Abstract
Background
Significant health disparities between sexual minority individuals (that is, lesbian, gay, bisexual, or transgender [LGBT]) and heterosexual individuals have been demonstrated.
Aim
To understand the barriers and facilitators to sexual orientation (SO) disclosure experienced by LGBT adults in healthcare settings.
Design and setting
Mixed methods systematic review, including qualitative, quantitative, and mixed methods papers following PRISMA guidelines.
Method
Study quality was assessed using the Mixed Methods Appraisal Tool (MMAT) and a qualitative synthesis was performed. Studies were included if their participants were aged ≥18 years who either identified as LGBT, had a same-sex sexual relationship, or were attracted to a member of the same sex.
Results
The review included 31 studies representing 2442 participants. Four overarching themes were identified as barriers or facilitators to SO disclosure: the moment of disclosure, the expected outcome of disclosure, the healthcare professional, and the environment or setting of disclosure. The most prominent themes were the perceived relevance of SO to care, the communication skills and language used by healthcare professionals, and the fear of poor treatment or reaction to disclosure.
Conclusion
The facilitators and barriers to SO disclosure by LGBT individuals are widespread but most were modifiable and could therefore be targeted to improve healthcare professionals’ awareness of their patients’ SO. Healthcare professionals should be aware of the broad range of factors that influence SO disclosure and the potential disadvantageous effects of non-disclosure on care. The environment in which patients are seen should be welcoming of different SOs as well as ensuring that healthcare professionals’ communication skills, both verbal and non-verbal, are accepting and inclusive.
Keywords: disclosure, general practice, LGBT, review, sexual orientation
INTRODUCTION
Significant health disparities between individuals identifying as part of a sexual minority (that is, lesbian, gay, bisexual, or transgender [LGBT]) and heterosexual individuals have been demonstrated internationally.1,2 In the UK, sexual orientation (SO) is a protected characteristic under the Equality Act (2010), which requires public services to promote and demonstrate equality for LGBT people. A large component of proving compliance with this mandate is monitoring SO, which is currently poorly done in the UK. National estimates of the adult LGBT population range from 1.7%3 to 9.9%,4 although the validity has been questioned.5 This has been recognised as a significant issue, and NHS England has worked with the LGBT Foundation and National LGB&T Partnership to implement an SO monitoring information standard from April 2017.6
Health disparities between heterosexual and LGBT people are still seen in mental health, with higher rates of anxiety and depression, self-harm, and suicide1,7–11 among the LGBT community, as well as in physical health. A recent UK-based review reported increased rates of some malignancies in the LGBT community, mixed diabetes rates, and higher rates of substance abuse, including binge drinking and smoking.1 Differences between sexual minority groups have also been reported, showing poorer mental and physical health in bisexual people of both sexes,8,9,11 as well as higher rates of high-risk health behaviours, such as smoking and excess alcohol intake.1,7,8,10 It has been noted that robust evidence comparing the different groups that make up the LGBT community is lacking,1 particularly in reference to transgender, queer, and intersex persons.
The most prominent theory for differences in health by SO is minority stress.12,13 This hypothesises that a combination and accumulation of internal and external stressors (such as stigma and victimisation, and the distress felt in response to stigma and concealment of one’s SO) interact to overcome an individual’s ability to cope, resulting in psychological and physical disease.13 A further theory is fundamental causes, which posits that advantaged groups in society have the skills and resources necessary to minimise risk of disease, as well as to harness the appropriate health resources to lessen the consequences of disease, should it occur.14 A Swedish study has presented support for the fundamental cause theory applicable to the LGBT community, describing increased rates of high-preventable diseases — such as ischaemic heart disease, chronic obstructive pulmonary disease (COPD), and lung cancer — in LGBT people, compared with heterosexual people.15
How this fits in
Significant health disparities exist between sexual minority (that is, lesbian, gay, bisexual, or transgender [LGBT]) and heterosexual individuals. Disclosure of sexual orientation (SO) in health care links to both the minority stress and fundamental cause theories in the context of accessing appropriate services, and is therefore likely to be a contributing factor in these health differences. Incorporating more LGBT-specific knowledge and communication skills into undergraduate medical education is essential in aiding SO disclosure. Altering the healthcare environment, such as displaying signs or symbols that convey an accepting atmosphere — for example, a rainbow symbol or the Human Rights Campaign logo — may also help.
