Abstract
Purpose:
A pilot study was done to evaluate knowledge regarding “cortical visual impairment (CVI) in children” among ophthalmologists.
Methods:
This study was conducted during the annual conference of a zonal ophthalmological society. All ophthalmologists who attended the conference were requested to participate in this study. Those who agreed were given a validated questionnaire to assess knowledge regarding CVI. Cronbach's alpha of the questionnaire was 0.6. Participants were asked to respond to multiple choice questions by choosing the single best option. The responses obtained were then evaluated.
Results:
The total number of registered delegates in the conference was 448. A total of 103 ophthalmologists showed interest to participate in the study with a response rate of 22.9%. Only 89/103 interested delegates were included in the study as remaining were unaware of CVI. No participant gave correct answers to all questions. Although more than 80% of them knew the most common association (87%) and site of pathology (84%), only 52% were sure about clinical features and even lesser respondents (39%) knew that magnetic resonance imaging is the correct investigation of choice. The majority responded correctly that these children need eye examination (89%) and can be managed by rehabilitation through multidisciplinary approach (82%), but only 58% could recognize differential diagnoses and had a correct idea regarding the prognosis of CVI. There was no correlation between the number of patients diagnosed per month by the respondent with knowledge of the disease.
Conclusion:
In this pilot study, ophthalmologists were found to have limited knowledge regarding clinical features, investigation, differential diagnosis, and visual prognosis of CVI in children. There is a need to improve awareness regarding CVI among ophthalmologists.
Keywords: Cerebral visual impairment, children, cortical blindness, cortical visual impairment, hypoxic-ischemic encephalopathy, visual impairment
Cortical visual impairment (CVI) in children is a disorder in which there is normal or minimal ocular morbidity with impairment in the visual acuity and/or functionality of vision-guided task, including motor planning due to retrochiasmal visual tract disorder.[1] Initially, the term “cortical blindness” was used for this disorder. Now, the terms “CVI” and “cerebral visual impairment” are used to describe this.[2]
CVI is a common cause of bilateral visual impairment during childhood in many developed countries.[3,4,5] Secondary analysis of data from two community-based studies reported the prevalence of 0.06% and 0.07% among children in the United Kingdom. Both the studies mentioned that CVI was the most common ophthalmological diagnosis in children.[4,6]
However, higher prevalence (2.4%) has been reported from the United States of America (USA).[7] Website of the American Association for Pediatric Ophthalmology and Strabismus mentions CVI as one of the leading causes of bilateral visual impairment in children.[3] So far, we have scarce data from India regarding the prevalence of CVI in the population or among children with visual impairment. This becomes more important in the context of the high incidence of risk factors of CVI like perinatal hypoxia in India.[8,9]
We searched the PubMed with keywords “CVI” or “cerebral visual impairment” and “prevalence” and “India” and “children,” and only five articles could be retrieved.[10,11,12,13,14] The scarcity of Indian literature in this area could be ascribed to inadequate information among ophthalmologists. Similarly, we searched the PubMed with the keywords “knowledge” and “CVI” and “ophthalmologist.” This search retrieved 8 articles, but none of them was related to the assessment of knowledge among ophthalmologists.[10,15,16,17,18,19,20,21]
Thus, we conducted a questionnaire-based survey among ophthalmologists to assess knowledge regarding CVI. Attitude and practice aspect were not included as we wanted to know the knowledge aspect first by doing this pilot survey.
Methods
The study had due approval from the ethics committee of the institute. The principal investigator, as well as the first author of the study, has a fellowship in pediatric ophthalmology with 8 years of exclusive practice in pediatric ophthalmology as faculty in a tertiary care teaching hospital. The study population was defined by job category and included ophthalmologists who attended the annual conference of a zonal ophthalmological society. Convenient sampling method was used. All delegates, irrespective of their experience or subspecialty preference, were requested to participate in this survey with the understanding that all of them were dealing with pediatric ophthalmology cases as they came to attend a zonal ophthalmological society annual conference (and not a subspecialty conference). Members of this zonal ophthalmological society in North India are working in five states and a union territory.[22] They provide services to 83.5 million people including 10.7 million children falling between the age range of 0–6 years.[23] Verbal consent was taken due to the nature of the study as no question related to personal identity was asked, and the study did not involve any procedure. The aim of the study was described beforehand, and queries, if any, were addressed.
