Abstract
The purpose of the study was to report a case of ulcerative keratitis caused by an unusual algae Prototheca wickerhamii in a diabetic patient. This study design was a case report. A 46-year-old male, who was a known diabetic for 3 years, had an injury to the left cornea with the sparks of fire from wielding at work that developed into an ulcerative keratitis over a period of next 3 months as the patient was not on any medication. Corneal scraping culture report and Vitek 2 system investigation result confirmed it to be a P. wickerhamii infection. The patient was started on intensive topical 1% voriconazole and 5% natamycin for 1 month and with no improvement subsequently underwent penetrating keratoplasty. No recurrence of infection postoperatively was noted. This opportunistic algae rarely known to cause human eye infections is so far reported in either patients with severe systemic immunosuppression causing posterior segment eye involvement or as postcorneal surgery infections. We report an ulcerative keratitis by P. wickerhamii in a diabetic patient post corneal trauma with no prior ocular surgery.
Keywords: Algae, corneal infiltrate, penetrating keratoplasty, Prototheca wickerhamii
Corneal infection by unusual organism with no established medical management is challenging. We report a similar situation that we came across.
Case Report
A 46-year old male, with the history of injury 3 months back in the left cornea with sparks of fire while wielding at work gave a history of occasional redness, glare, and watering initially, which the patient ignored as it resolved spontaneously but later noticed a white spot in that eye. With no treatment, the lesion showed a gradual increase in size, and so he visited us. He was a known diabetic for 3 years before the incident. At presentation to us, his distant-corrected visual acuity in the right eye was 20/80 and left eye was 20/40. On the clinical and slit-lamp examination, his right eye was normal and the left eye was mildly congested, but no discharge was noted. The cornea showed a single, dense cheesy white, full thickness, 5 sq mm infiltrate with serrated margins that were well delineated and had a 3 sq mm central epithelial defect with 20% thinning [Fig. 1a]. The infiltrate was partly involving the pupillary area [Fig. 1b]. There was no anterior chamber reaction, and dense lens changes were noted [Fig. 1c]. Intraocular pressure was 18 mmHg in the right eye and normal digital tension in the left eye. Both eyes' dilated fundus examination was normal. Corneal scraping was collected from the left eye and was processed for microbiological investigations including direct smear and culture. Fungal elements were not seen in the KOH/Calcofluor stained smear, and bacteria or yeasts were not seen in the Gram-stained smear. With the clinical suspicion of an indolent fungal keratitis, the patient was started on intensive topical antifungals of 1% voriconazole and 5% natamycin hourly, along with suitable adjuvant treatment and strict control of diabetes. Culture for fungus was positive at the end of 10 days of incubation only from liquid medium (brain–heart infusion medium), and on subculturing onto solid medium, the growth was identified as Gram-positive spherical yeast cells [Fig. 2]. Based on the morphology, suspecting it to be an unusual yeast, it was subjected to identification byVitek 2 system and was identified as Prototheca wickerhamii.
Figure 1.
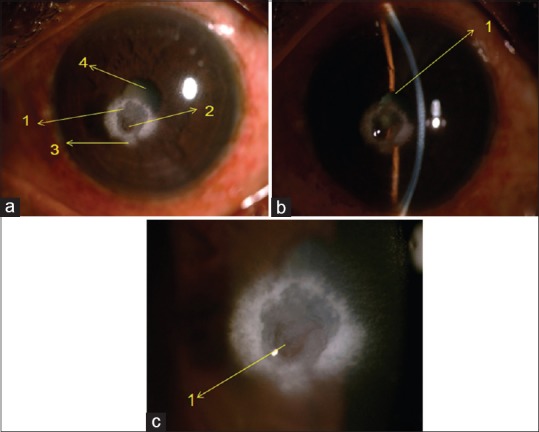
Silt lamp appearance of corneal Prototheca wickerhamii. (a) High magnification of diffuse elimination. (1) Area of thinning visible in transillumination. (b) Slit view of the ulcer. (1) Pupillary area involved partly. (c) Diffuse illumination of ulcer. (1) 3 sq mm central ulcer, (2) 20% area of thinning, (3) surrounding dense 5 sq mm white infiltrate involving the papillary area, (4) dense lens changes
Figure 2.