Disclosure of SO in health care links to both the minority stress and fundamental cause theories in the context of accessing appropriate services, and is therefore likely to be a contributing factor in the health differences. In line with this, a recent British review found that many LGBT people are reluctant to disclose their SO, and will sometimes delay care due to fear of disclosure, even in the face of inappropriate or less appropriate care.16 The purpose of this review was to investigate the barriers and facilitators to SO disclosure in health care by LGBT adults, with the aim of identifying factors that can be easily modified in healthcare education and practice to improve disclosure, and therefore ensure provision of appropriate care.
METHOD
Search strategy
A search of eight databases (AMED, CINAHL, Embase, MEDLINE, PsycINFO, RCNi, ScienceDirect, and Web of Science) was conducted in March 2017. Terms were chosen to include all standard gender categories and minority SOs, focusing on SO disclosure in healthcare settings or to a healthcare professional. The final search conducted was: ((disclos* OR reveal* OR openness) AND (lgb* OR gay OR bisexual OR lesbian OR msm OR wsw OR homosex*) AND (health* OR care OR consult*)). The authors excluded all editorials, commentaries, reviews, and conference abstracts. Only articles published after 2000 were considered to ensure recent barriers and facilitators were captured, and only those in English were included.
Inclusion and exclusion criteria
Participants were aged ≥18 years and samples contained at least some self-identified as LGBT. Furthermore, only studies that displayed data provided by the participants on the barriers and/or facilitators to disclosure (or non-disclosure) of SO to a healthcare professional were included. Studies that did not specify disclosure to a healthcare professional, or those outside a healthcare setting, were excluded. Although the authors recognise that transgender is a gender identity rather than an SO, they have included transgender as they were unable to disaggregate transgender from LGB data.
Study selection and data extraction
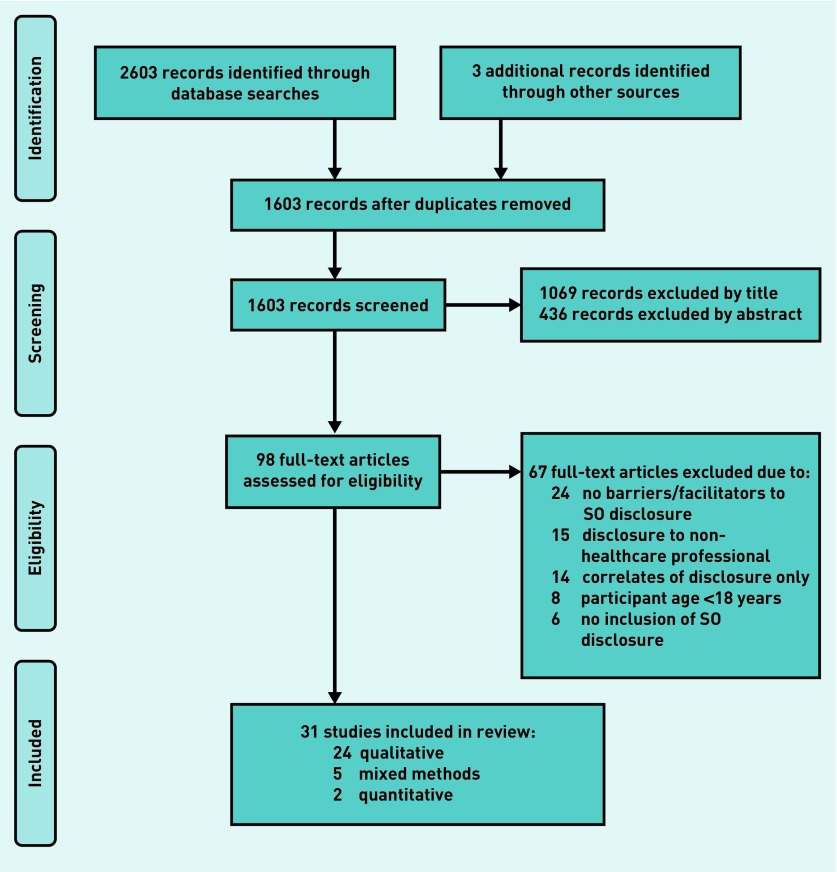
The process of systematic review is summarised using the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA)17 (Figure 1). Data were extracted using a proforma, followed by qualitative analysis.
