Abstract
Purpose:
This study aims to report a case series of upper eyelid cicatricial margin entropion with retraction, corrected through a grey-line approach only. We remind readers of the grey-line approach to levator recession (LR) and lamellar repositioning surgery.
Methods:
A retrospective review of clinic notes and photographs of patients who underwent grey-line split (GLS), LR, release of orbital septum, recession of levator, advancement of posterior lamella and anterior lamellar repositioning without a skin crease incision, from December 2015 to December 2016. Indications for surgery included mild-to-moderate cicatricial margin upper eyelid entropion, tarsal curling, and meibomian gland inversion. Patients requiring spacer interposition to lengthen the posterior lamella were excluded from the study. Parameters of the study included lid margin position, lid height, ocular surface health and symptom improvement.
Results:
Eleven eyelids of eight patients were included in the study, and underwent the procedure described. Lid margin position measured as the marginal reflex distance lowered (improved) in 72.7% of patients. Lid margin eversion was achieved in all eyes (100%). Corneal punctate epithelial erosions markedly improved, being present in 72.7% of patients preoperatively, and only 9.1% of patients postoperatively. Eight of eleven eyes showed symptomatic improvement, with six (54.5%) being completely asymptomatic and two achieving partial relief. An added observation was a pretarsal show asymmetry in some patients which improved in 36.4% of surgeries postoperatively.
Conclusion:
Upper eyelid LR with GLS and anterior lamella repositioning can all be performed through the plane of the split, avoiding a skin incision. Normal lid margin apposition was achieved in all eyes with 91% demonstrating a clear cornea and 72% having symptomatic improvement.
Keywords: Cicatricial changes, grey-line split, levator recession, single incision, upper lid
Anterior lamellar repositioning (ALR) is a well-known, simple, and widely popular method for treating both upper and lower eyelid cicatricial margin entropion.[1,2,3,4,5,6] Welsh[1] described ALR with grey-line split (GLS) and suture repositioning for correcting cicatricial entropion in 1969. Some other published techniques have added a lid crease incision with GLS to recess the levator.[2,3,7] Studies that describe GLS with the recession of the anterior lamellar and no lid crease incision do not describe concurrent levator recession (LR).[5,6,8] We report results of a procedure of ALR and LR through a single GLS for upper eyelid cicatricial changes [Fig. 1a and b].
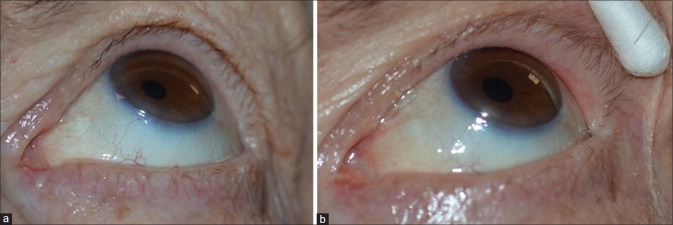
Figure 1.
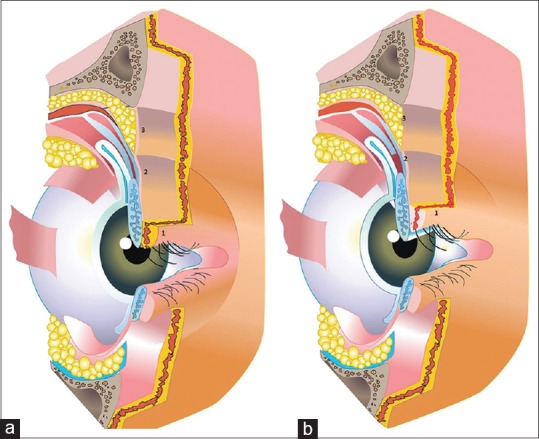
(a) Cross section of upper lid showing the three points of incision: (1) The grey line, (2) the levator attachment at the tarsus, (3) the orbital septum (b) cross section of upper lid showing: (1) The recessed anterior lamella, (2) the recessed levator, (3) the opened septum
Methods
The study method was a retrospective review of case notes and photographs of all consecutive patients undergoing the described procedure, over the 1 year period, from December 2015 to December 2016. All surgeries were performed at a single center. The study was approved by the Institutional Ethics Committee. All patients in this study had cicatricial changes in upper lid and underwent a GLS, upper eyelid LR, and ALR without a skin crease incision. Patients with severe retraction requiring mucous membrane grafting at the same time as lamella repositioning or patients with incomplete medical records were excluded. All procedures were performed or supervised by a single surgeon. Outcomes were assessed based on the review of medical case notes and comparison of standardized pre- and post-operative clinical photographs assessed by an independent reviewer. Primary outcome measures were as follows: (1) improvement in eyelid margin position and retraction, (2) improvement in symptoms, and (3) improvement in ocular surface health.