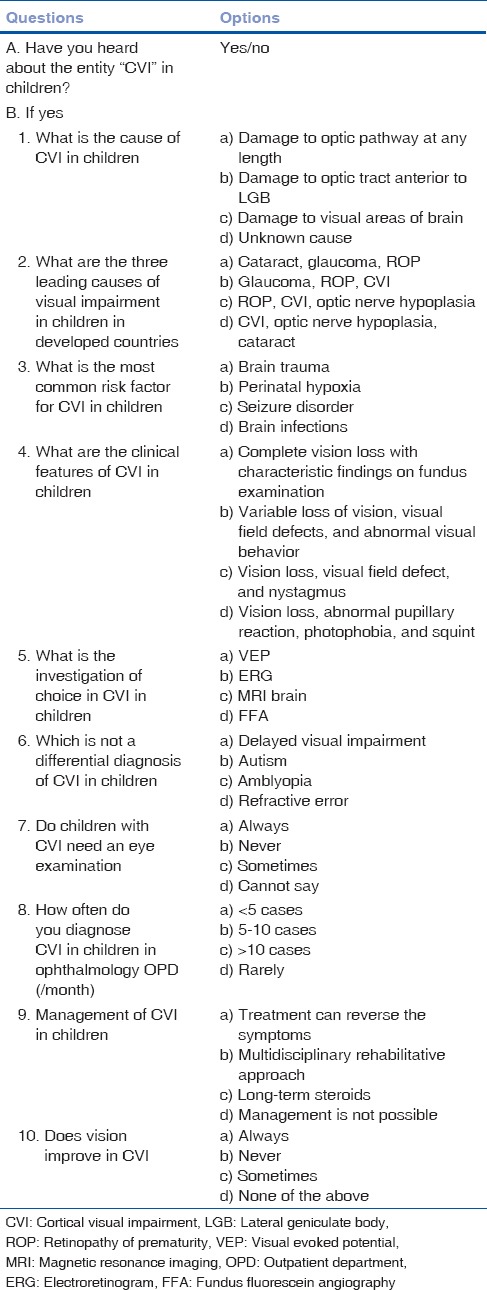
Data collection was done by administering a preformed, prevalidated paper questionnaire at the registration counter, to be filled by ophthalmologists at the reception counter, in front of one of the authors (DR), and the filled questionnaire was immediately collected [Table 1]. The questionnaire was developed by the first author (AM) who has a special interest in the topic of the study and is working in this area for the past 8 years. The study was planned as the clinical experience of the first author suggested that many cases of CVI remain undiagnosed which could have been due to the lack of information among ophthalmologists. However, PubMed search did not reveal any validated questionnaire that could be used in this study. Hence, the first author developed the questionnaire [Table 1] based on the available literature and his clinical experience to assess the extent of knowledge regarding CVI among ophthalmologists who primarily deal with mixed population, i.e. adults and children. The questionnaire had a total of 11 items where the first item examined the awareness about CVI. Further items were to be responded by only those participants who had awareness of the term CVI. Each item had four responses, and respondents were instructed to mark the best response for the given item. Nine of these items were about prevalence, etiopathogenesis, clinical presentation, differential diagnosis, investigations, management, and prognosis of CVI among children. Correct responses from each item were summed to attain a “knowledge score” for each respondent. Correct score was given 1 mark, and the incorrect score was given 0. One of the items inquired the number of CVI cases seen by each respondent in a given month to find any relation between the number of cases seen and knowledge score.
Table 1.
Questionnaire about cortical visual impairment in children
Cronbach's alpha of the questionnaire was 0.6. Ophthalmologists who were not willing to participate were excluded from the study. The outcome measure was to get an overview of knowledge regarding CVI in children among ophthalmologists.
Descriptive statistics was obtained using Microsoft Excel 2007. Data analysis was done by one of the authors (SP) who is a qualified statistician. For continuous variables, the mean and standard deviation was calculated. Testing of the hypothesis was done by Student's t-test. Proportions were calculated for categorical variables. Reliability analysis was done by Cronbach's alpha method. Student's t-test was used to analyze a number of cases diagnosed in a month with the extent of knowledge of ophthalmologist.