Figure 1.
Preferred reporting items for systematic review and meta-analysis flow diagram for the inclusion of studies reporting barriers and facilitators to sexual orientation (SO) disclosure in healthcare.
Assessment of study quality
The Mixed Methods Appraisal Tool (MMAT) 18 was used to assess methodological quality. Two screening questions and four criteria for assessment were applied to each study, scoring sampling, measurement, analysis, and limitation consideration. This gave a score ranging from 0% (no criteria met) to 100% (all four criteria met) for each study, allowing one robust score to be used for multiple study types. Quality assessment was carried out by three assessors. Kappa scores were calculated to assess inter-rater variability.19
RESULTS
Studies identified
From 2603 records, 31 studies met the inclusion criteria (Figure 1; Table 1). Six studies presented data relevant to disclosure solely in a primary care setting, three in oncology, three in military medical settings, and one each in mental health and a home care setting. Eleven studies did not state or did not specify a precise healthcare setting but instead presented data from generic health settings, and six presented data from a variety of settings. In total, 2442 participants were included across the 31 studies identified for review.
Table 1.
Characteristics of studies included in the review (presented in chronological order)
| Author (publication year) country | Healthcare specialty | Study population | Selected sample characteristics (age, ethnicity, education level) | Sample size | Study design | Recruitment method | MMAT score, % |
|---|---|---|---|---|---|---|---|
| Barbara46 (2001) US | Not stated | Lesbian women | Age range 24–65 years; 69% white; 90% some college education | 32 | Qualitative, focus groups | Purposive, community-based | 75 |
| Beehler21 (2001) US | Primary care | Gay men | Median age 38 years (range 25–52); 82% white; 91% some college education | 11 | Qualitative, interview | Snowball | 50 |
| Stein29 (2001) US | Range — 77% primary care | Men and women of any sexual orientation | Mean age 45 years (range 19–83); 76% white; 80% at least college education | 575 | Quantitative descriptive, survey | Convenience, snowball; community-based | 25 |
| Boehmer32 (2004) US | Oncology | Lesbian and bisexual women | Mean age 49 years (range 26–67); 94% white; 97% at least college | 39 | Qualitative, interview | Purposive, community-based snowball | 75 |
| Clover48 (2006) UK | Not specified | Gay men | Age range 60–75 years; 100% white | 10 | Qualitative, interview | Purposive, community-based | 50 |
| McDonald50 (2006) Canada | Not specified | Lesbian women | Age range 26–56 years; 100% white; 73% at least some college education | 15 | Qualitative, interview | Purposive, community-based | 25 |
| Bjorkman40 (2007) Norway | Primary care | Lesbian women | Mean age 41 years (range 28–59); all white; all well educated | 6 | Qualitative, focus groups | Convenience, online | 75 |
| Mulligan35 (2007) Australia | Not specified | Lesbian and bisexual women | Age range 20–71 years | 47 | Qualitative, interview | Purposive, online, and community-based | 50 |
| Adams20 (2008) New Zealand | Primary care | Gay men | Not specified | 50 | Qualitative, focus groups | Not specified | 50 |
| Bjorkman31 (2009) Norway | Any, majority primary care | Lesbian women | Age range 18–≥60 years (68% aged 20–39); 87% Norwegian native; 67% some college education | 121 | Qualitative, online | Convenience, online questionnaire | 75 |
| Politi36 (2009) US | Not specified | Women of any sexual orientation | Mean age 55 years; 98% white; 73% at least college education | 40 | Qualitative, interview | Convenience, community-based | 50 |
| Daley41 (2012) Canada | Mental health | Lesbian women | Age range 20–58 years; 83% white | 18 | Qualitative, interview | Purposive, healthcare, and community | 75 |