Surgical technique
All procedures were performed under local anesthesia (with bupivacaine 0.25% and 1:200,000 adrenaline) and intravenous sedation.
A grey-line incision was first made along the length of the upper eyelid using a No. 15 Bard-Parker blade from the lateral commissure to a point just lateral to the lacrimal punctum [Fig. 2]. Dissection was performed between the tarsus and pretarsal orbicularis oculi, using Westcott scissors, to reach the superior margin of tarsus [Fig. 3a]. Placing the tarsus on traction by the aid of an assistant, the anterior lamella was stretched away from the tarsus to help expose the orbital septum and levator aponeurosis [Fig. 3b]. The orbital septum was incised and the levator aponeurosis exposed. Placing the levator aponeurosis on traction by the aid of an assistant, the septum was further dissected medially and laterally to fully expose levator palpebrae superioris (LPS). LPS and its aponeurosis were subsequently dissected off Muller's muscle and recessed for approximately three to four mm [Fig. 4a-c]. Tarsal curling was managed by polishing of the anterior surface of tarsus with a No. 15 Bard-Parker blade [Fig. 5]. The composite flap of skin and pretarsal orbicularis was recessed, sutured to anterior tarsal surface using three to four interrupted six-zero absorbable mattress sutures, leaving up to two mm of tarsus visible below the anterior lamella margin. Where anterior lamella was horizontally contracted causing cicatricial lash ptosis, posterior radial incisions were made at the lid margin to restore normal lash direction [Fig. 6].
Figure 2.

Steps of surgery - grey-line split
Figure 3.
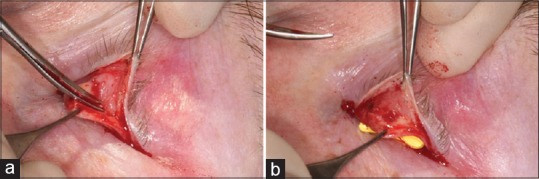
(a) Dissection of anterior lamella off the posterior lamella (b) dissection of skin muscle lamina till the superior border of tarsus
Figure 4.
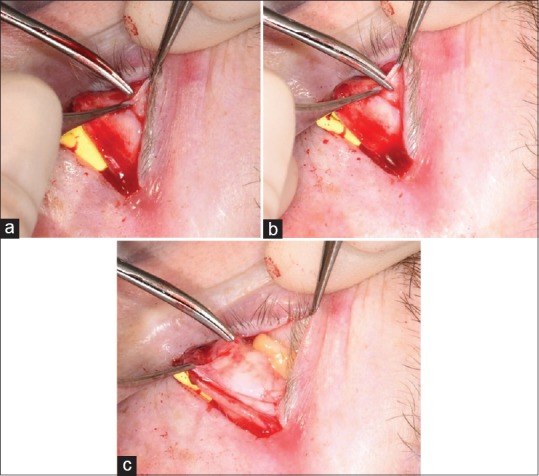
(a) Orbital septum grasped (b) opening the septum (c) the recessed levator and opened septum
Figure 5.
