Abstract
Purpose:
The study aimed to evaluate the classroom environment of children with low vision and provide recommendations to reduce visual stress, with focus on mainstream schooling.
Methods:
The medical records of 110 children (5–17 years) seen in low vision clinic during 1 year period (2015) at a tertiary care center in south India were extracted. The visual function levels of children were compared to the details of their classroom environment. The study evaluated and recommended the chalkboard visual task size and viewing distance required for children with mild, moderate, and severe visual impairment (VI).
Results:
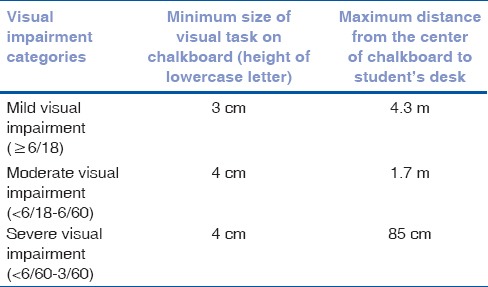
The major causes of low vision based on the site of abnormality and etiology were retinal (80%) and hereditary (67%) conditions, respectively, in children with mild (n = 18), moderate (n = 72), and severe (n = 20) VI. Many of the children (72%) had difficulty in viewing chalkboard and common strategies used for better visibility included copying from friends (47%) and going closer to chalkboard (42%). To view the chalkboard with reduced visual stress, a child with mild VI can be seated at a maximum distance of 4.3 m from the chalkboard, with the minimum size of visual task (height of lowercase letter writing on chalkboard) recommended to be 3 cm. For 3/60–6/60 range, the maximum viewing distance with the visual task size of 4 cm is recommended to be 85 cm to 1.7 m.
Conclusion:
Simple modifications of the visual task size and seating arrangements can aid children with low vision with better visibility of chalkboard and reduced visual stress to manage in mainstream schools.
Keywords: Children, low vision, school classroom, visual impairment
Globally, almost three million children are estimated to be affected by low vision.[1,2] The causes of low vision in children are categorized based on the etiology and the site of abnormality to have an uniformity in reporting its prevalence, and this eye examination recording system was developed by the World Health Organization (WHO).[3] The most common cause of pediatric low vision based on a population survey in Asia, Africa, and Latin America was retinal lesions or dystrophies and amblyopia.[1] A recent population-based study conducted in children ≤15 years in South India reported the prevalence of childhood blindness of 0.08% (95% confidence interval [CI]: 0.04%–0.11%) and the major cause was reported to be due to retinal conditions.[4] Extensive work has been done in pediatric low vision on evaluating the prevalence, etiology, functional vision, intervention, and barriers in accessing the care.
The Sarva Shiksha Abhiyan or the Education for All movement is an Indian government program initiated to universalize elementary education by providing free and compulsory education to all the children aged 6–14 years and to provide a barrier-free school environment for children with disability.[5] In India, majority of children with different forms of disabilities including visual impairment (VI) are included in regular or mainstream schools. The policies for the inclusive education system have been in place for a considerable number of years.[6] However, limited work has been done on evaluating the match between the visual demands placed in school classroom and the visual capability of children. An increased distance and near visual task demand in Grades 4–12 has been reported in classrooms of mainstream schools in Chennai city.[7]
To the best of our knowledge, limited research work has been to understand the classroom environment of children with low vision placed in mainstream schools. The current study evaluated and compared the visual function levels and respective classroom environment of children with low vision. The study also provides recommendations on the visual task size and seating distance in a classroom to reduce visual stress and discomfort in children based on the severity of VI, with focus on mainstream schooling.
Methods
The medical records of all the children referred to the low vision care department between January and December 2015 were reviewed. A retrospective study of all children between 5 and 17 years of age seen in the low vision care department of a tertiary eye care hospital in India was conducted. The clinical information extracted from the outpatient department records included the clinical diagnosis of the patient. The information extracted from the medical records of low vision care department included the evaluation of visual functions, low vision aid (LVA) trial, intervention, and detailed report about child's classroom environment. This study was approved by the Institutional Review Board and Ethics Committee.
