Abstract
Purpose:
The purpose of this study is to describe the presenting features, management strategies, and clinical outcome following bee sting injury to the cornea.
Methods:
Retrospective case series involving 11 eyes of 11 patients with corneal bee sting injuries who presented over a period of 2 years. Nine of these 11 eyes had the presence of intact bee stinger in the cornea, which was removed immediately under an operating microscope and sent for microbiological and histopathological evaluation. The patients were managed as per the individual treatment protocol of the respective treating physicians.
Results:
Six eyes (54.5%) had a good clinical outcome (best-corrected visual acuity [BCVA] >20/40) with medical therapy alone with no need for surgical intervention. Five eyes (45.5%) had a poor clinical outcome (BCVA <20/40) with medical therapy and required surgery; of which three required a combined penetrating keratoplasty with cataract surgery, while one required isolated cataract surgery and one underwent penetrating keratoplasty. Glaucoma was present in 3/5 eyes undergoing surgery, one of which required a trabeculectomy. Five of the six eyes who had a good clinical outcome with medical therapy alone had been treated with concomitant oral steroids, along with topical antibiotic-steroid combination therapy.
Conclusion:
Oral corticosteroid supplementation to the topical steroid antibiotic treatment in patients with corneal bee sting injury where corneal involvement and anterior reaction is severe at presentation or inflammation not ameliorating with topical steroids alone prevents serious vision-threatening complications such as corneal decompensation, cataract, and glaucoma.
Keywords: Combined surgery, corneal bee sting, corneal decompensation, oral corticosteroids, penetrating keratoplasty
