Abstract
We describe a case of 55-year-old male farmer presented with recurrent corneal abrasions with a spastic entropion in the left eye. Superior cornea showed typical nummular opacities suggestive resolved herpetic eye diseases. On further enquiry, he had similar episodes in the past. Contralateral eye was essentially normal. Following the botulinum toxin injection for the management of spastic entropion, subject developed reactivation of herpetic necrotizing stromal keratitis. Diagnostic corneal scrapings were negative for herpes simplex virus-1 antigen by immunofluorescence assay and for DNA by molecular techniques. The case was successfully managed with topical steroids and antiviral medications.
Keywords: Botulinum toxin, herpes simplex viral keratitis, reactivation of herpes
Epithelial herpes simplex keratitis is the most common form of the recurrent disease, typically presents mild clinical course, mostly which heals without any sequelae. Conversely, recurrent herpetic stromal keratitis is an immunopathologic process, can lead to stromal scarring, neovascularization, stromal thinning, and/or endothelial dysfunction and resultant astigmatism leading to visual impairment.[1] Anecdotally, various trigger factors have been implicated in the causation of herpetic reactivation, namely, immunosuppression, febrile condition, exposures to ultraviolet light, cold wind, systemic illness, surgery, menstruation, emotional stress, and minor local trauma; many patients can clearly foresee recurrent disease following a given event. Nevertheless, the HEDS epidemiological study did not show such a statistical correlation with above-stated risk factors. In published literature, the herpetic recurrence documented in the following circumstances use of topical medications such as steroids, prostaglandin analogs, intravitreal injections of anti-vascular endothelial growth factor agents, corneal-based laser procedures, laser iridectomy or trabeculoplasty, or any corneal interventions such as partial or full thickness keratoplasty particularly in those who had an active herpetic eye diseases in the past.[2,3]
In this context, we intend to present a case of unusual reactivation of herpetic necrotizing stromal keratitis 1 week after the periocular injection of botulinum toxin for the management of spastic entropion.
Case Report
We report a case that developed a reactivation of herpes simplex viral keratitis (HSK) following the periocular injection of botulinum toxin at a tertiary eye care center in South India. The clinical history, systemic, and ocular findings were assessed. A 55-year-old male farmer presented to us on September 2015 with chief complaints of redness, pain, and watering in the left eye for 10 days duration. On further enquiry, he had a viral keratitis in the left eye 6 years ago and had few episodes thereafter. Past 1 year, there were no recurrences. Systemic medical history was noncontributory. At the time of presentation, the patient was using moxifloxacin 0.3% eye drops every 3 hourly, homatropine, 2% eye, drops thrice daily, as prescribed by a local ophthalmologist.
On general examination, we found a healthy looking middle-aged man with no significant systemic abnormality, the examination of his eyes revealed: essentially normal right eye (OD), the distant visual acuity (VA) with his glasses was 20/20; however, the distant VA in the affected left eye with his glasses was 20/200, and there was no improvement with pinhole. The cornea showed multiple corneal abrasions inferiorly, wherever eyelashes brushed against the cornea due to spastic entropion whereas superiorly typical anterior stromal scarring with vascularization was observed [Fig. 1a]. Rest of the anterior and posterior segment of both eyes was normal. A diagnosis of corneal abrasions was due to spastic entropion, and herpetic stromal scarring in the left eye was made. He was started on chloramphenicol 0.5% eye drops four times a day; preservative free tear substitutes every 2 hourly, carboxymethyl cellulose eye ointment at bed time and lid scrubs with warm compresses were suggested. The patient was explained that his eyelid disorder might need an intervention. The patient was reviewed after 1 week, and his corneal abrasions were completely resolved. He was referred to an oculoplasty colleague for the management of spastic entropion, where periocular Injection botulinum toxin (Botox) 50 units were given. By the next visit, patient's eyelid condition had improved, but he developed a classic dendritic ulcer with stromal involvement typical of necrotizing stromal keratitis [Fig. 1b and c]. A diagnosis of herpes simplex viral necrotizing stromal keratitis secondary to botox injection was made. To rule out bacterial or fungal infection, the corneal scrapings were examined by direct microscopy (potassium hydroxide with calcofluor white and Gram stain) and cultured in 5% blood agar, chocolate agar, potato dextrose agar, and brain heart infusion broth. Corneal scrapings were also submitted for immunofluorescence assay for herpes simplex virus 1 (HSV1) antigen and polymerase chain reaction for HSV1 DNA.
Figure 1.