| Biddix44 (2013) US | Military | Gay and bisexual men | Age range 18–47 years (56% 18–27); 86% white; 91% some college education | 30 | Quantitative, descriptive survey | Convenience, online | 0 |
| Johnson22 (2014) US | Not specified | Non-heterosexual women | Mean age 20 years (range 18–23); 77% white; all university students | 9 | Qualitative, interview | Purposive, online | 75 |
| Koh23 (2014) Australia | Primary care | Lesbian, gay, bisexual, or transgender men and women | Modal age 20–29 years (range 18–≥60) | 99 | Qualitative, online questionnaire | Purposive, online, and print | 75 |
| Sharek38 (2014) Ireland | Range | Lesbian, gay, bisexual, or transgender men and women | 59% aged 55–59 years | 144 survey + 36 interview | Mixed methods | Convenience, print/events/online | 50 |
| Sherman28 (2014) US | Military | Lesbian, gay, bisexual, or transgender men and women | >50% aged 40–59 years; 84% white | 58 | Mixed methods | Convenience, healthcare, online, and community | 0 |
| Wirtz49 (2014) Malawi | Range | Men who have sex with men | Not specified | 8 | Qualitative, interview | Responder-driven, purposive | 75 |
| Law34 (2015) Canada | Primary care | Lesbian, gay, bisexual, or transgender men and women | Mean age 32 years; 91% university education | 12 | Qualitative, interview | Purposive, snowball | 75 |
| Marques24 (2015) Portugal | Not specified | Lesbian women | Mean age 37 years (range 21–63) | 30 | Qualitative, interview | Snowball | 75 |
| Mattocks25 (2015) US | Military | Lesbian women | Age range 41–50 years; 35% white, 30% Hispanic, 15% African American | 20 | Mixed methods | Purposive, print, and healthcare | 0 |
| Quinn42 (2015) US | Not specified | Men and women of any sexual orientation | Not specified | 632 | Mixed methods | Purposive, online | 50 |
| Underhill39 (2015) US | Range | Men who have sex with men | Median age 27 years (male sex workers); median age 39 years (MSM); 76% white; 40–50% college education | 56 | Qualitative, interview | Convenience, snowball | 75 |
| Fish33 (2016) UK | Oncology | Lesbian, gay, or bisexual men and women | Mean age 54 years (range 41–71) | 15 | Qualitative, interview | Purposive, community, and web-based | 75 |
| Furlotte47 (2016) Canada | ‘Home care’ | Lesbian, gay, bisexual, or transgender men and women and their partners | Mean age 64 years (range 39–75); 96% white | 24 (12 couples) | Qualitative, individual and paired interviews | Web-based, purposive, snowball | 75 |
| Legere45 (2016) Canada | Oncology | Lesbian and bisexual women | 2 in 20s, 4>40 years; 28% black | 7 (6 patients, 1 HCP) | Qualitative, interview | Purposive, print, and online | 100 |
| Munson26 (2016) New Zealand | Primary care | Lesbian and bisexual women | Age range 23–47 years; 83% higher education | 6 | Qualitative, interview | Purposive, snowball | 100 |
| Roller27 (2016) US | Not specified | Lesbian and bisexual women | Mean age 41 years (range 21–59); all white; 67% college degrees | 13 | Qualitative, interview | Purposive, online | 75 |
| Venetis30 (2017) US | Not specified | Lesbian, gay, bisexual, or transgender men and women | Mean age 28 years (range 21–44); 66% white | 24 | Qualitative, interview | Purposive, community and online, snowball | 100 |
| Wanyenze43 (2016) Uganda | Not specified | Men who have sex with men | 50% aged 21–25 years | 85 + 61 key informants | Mixed methods | Purposive, snowball, responder-driven | 0 |
| Rose37 (2017) International | Oncology or primary care | Gay and bisexual men | Mean 64 years; 67% white | 124 + 21 partners | Qualitative, interview | Purposive, online, and postal | 50 |
HCP = healthcare professional. MMAT = Mixed Methods Appraisal Tool. MSM = men who have sex with men.
Data synthesis
The barriers and facilitators identified are presented in four overarching themes (Box 1).
Box 1. Facilitators and barriers to sexual orientation disclosure in health care.