Bee sting injury to the cornea is a rare occurrence with a sequelae ranging from mild conjunctival hyperemia to intractable secondary glaucoma.[1] Apart from one case series of four eyes,[2] the rest of the literature consists of isolated case reports. Since this form of trauma is very rare, no widely accepted treatment regimen exists. We report the clinical outcome of treatment strategies in patients with corneal bee sting injury, which allows comparison of the existing treatment modalities.
Methods
This is a retrospective case series of 11 eyes of 11 patients with a corneal bee sting injury, managed by five different attending physicians at Aravind Eye Hospital, Madurai, India, over a period of 2 years (2011–2013). In view of the absence of any existing accepted protocol for this rare condition, each patient was treated as per the discretion of the treating physician.
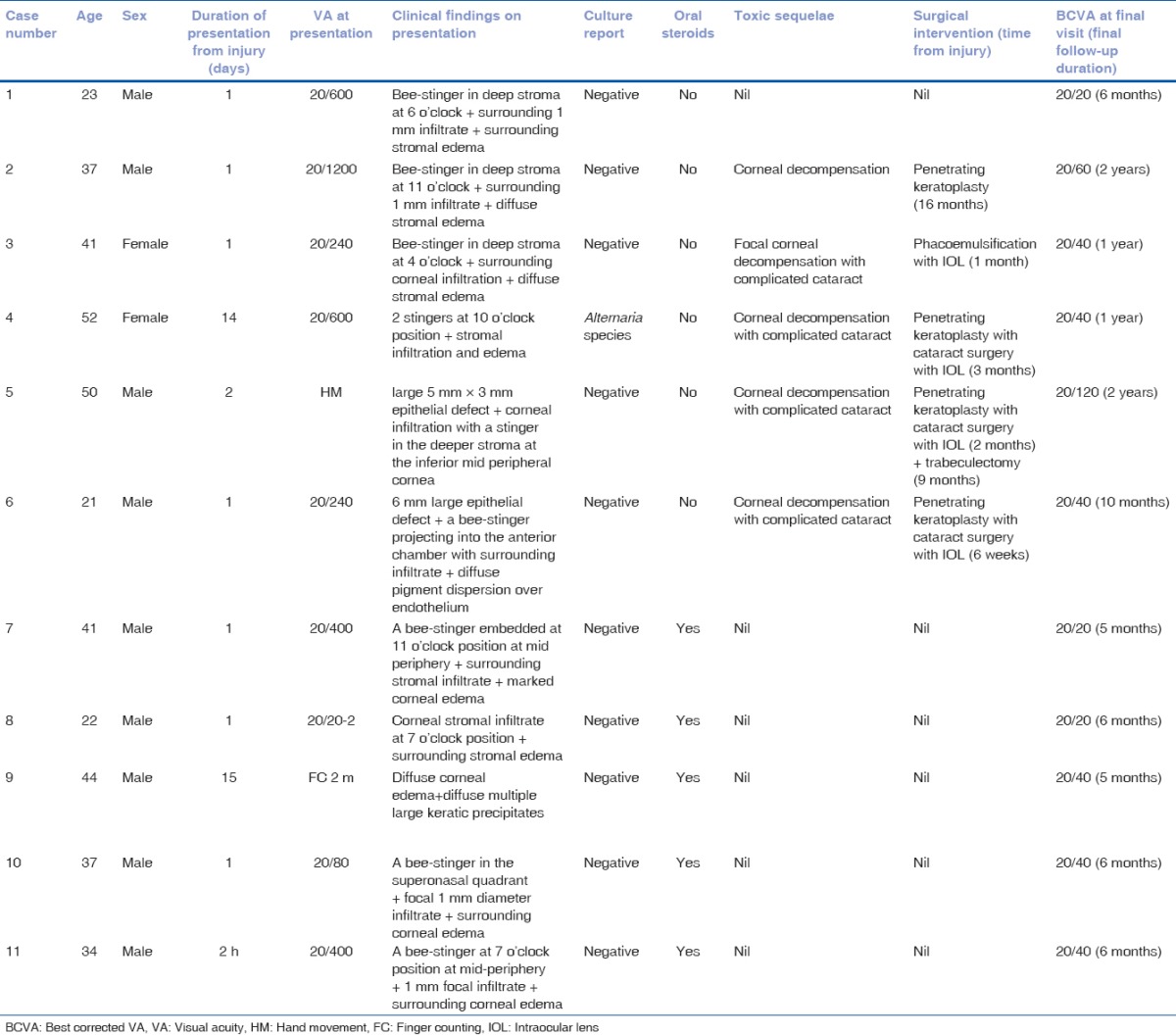
The bee stinger, if present during the slit lamp examination was removed as a uniform practice, with strict aseptic conditions under an operating microscope using topical anesthesia. The corneal entry wound was extended slightly with a side port blade. A 26 G needle was used to dislodge and hook the stinger out, and finally, it was plucked out with a Jewellers Forcep and sent for microbiological evaluation by plating on blood agar and histopathological examination [Fig. 1a]. In addition, all the eyes were treated with a combination of topical antibiotic and steroid therapy. The clinical sequelae and the adjuvant treatment strategies have been described on a case by case basis. The demographic description and treatment summary has been compiled in Table 1.
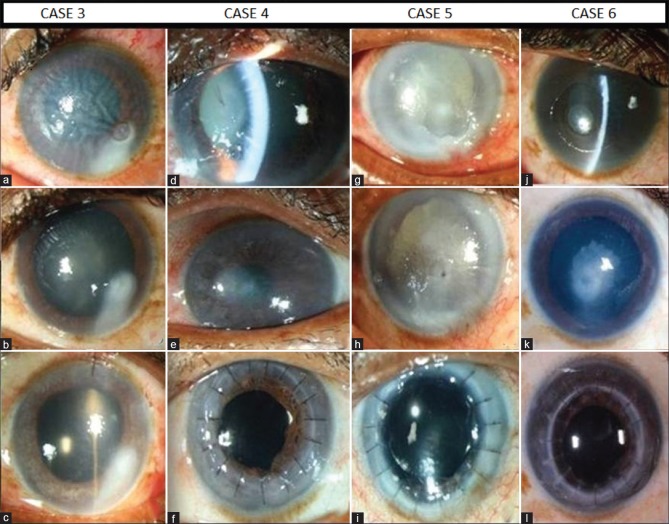
Figure 1.
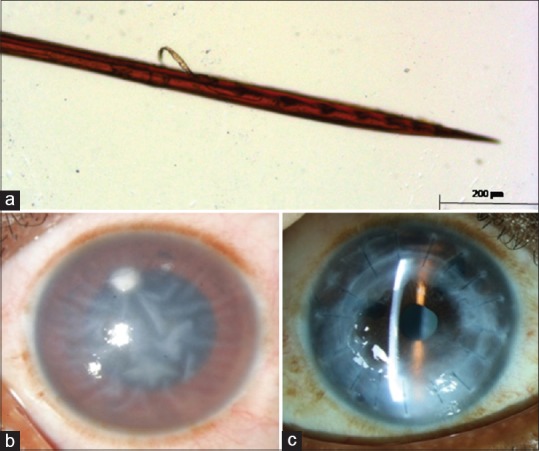
(a) Histopathological examination of the bee-stinger. (b) Clinical picture of case 2 at presentation showing diffuse corneal edema with infiltrate at the site of the bee sting (c) Clinical picture of case 2 after penetrating keratoplasty
Table 1.