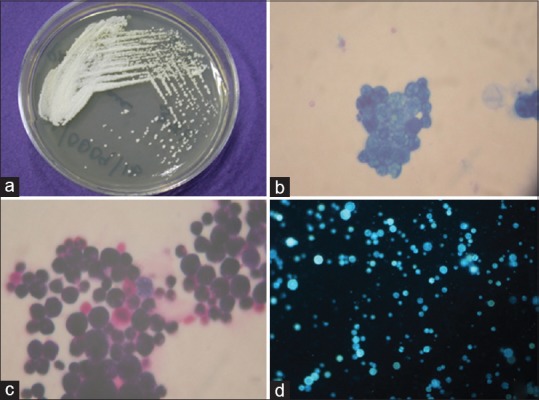
Macroscopic and microscopic appearance of Prototheca wickerhamii isolated from corneal scraping. (a) Colony morphology of P. wickerhamii on sabouraud dextrose agar. (b-d) Methylene blue stain (×100), Gram stain (×100), and potassium hydroxide/calcofluor (×20) stained preparations showing the oospores of Prototheca wickerhamii
Since there was no clinical improvement for more than a month of medical management, the patient underwent therapeutic penetrating keratoplasty, with 8 mm diameter graft to make sure a minimum of 2 mm clear zone to encompass the infiltrate was left. Graft was anchored with 16 10-0 nylon interrupted sutures. Postoperatively, the patient was on continued intensive topical antifungals; there was no sign of recurrence. The corneal button was subjected to microbiological investigations, and the culture confirmed the algae which was identified by automated Vitek 2 system as P. wickerhamii. Corneal button subjected to histopathology showed focal defects in epithelial and Bowman's layers with no cellular infiltration of stroma with normal Descemet's membrane and sparse endothelium. Gomori's Methenamine Silver (GMS) stain was negative. Postoperatively, patient continued topical voriconazole for 1 month, and steroid was started after 3 weeks and he is maintaining clear graft, and the eye is uninflammed with no recurrence of infection for a period of 2 months of postoperative follow-up.
To confirm the identification of P. wickerhamii, we used primer set specific for P. wickerhamii targeting 18Sr RNA gene, forward primer 5′-TCA AAA AGT CCC GGC TAA TCT CGT GC-3′, reverse primer 5′-CGC TTT CGT GCC TCA ATG TCA GTG TT-3′, with the annealing temperature of 58°C, 35 cycles as described by Hariprasad et al.[1] However, the polymerase chain reaction (PCR) profile was optimized by us with the denaturation at 94°C annealing at 58°C, and extension at 72°C, for 35 cycles and the expected product was 319 base pairs (bp). The PCR performed yielded 319 bp specific product [Fig. 3] and further DNA sequencing performed with the amplified product also confirmed it to be P. wickerhamii. The sequences were also deposited in the Genbank (Genbank accession number for SUB3006650 seq1 MF796662).
Figure 3.