| Facilitators | References | Barriers | References |
|---|---|---|---|
| Moment of disclosure | Moment of disclosure | ||
|
|
|
||
| Communication skills of healthcare professional | Communication skills of healthcare professional | ||
| Response to a direct question | 21,23,26–28,31,33,34,36,37,39,41,44,45 | Response to a direct question | 25,27,30,41 |
| Inclusive language | 30,34,36,40,41 | Heteronormative language | 26,34 |
| Open body language | 23,34,36,41–43 | Closed body language | 41 |
| No opportunity in conversation | 33,37 | ||
| Relevant to care | 20–30 | Irrelevant to care | 21,23–25,27–29,31–39 |
| Written disclosure | 22,35,39,41,42,46 | Written disclosure | 26,36 |
| Confronting heteronormative assumptions | 21,27,29–31,33,40,47 | Conforming to heteronormative assumptions | 21,26,45,46 |
|
|
|
||
| Perceived outcome of disclosure | Perceived outcome of disclosure | ||
|
|
|
||
| Patient–provider confidentiality | 22 | Breach of confidentiality | 20,24,29,34,37,39,43,46,47,49 |
| Documented on medical record | 24 | Documented on medical record | 24,25,28,29,46 |
| Good/open healthcare professional response | 32 | Poor healthcare professional response | 23,24,29,30,37–41,43,46,48,49 |
| Embarrassment | 31,33,37,39,46 | ||
| Discrimination | |||
| Poorer care | 23,26–29,32,40,43,45,47,48 | ||
| Loss/impact on job | 25,43 | ||
| Loss of benefits | 25,28 | ||
| Criminalisation | 43,49 | ||
|
|
|
||
| Healthcare professional factors | Healthcare professional factors | ||
|
|
|
||
| Perceived accepting of LGBT | 32,34,39,40,43,46 | Perceived non-accepting of LGBT | 32,37,38,48 |
| Long relationship with patient | 23,39,47 | Long relationship with patient | 34 |
| Short relationship with patient | 39 | Short relationship with patient | 46 |
| Gender | 36,38,39 | Ill-informed of LGBT issues | 20,31,36,46,48 |
| LGBT | 20,25,32,38,41,46,48 | ||
|
|
|
||
| Environmental factors | Environmental factors | ||
|
|
|
||
| Location/setting | 35 | Location/setting | 32,35,38,39,44 |
| Accepting visual cues | 23,26,39,41,42,48,50 | Religious icons | 23 |
| Supportive community | 32,41 | Unsupportive community | 43,49 |
LGBT = lesbian, gay, bisexual, or transgender.
The moment of disclosure
Twenty studies commented on patients’ beliefs of the relevance of SO to health care as both a barrier and facilitator to disclosure; people who thought it was relevant were more likely to disclose,20–30 whereas those who thought it was irrelevant were less likely to reveal their identity.21,23–25,27–29,31–39 One participant felt the need to disclose to enable their healthcare professional to provide ‘more focused advice’ 24 and another thought their ‘gayness to be highly relevant to [their] health needs’.21 Others asked ‘what’s [my SO] got to do with, you know, my toe hurting?’ 28 and felt ‘ [SO] would only be important if a problem was discovered’.36
Communication factors, such as using inclusive language30,34,36,39–41 and open, welcoming body language,23,34,36,41–43 were seen as facilitators to disclosure whereas the opposites — closed-off or unfriendly body language41 and heteronormative language,26,34 such as using a male pronoun to identify a female patient’s partner, and vice versa — were viewed as barriers. There were mixed opinions on the merits of using direct questions to explore a patient’s SO. The majority of participants appreciated being asked and felt this was a good way to facilitate open communication between patient and provider,21,23,26–28,31,33,34,36,37,39,41,44,45 but a small number did not agree.25,27,30,41 There were similarly mixed views of the benefits of patient registration forms to document SO. Some described their delight at finding a registration form that included their SO as an option,35 whereas many felt their SO was not accommodated by the options presented.26,36 Most described these types of written disclosure as a facilitator to disclosure,22,35,39,41,42,46 but only if they were adapted to be more inclusive and depict a broad spectrum of SOs.22
The final barrier at the moment of disclosure was the patient’s response to heteronormative assumptions. This was most commonly identified in the context of contraception and sexual health, with the giving of only heterosexually appropriate advice.27,30,31,45
Perceived outcome of disclosure
Fear of discrimination, including receiving poor or unequal care,23,26–29,32,40,43,45,47,48 having a negative impact on their career25,43 or benefits,25,28 as well as criminalisation,43,49 were all cited as reasons not to disclose. In addition, many participants were hesitant to disclose for fear of a negative personal reaction from their healthcare professional,23,24,29,30,37–41,43,46,48,49 or feeling embarrassment or humiliation after disclosure.31,33,37,39,46 Many participants cited concerns of breaches in patient–provider confidentiality20,24,29,34,37,39,43,46,47,49 that would lead to non-clinical staff,47 their family and friends,34 or the wider community43,49 discovering their SO as reasons not to disclose. Similarly, documentation of SO in medical records was seen as a barrier to disclosure.24,25,28,29,46