Demographic and clinical summary
Results
Case 1
A 23-year-old male presented with a history of bee sting injury followed by defective vision, pain and redness in his left eye for 1 day. Left eye best-corrected visual acuity (BCVA) was 20/600. On slit lamp examination, the cornea showed a bee stinger in the anterior stroma at 6'0 clock surrounded by infiltration with diffuse stromal edema in the left eye. After stinger removal moxifloxacin 0.5% and dexamethasone 0.1% combination eye drops were started for 6 times a day. In 1 week, the BCVA improved to 20/40 with marked resolution of the corneal signs. Topical antibiotic-steroid eye drops were gradually tapered over 6 weeks. By then the lesion completely resolved with a faint scar and the BCVA further improved to 20/20.
Case 2
A 37-year-old male presented with redness, pain, and profound defective vision in right eye for 1 day following a bee sting injury. Right eye BCVA was counting finger close to face. Slit lamp examination revealed a stinger in deep corneal stroma at 11 o'clock with a surrounding 1 mm infiltrate and diffuse corneal stromal edema [Fig. 1b]. After stinger removal, tobramycin 0.3% and dexamethasone 0.1% combination eye drops were started for 6 times a day. The patient was lost to follow-up and presented directly 16 months later. A history revealed that he had discontinued medications after the 1st month. Right eye BCVA was finger counting at 1 meter. The cornea was edematous with evidence of bullous changes. A penetrating keratoplasty was then performed and the BCVA improved to 20/60 at 3 months after surgery [Fig. 1c].
Case 3
A 41-year-old female presented with pain, redness, and defective vision in the left eye after being stung by a bee. Left eye BCVA was 20/600. Slit lamp examination revealed a stinger in deep corneal stroma at 4 o'clock with surrounding infiltration [Fig. 2a] and diffuse stromal edema. After stinger removal, combination moxifloxacin 0.5% and dexamethasone 0.1% eye drops were started for 6 times a day. At 1-week follow-up, BCVA improved to finger counting at 5 meters. The corneal infiltration and edema had reduced. Topical antibiotic-steroid eye drops were tapered over a period of 3 weeks. At the 4th week follow-up, the patient presented with a healed corneal opacity with a complicated cataract [Fig. 2b]. The intraocular pressure (IOP) was elevated to 30 mmHg. Timolol maleate 0.5% eye drops were initiated twice daily and IOP was stabilized following which, phacoemulsification with posterior chamber intraocular lens (IOL) implantation was performed [Fig. 2c]. BCVA improved to 20/40 1 month after surgery. Anti-glaucoma medications had to be continued postcataract surgery.
Figure 2.
Pre- and post-operative clinical pictures of eyes which required surgery following a bee-sting injury (Case 3–6). Row 1 - At presentation. Row 2 - At intermediate follow-up. Row 3 - postsurgery
Case 4
A 52-year-old female presented with pain and defective vision in the left eye for 2 days following an episode of attack by a swarm of bees. The left eye BCVA was 20/600. Slit-lamp examination revealed 2 stingers in the cornea at 10 o'clock position with associated stromal infiltration and edema [Fig. 2d]. The stinger was removed and topical tobramycin 0.3% and dexamethasone 0.1% combination eye drops were started for 6 times a day. Four days later, the patient presented with increased intensity of pain and infiltrate size. As the stinger meanwhile had grown fungus (Alternaria species) on blood agar, the topical steroid-antibiotics were stopped, and the patient was treated with natamycin 5% eye drops hourly. The infiltrate healed over the next 4 weeks. Antifungal treatment was then stopped. At 3-month follow-up, the cornea showed signs of decompensation and scarring; and the lens was cataractous [Fig. 2e]. A combined penetrating keratoplasty with cataract surgery and intraocular lens implantation was performed [Fig. 2f]. One month after surgery, her BCVA improved to 20/200.