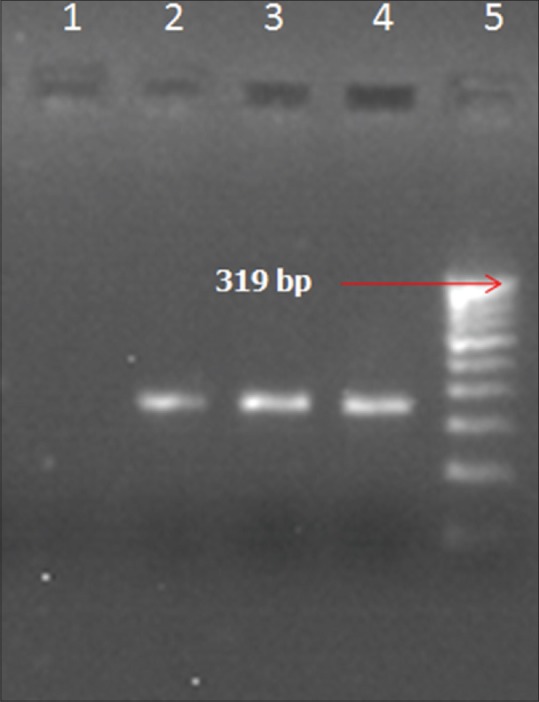
Agarose Gel Electro photogram showing the amplified products of polymerase chain reaction targeting 18Sr RNA gene of Prototheca wickerhamii Genome. Lane 1: Negative control – Negative. Lane 2: M_0009/16 (Prototheca wickerhamii isolate in 10μl DNA) – Positive. Lane 3: M_0009/16 (Prototheca wickerhamii isolate in 15μl DNA) – Positive. Lane 4: M_0009/16 (Prototheca wickerhamii isolate in 15μl DNA-duplicate) – Positive. Lane 5: Molecular weight marker (100 bp ladder)
Discussion
Prototheca is eukaryotic fungus-like species, belonging to the kingdom Protista. Kruger first isolated it from mucous flux of Tilia and Ulmus spp. in the year 1894.[2] In 1913, Chodat reclassified them as algae due to their internal spore formation identical to that of the green algae Chlorella.[3] Unlike chlorella, Prototheca lacks chloroplasts and has two layered, instead of three-layered cell wall by electron microscopy.
They are unicellular, spherical in shape, and of diameter ranging from 3 to 30 μm. They differ from both bacteria and fungus as their cell wall shows the absence of muramic acid and glucosamine, respectively.[4]
Prototheca is ubiquitous in nature, and their reproduction is asexual and often endemic in cattle and commonly reported as bovine mastitis due to repeated trauma of teats. For long, it was considered nonpathogenic to human thought to be a skin saprophyte and even initial species isolated from blood and feces were interpreted as contaminants. The first human protothecal infection was reported by Ashforth in 1930 from a patient's skin lesion suffering from sprue in Sierra Leone.[5]
Out of the five species of Prototheca classified based on physiological characteristics by Arnold and Arhean in 1972,[6] only two species namely wickerhamii and Zopfii are known to have caused more than 100 human infections so far. Wickerhamii is more common than zopfii. Among Zopfii, genotype 1 is nonpathogenic, whereas genotype 2 is pathogenic to human.[7] The definitive diagnosis of Protothecal infection usually depends on morphological identification of organism in wet slide preparations of cultures or direct identification in tissue specimens.[4] The speciation of Prototheca ultimately depends on carbohydrate assimilation tests or using the API strip series (bioM'erieux, Marcy l'Etoile, Paris, France) applicable for yeasts, the Vitek yeast identification database (bioM'erieux, Marcy l'Etoile, Paris, France), the Vitek 2 test (bioM'erieux, Marcy l'Etoile, Paris), and the RapidID Yeast Plus test (Remel, Santa Fe, NM, USA), but several clues can be found in tissue staining.[4] Reports on molecular techniques[8] and mass spectrometry[9] for the identification of Prototheca are available.
Prototheca species have simple nutritional requirements and readily grow on a variety of media. Sabouraud dextrose agar (SDA) without cycloheximide, beef infusion broth, blood agar, and brain heart infusion agar are suitable for culturing. Growth is optimized between 25 and 37°C and proliferate within 48 h usually as soft, wet, yeast-like, white-to-tan colonies. Colony morphology varies depending on the culture medium and nutrition used for growth. Pore suggested Prototheca selective isolation medium with a combination of flucytosine and potassium hydrogen phthalate that inhibits most bacteria and fungus and it allows isolation even from densely contaminated sources.[4] Wet mount of culture material can be stained by lactophenol cotton blue or calcofluor-white, and the characteristic endosporulating sporangia or morula of Prototheca can be noted. Wickerhamii has a typical symmetrical daisy-shaped morula that helps to distinguish it from Zopfii. Prototheca organisms from tissue specimen stain positive with periodic aid-Schiff stains with and without diastase, Gridley fungus stain and Grocott modification of GMS.