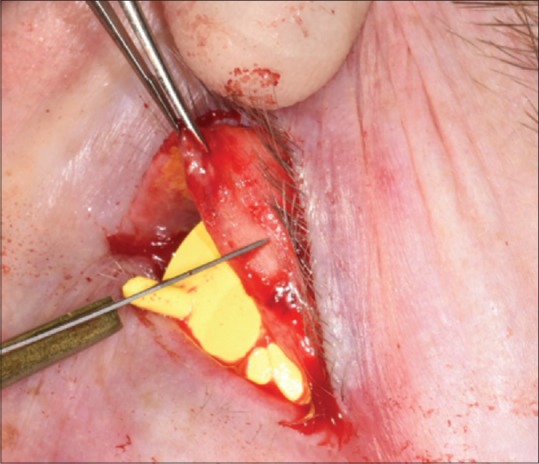
Tarsal scraping to flatten the curling tarsal plate
Figure 6.
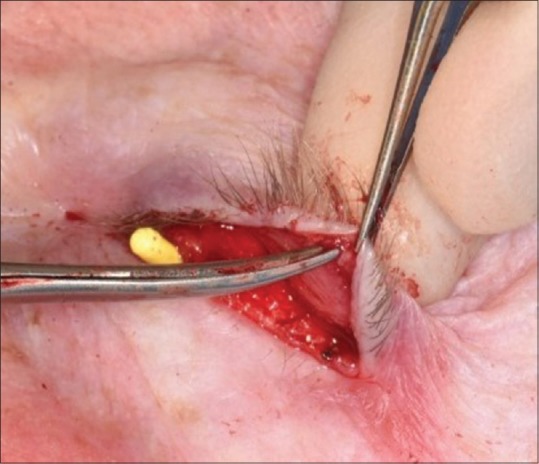
Radial cuts in lid margin to lengthen the contracted margin and reverse lash ptosis
Postoperatively, all patients were prescribed chloramphenicol ointment four times per day for 7 days and a review arranged at 2 weeks, and subsequently at 2 months.
Results
Eleven eyelids of eight patients (5 females) underwent the procedure over the time period of the study. The mean age at surgery was 65.6 years (range 46–81). Of the eight patients, three patients underwent bilateral surgery, three had surgery to the left eye, and two to the right eye. The presenting complaints were most commonly a combination of symptoms of itching, soreness, and watering in four patients (50%), foreign body sensation in two patients (25%), asymmetry between the lids in one patient (12.5%), and scratchiness in one patient (12.5%). The patient with asymmetry as presenting complaint was found to have meibomian gland inversion (MGI), and chronic meibomian gland disease and hence was advised lid eversion surgery. Significant past ocular history included facial nerve palsy in two patients (25%). The ocular surface changes included inferior punctate epithelial erosions (PEE) in four eyes (36.3%), superotemporal PEEs in three eyes (27.27%), and diffuse PEEs in one eye (9%). Only three eyes had clear corneas at presentation (27.27%), the remainder demonstrating superficial corneal punctate staining. Indications for surgery included MGI plus meibomian gland dysfunction (MGD) in five eyes (45.5%); MGI with MGD, entropion, and tarsal curling in two eyes (18.18%); entropion plus lash ptosis in two eyes (18.18%); MGI in one eye (9%); and entropion in one eye (9%). All 11 eyes underwent a GLS with ALR and LR. Follow-up at two weeks was uneventful in seven eyes; three eyes had swelling and one patient complained of irritation. At two-month postoperative review, one eye had trichiatic lashes, which were epilated and one eye had residual lash ptosis. The change of lid height and position is demonstrated in Table 1.
Table 1.