Case 5
A 50-year-old male presented with profound diminution of vision with associated pain and redness in right eye for 2 days following a bee sting injury. He had been using topical moxifloxacin 0.5% eye drops following the injury but did not experience any symptomatic relief. Right eye BCVA was hand movement. Slit-lamp examination revealed a large 5 × 3 mm epithelial defect with associated corneal infiltration in the right eye [Fig. 2g]. A stinger was seen in the deeper corneal stroma at the inferior mid-periphery. After stinger removal, moxifloxacin 0.5% and dexamethasone 0.1% combination eye drops were started 6 times a day. He reported the next day with increased symptoms. On examination, the epithelial defect was same, but stromal edema had increased. The presence of an immune ring with intense anterior chamber reaction was noted. The patient was admitted to the hospital, and the same medications were continued under supervision. After 2 weeks, the infiltrate had resolved, and the epithelial defect had healed. However, the corneal edema increased and a complicated cataract developed along with increase in IOP [Fig. 2h]. After stabilizing the IOP with timolol maleate 0.5% eye drops twice daily, the patient underwent a combined penetrating keratoplasty and cataract extraction with IOL implantation [Fig. 2i]. At 2-month follow-up, the graft was clear however, the IOP had increased to 32 mm Hg. On fundus examination, the media appeared hazy, but the optic disc and vessels were normal. The IOP showed fluctuations with bouts of increasing spikes while remaining normal at times. After 9 months, when IOP was not stabilised with maximum anti-glaucoma medications, trabeculectomy was performed, after which the IOP remained controlled. His BCVA was 20/120 6 months after trabeculectomy.
Case 6
A 21-year-old male presented with severe pain, redness, and defective vision in the right eye for 1 day following a bee sting injury. Right eye BCVA was 20/240. Slit-lamp examination revealed a 6 mm large corneal epithelial defect. A bee stinger was seen projecting into the anterior chamber with surrounding infiltrate [Fig. 2j]. Diffuse pigment dispersion was present over endothelium. After removal of stinger, a bandage contact lens was applied and topical moxifloxacin 0.5% eye drops were started 2 hourly. On day 3, the epithelial defect had healed and hence the bandage contact lens was removed and the patient was started on a moxifloxacin 0.5% and dexamethasone 0.1% combination eye drops 6 times a day with a plan to taper over 6 weeks. A rise of IOP was noted at 2 weeks which was controlled with topical timolol maleate 0.5% eye drops twice daily. At 6 weeks, cornea showed diffuse decompensation and scarring at the site of infiltration along with anterior capsular cataract formation [Fig. 2k]. BCVA was reduced to finger counting at 5 meters. He then underwent combined penetrating keratoplasty with cataract extraction and IOL implantation [Fig. 2l]. His BCVA improved to 20/40 and was advised to continue the anti-glaucoma medications.
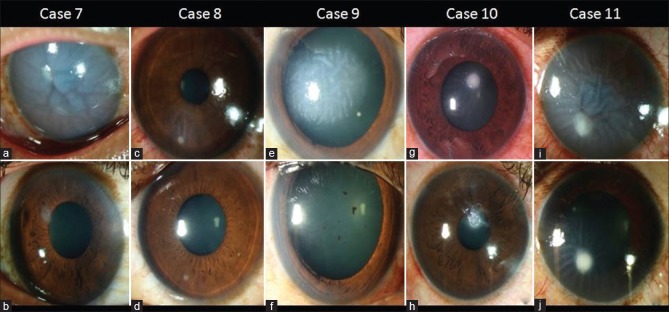
Case 7
A 41-year-old male presented with severe pain and defective vision in his right eye for 1 day, following a bee sting injury to his eye. Right eye BCVA was 20/400. Slit-lamp examination revealed a stinger embedded in the cornea with surrounding stromal infiltrate at 11 o'clock position at mid-periphery associated with marked corneal edema [Fig. 3a]. After removal of the stinger, topical prednisolone acetate 1% eye drops and moxifloxacin 0.5% eye drops were started 6 times a day each with oral Prednisolone in a dose of 60 mg a day. In 1 week, the BCVA had recovered to 20/40 with marked decrease in pain and corneal edema. He was then maintained on tapering doses of oral steroids (dose reduced by 10 mg/week) and topical steroids while his topical antibiotics were continued. On the 4th week follow-up, BCVA had improved to 20/20 and he was asymptomatic. As per the original strategy, the topical antibiotics were stopped and the topical and oral steroids were tapered over the next 2 weeks. The patient continued to have good vision and did not have any recurrence in his symptoms. On his final follow-up at 5 months, the cornea revealed a small residual scar [Fig. 3b] and the BCVA was maintained at 20/20.