Healthcare professional factors
The majority of patients were more likely to disclose to a healthcare professional with whom they had a long relationship.23,39,47 Seven studies reported an increased likelihood of disclosure if the healthcare professional was themselves a member of the LGBT community.20,25,32,38,41,46,48 Although having a heterosexual healthcare professional was not seen as a particular barrier to disclosure, a healthcare professional being perceived as accepting of the LGBT community, or of their patient being LGBT, was a significant facilitator.32,34,39,40,43,46
Environmental factors
Some participants preferred to disclose their SO in sexual health clinics rather than to their primary care provider.33 On the other hand, military44 and religious-affiliated32 settings were seen as impeding disclosure, as was care conducted in a group treatment setting.39 Most notably, seven studies commented on visual clues in the healthcare setting that facilitated disclosure.23,26,39,41,42,48,50 These included seeing leaflets, stickers, and posters that were deemed LGBT friendly, such as the Human Rights Campaign logo or a rainbow sign.41,42,48 Religious symbols or icons displayed in the healthcare professional setting were barriers.23
DISCUSSION
Summary
In the UK, it is estimated that only half of lesbian and gay people are out to their GP, with disclosure rates lower in bisexual people.16 The authors have found that the factors promoting or discouraging patient SO disclosure in health care are widespread and varied. The most commonly cited factors were associated with the patient–provider interaction, which may provide useful targets to improve disclosure rates. Factors that were deemed to either enhance or reduce SO disclosure among females were having SO documented in their medical record and using written forms as a means of disclosing SO, as well as the type of language used during a consultation. Perhaps the use of prompts to aid disclosure, such as having a partner, a written form, or picking up on clues from the healthcare professional’s speech, are more important to LGBT women than men as they may be more commonly assumed heterosexual, particularly in discussing their reproductive health,30,51 and are less frequently asked directly about their SO.28
Although almost all studies were conducted in countries where homosexuality is legal, two were not. In both of these, barriers to disclosure were almost exclusively explored: commonly, the effect of an unsupportive community, fears of discrimination, and breaches in confidentiality were described by participants. They were, unsurprisingly, the only two studies to mention criminalisation as a barrier. Although the factors explored were often extreme, ranging from not being treated by their healthcare professional at all, to the police being informed of the participant’s SO, and fears of being ostracised from their community, they were echoed to a lesser extent in studies based in other countries.
Strengths and limitations
Although this is the first review to include participants that are both men and women, as well as participants from any sexual LGBT subgroup, there are some limitations. The MMAT has shortcomings. Although it allows the authors to assess different study types with one tool, they often found it difficult to assess the methodological qualities of each study without assessing the quality of reporting. Further, the authors found the MMAT criteria to be fairly crude measures of quality, particularly for qualitative studies. The quality assessment was not taken into account when extracting data from each study, with all the evidence being treated equally. Additionally, most of the mixed methods studies had particularly weak evidence from the quantitative branch of the study. The richest and most appropriate data were extracted from the qualitative arms.
The studies included for review also have limitations. Sampling the LGBT community is recognised as difficult due to the hidden nature of the population. The authors recognise participants need to have disclosed their SO before being recruited to studies, so may not have the same barriers and facilitators to disclosure as those who had not disclosed at all. Furthermore, the participants from each study were largely homogenous, comprising mostly well-educated, white, middle-aged people, who are the groups most likely to disclose their SO.52–55
Comparison with existing literature
Studies with only correlates of SO disclosure were excluded as they were outside the remit of this review. They do include, however, important information on the effects of patient sex, age, ethnicity, and SO on disclosure. For example, LGBT people who are from ethnic minorities,52–55 or identify as bisexual,52,53,55–57 or do not have a college education,53,54,58 or have a low income53,54 are less likely to disclose their SO to a healthcare professional. There is mixed evidence for the effect of patient age53,54,58 and sex16,52,59 on disclosure. These are important factors to consider when implementing interventions in terms of targeting population groups.
