Abstract
Amniotic membrane transplantation is a useful in the management of corneal melts and descemetocele. We describe high-resolution anterior segment optical coherence tomography (OCT) (Optovue) in a patient with descemetocele who was managed surgically with amniotic membrane transplantation. A 60-year-old female presented with a corneal melt in the right eye. She was a case of rheumatoid arthritis and was on systemic treatment with immunomodulators. Slit lamp examination revealed a severe thinning paracentrally. High-resolution OCT was performed at the site of descemetocele. She underwent amniotic membrane transplantation using fibrin glue and bandage contact lens application. At 6 weeks postoperative, the bandage contact lens was removed. The area of thinning healed with scarring. OCT at the healed site revealed stable surface and an increase in stromal thickness to 281 μ this case describes the utility of amniotic membrane in the healing of sterile corneal melts by providing tectonic support and its integration in the stroma. The stromal healing and increased thickness at the site of descemetocele could be delineated on high-resolution OCT imaging.
Keywords: Amniotic membrane transplantation, corneal melt, descemetocele, optical coherence tomography
Rheumatoid arthritis is a chronic progressive disease characterized by a polyarticular synovitis and is a common cause of secondary Sjogrens syndrome. Patients can present with sterile melts, descemetocele, and perforations.[1] The management of sterile melts associated with rheumatoid arthritis needs an aggressive systemic control of the disease and surgical intervention to improve the tectonic stability of the cornea and prevent perforations in those presenting with corneal melts.[2]
Corneal melts can be managed by several methods such as cyanoacrylate glue application, amniotic membrane grafting, and patch grafts. Amniotic membrane transplantation is effective in treating persistent neurotrophic ulcers, nontraumatic corneal perforations, and descemetocele.[3,4,5,6] Apart from providing stromal and epithelial healing factors, amniotic membrane also can get integrated into the stroma and contributes to increase in stromal volume.[7,8,9]
Optical coherence tomography (OCT), first introduced in 1991, is a high-speed, high-resolution, noncontact imaging technique developed for noninvasive cross-sectional imaging in biological systems.[10] Herein, we describe the high-resolution OCT (Optovue RTvue) findings in a patient with sterile corneal melt with descemetocele and was successfully managed with amniotic membrane transplantation.
Case Report
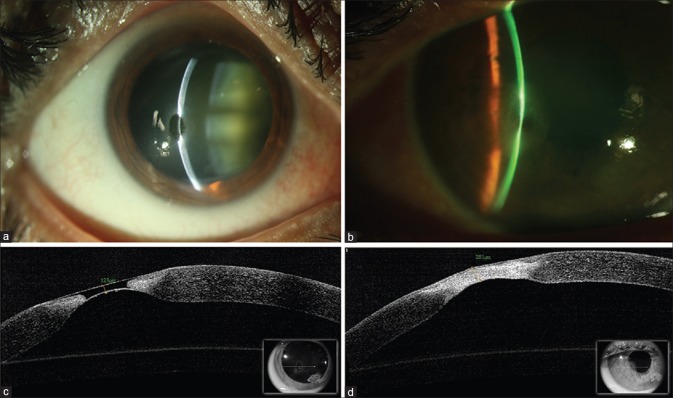
A 60-year-old female presented with complaints of redness, tearing, and irritation in the right eye of 1-week duration. She had rheumatoid arthritis and was on hydroxychloroquine, Vitamin D and calcium supplements for 8 years. The best-corrected visual acuity was 20/60 in the right eye and 20/80 in the left eye. Slit lamp examination of the right eye revealed a paracentral descemetocele with surrounding cellular reaction [Fig. 1a]. Anterior chamber was well formed. OCT showed the area of extreme corneal melt with a slight bulge suggestive of descemetocele [Fig. 1b]. The left eye had an adherent leukoma in peripheral cornea. There was nuclear cataract in both eyes. The fundus examination was within normal limits. In view of the risk of impending perforation, the right eye underwent a double-layered amniotic membrane grafting. The surrounding 0.5–1 mm epithelium around the site of melt was debrided carefully using a 15 No blade. The first layer of amniotic membrane was fashioned to cover the crater of melt using fibrin glue. The second layer of amniotic membrane was secured over smaller graft using fibrin glue and was approximately 1–1.5 mm larger to cover the site of defect including the debrided area. Thereafter, a bandage contact lens was placed on the surface to anchor the membrane and prevent dislodgement. The patient was treated with a broad-spectrum antibiotic every 6 hourly for 1 week, cyclosporine 0.1% eye drops twice a day, preservative-free artificial tears every 2 hourly, and advised to consult her rheumatologist in view of the corneal melt. At 6-week follow-up, the bandage contact lens was removed. The best-corrected visual acuity was 20/60. The site of descemetocele had healed well [Fig. 1c]. OCT image was captured from the site of the previous descemetocele taking care of alignment in the same axis as baseline [Fig. 1b and d insets]. OCT showed a stable surface, continuity with the surrounding epithelium with increased stromal thickness to 281 μ at the site of melt [Fig. 1d]. The patient was advised to continue preservative-free artificial tears and systemic medications as per the advice of her treating rheumatologist.
Figure 1.