Pre- and post-operative lid height and position, corneal health and residual disease
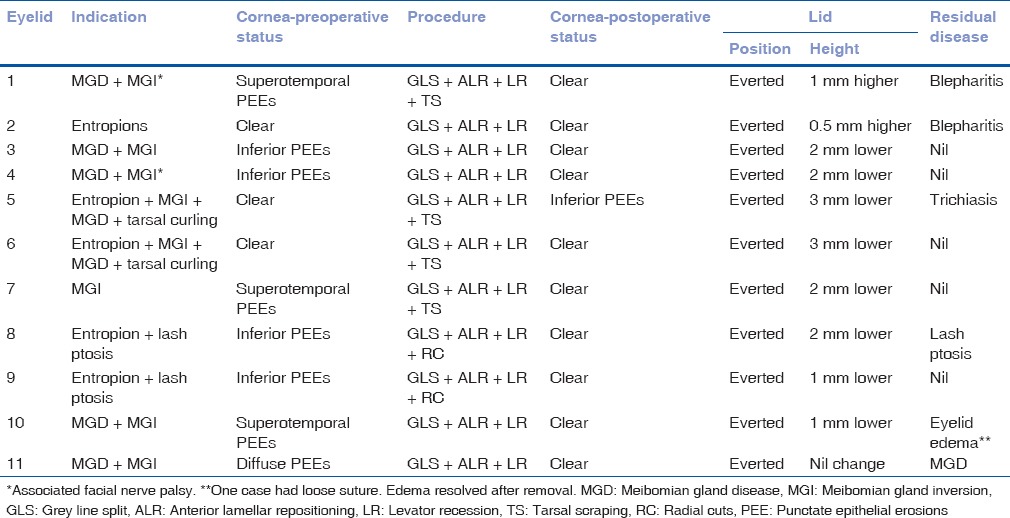
The marginal reflex distance value lowering was considered as a parameter of reversal of lid retraction associated with cicatricial lid changes. The lowering achieved was by 2 mm in four eyes (36.36%), by 1 mm in two eyes (18.18%), and 3 mm in two eyes (18.18%). It increased by 1 mm in one eye and 0.5 mm in one eye which could be attributed to suboptimal recession of levator. There was no change in one eye. The mean lowering of upper eyelid was 2 mm. The additional parameter observed was PTS asymmetry, which was zero in four patients who had unilateral or bilateral surgery (36.36%) (2 having improved and 2 unchanged), and increased by 2 mm in one eye (9.09%) and by 1 mm in one eye (9.09%). Both these patients with an increased asymmetry were suffering from facial palsy, therefore, lids had to be lowered more than the fellow eye. Six eyes (54.54%) were totally asymptomatic after 2-month follow-up. Two eyes (18.18%) showed partial symptomatic relief and were diagnosed with MGD and managed conservatively. One eye had persistent eyelid edema and had a loose vicryl suture leading to ocular surface irritation which was relieved by suture removal. One eye had residual lash ptosis at 2-month follow-up and persistent MGD which was treated conservatively. One eye had residual trichiatic lashes which were manually epilated. Lid margin eversion was achieved in all eyes [Fig. 7]. The cornea was clear in all eyes but one at the final follow-up.
Figure 7.