Figure 3.
Clinical pictures of the eyes (Case 7–11) which were treated with concomitant oral steroids. Row 1 - At presentation. Row 2 - At the last follow-up
Case 8
A 22-year-old male presented with severe pain and redness in left eye for 1 day following a bee sting injury. The retained stringer was reportedly removed by an ophthalmologist elsewhere 2 h after the injury and topical gatifloxacin 0.3% eye drops were started 6 times a day. He was referred to us for further management. Left eye BCVA was 20/20p and was unaffected as the site of trauma was in the inferonasal quadrant sparing the visual axis. The left eye showed an edematous upper eyelid with congested conjunctiva. Slit lamp examination revealed a corneal stromal infiltrate at 7 o'clock position presumably at the site of the stinger removal with surrounding stromal edema [Fig. 3c]. He was started topical gatifloxacin 0.3% and dexamethasone 0.1% eye drops, 6 times a day, homatropine 2% eye drops 2 times a day with oral prednisolone 40 mg/day. At the 1st week follow-up, the BCVA was maintained to 20/20p with marked decrease in the pain and corneal edema. He was then maintained on tapering doses of oral steroids (reducing 10 mg/week) and topical steroids. In 4 weeks, the lesion had healed with residual scarring at the site of the infiltrate [Fig. 3d] and the BCVA had improved to 20/20. At this time, oral prednisolone was stopped and topical steroids were tapered over a period of 2 weeks. On his final follow-up at 4 months, the BCVA was maintained at 20/20.
Case 9
A 44-year-old male presented with defective vision in right eye for 15 days after he sustained bee sting injury. He gave a history of being treated elsewhere with topical steroids and antibiotics. Right eye BCVA was counting fingers at 2 meters. Slit lamp examination revealed diffuse corneal edema [Fig. 3e]. Multiple large keratic precipitates were seen on the endothelium throughout the cornea. He was started on topical prednisolone acetate 1% eye drops 6 times a day, chloramphenicol 1% eye ointment twice daily, atropine 1% eye ointment twice daily, and oral prednisolone in a dose of 40 mg/day. At the 1st week follow-up, the BCVA had recovered to 20/120 with marked decrease in pain and corneal edema. He was then maintained on tapering doses of oral steroids (reducing 10 mg/week). The patient showed significant clinical improvement in 4 weeks and the BCVA improved to 20/40 with a residual corneal scarring [Fig. 3f]. Oral prednisolone was stopped and topical steroids were tapered over 10 days while the topical antibiotics were continued for 10 days and then stopped. On his final follow-up at 5 months, the BCVA was maintained to 20/40.
Case 10
A 37-year-old male presented with defective vision, pain, and redness in right eye for 1 day following a bee sting injury. Right eye BCVA was 20/80. Slit-lamp examination revealed a focal 1 mm diameter corneal infiltrate in the superonasal quadrant with a retained stinger at the center [Fig. 3g] with surrounding corneal edema. After the stinger removal, topical moxifloxacin 0.5% eye drops 4 times a day and dexamethasone 0.5% eye drops were started 6 times a day in a weekly tapering dose, along with oral prednisolone at a dose of 40 mg/day. At the 1st week follow-up, the BCVA had recovered to 20/40 with marked decrease in the pain and corneal edema. He was then maintained on tapering doses of oral steroids (reducing 10 mg/week) and topical steroids while his topical antibiotics were continued. At the 6th week follow-up, the corneal lesion had healed completely with a residual scar at the site of the infiltrate [Fig. 3h] and BCVA had improved to 20/40 and all his medications were stopped. On his last follow-up at 6 months, patient maintained the BCVA of 20/40.