Visual function evaluation
The evaluation of visual functions included the assessment of the visual acuity, contrast acuity, color vision, subjective and objective refraction, and visual field (confrontation method performed in cases wherever suspected and if the child is cooperative). The distance visual acuity was measured using either Lea symbols or Bailey-Lovie logMAR visual acuity chart. The near visual acuity was evaluated using a reduced Snellen chart or Minnesota near reading (MNREAD) testing acuity chart. Each eye was tested separately and then both together. The severity of VI was categorized based on the WHO consultation on “Development of Standards for Characterization of Vision Loss and Visual Functioning”[8,9] and the proportion of children in each category is shown in Table 1. The contrast acuity and color vision were evaluated using a Bailey-Lovie 25% low contrast chart and D-15 test, respectively, in children providing reliable response. The subjective and objective refraction was performed manually using retinoscopy. The anterior segment, posterior segment, and intraocular pressure examination was performed using slit-lamp biomicroscopy or torchlight, indirect ophthalmoscopy, and Goldmann Applanation tonometry or manually by finger tension, respectively. The clinical diagnosis of the children with low vision was categorized based on the WHO/PBL eye examination record for children with blindness and low vision.[3] The classification system was based on the anatomical site of the abnormality (cornea, lens, uvea, retina, optic nerve, and globe) and underlying etiology (genetic, prenatal, perinatal, and childhood).
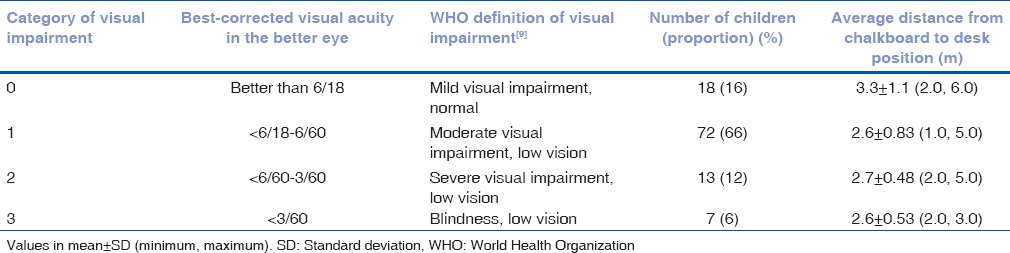
Table 1.
Proportion of children with low vision based on visual impairment categories and the viewing distance of chalkboard in their respective classrooms
Low vision aid trial for distance and near
The LVA commonly prescribed for distance included monocular telescope and see TV binocular telescope. For near, spectacles with higher plus, handheld magnifiers (dome, cutaway stand magnifier), and electronic magnifiers (CCTV and electronic assistive devices) were commonly prescribed. Other trials included the trial of tinted lenses and typoscopes.
Classroom environment
The details regarding the classroom environment were obtained from the child and confirmed by their parents or attendants. The domains included were seating position, illumination levels, academic performance, school authorities, and peer support and the management strategies adopted in classroom for better visibility. The approximate distance from the chalkboard to student's desk was obtained. The color of the chalkboard and chalk color was documented. The details of the number of windows/doors and available artificial light sources and the illuminance level on student's desk categorized as poor, normal, or excess were obtained.
Classroom simulation for chalkboard writing and seating distance
The visually demanding task in a classroom mainly includes viewing teacher's writing on chalkboard and reading small prints in books or reading materials. The visual angle subtended by the distance task is based on the size of the letter written on the chalkboard and its viewing distance. In a previous study on evaluating the visual acuity demand in Indian school classrooms, the average size of distance visual task, i.e., the vertical height of lower case letter written on the chalkboard (teacher's writing) was 3.43 cm (95% CI: 1.51–5.35 cm).[7] The visual acuity demand of children with low vision in the study sample was evaluated based on the distance visual task size fixed at 3.4 cm and their reported seating position or viewing distance in their respective classrooms. The visual angle subtended at the eye level was calculated and represented in terms of Snellen or logMAR equivalent visual acuity demand adopting the same method in previous studies.[7,10] The contrast and illuminance levels on chalkboard can have an effect on the visual acuity demand measure and necessitates a correction factor. Prof. Grundy proposed that the visual acuity necessary for any demanding visual task should be approximately twice that of the minimum value and considered as acuity reserve.[11] The calculated visual acuity demand included a correction factor of two logMAR lines to present the actual visual acuity demand. Visual stress was defined as children having visual acuity levels worse than the actual visual acuity demand in their respective classroom.