Prototheca causes both exogenous and endogenous infections and is nontransmissible. Exogenous local infection often seen in immunocompetent patients occurs by direct exposure, traumatic inoculation, or insect bite leading to source of infection. Workers in rice paddies and fishers are at high risk of exposure to contaminant source of infection. The three known common clinical forms of human protothecosis are cutaneous, olecranon bursitis, and disseminated.[10,11]
Protothecal retinitis has been reported in literature on canine infections, and so far only three human ocular infections are published. Hariprasad et al. in 2005 reported first ocular infection of bilateral choroiditis by P. Wickerhamii algaemia in an immunocompromised patient with myelodysplastic syndrome.[1] In 2011, Solky et al. described a nonulcerative stromal keratitis that gradually leads to graft failure in a patient postpenetrating keratoplasty who had Fuchs endothelial dystrophy and uncontrolled steroid-induced glaucoma.[12] Recently, in 2016, protothecal infection of an eye with Boston type 1 keratoprosthesis in a patient with Stevens-Johnson Syndrome and chronic ocular surface disease and multiple systemic complications was reported by Ng et al.[13] Although low virulence was noted, treatment was difficult with persistence, recurrence, or even widespread dissemination as in immunocompromised individuals.
Etest (AB Biodisk, Solna, Sweden), broth and agar dilution, and agar disk diffusion tests have been adopted for the determination of minimum inhibitory concentrations (MICs) for Prototheca spp. by several authors. Since these were done identical to that developed and standardized for yeasts, reliability for evaluating algae remains unclear. Often Prototheca shows various susceptibility profiles with no correlation to in vitro results. And so treatment of protothecal infection remains controversial even after many reports on nonophthalmic clinical forms so far.
From the in vitro studies done so far on protothecosis, the algae is sensitive to amphotericin B and certain azoles such as fluconazole, itraconazole, and voriconazole. This is due to the presence of ergosterol in neutral lipid fraction of cell membrane, and voriconazole shows superior activity against wickerhamii having 4% ergosterol.[8,14] Phospholipid components of Prototheca enable them to be susceptible to polymyxin B. Imidazole susceptibility is due to free fatty acid fraction of their cell membrane.[4] Variable sensitivities are also noted to tetracycline, gentamycin, and amikacin, with synergistic activity between amphotericin B and tetracycline combination in vitro.[15] Furthermore, a wide range of agents with possible synergistic effects, including miltefosine, terbinafine, aminoglycosides, echinocandins, polymyxin, and pentamidine, have been described in the treatment of Prototheca spp. but with variable outcomes. Takaki et al. showed secondary resistance with a 3-year period of treatment to amphotericin B and fluconazole. Casal et al. showed the presence of beta-lactamase in zopfii that can inactivate several compounds.[4]
In cases of keratitis, medical management based on the above-mentioned susceptibility tests of Prototheca can be with topical Amphotericin B as first choice, since it was shown to have least MIC range of 0.09–1.56 to P. wickerhamii. Azoles with higher MIC and variable susceptibility can be used as the second line of medical management.[14] However, in the ocular infections by Prototheca reported so far, medical management with various agents has not been successful. Complete surgical removal of possible localized infective lesions such as in our patient with penetrating keratoplasty is curative of infection.