Results
Total registered delegates at the conference were 448. A total of 103 ophthalmologists were willing to participate in the study with a response rate of 22.9%. Fourteen of those had never heard about CVI in children, and they were excluded from the study. Responses of the remaining 89 ophthalmologists were further evaluated [Table 2].
Table 2.
Responses with correct answer to the questions asked about cortical visual impairment in children in the questionnaire
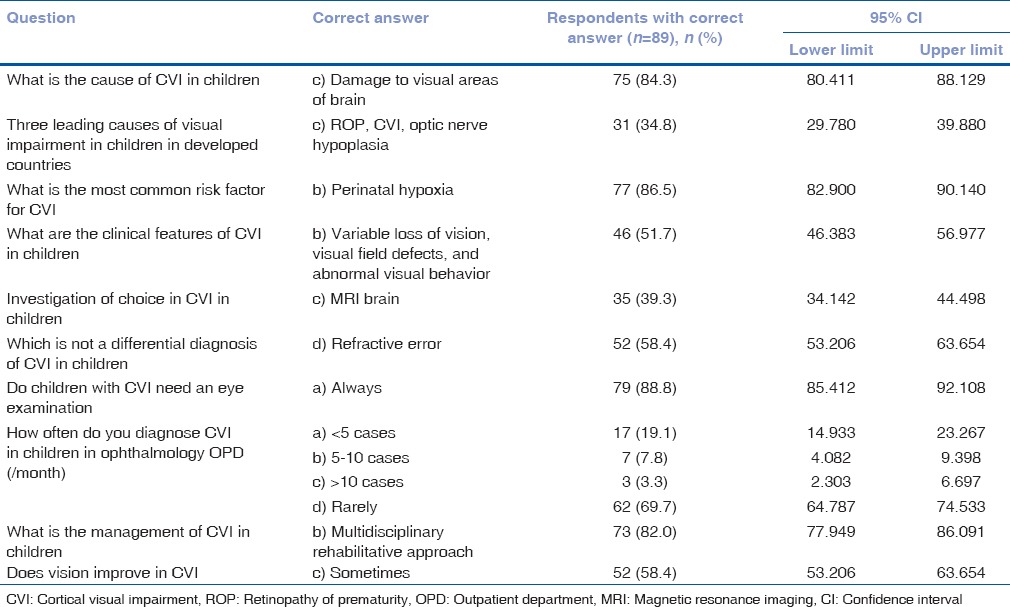
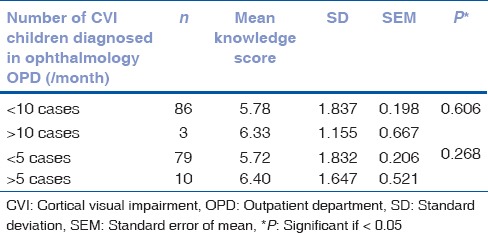
Most of the ophthalmologists had limited knowledge of CVI [Table 3]. A number of cases diagnosed in a month by an ophthalmologist with the extent of knowledge were analyzed [Table 4], and it was not found statistically significant.
Table 3.
Respondents who knew less than or equal to 25% correct answers, 50% correct answers, and all the answers about cortical visual impairment in children

Table 4.
Correlation between patient load and awareness of cortical visual impairment in children
Discussion
To the best of our knowledge, this was the first survey of its kind that showed that although practising ophthalmologists had some information regarding CVI, still, it was inadequate to diagnose and manage a child having CVI. Lack of information regarding a particular disease among health professional is not uncommon, and we have similar reports regarding other disorders.[24]
The prevalence of CVI in children is more than that of pediatric cataract in developed countries. Three leading causes of childhood blindness in the USA are CVI, optic nerve hypoplasia, and retinopathy of prematurity (ROP).[25] Perinatal hypoxia is the most common risk factor for CVI,[7,26] and the prevalence of perinatal hypoxia is more in India than the USA.[8,27] Hence, there should be many more children with CVI in India. However, Indian literature in this area is sparse indicating two possibilities – first, either the prevalence of CVI is actually low in our country or second, many cases remain undiagnosed/misdiagnosed. Addressing the first question requires a population-based study and the second question will require Knowledge, Attitude, and Practice (KAP) studies among ophthalmologists. The current study was a pilot survey and the first step, i.e., to know the knowledge aspect of this entity in a small group of ophthalmologists.