All the data were entered in Microsoft Office Excel 2010 and analysis was performed using IBM SPSS version 17 (IBM Corporation, 1 New Orchard Road, Armonk, New York 10504-1722, United States). Descriptive analysis was performed, and the proportion of children under each category is provided. The risk of visual stress based on mild, moderate, and severe VI was evaluated, and the statistical significance was set at the P < 0.05 level.
Results
A total of 424 children were referred to the low vision care department. All the medical records were scrutinized and the records of 110 children were manually entered into excel. The medical records excluded were children referred to blind school and lack of detailed classroom environment information.
Visual function
The proportion of children with VI based on the WHO VI categorization[8,9] is shown in Table 1. The binocular near visual acuity was better than N6 in 78 children (71%), between N8 and N 10 in 17 children (15%), and worse than N12 in 15 children (14%). The mean difference in contrast acuity (n = 35) between low contrast and high contrast logMAR chart was 0.15 logMAR (range: 0.00, 0.98 logMAR). The difference between contrast acuity with Bailey-Lovie 25% low contrast chart and high contrast visual acuity measure was >1.5 logMAR lines in 13 children (37%). The visual acuity improved with refractive error correction in 58% of children.
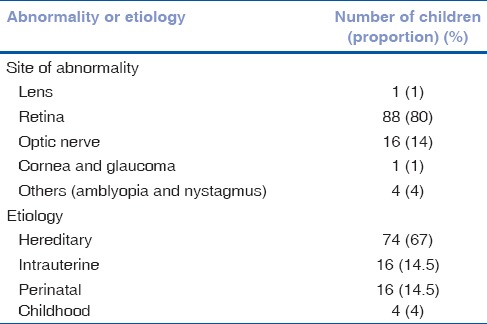
The major cause of low vision based on the site of abnormality and etiology was retinal (80%) and hereditary (67%) conditions, respectively. The proportion of children with visual anomalies based on the site of abnormality and etiology categorization is shown in Table 2.
Table 2.
Causes of low vision in children categorized based on the site of abnormality and aetiology
Low vision aid trial
Of the 110 children, LVAs were prescribed to 72 children (65%). Among them, the commonly prescribed and preferred LVAs were stand/dome magnifiers (n = 48, 72%) and tinted spectacles (n = 15, 21%). The prescription of electronic magnifiers/CCTV was provided to four children out of twenty children with severe impairment. The improvement in visual acuity with monocular telescopes was demonstrated to all the children and only one child preferred and was prescribed 4x monocular telescope. Approach magnification (sitting closer to the chalkboard), use of felt tip pens, and typoscopes were advised. Letter to school describing child's vision level and classroom modifications to be implemented for better visibility and to encourage the child were provided.
Classroom environment
Seating position in classroom
The average class size was 34 ± 7 (20, 50) students per classroom. The color of chalkboard was black in 92% classrooms. The approximate distance from the chalkboard to the child's desk position in their respective classrooms reported was 2.7 ± 0.86 m (1.0, 6.0) and 84 children (76%) needed to go closer to the chalkboard for better visibility. The average distance from the front desk (70%, n = 77) was 2.5 ± 0.75 m (1.0, 4). The front desk position from the chalkboard was >2.2 m in classrooms of 71 children (65%). The average viewing distance in respective classrooms of children with low vision based on the VI categories is shown in Table 1. For better visibility, the managing strategies adopted by children (n = 79, 72%) included copying from friends (n = 37), going closer to the chalkboard (n = 33), taking friends notebooks home (n = 5), and teacher's dictation (n = 4).
Illumination and light sources
The classroom illumination was reported to be low, optimal, and excess by 3%, 95%, and 2% of children, respectively. The classrooms of maximum of 45% children had windows ranging 1–4 per room and 17% reported to be seated beside window for better visibility.
Academic performance and school support
The academic performance was reported to good in 45% of children and the rest reported to have poor or average performance. All the school managements were ready to make the necessary changes in classroom settings and educational methods to encourage and motivate the children with low vision.