(a) Slit lamp photograph of the right eye showing significant thinning paracentrally. (b) High-resolution optical coherence tomography at the site of corneal melt and descemetocele. (c) Slit lamp photograph at 6 weeks showing scarring and increased stromal thickness at the site of melt. (d) High-resolution optical coherence tomography showing the healed area with epithelization and incorporation of amniotic membrane at the site of descemetocele. The stromal thickness measured 281 μ. The line scan (inset) shows the same area of imaging as obtained at baseline before amniotic membrane transplantation
Discussion
High-resolution OCT is a useful tool in delineating the corneal structures. The resolution of RTvue (Optovue) OCT is 5 μ. Hence, it can help in characterizing and monitoring of various corneal pathologies. In the case described here, the healing pattern at the site of descemetocele managed with amniotic membrane grafting was studied using OCT imaging. The postoperative OCT [Fig. 1d] after complete healing at 6 weeks showed integration of amniotic membrane with epithelialization of the entire area. The OCT delineated continuity of surrounding cornea epithelium over the affected area. There was a noticeable increase in stromal thickness on clinical slit lamp examination, and this was quantified at the site of descemetocele using the caliper tool on OCT. As the amniotic membrane was sized and used to cover the area of the defect, it is likely that the increased thickness at the site of descemetocele is seen due to the integration of the amniotic membrane in the stroma, an observation well-documented in previous histologic studies.[7,9]
Although the use of amniotic membrane in corneal melts offers an advantage of increasing the stromal mass by its integration at the site of melt or perforation, the demerits of its usage could be a potential increase in haze in the melts that involve the central visual axis.[11] Rare cases of infection after amniotic membrane transplantation have also been reported.[12]
Conclusion
OCT imaging of descemetocele and their management with various techniques can help in documentation and characterizing of the exact nature of healing pattern.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Tong L, Thumboo J, Tan YK, Wong TY, Albani S. The eye: A window of opportunity in rheumatoid arthritis? Nat Rev Rheumatol. 2014;10:552–60. doi: 10.1038/nrrheum.2014.85. [DOI] [PubMed] [Google Scholar]
- 2.Bernauer W, Ficker LA, Watson PG, Dart JK. The management of corneal perforations associated with rheumatoid arthritis. An analysis of 32 eyes. Ophthalmology. 1995;102:1325–37. doi: 10.1016/s0161-6420(95)30867-6. [DOI] [PubMed] [Google Scholar]
- 3.Solomon A, Meller D, Prabhasawat P, John T, Espana EM, Steuhl KP, et al. Amniotic membrane grafts for nontraumatic corneal perforations, descemetoceles, and deep ulcers. Ophthalmology. 2002;109:694–703. doi: 10.1016/s0161-6420(01)01032-6. [DOI] [PubMed] [Google Scholar]
- 4.Kim HK, Park HS. Fibrin glue-assisted augmented amniotic membrane transplantation for the treatment of large noninfectious corneal perforations. Cornea. 2009;28:170–6. doi: 10.1097/ICO.0b013e3181861c54. [DOI] [PubMed] [Google Scholar]
- 5.Lee SH, Tseng SC. Amniotic membrane transplantation for persistent epithelial defects with ulceration. Am J Ophthalmol. 1997;123:303–12. doi: 10.1016/s0002-9394(14)70125-4. [DOI] [PubMed] [Google Scholar]
- 6.Seitz B. Amniotic membrane transplantation. An indispensable therapy option for persistent corneal epithelial defects. Ophthalmologe. 2007;104:1075–9. doi: 10.1007/s00347-007-1661-3. [DOI] [PubMed] [Google Scholar]
- 7.Resch MD, Schlötzer-Schrehardt U, Hofmann-Rummelt C, Sauer R, Kruse FE, Beckmann MW, et al. Integration patterns of cryopreserved amniotic membranes into the human cornea. Ophthalmology. 2006;113:1927–35. doi: 10.1016/j.ophtha.2006.03.065. [DOI] [PubMed] [Google Scholar]
- 8.Resch MD, Schlötzer-Schrehardt U, Hofmann-Rummelt C, Sauer R, Cursiefen C, Kruse FE, et al. Adhesion structures of amniotic membranes integrated into human corneas. Invest Ophthalmol Vis Sci. 2006;47:1853–61. doi: 10.1167/iovs.05-0983. [DOI] [PubMed] [Google Scholar]
- 9.Seitz B, Resch MD, Schlötzer-Schrehardt U, Hofmann-Rummelt C, Sauer R, Kruse FE, et al. Histopathology and ultrastructure of human corneas after amniotic membrane transplantation. Arch Ophthalmol. 2006;124:1487–90. doi: 10.1001/archopht.124.10.1487. [DOI] [PubMed] [Google Scholar]
- 10.Huang D, Swanson EA, Lin CP, Schuman JS, Stinson WG, Chang W, et al. Optical coherence tomography. Science. 1991;254:1178–81. doi: 10.1126/science.1957169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dua HS, Gomes JA, King AJ, Maharajan VS. The amniotic membrane in ophthalmology. Surv Ophthalmol. 2004;49:51–77. doi: 10.1016/j.survophthal.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 12.Khokhar S, Sharma N, Kumar H, Soni A. Infection after use of non-preserved human amniotic membrane for the reconstruction of the ocular surface. Cornea. 2001;20:773–4. doi: 10.1097/00003226-200110000-00023. [DOI] [PubMed] [Google Scholar]