Conclusion
We report a case of ulcerative keratitis caused by an algae P. wickerhamii acquired postcorneal trauma, with no prior history of an eye surgery. Although keratitis due to algae is uncommon, it should be considered in the differential diagnosis of recalcitrant keratitis in patients with prior ocular surgery, local or systemic immunocompromised states, or also history of ocular trauma. Since identification of rare organisms such as Prototheca is difficult, a high level of clinical suspicion and microbiologist's assistance in using advanced techniques can aid in proper diagnosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Hariprasad SM, Prasad A, Smith M, Shah GK, Grand MG, Shepherd JB, et al. Bilateral choroiditis from Prototheca wickerhamii algaemia. Arch Ophthalmol. 2005;123:1138–41. doi: 10.1001/archopht.123.8.1138. [DOI] [PubMed] [Google Scholar]
- 2.Rodriguez E. Prototheca Infections. Harvard Wide Conference. 2003 Mar 19; [Google Scholar]
- 3.Chodat R. Monographies d'algues en culture pure. Mat Crypt Suisse. 1913;4:234–41. [Google Scholar]
- 4.Florl CL, Mayr A. Human protothecosis. Clin Microbiol Rev. 2007;20:230–42. doi: 10.1128/CMR.00032-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ashford B, Ciferri R, Dalmau L. A new species of Prototheca and a variety of the same isolated from the human intestine. Arch Protistk. 1930;70:619–38. [Google Scholar]
- 6.Arnold P, Ahearn DG. The systematics of the genus Prototheca with a description of a new species P. filamenta. Mycologia. 1972;64:265–75. [Google Scholar]
- 7.Liu YZ, Wang H, Zhu JH, Han DM, Kudinha T, Kong FR, et al. Isobaric tag for relative and absolute quantitation-based comparative proteomic analysis of human pathogenic Prototheca zopfii genotype 2 and environmental genotype 1 strains. J Microbiol Immunol Infect. 2016 doi: 10.1016/j.jmii.2016.07.003. pii: S1684-1182(16)30072-X. [DOI] [PubMed] [Google Scholar]
- 8.McMullan B, Pollett S, Biswas C, Packham D. Successful treatment of cutaneous protothecosis with liposomal amphotericin and oral itraconazole. Med Mycol Case Rep. 2016;12:21–3. doi: 10.1016/j.mmcr.2016.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Murugaiyan J, Ahrholdt J, Kowbel V, Roesler U. Establishment of a matrix-assisted laser desorption ionization time-of-flight mass spectrometry database for rapid identification of infectious achlorophyllous green micro-algae of the genus prototheca. Clin Microbiol Infect. 2012;18:461–7. doi: 10.1111/j.1469-0691.2011.03593.x. [DOI] [PubMed] [Google Scholar]
- 10.Pal M, Abraha A, Rahman MT, Dave P. Protothecosis: An emerging algal disease of humans and animals. Int J Life Sci Biotechnol Pharm Res. 2014;3:1–13. [Google Scholar]
- 11.Torres HA, Bodey GP, Tarrand JJ, Kontoyiannis DP. Protothecosis in patients with cancer: Case series and literature review. Clin Microbiol Infect. 2003;9:786–92. doi: 10.1046/j.1469-0691.2003.00600.x. [DOI] [PubMed] [Google Scholar]
- 12.Solky AC, Laver NM, Williams J, Fraire A. Prototheca wickerhamii infection of a corneal graft. Cornea. 2011;30:1173–5. doi: 10.1097/ICO.0b013e3182011f28. [DOI] [PubMed] [Google Scholar]
- 13.Ng J, Minckler D, Walsh TJ, Farid M. An intractable case of prototheca keratitis and chronic endophthalmitis in Stevens-Johnson syndrome with Boston type 1 keratoprosthesis. Cornea. 2016;35:1257–60. doi: 10.1097/ICO.0000000000000949. [DOI] [PubMed] [Google Scholar]
- 14.Segal E, Padhye AA, Ajello L. Susceptibility of Prototheca species to antifungal agents. Antimicrob Agents Chemother. 1976;10:75–9. doi: 10.1128/aac.10.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Min Z, Moser SA, Pappas PG. Prototheca wickerhamii algaemia presenting as cholestatic hepatitis in a patient with systemic lupus erythematosus: A case report and literature review. Med Mycol Case Rep. 2012;2:19–22. doi: 10.1016/j.mmcr.2012.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]