Results of the present survey showed that only half of the respondents had knowledge regarding the important clinical features of CVI in children, i.e. variable loss of vision, visual field defects, and abnormal visual behavior. Children with CVI may have variable vision loss and/or visual field defects due to pathology in optic radiations and/or occipital cortex and/or abnormal visual behavior due to involvement of dorsal stream (which connects fibers from the occipital cortex to parietal lobe and is responsible for deciding an object in a visual environment, i.e. where an object is in an individual's visual environment) or ventral stream (which connects fibers from the occipital cortex to the temporal lobe and is responsible for remembering an object in a visual environment, i.e. what the object is, in this individual's visual environment – visual memory). Children with dorsal stream involvement have problems in handling complex visual situations while children with ventral stream disorders have visual agnosia, i.e. problem in remembering faces/objects.[28,29] All these symptoms may occur in isolation or in any combination depending on the site of disease. When hypoxic insult involves other areas of the brain, children may have associated neurological symptoms, such as cerebral palsy.[7] Children having abnormal visual behavior only are the most difficult to diagnose, as they may have normal visual acuity on the Snellen chart with normal pupillary reaction and normal eye examination.[30] They may go to a normal school and remain undiagnosed but may suffer due to abnormal visual behavior as mentioned earlier.
In the current survey, correct answers by majority respondents about the most common risk factor but less awareness regarding the investigation of choice may be an indication that exact pathology is less understood by respondents. Basic pathology of CVI in children is a hypoxic injury to the brain. In premature children, perinatal hypoxia causes damage to periventricular deep white matter (optic radiations run within this) leading to CVI.[31,32] In an magnetic resonance imaging (MRI) of the brain, this is diagnosed as periventricular leukomalacia (PVL).[33] In full-term children, perinatal hypoxia causes loss of autoregulation of brain blood flow and leads to areas of infarction at junctional areas between the anterior and middle cerebral arteries and between the middle and posterior cerebral arteries.[31] This is evident in MRI of the brain. Other not very common causes of CVI in children such as meningitis, hydrocephalus, and brain trauma show specific findings of these disorders on a brain MRI. Hence, the investigation of choice for detecting CVI in children is MRI of the brain.[33]
Another important outcome of the survey was that majority of the ophthalmologists knew that children with CVI need an eye examination but not all of them responded correctly regarding the differential diagnosis. Differentiation of CVI in children from related entities is important and simple. Delayed visual maturation is one of the differential diagnoses of CVI in children till 1 year of age, but children with delayed visual maturation become normal by the age of 1 year whereas children with CVI do not.[30] Autism is also an important differential diagnosis, especially in children with CVI with normal visual acuity but abnormal visual behavior. However, MRI of the brain differentiates between autism and CVI. Amblyopia may mimic CVI in children due to decreased visual acuity in the presence of normal eye examination, but amblyopia may be unilateral whereas CVI is always bilateral. Moreover, in amblyopia, there will always be an amblyogenic factor which is not present in children with CVI.
Lifestyle modification is the key to management from an ophthalmologist's point of view. However, the management of CVI in children is a multidisciplinary rehabilitative approach. This involves a pediatric ophthalmologist, pediatrician, radiologist, otorhinologist, neurologist, and physiotherapist depending on the severity and extent of the disease.[30] Majority respondents knew that management of these children requires a multidisciplinary approach, but the correct responses about the outcome of the management, i.e., visual prognosis were less. It is important to know about the visual prognosis of CVI in children as it helps parents in preparing themselves for the future course of events. Children with CVI usually have variable improvement in vision over time, but most of them never get a normal vision.[34] Children of CVI having PVL can have a poorer prognosis, in comparison to damage to occipital cortex only. Similarly, children with CVI due to meningitis, seizures typically do not improve much.[35] Early age at the time of hypoxic insult indicates poor visual prognosis. CVI due to asphyxia in premature children has the poorest visual outcome.[34]
This study concludes that most of the ophthalmologists in the survey, who have heard about CVI in children, knew the basic etiopathogenesis of the same. They also knew that these children require an eye examination and can be managed by the multidisciplinary rehabilitative approach. However, almost half the respondents were not sure about the clinical features, investigation of choice, differential diagnosis, and visual prognosis of CVI in children. This limited knowledge may be due to the reason that with improvements in medical facilities, the survival rate of children with perinatal asphyxia is improving and disorders such as ROP and CVI are seen more now which were not prevalent previously. Hence, there is a need to increase knowledge among ophthalmologists regarding clinical features, investigation, differential diagnosis, and visual prognosis of CVI in children. This can be done by publication of review as well as original research articles in indexed, peer-reviewed journals, workshops, and presentations in conferences about CVI in children and by giving more emphasis on the topic in undergraduate as well as postgraduate curriculum.