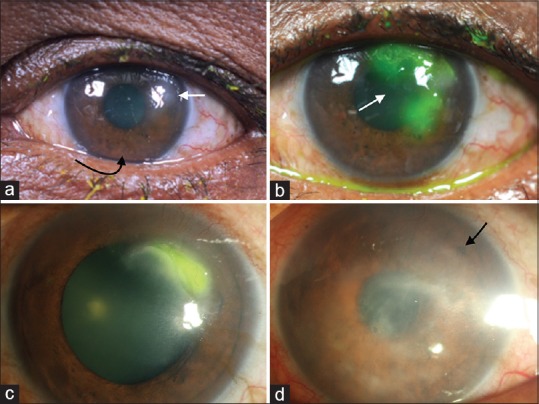
(a-d) The left eye corneal digital images of clinical course as observed in a chronological sequence. (a): At presentation, corneal epithelial abrasions were seen, where ever eyelashes brush against cornea due to lower lid spastic entropion (black curved arrow). Superiorly, tell-tale of herpetic stromal scarring noted (white arrow). (b) Typical fluorescein stained herpetic necrotizing stromal keratitis, which developed 1 week after periocular botulinum injection for a spastic entropion correction. (c) Resolving necrotizing stromal keratitis. (d) Recent slit lamp image taken 2 years after the initial botulinum injection showing extensive anterior stromal scarring due to recurrent episodes of stromal diseases (black arrow). Images a and b were captured through external digital camera and whereas c and d through slit lamp photography
The patient was started on acyclovir 3% eye ointment 5 times a day, Atropine sulfate 1% eye drops thrice daily, and tablet acyclovir 400 mg prophylaxis started considering the previous recurrent episodes.[4,5,6] Diagnostic corneal scrapings were negative for bacteria and fungus as well as for HSV1 antigen and for HSV1 DNA; however, clinically patient showed significant improvement with antiviral medications. Topical prednisolone acetate 1% eye drops 8 times a day was added at the end of 1 week after microbiological results were obtained and under the cover of topical acyclovir. Patient's corneal lesions resolved completely in 3–4 weeks after intense steroids under antiviral cover. Thereafter, the patient lost to follow-up for 2 long years, and his latest follow-up facilitated through our primary health-care worker. Recent examination showed extensive anterior stromal scarring with varying degrees of superficial vascularization [Fig. 1d]. Apparently, he had multiple episodes after discounting the systemic treatment. The patient did not comply to follow-ups and long-term systemic acyclovir prophylaxis in view of financial constraints.
Botulinum toxin use is a well-accepted treatment modality in the management of spastic eyelid disorders. A thorough MEDLINE search in English literature using search words did not show any previously published report of systemic or ocular HSK reactivation following the periocular botulinum toxin injection. We herein describe a case of unusual reactivation of HSK following the injection of botulinum toxin for the spastic entropion correction.
Discussion
HSK is an important cause of visual morbidity worldwide and a principal cause of corneal blindness in the developed countries, mainly due to its relentless relapses. Subclinical reactivation occurs periodically during which the live virus is shed, and patients are contagious, hundreds of reactivations can occur during lifetime. Nevertheless, clinical reactivation presents different patterns and severity of the disease depending on the site of reactivation and the associated risk factors.[1]
Although predictably, primary herpetic infection occurring early in life often resolves without any visual consequence. After the primary infection, the virus travels as an un enveloped particle by retrograde axoplasmic flow to the sensory ganglia where the virus remains dormant, gets incorporated in the host DNA and not amenable to eradication. Reactivation is the most intriguing aspect of immunopathogenesis of herpetic eye disease. With each episode of stromal keratitis, it is known to further escalate the risk of imminent relapses. Although complete immunopathogenesis in humans is still not fully understood, it has been described that aberrant mechanisms involving the CD4+ cells and many molecules conceivably play a critical role in causation of frequent relapses.[2,3,4,5,6]
Any surgical intervention on an eye with an antecedent history of herpetic eye disease increases the potential for viral reactivation. Although herpetic reactivating following local laser or surgical procedures remains controversial but published literature evidence that following the use of ocular laser or surgical procedures, i.e., laser-assisted in situ keratomileusis, laser iridotomy, laser trabeculoplasty, therapeutic laser keratectomy, cataract surgery, penetrating keratoplasty, and lamellar corneal transplantation. Plausible explanations are surgical or laser trauma to corneal nerves and or the cornea itself with secondary inflammation, a direct activating effect of laser light, and postoperative corticosteroid use.[6,7]
Topical antiglaucoma drugs, particularly the prostaglandin analogs have been reported as a trigger factor for stromal keratitis. Morales et al.[8] reported two cases of HSV blepharitis with Latanoprost use and Kaufman et al.[9] found that experimental HSV keratitis was worsened and recurred more often with Latanoprost therapy Schumer,[10] However, direct causal relationship has not been scientifically established between this drug therapy and rare side effects.