Classroom simulation and evaluation of visual stress
The visual acuity demand was calculated based on the size of the visual task and the viewing distance. Previous work on evaluating the visual demand in Indian school classrooms, the average size of visual task (vertical height of lower case letter written on the chalkboard) was 3.4 cm.[7] With the simulation of chalkboard with visual task size as 3.4 cm and the reported viewing or seating distance of the child in their respective classrooms, the visual acuity demand placed on each children in their respective classrooms was calculated. The visual acuity demand was represented in logMAR equivalent. The visual demand was compared with the actual visual acuity of children. We noted 59% of children not meeting the visual demand and were defined as having visual stress. Based on the categories of VI, 16 children (n = 18, 89%) with mild VI and 29 (n = 72, 40%) with moderate impairment were able to meet the visual demand placed in their respective classrooms. All the children with severe VI (n = 20) were under visual stress in their respective classrooms based on their actual visual acuity level. A logistic regression was performed to ascertain the effect of VI (mild, moderate, and severe) on having visual stress. Children with moderate VI were at 11 times (95% CI: 2.534, 55.530, P = 0.002) risk of visual stress in their respective classroom when compared to children with mild VI.
Recommendations to accommodate visually impaired children by environmental modifications
With an acuity reserve or correction factor of two logMAR lines, the minimum size of distance visual task (writing on chalkboard) and maximum distance from the center of the chalkboard to student's desk based on VI categories are presented in Table 3.
Table 3.
Recommendations for the minimum size and maximum viewing distance for children based on categorizes of visual impairment
Discussion
An inclusive education enables educational structures, systems, and methodologies to meet the needs of children with disability in mainstream schools.[6] The inclusion of children with low vision in mainstream schools needs a barrier-free classroom visual environment. This study reported the nature of classroom environment of low vision children and recommendations for the size of distance visual task and the seating distance in classroom.
The major cause of pediatric low vision can vary region to region, based on the socioeconomic development and availability of primary eye care.[12] We noted retinal lesions (retinal dystrophies), optic nerve diseases, and hereditary causes as the major reasons for low vision in children. This highlights the need for genetic counseling to low vision patients. In addition to the effect of distance and near visual acuity, reduction in other visual functions such as contrast sensitivity, visual field, and color vision due to ocular conditions, can increase visual discomfort and cause visual stress. Appropriate choice of LVA considering the reduction in other visual functions can improve the visual performance. We noted 29% of children having near visual acuity worse than N8, indicating the need to choose appropriate LVA considering factors such as the contrast of the material, better light levels, and appropriate magnification. The commonly preferred near LVD was dome or stand magnifiers. Children with N6 vision preferred additional LVDs for near, and this could be due to the poor contrast of reading material which could affect the near viewing task in these children. The peripheral vision has a poorer spatial resolution as compared to central vision, highlighting the need for larger critical print sizes to achieve maximum reading speed in an individual with central field loss.[13] One of the limitations of the current study was lack of quantification of visual fields in children with low vision. The distance visual acuity is improved by prescribing telescopes to children with low vision. In the current study, only one child preferred and was a prescribed telescope. The other children might have not preferred telescopes due to social stigma, i.e., being teased by friends. Lam and Leat reviewed the barriers to accessing low vision care based on the patient's perspective. They found misconception of low vision services, miscommunication by eye care professionals, lack of awareness, location and transportation, negative societal views, influence of family and friends, cost of LVDs, and reduced perception of vision loss relative to other losses in life as key barriers.[14,15] Khan et al. analyzed the perceived barriers to provision of LVDs among ophthalmologists in India and concluded lack of training/knowledge, lack of awareness, and nonavailability of LVDs as the major barriers.[16] They emphasized the importance of increasing knowledge and awareness of eye care professionals about the benefits of low vision rehabilitation. The use of telescopes or any LVDs in a classroom needs the motivation of a child and support from teachers and peers. The current study reported poor academic performance in 55% of children. However, the school authorities were supportive to make changes in classroom environment.
The clinical pediatric low vision assessment includes detailed history including the information regarding schooling and level of support and child, parent, and teacher concern and the visual function assessment (distance and near visual acuity, contrast sensitivity, color vision, and when feasible, visual fields).[17,18] These evaluations are essential for developing interventional and educational program. Legge et al. suggested the understanding and measure of the determinants of reading, i.e., reading speed in addition to the routine visual function assessment.[19] The current study provides detailed information regarding the classroom environment of children with low vision. The major concern was seating position of children with low vision, with many seated at a distance greater than the recommended standard of 2.2 m from the chalkboard. However, the limitation of the study was the recall bias and exact measure of distance for the provided information. The most commonly reported difficulties are copying from the chalkboard, reading textbooks at arm's length, and writing along a straight line. Most of the children used copying from friends (47%) or approach magnification by going closer to board (42%) as their managing strategies for better visibility. The average distance from the chalkboard was 2.7 m with a maximum of 6 m distance, highlighting an increased visual task demand in a classroom environment. The children sitting in front desk were seated at 2.5 m with a maximum of approximately 4 m, whereas the BIS recommended standard is 2.2 m from the chalkboard.[20] The mean distance visual task demand in Indian school classrooms was 20/40 and the average visual demand in front desk position was 20/70.[7] However, simple modifications in classroom parameters, i.e., the size of teacher's writing on the chalkboard and viewing distance can aid children with mild-to-moderate VI to manage visual task in classroom without any visual stress. The current study provides recommendations for the minimum size of chalkboard writing and the maximum seating distance in classroom for children with VI.