Case 11
A 29-year-old male presented with severe pain, redness, and defective vision in his left eye for 2 h following a bee sting injury while driving a motorcycle. Left eye BCVA was 20/400. Slit lamp examination of the cornea of his left eye revealed an intact bee stinger at 7 o'clock position at mid-periphery with 1 mm focal infiltrate associated with surrounding corneal edema [Fig. 3i]. After the stinger removal, the patient was started on topical moxifloxacin 0.5% eye drops 6 times a day and dexamethasone 0.5% eye drops 6 times a day along with oral prednisolone at a dose of 50 mg a day. At the 1st week follow-up, the BCVA had recovered to 20/80 with marked decrease in the pain and corneal edema. He was then maintained on tapering doses of oral steroids (reducing 10 mg/week) and topical steroids while his topical antibiotics were continued. By 6 weeks, the infiltrate had healed with residual scarring [Fig. 3j] and BCVA had improved to 20/40. All his medications were stopped.
Six eyes (54.5%) had a good clinical outcome (best-corrected visual acuity [BCVA] >20/40) with medical therapy alone with no need for surgical intervention. Five eyes (45.5%) had a poor clinical outcome (BCVA <20/40) with medical therapy and required surgery; of which three required a combined penetrating keratoplasty with cataract surgery, while one required isolated cataract surgery and one underwent penetrating keratoplasty. Glaucoma was present in 3/5 eyes undergoing surgery, one of which required a trabeculectomy. Five of the six eyes who had a good clinical outcome with medical therapy alone had been treated with concomitant oral steroids, along with topical antibiotic-steroid combination therapy.
Discussion
Isolated bee sting injury to the eye is presumably a rare occurrence. The ocular morbidity associated with this trauma would depend on the interplay between the nature and virulence of the venomous toxins elaborated by the constituents of the bee and the subsequent inflammatory response of the patient.[3] The symptoms can vary from a trivial irritation to a profound diminution of vision.
The components of the bee venom affect the various eye tissues with varying levels of severity. The biologic amines such as histamine and dopamine cause vasodilation leading to congestion and chemosis.[4] The nonenzymatic polypeptide toxins melittin (most potent and more than 50%),[5] apamin (neurotoxin), mast-cell degranulating peptide cause membrane disruption, direct hemolysis, and denaturation of the protein which in turn is responsible for endothelial cell damage, cataract, zonulolysis, and lens subluxation.[6] The high molecular weight enzymes such as phospholipase A and B and hyaluronidase degenerate the chromatophores of anterior iris layers which manifests as heterochromia.[7] The other visually debilitating complications reported in literature are uveitis, optic neuritis,[8,9] external and internal ophthalmoplegia, optic atrophy, and papillitis.[1]
The ocular surface faces the initial injury due to its contact with the atmosphere. The initial injury to the cornea, especially if associated with the presence of an intact stinger, elicits a nonspecific inflammatory response. The high molecular weight enzymes induce a type 1 hypersensitivity response.[5] The immune reaction in the cornea leads to the release of various chemotactic factors and anaphylotoxins which leads to accumulation of inflammatory cells and ultimately cell death. This manifests clinically as corneal edema and the sterile infiltrate around the stringer.[10] The endothelial cell density is known to decrease at a late stage.[11]
Reports about the management of ocular bee sting injury have been few and far in between. Varied treatment strategies have been reported but mostly in the form of isolated case reports. Al Towerki reported that immediate removal of the stinger mitigated the need of any additional therapy with good outcome.[12] In a small case series of 4 cases Lin et al. have reported that early stinger removal along with topical antibiotics and steroids ensure the good visual outcome.[2] On the other hand, there have been reports about the serious complications incited by the bee sting injuries. The serious complications reported include corneal decompensation[13] and intractable glaucoma,[14] necessitating complicated surgical procedures.
In our series, the eleven patients presented to five different cornea trained attending physicians over a period of 2 years. Since there was no established treatment protocol, the patients were treated as per the preference of the individual treating physician. An analysis of the final results reveals important observations. Six patients (54.5%) had a good clinical outcome (BCVA >20/40) with medical therapy alone without a need for any additional surgical intervention, apart from the removal of the stinger. Of these six patients, five had received concomitant oral steroids along with topical antibiotic-steroid therapy. Of the five (45.45%) patients which had a poor clinical outcome (BCVA <20/40) with medical therapy, three required a combined penetrating keratoplasty with cataract surgery; while two required isolated cataract surgery and penetrating keratoplasty, respectively. Penetrating keratoplasty was preferred over endothelial due to stromal scarring, poor visibility and shallow anterior chamber (AC) in patients with associated complicated cataract. Glaucoma was present in 3/5 eyes undergoing surgery, one of which required a trabeculectomy. None of the patients treated with supplemental steroids required any surgery.