Although useful to enhance the authors’ understanding of demographics and disclosure, the quantitative data also support the predominantly qualitative findings. For example, a recent study from Canada found that higher levels of self-esteem, having a partner, and higher levels of social support from friends were significantly associated with healthcare professionals knowing a patient’s SO, whereas participants with previous experiences of discrimination and higher levels of internalised homonegativity were less likely to discuss LGBT-related health issues with their healthcare professionals.60
Implications for research and practice
Although some of the factors identified in this study are fixed, some could be targeted to minimise the barriers to disclosure. Five of the studies in this review commented on healthcare professionals’ lack of LGBT-specific knowledge as a barrier to disclosure. This problem stems from the beginning of medical education, with one study noting a median of five LGBT-dedicated curriculum hours in US medical schools,61 and another study showing medical students in the UK lack confidence in the use of LGBT-specific health terms and their ability to locate LGBT-specific health information.62 Incorporating more LGBT-specific knowledge and communication skills into undergraduate medical education is essential to ensure that future healthcare professionals are armed with the tools they need to help their future patients disclose their SO, and then provide them with appropriate care and advice. The responsibility for medical education does not just sit within the undergraduate realm: there should be increased presence of LGBT-specific issues and appropriate communication tools in postgraduate curricula also.
At an institutional level, the design of healthcare settings should take into account the needs of LGBT patients. There are some changes that are easily implemented and inexpensive, including displaying signs or symbols that convey an accepting atmosphere, such as a rainbow symbol or the Human Rights Campaign logo, while others may take more time. It is important to ensure, however, that any healthcare setting changes are congruent with the beliefs of the healthcare professional working within them. A key intervention is the production of patient information leaflets that are accepting of the LGBT community and that consider the differing needs of LGBT individuals compared with heterosexual individuals, providing LGBT-specific information when necessary.
Individual healthcare professionals should be aware of the differing physical and psychological needs of the LGBT community and remain open minded regarding their patients’ SO. The authors encourage all healthcare professionals to reflect on their use of language, keeping an eye out for heteronormative phrases and assumptions, as well as those that may be inhibiting their patients’ ability to disclose, and consider using alternative terms. The most common example of this is referring to a patient’s partner as ‘he’ or ‘she’, rather than asking whether they are male or female or going further to ask whether the patient is, or ever has been, involved in a relationship with men, women, or both. Healthcare professionals should also consider asking questions about each patient’s SO in their daily practice, using open and accepting language. Further investigation into issues surrounding disclosure from a healthcare professional perspective would also provide a fuller understanding of the complexities surrounding SO disclosure in health care.
Ideally, robust population-level studies that include an accurate portrayal of the breadth encompassed within LGBT are needed. The current SO monitoring question in the UK has only five possible answers (heterosexual, gay/lesbian, bisexual, other, prefer not to say), which does not display the full spectrum of orientations and focuses only on sexual identity rather than attraction or behaviours. For example, an alternative means of monitoring those who describe themselves as ‘other’ would allow a much richer, and much needed, analysis of the population.
Funding
None given.
Ethical approval
Not applicable.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Hudson-Sharp N, Metcalf H. Inequality among lesbian, gay, bisexual, and transgender groups in the UK: a review of evidence. 2016 https://www.gov.uk/government/publications/inequality-among-lgbt-groups-in-the-uk-a-review-of-evidence (accessed 15 Jan 2018) [Google Scholar]
- 2.Institute of Medicine . The health of lesbian, gay, bisexual, and transgender people: building a foundation for better understanding. Washington, DC: IOM; 2011. [PubMed] [Google Scholar]