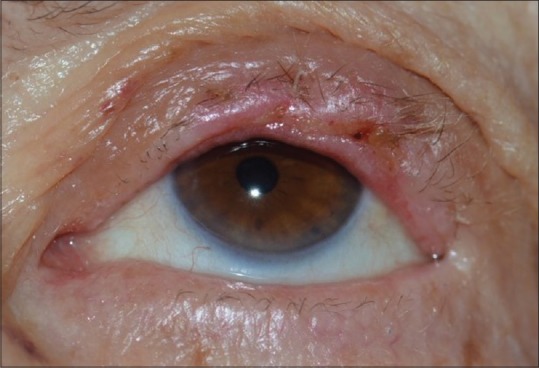
The final correction of lid margin after the grey line split, levator recession, and anterior lamellar re positioning
Discussion
Cicatricial upper eyelid entropion occurs due to shortening of the posterior lamellar and resultant in-turning of the lid margin which may be secondary to various etiologies. These range from trachoma to advanced MGD. Other causes include vernal keratoconjunctivitis, herpes zoster ophthalmicus, burns, Stevens-Johnson's syndrome, and ocular cicatricial pemphigoid (OCP). Published techniques for correction are multiple, and their success may depend on the underlying cause, and so the selection of an appropriate technique for the pathology should be a consideration. The original description of ALR with GLS by Welsh, for the correction of trachomatous cicatricial entropion, did not involve a lid crease incision. However, he made a vertical cut along the anterior lamella at lateral canthal area to lift the anterior lamella and sutured the two lamellae using nonabsorbable sutures, 4–6 mm away from the lash line.[1] This procedure was further modified by various surgeons. Sodhi et al. additionally made 2–3 mm vertical incisions through the medial (1 mm lateral to the lacrimal punctum) and lateral anterior margin of the tarsal plate to aid lid splitting into anterior and posterior lamellae[6] and also added full thickness posterior lamella sutures at the level of the fornix back onto the skin.[8] Seiff et al. combined the original procedure with terminal tarsal rotation.[9] As previously discussed, other authors have reported lid crease incision and lifting the anterior lamella off the posterior with or without a GLS[4,5,6] the obvious advantage being avoidance of surgery to the conjunctiva and hence improve safety in conditions such as OCP.[2]
GLS with ALR through a lid crease and LR has been used to correct a wide spectrum of lid margin abnormalities as described above. Kemp and Collin have included treatment of meibomian gland migration but as stated, have used a skin crease incision for their procedures.[3] Ross has shown a 98% anatomical success rate of achieving normal lid margin position using ALR or terminal tarsal rotation, again involving a skin crease incision.[10]
Our case series demonstrates surgical correction of subtle changes such as MGI [Fig. 8], lash ptosis, and tarsal curling [Fig. 9] due to advanced MGD which may cause bothersome symptoms. Chronic MGD leads to structural changes in the lid margin, which may not be identified if not carefully assessed at the examination, and these may result in symptoms of scratchiness, irritation, and soreness. In our case series, only one eye had frank entropion, the remaining having one or more of following changes (1) lash ptosis, (2) MGI, (3) tarsal curling, and (4) trichiasis. To the best of our knowledge, previously published reports have not demonstrated use of this procedure to correct these changes. The percentage improvement of symptoms was 72.72% and was comparable to earlier such series.[2,10,11,12] Changes in lid height and pretarsal show have not been documented in previous reports.
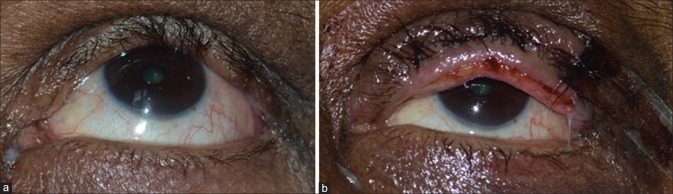
Figure 8.
(a) Meibomian gland inversion (b) cotton-tipped applicator used to evert the lid which provides immediate relief from scratching sensation that patients with this condition often complain of
Figure 9.
(a) Tarsal curling, lash ptosis with chronic meibomian gland dysfunction (b) correction of tarsal and lash ptosis curling with grey-line split + levator recession + anterior lamellar repositioning
This case series involves LR to correct the associated lid retraction, which has not been mentioned in previous studies through a GLS approach. Cicatricial entropion involves lid retraction due to posterior lamellar contraction; therefore, a simple ALR will not be able to fully address the ocular surface compromise. The combination of repositioning the offending anterior lamella and ensuring complete lid closure is proposed as a better procedure for treating cicatricial lid changes.