Kalloniatis and Johnston compared the distance and near visual acuity, with and without prescribed LVAs and comprehensive reading assessment between the clinical data and assessment in a visually demanding classroom environment.[21] They concluded no significant difference in acuity measure, but children performed poorly on reading rate and comprehension. They also concluded that the poor performance could be due to the poor development of reading skills, abnormal reading procedures adopted by children as a result of LVA use, or due to the lack of adequate reserve of resolving power.[21] To achieve maximum reading rate, an acuity reserve of at least 2.5 times the threshold print size of recommended.[22]
Recent figures from the National University of Educational Planning and Administration 2015–2016 showed 0.20% having visual disability over a total number of children enrolled in mainstream schools.[23] However, the cost and worth of treatment should not depend entirely on the number of children affected, but rather on the number of years over which the impairment is likely to persist. With most of the school authorities and management ready to make modifications in the classroom environment to aid children with low vision, it is important for an eye care professional to provide an appropriate recommendation. We recommend the distance of seating position in a classroom for children with a low vision based on their level of VI [Table 3]. It is important to consider an acuity reserve of twice the logMAR lines while evaluating the visual task demand based on chalkboard writing. Magnifying the view of near material can be done by increasing the font size by taking print of the material with increased size or use of magnifiers such as stand or dome magnifiers. Contrast sensitivity can be affected even with a better visual acuity measure. Constant painting of blackboard is recommended to maintain good contrast in viewing the chalkboard. The illuminance on the chalkboard and student's desk needs to be maintained at optimal recommended level (150–300 lux).[24] This can be achieved by recommending the teacher's to check the light levels using any mobile application. These recommendations can be informed during a patient's visit to eye care professional and can also be included as a part of school vision screening program.
Conclusion
Simple modifications of the visual task size and seating arrangements can aid children with low vision with better visibility of the chalkboard and reduced visual stress to manage in mainstream schools.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Gilbert CE, Ellwein LB. Refractive Error Study in Children Study Group. Prevalence and causes of functional low vision in school-age children: Results from standardized population surveys in Asia, Africa, and Latin America. Invest Ophthalmol Vis Sci. 2008;49:877–81. doi: 10.1167/iovs.07-0973. [DOI] [PubMed] [Google Scholar]
- 2.Thomas R, Barker L, Rubin G, Dahlmann-Noor A. Assistive technology for children and young people with low vision. Cochrane Database Syst Rev. 2015;18:CD011350. doi: 10.1002/14651858.CD011350.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gilbert C, Foster A, Négrel AD, Thylefors B. Childhood blindness: A new form for recording causes of visual loss in children. Bull World Health Organ. 1993;71:485–9. [PMC free article] [PubMed] [Google Scholar]
- 4.Kemmanu V, Hegde K, Giliyar SK, Shetty BK, Kumaramanickavel G, McCarty CA, et al. Prevalence of childhood blindness and ocular morbidity in a rural pediatric population in Southern India: The pavagada pediatric eye disease study-1. Ophthalmic Epidemiol. 2016;23:185–92. doi: 10.3109/09286586.2015.1090003. [DOI] [PubMed] [Google Scholar]
- 5.Sarva Shiksha Abhiyan: Framework for Implementation. Ministry of Human Resource Development and Department of School Education and Literacy. New Delhi: 2011. [Last accessed on 2017 Aug 21]. Available from: http://www.mhrd.gov.in/sarva-shiksha-abhiyan . [Google Scholar]
- 6.Punani B, Rawal N. Visual Impairment Handbook. 2nd Ed. Ahmadabad: Blind People's Association; 2000. pp. 239–96. [Google Scholar]
- 7.Negiloni K, Ramani KK, Sudhir RR. Do school classrooms meet the visual requirements of children and recommended vision standards? PLoS One. 2017;12:e0174983. doi: 10.1371/journal.pone.0174983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organisation. Change the Definition of Blindness Report. [Last accessed on 2017 Aug 21]. Available from: http://www.who.int/blindness/Change%20the%20Definition%20of%20Blindness.pdf .