An increment of awareness among ophthalmologists will lead to better detection and optimal management of children having CVI that includes lifestyle modification, timely rehabilitation, better quality of life, and less financial burden on the country.
A simple approach of suspecting CVI in children, which can be adopted in the day-to-day practice, could be an eye examination that cannot fully explain the child's use of vision, a history or presence of neurological problems, and the presence of the behavioral or visual responses that are collectively associated with CVI.[36] After clinical suspicion, MRI brain will confirm the diagnosis in most of the cases.
Like any other study, the present study also had some limitations. A limitation of this pilot study was the lack of attitude- and practice-related questions in the questionnaire. As there is scanty literature on CVI in children in India, this survey was done with the aim to know about the knowledge aspect. It was thought that once knowledge aspect is known, then attitude and the practice aspect can be tested in a large-scale KAP survey in the future.
Another limitation is that results cannot be generalized as the sample size was small; sampling was done by convenient method which is a nonrandomized method. However, even with all these limitations, this study indicates that there is a need to increase the knowledge about CVI in children among ophthalmologists.
Cronbach's alpha in the study was 0.6 and is considered low by many researchers. However, it is imperative to understand the actual inference and the variables that determine its value. A recent review on the value of Cronbach's alpha showed that the average relation between different items in a given scale is directly proportional to the length of items, i.e., increase in number of items will give a higher value. However, increase in the number of items comes at the cost of redundancy. Moreover, the cutoff value of 0.7 that is traditionally considered adequate is often arbitrary and depends on the intended scale. In studies assessing knowledge regarding a particular area, instruments often contain items that represent multiple dimensions. In such cases, lower values of Cronbach's alpha are acceptable.[37] In the present study, the scale was designed to assess knowledge regarding CVI, and the instrument had items from various dimensions ranging from etiology to management; hence, the value of Cronbach's alpha (0.6) appears adequate.
Conclusion
In this pilot study, ophthalmologists were found to have limited knowledge regarding clinical features, investigation, differential diagnosis, and visual prognosis of CVI in children. There is a need to improve awareness regarding CVI among ophthalmologists.
This can be a base for further large-scale and more organized studies involving more ophthalmologists to assess the KAP regarding CVI in children so that future strategies can be planned about increasing awareness regarding CVI among ophthalmologists in India.
Financial support and sponsorship
Financial support for the study was provided by “Swami Rama Himalayan University.”
Conflicts of interest
There are no conflicts of interest.
References
- 1.Lehman SS. Cortical visual impairment in children: Identification, evaluation and diagnosis. Curr Opin Ophthalmol. 2012;23:384–7. doi: 10.1097/ICU.0b013e3283566b4b. [DOI] [PubMed] [Google Scholar]
- 2.Good WV. Development of a quantitative method to measure vision in children with chronic cortical visual impairment. Trans Am Ophthalmol Soc. 2001;99:253–69. [PMC free article] [PubMed] [Google Scholar]
- 3. [Last accessed on 2017 Sep 24]. Available from: https://www.aapos.org/terms/conditions/40 .