We acknowledge the limitations of this study in that there are only a small number of patients treated in this preliminary study. Longer follow-up is required to assess the long-term efficacy of this procedure; however, a skin crease does not appear to be essential in the correction of upper eyelid cicatricial margin entropion.
Conclusion
ALR with only a GLS avoids a skin incision, and LR can also effectively be performed through the plane thus created. A grey-line incision should be preferred to conjunctival incisions in cicatrizing conditions to avoid trauma to the conjunctiva. The levator, if recessed a few millimeters, adds to the lengthening of posterior lamella thereby reducing posterior lamella retraction and improving lagophthalmos. Although only a small pilot study, we remind authors that LR can easily be performed through a GLS and avoids both a lid crease incision with skin scar and a conjunctival incision.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Welsh NH. The treatment of cicatricial entropion. S Afr Med J. 1969;43:172–5. [PubMed] [Google Scholar]
- 2.Elder MJ, Collin R. Anterior lamellar repositioning and grey line split for upper lid entropion in ocular cicatricial pemphigoid. Eye (Lond) 1996;10:439–42. doi: 10.1038/eye.1996.96. [DOI] [PubMed] [Google Scholar]
- 3.Kemp EG, Collin JR. Surgical management of upper lid entropion. Br J Ophthalmol. 1986;70:575–9. doi: 10.1136/bjo.70.8.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rhatigan MC, Ashworth JL, Goodall K, Leatherbarrow B. Correction of blepharoconjunctivitis-related upper eyelid entropion using the anterior lamellar reposition technique. Eye (Lond) 1997;11:118–20. doi: 10.1038/eye.1997.24. [DOI] [PubMed] [Google Scholar]
- 5.Ahmed RA, Abdelbaky SH. Short term outcome of anterior lamellar reposition in treating trachomatous trichiasis. J Ophthalmol. 2015;2015:568363. doi: 10.1155/2015/568363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sodhi PK, Yadava U, Mehta DK. Efficacy of lamellar division for correcting cicatricial lid entropion and its associated features unrectified by the tarsal fracture technique. Orbit. 2002;21:9–17. doi: 10.1076/orbi.21.1.9.2600. [DOI] [PubMed] [Google Scholar]
- 7.Dhaliwal U, Monga PK, Gupta VP. Comparison of three surgical procedures of differing complexity in the correction of trachomatous upper lid entropion: A prospective study. Orbit. 2004;23:227–36. doi: 10.1080/01676830490518714. [DOI] [PubMed] [Google Scholar]
- 8.Sodhi PK, Yadava U, Pandey RM, Mehta DK. Modified grey line split with anterior lamellar repositioning for treatment of cicatricial lid entropion. Ophthalmic Surg Lasers. 2002;33:169–74. [PubMed] [Google Scholar]
- 9.Seiff SR, Carter SR, Tovilla y Canales JL, Choo PH. Tarsal margin rotation with posterior lamella superadvancement for the management of cicatricial entropion of the upper eyelid. Am J Ophthalmol. 1999;127:67–71. doi: 10.1016/s0002-9394(98)00277-3. [DOI] [PubMed] [Google Scholar]
- 10.Ross AH, Cannon PS, Selva D, Malhotra R. Management of upper eyelid cicatricial entropion. Clin Exp Ophthalmol. 2011;39:526–36. doi: 10.1111/j.1442-9071.2011.02503.x. [DOI] [PubMed] [Google Scholar]
- 11.Yeung YM, Hon CY, Ho CK. A simple surgical treatment for upper lid trichiasis. Ophthalmic Surg Lasers. 1997;28:74–6. [PubMed] [Google Scholar]
- 12.Koreen IV, Taich A, Elner VM. Anterior lamellar recession with buccal mucous membrane grafting for cicatricial entropion. Ophthal Plast Reconstr Surg. 2009;25:180–4. doi: 10.1097/IOP.0b013e3181a13f0e. [DOI] [PubMed] [Google Scholar]