Dueñas JM, Castilla Cortázar I. Physical characterization of polycaprolactone scaffolds. J Mater Sci Mater Med. 2008;19:189–95. doi: 10.1007/s10856-006-0101-2. [DOI] [PubMed] [Google Scholar]
- 9.van Aalst JA, Reed CR, Han L, Andrady T, Hromadka M, Bernacki S, et al. Cellular incorporation into electrospun nanofibers: Retained viability, proliferation, and function in fibroblasts. Ann Plast Surg. 2008;60:577–83. doi: 10.1097/SAP.0b013e318168db3e. [DOI] [PubMed] [Google Scholar]