Of 11 eyes, 1 eye had fungal infection, and hence microbiological examination of the removed stinger is recommended. Furthermore, frequent initial follow-up is necessary to diagnose any worsening of the infiltrate with the use of steroids which then will prompt a change in treatment.
This case series presents interesting observations regarding the benefits of the supplementation of systemic corticosteroids in treating the condition. The result of this series has prompted us to establish a treatment protocol at our institution, which advocates use of systemic corticosteroids along with topical antibiotic-steroid combination, especially in cases where corneal involvement and anterior reaction is severe at presentation or inflammation not ameliorating with topical steroids alone. The absence of randomization is an obvious weakness in this study. However, the rarity of this condition might not allow the feasibility of conducting a randomized clinical trial.
Conclusion
Oral corticosteroid supplementation to the topical steroid antibiotic treatment in patients with corneal bee sting injury where corneal involvement and anterior reaction is severe at presentation or inflammation not ameliorating with topical steroids alone prevents serious vision-threatening complications such as corneal decompensation, cataract, and glaucoma.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Chinwattanakul S, Prabhasawat P, Kongsap P. Corneal injury by bee sting with retained stinger – A case report. J Med Assoc Thai. 2006;89:1766–9. [PubMed] [Google Scholar]
- 2.Lin PH, Wang NK, Hwang YS, Ma DH, Yeh LK. Bee sting of the cornea and conjunctiva: Management and outcomes. Cornea. 2011;30:392–4. doi: 10.1097/ICO.0b013e3181f234a6. [DOI] [PubMed] [Google Scholar]
- 3.Razmjoo H, Abtahi MA, Roomizadeh P, Mohammadi Z, Abtahi SH. Management of corneal bee sting. Clin Ophthalmol. 2011;5:1697–700. doi: 10.2147/OPTH.S26919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen CJ, Richardson CD. Bee sting-induced ocular changes. Ann Ophthalmol. 1986;18:285–6. [PubMed] [Google Scholar]
- 5.Smolin G, Wong I. Bee sting of the cornea: Case report. Ann Ophthalmol. 1982;14:342–3. [PubMed] [Google Scholar]
- 6.Ghosh SK, Chattopadhyay D, Sen AC, Chakrabarti B. Melittin-induced conformational changes in human lens protein. Curr Eye Res. 1991;10:1065–8. doi: 10.3109/02713689109020345. [DOI] [PubMed] [Google Scholar]
- 7.Singh G. Bee sting of the cornea. Ann Ophthalmol. 1984;16:320–2. [PubMed] [Google Scholar]
- 8.Song HS, Wray SH. Bee sting optic neuritis. A case report with visual evoked potentials. J Clin Neuroophthalmol. 1991;11:45–9. [PubMed] [Google Scholar]
- 9.Choi MY, Cho SH. Optic neuritis after bee sting. Korean J Ophthalmol. 2000;14:49–52. doi: 10.3341/kjo.2000.14.1.49. [DOI] [PubMed] [Google Scholar]
- 10.Yildrim N, Erol N, Basmak H. Bee sting of the cornea: a case report. Cornea. 1998;17:333–4. doi: 10.1097/00003226-199805000-00015. [DOI] [PubMed] [Google Scholar]
- 11.Gürlü VP, Erda N. Corneal bee sting-induced endothelial changes. Cornea. 2006;25:981–3. doi: 10.1097/01.ico.0000226364.57172.72. [DOI] [PubMed] [Google Scholar]
- 12.Al-Towerki AE. Corneal honeybee sting. Cornea. 2003;22:672–4. doi: 10.1097/00003226-200310000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Sedaghat MR, Mazouchi M, Poor SS. Corneal bee-sting causing visual complications: A case report. Iran J Ophthalmol. 2012;24:66–70. [Google Scholar]
- 14.Teoh SC, Lee JJ, Fam HB. Corneal honeybee sting. Can J Ophthalmol. 2005;40:469–71. doi: 10.1016/S0008-4182(05)80008-0. [DOI] [PubMed] [Google Scholar]