- 4.Flanagan NM, Jackson AJ, Hill AE. Visual impairment in childhood: Insights from a community-based survey. Child Care Health Dev. 2003;29:493–9. doi: 10.1046/j.1365-2214.2003.00369.x. [DOI] [PubMed] [Google Scholar]
- 5.Rosenberg T, Flage T, Hansen E, Riise R, Rudanko SL, Viggosson G, et al. Incidence of registered visual impairment in the nordic child population. Br J Ophthalmol. 1996;80:49–53. doi: 10.1136/bjo.80.1.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rogers M. Vision impairment in liverpool: Prevalence and morbidity. Arch Dis Child. 1996;74:299–303. doi: 10.1136/adc.74.4.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huo R, Burden SK, Hoyt CS, Good WV. Chronic cortical visual impairment in children: Aetiology, prognosis, and associated neurological deficits. Br J Ophthalmol. 1999;83:670–5. doi: 10.1136/bjo.83.6.670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. [Last accessed on 2017 Sep 24]. Available from: http://www.newbornwhocc.org/nnpo.html .
- 9.de Haan M, Wyatt JS, Roth S, Vargha-Khadem F, Gadian D, Mishkin M, et al. Brain and cognitive-behavioural development after asphyxia at term birth. Dev Sci. 2006;9:350–8. doi: 10.1111/j.1467-7687.2006.00499.x. [DOI] [PubMed] [Google Scholar]
- 10.Philip SS. Setting up of a cerebral visual impairment clinic for children: Challenges and future developments. Indian J Ophthalmol. 2017;65:30–4. doi: 10.4103/0301-4738.202303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kemmanu V, Hegde K, Giliyar SK, Shetty BK, Kumaramanickavel G, McCarty CA, et al. Prevalence of childhood blindness and ocular morbidity in a rural pediatric population in Southern India: The pavagada pediatric eye disease study-1. Ophthalmic Epidemiol. 2016;23:185–92. doi: 10.3109/09286586.2015.1090003. [DOI] [PubMed] [Google Scholar]
- 12.Chhablani PP, Kekunnaya R. Neuro-ophthalmic manifestations of prematurity. Indian J Ophthalmol. 2014;62:992–5. doi: 10.4103/0301-4738.145990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Philip SS, Dutton GN. Identifying and characterising cerebral visual impairment in children: A review. Clin Exp Optom. 2014;97:196–208. doi: 10.1111/cxo.12155. [DOI] [PubMed] [Google Scholar]
- 14.Swaminathan M. Cortical visual impairment in children – A new challenge for the future? Oman J Ophthalmol. 2011;4:1–2. doi: 10.4103/0974-620X.77654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Morale SE, Hughbanks-Wheaton DK, Cheng C, Subramanian V, O'Connor AR, Birch EE, et al. Visual acuity assessment of children with special needs. Am Orthopt J. 2012;62:90–8. doi: 10.3368/aoj.62.1.90. [DOI] [PubMed] [Google Scholar]
- 16.Alimović S, Mejaski-Bosnjak V. Stimulation of functional vision in children with perinatal brain damage. Coll Antropol. 2011;35(Suppl 1):3–9. [PubMed] [Google Scholar]
- 17.García-Ormaechea I, González I, Duplá M, Andres E, Pueyo V. Validation of the preverbal visual assessment (PreViAs) questionnaire. Early Hum Dev. 2014;90:635–8. doi: 10.1016/j.earlhumdev.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 18.Jacobson LK, Dutton GN. Periventricular leukomalacia: An important cause of visual and ocular motility dysfunction in children. Surv Ophthalmol. 2000;45:1–3. doi: 10.1016/s0039-6257(00)00134-x. [DOI] [PubMed] [Google Scholar]
- 19.van der Zee YJ, Stiers P, Evenhuis HM. Should we add visual acuity ratios to referral criteria for potential cerebral visual impairment? J Optom. 2017;10:95–103. doi: 10.1016/j.optom.2016.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bunce C, Wormald R. Causes of blind certifications in England and wales: April 1999-march 2000. Eye (Lond) 2008;22:905–11. doi: 10.1038/sj.eye.6702767. [DOI] [PubMed] [Google Scholar]
- 21.Bunce C, Zekite A, Wormald R, Bowman R. Is there evidence that the yearly numbers of children newly certified with sight impairment in England and wales has increased between 1999/2000 and 2014/2015? A cross-sectional study. BMJ Open. 2017;7:e016888. doi: 10.1136/bmjopen-2017-016888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. [Last accessed on 2017 Sep 24]. Available from: http://www.nzos-online.com/about-us.php .