Diagnosis of herpetic eye disease is typically made based on characteristic history, prior episodes, tell-tale signs, and constellation of clinical features, which help in clinching the diagnosis. Despite negative microbiology, we did persist with antiviral and judiciously topical steroids, which resulted in complete resolution of corneal lesions that further substantiates the viral reactivation in our case.[6]
Herpetic reactivation following the periocular botulinum injection has not been described in ophthalmic and or systemic literature. We treated our patient with topical antiviral, which resulted in complete resolution of corneal lesions. The rationale for treating with antiviral is based on typical history, dendritic lesions, and negative diagnostic scrapings. This entire clinical scenario corroborates the fact that periocular botulinum injection might have triggered the herpetic reactivation. It is also biologically plausible that herpetic recurrence in our case might be unrelated to periocular botulinum injections, and or merely be a coincidence. Although this causal association difficult to prove, but too important to ignore.
Conclusion
In conclusion, the recurrence of necrotizing stromal keratitis in this report after the injection of periocular botulinum toxin illustrates that either the drug or periocular needle injury or combination of factors could have played a role in causation. Therefore, it is important to probe prior history herpetic eye disease and explain the possible risk of herpetic reactivation following use of periocular botulinum injections in ophthalmic practice. Therefore, antiviral prophylaxis should be strongly considered for all patients with antecedent history of herpetic eye diseases in the immediate perioperative period, particularly while under topical corticosteroids.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This study was financially supported by Hyderabad Eye Research Foundation., India.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Pavan-Langston D. Viral disease of the ocular anterior segment: Basic science and clinical disease. In: Foster S, Azar D, Dohlman C, editors. Reactivation of Herpes simplex viral keratitis Following the Botulinum Toxin Injection. Philadelphia, PA: Lippincott, Williams & Wilkins; 2005. pp. 297–397. [Google Scholar]
- 2.Herpetic Eye Disease Study Group. Predictors of recurrent herpes simplex virus keratitis. Cornea. 2001;20:123–8. doi: 10.1097/00003226-200103000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Herpetic Eye Disease Study Group. Psychological stress and other potential triggers for recurrences of herpes simplex virus eye infections. Arch Ophthalmol. 2000;118:1617–25. doi: 10.1001/archopht.118.12.1617. [DOI] [PubMed] [Google Scholar]
- 4.Herpetic Eye Disease Study Group. Oral acyclovir for herpes simplex virus eye disease: Effect on prevention of epithelial keratitis and stromal keratitis. Arch Ophthalmol. 2000;118:1030–6. [PubMed] [Google Scholar]
- 5.Herpetic Eye Disease Study Group. Acyclovir for the prevention of recurrent herpes simplex virus eye disease. N Engl J Med. 1998;339:300–6. doi: 10.1056/NEJM199807303390503. [DOI] [PubMed] [Google Scholar]
- 6.White ML, Chodosh J. Herpes Simplex Virus Keratitis: A Treatment Guideline- 2014. This Guideline was Approved by the Ocular Microbiology and Immunology Group in May 2014. This Guideline Was Reviewed and Accepted by the Hoskins Center for Quality Eye Care, American Academy of Ophthalmology in the Compendium of Evidence-Based Eye Care™. 2014 Jun [Google Scholar]
- 7.de Rojas Silva MV, Díez-Feijóo E, Javaloy J, Sánchez-Salorio M. Prophylactic perioperative antiviral therapy for LASIK in patients with inactive herpetic keratitis. J Refract Surg. 2006;22:404–6. doi: 10.3928/1081-597X-20060401-19. [DOI] [PubMed] [Google Scholar]
- 8.Morales J, Shihab ZM, Brown SM, Hodges MR. Herpes simplex virus dermatitis in patients using latanoprost. Am J Ophthalmol. 2001;132:114–6. doi: 10.1016/s0002-9394(01)01012-1. [DOI] [PubMed] [Google Scholar]
- 9.Kaufman HE, Varnell ED, Toshida H, Kanai A, Thompson HW, Bazan NG, et al. Effects of topical unoprostone and latanoprost on acute and recurrent herpetic keratitis in the rabbit. Am J Ophthalmol. 2001;131:643–6. doi: 10.1016/s0002-9394(00)00910-7. [DOI] [PubMed] [Google Scholar]
- 10.Schumer RA, Camras CB, Mandahl AK. Putative side effects of prostaglandin analogs. Surv Ophthalmol. 2002;47(Suppl 1):S219. doi: 10.1016/s0039-6257(02)00328-4. [DOI] [PubMed] [Google Scholar]