- 9.International Statistical Classification of Diseases and Related Health Problems, ICD-10 Version. 2016. [Last accessed on 2017 Aug 21]. Available from: http://www.apps.who.int/classifications/icd10/browse/2016/en#/H54.1 .
- 10.Narayanasamy S, Vincent SJ, Sampson GP, Wood JM. Visual demands in modern Australian primary school classrooms. Clin Exp Optom. 2016;99:233–40. doi: 10.1111/cxo.12365. [DOI] [PubMed] [Google Scholar]
- 11.Grundy JW. A diagrammatic approach to occupational optometry and illumination. Optom Today. 1987;1:503–8. [Google Scholar]
- 12.Gilbert C, Foster A. Childhood blindness in the context of VISION 2020 – The right to sight. Bull World Health Organ. 2001;79:227–32. [PMC free article] [PubMed] [Google Scholar]
- 13.Chung ST, Mansfield JS, Legge GE. Psychophysics of reading. XVIII. The effect of print size on reading speed in normal peripheral vision. Vision Res. 1998;38:2949–62. doi: 10.1016/s0042-6989(98)00072-8. [DOI] [PubMed] [Google Scholar]
- 14.Lam N, Leat SJ. Barriers to accessing low-vision care: The patient's perspective. Can J Ophthalmol. 2013;48:458–62. doi: 10.1016/j.jcjo.2013.02.014. [DOI] [PubMed] [Google Scholar]
- 15.Schurink J, Cox RF, Cillessen AH, van Rens GH, Boonstra FN. Low vision aids for visually impaired children: A perception-action perspective. Res Dev Disabil. 2011;32:871–82. doi: 10.1016/j.ridd.2011.01.027. [DOI] [PubMed] [Google Scholar]
- 16.Khan SA, Shamanna B, Nuthethi R. Perceived barriers to the provision of low vision services among ophthalmologists in India. Indian J Ophthalmol. 2005;53:69–75. doi: 10.4103/0301-4738.15293. [DOI] [PubMed] [Google Scholar]
- 17.Gur SL. Pediatric low vision management. Sci J Delhi Ophthalmol Soc. 2015;26:81–7. [Google Scholar]
- 18.Lennon J, Harper R, Biswas S, Lloyd C. Paediatric low-vision assessment and management in a specialist clinic in the UK. Br J Vis Impair. 2007;25:103–19. [Google Scholar]
- 19.Legge GE, Ross JA, Isenberg LM, LaMay JM. Psychophysics of reading. Clinical predictors of low-vision reading speed. Invest Ophthalmol Vis Sci. 1992;33:677–87. [PubMed] [Google Scholar]
- 20.Bureau of Indian Standards. Indian Standard Recommendations for Basic Requirements of School Building IS: 8827±1978. Reaffirmed. 2006. [Last accessed on 2017 Aug 21]. Available from: https://www.law.resource.org/pub/in/bis/S03/is.8827.1978.pdf .
- 21.Kalloniatis M, Johnston AW. Visual characteristics of low vision children. Optom Vis Sci. 1990;67:38–48. doi: 10.1097/00006324-199001000-00009. [DOI] [PubMed] [Google Scholar]
- 22.Lovie-Kitchin JE, Bevan JD, Hein B. Reading performance in children with low vision. Clin Exp Optom. 2001;84:148–54. doi: 10.1111/j.1444-0938.2001.tb04958.x. [DOI] [PubMed] [Google Scholar]
- 23.Mehta AC. National University of Educational Planning and Administration and Unified District Information System for Education, Analytical Report. 2015-16. [Last accessed on 2017 May 25]. Available from: http://www.nuepa.org .
- 24.Bureau of Indian Standards. Indian Standard Code of Practice for Day Lighting of Educational Buildings (IS 7942: 1976). Reaffirmed. 2004. [Last accessed on 2017 Aug 21]. Available from: https://www.law.resource.org/pub/in/bis/S03/is.7942.1976.pdf .