- 23. [Last accessed on 2017 Sep 24]. Available from: http://www.census2011.co.in/states.php .
- 24.Southwell C, Moallem M, Auckley D. Cardiologist's knowledge and attitudes about obstructive sleep apnea: A survey study. Sleep Breath. 2008;12:295–302. doi: 10.1007/s11325-008-0170-1. [DOI] [PubMed] [Google Scholar]
- 25.Kong L, Fry M, Al-Samarraie M, Gilbert C, Steinkuller PG. An update on progress and the changing epidemiology of causes of childhood blindness worldwide. J AAPOS. 2012;16:501–7. doi: 10.1016/j.jaapos.2012.09.004. [DOI] [PubMed] [Google Scholar]
- 26.Khetpal V, Donahue SP. Cortical visual impairment: Etiology, associated findings, and prognosis in a tertiary care setting. J AAPOS. 2007;11:235–9. doi: 10.1016/j.jaapos.2007.01.122. [DOI] [PubMed] [Google Scholar]
- 27.Wu YW, Backstrand KH, Zhao S, Fullerton HJ, Johnston SC. Declining diagnosis of birth asphyxia in california: 1991-2000. Pediatrics. 2004;114:1584–90. doi: 10.1542/peds.2004-0708. [DOI] [PubMed] [Google Scholar]
- 28.Dutton GN, Jacobson LK. Cerebral visual impairment in children. Semin Neonatol. 2001;6:477–85. doi: 10.1053/siny.2001.0078. [DOI] [PubMed] [Google Scholar]
- 29.Dutton GN. Cognitive vision, its disorders and differential diagnosis in adults and children: Knowing where and what things are. Eye (Lond) 2003;17:289–304. doi: 10.1038/sj.eye.6700344. [DOI] [PubMed] [Google Scholar]
- 30.Good WV, Jan JE, DeSa L, Barkovich AJ, Groenveld M, Hoyt CS, et al. Cortical visual impairment in children. Surv Ophthalmol. 1994;38:351–64. doi: 10.1016/0039-6257(94)90073-6. [DOI] [PubMed] [Google Scholar]
- 31.Hoyt CS. Visual function in the brain-damaged child. Eye (Lond) 2003;17:369–84. doi: 10.1038/sj.eye.6700364. [DOI] [PubMed] [Google Scholar]
- 32.Kozeis N. Brain visual impairment in childhood: Mini review. Hippokratia. 2010;14:249–51. [PMC free article] [PubMed] [Google Scholar]
- 33.Casteels I, Demaerel P, Spileers W, Lagae L, Missotten L, Casaer P, et al. Cortical visual impairment following perinatal hypoxia: Clinicoradiologic correlation using magnetic resonance imaging. J Pediatr Ophthalmol Strabismus. 1997;34:297–305. doi: 10.3928/0191-3913-19970901-09. [DOI] [PubMed] [Google Scholar]
- 34.Lambert SR, Hoyt CS, Jan JE, Barkovich J, Flodmark O. Visual recovery from hypoxic cortical blindness during childhood. Computed tomographic and magnetic resonance imaging predictors. Arch Ophthalmol. 1987;105:1371–7. doi: 10.1001/archopht.1987.01060100073030. [DOI] [PubMed] [Google Scholar]
- 35.Chen TC, Weinberg MH, Catalano RA, Simon JW, Wagle WA. Development of object vision in infants with permanent cortical visual impairment. Am J Ophthalmol. 1992;114:575–8. doi: 10.1016/s0002-9394(14)74485-x. [DOI] [PubMed] [Google Scholar]
- 36. [Last accessed on 2017 Sep 24]. Available from: http://www.afb.org/info/living-with-vision-loss/eye-conditions/cortical-visual-impairment-traumatic-brain-injury-and-neurological-vision-loss/statement-on-cortical-visual-impairment/1235 .
- 37.Taber KS. The use of cronbach's alpha when developing and reporting research instruments in science education. Res Sci Educ. 2017 doi: 10.1007/s11165-016-9602-2. [Google Scholar]