- 3.Office for National Statistics . Sexual identity, UK: 2015. Experimental official statistics on sexual identity in the UK in 2015 by region, sex, age, marital status, ethnicity, and NS-SEC. ONS; 2016. http://www.ons.gov.uk/peoplepopulationandcommunity/culturalidentity/sexuality/bulletins/sexualidentityuk/2015 (accessed 15 Jan 2018) [Google Scholar]
- 4.Public Health England Producing modelled estimates of the size of the lesbian, gay, and bisexual (LGB) population of England. 2017 http://www.gov.uk/government/uploads/system/uploads/attachment_data/file/585349/PHE_Final_report_FINAL_DRAFT_14.12.2016NB230117v2.pdf (accessed 15 Jan 2018) [Google Scholar]
- 5.LGBT Foundation, NHS England Sexual orientation monitoring: full specification. 2017. https://www.england.nhs.uk/wp-content/uploads/2017/10/sexual-orientation-monitoring-full-specification.pdf (accessed 22 Jan 2017)
- 6.Equality and Health Inequalities Unit NHS England response to the specific equality duties of the Equality Act 2010: NHS England’s equality objectives in equality information. 2017 http://www.england.nhs.uk/wp-content/uploads/2017/03/nhse-sed-response.pdf (accessed 15 Jan 2018) [Google Scholar]
- 7.Lindley LL, Walsemann KM, Carter JW. The association of sexual orientation measures with young adults’ health-related outcomes. Am J Public Health. 2012;102(6):1177–1185. doi: 10.2105/AJPH.2011.300262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Semlyen J, King M, Varney J, Hagger-Johnson G. Sexual orientation and symptoms of common mental disorder or low wellbeing: combined meta-analysis of 12 UK population health surveys. BMC Psychiatry. 2016;16:67. doi: 10.1186/s12888-016-0767-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Conron KJ, Mimiaga MJ, Landers SJ. A population-based study of sexual orientation identity and gender differences in adult health. Am J Public Health. 2010;100(10):1953–1960. doi: 10.2105/AJPH.2009.174169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sandfort TG, Bakker F, Schellevis FG, Vanwesenbeeck I. Sexual orientation and mental and physical health status: findings from a Dutch population survey. Am J Public Health. 2006;96:1119–1125. doi: 10.2105/AJPH.2004.058891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elliott MN, Kanouse DE, Burkhart Q, et al. Sexual minorities in England have poorer health and worse health care experiences: a national survey. J Gen Intern Med. 2015;30(1):9–16. doi: 10.1007/s11606-014-2905-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lick DJ, Durso LE, Johnson KL. Minority stress and physical health among sexual minorities. Perspect Psychol Sci. 2013;8(5):521–548. doi: 10.1177/1745691613497965. [DOI] [PubMed] [Google Scholar]
- 13.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995 Spec No: 80–94. [PubMed] [Google Scholar]
- 15.Bränström R, Hatzenbuehler ML, Pachankis JE, Link BG. Sexual orientation disparities in preventable disease: a fundamental cause perspective. Am J Public Health. 2016;106(6):1109–1115. doi: 10.2105/AJPH.2016.303051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mitchell M, Howarth C, Kotecha M, Creegan C. Sexual orientation research review. 2008 http://www.equalityhumanrights.com/sites/default/files/research_report_34_sexual_orientation_research_review.pdf (accessed 15 Jan 2018) [Google Scholar]
- 17.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pluye P, Robert E, Cargo M, et al. Proposal: a mixed methods appraisal tool for systematic mixed studies reviews. Montreal, QC: Department of Family Medicine, McGill University; 2011. [Google Scholar]
- 19.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- 20.Adams J, McCreanor T, Braun V. Doctoring New Zealand’s gay men. N Z Med J. 2008;121(1287):11–20. [PubMed] [Google Scholar]
- 21.Beehler GP. Original research: confronting the culture of medicine: gay men’s experiences with primary care physicians. J Gay Lesbian Med Assoc. 2001;5(4):135–141. [Google Scholar]
- 22.Johnson MJ, Nemeth LS. Addressing health disparities of lesbian and bisexual women: a grounded theory study. Womens Health Issues. 2014;24(6):635–640. doi: 10.1016/j.whi.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 23.Koh CS, Kang M, Usherwood T. ‘I demand to be treated as the person I am’: experiences of accessing primary health care for Australian adults who identify as gay, lesbian, bisexual, transgender, or queer. Sex Health. 2014;11(3):258–264. doi: 10.1071/SH14007. [DOI] [PubMed] [Google Scholar]
- 24.Marques AM, Nogueira C, de Oliveira JM. Lesbians on medical encounters: tales of heteronormativity, deception, and expectations. Health Care Women Int. 2015;36:988–1006. doi: 10.1080/07399332.2014.888066. [DOI] [PubMed] [Google Scholar]
- 25.Mattocks KM, Sullivan JC, Bertrand C, et al. Perceived stigma, discrimination, and disclosure of sexual orientation among a sample of lesbian veterans receiving care in the Department of Veterans Affairs. LGBT Health. 2015;2(2):147–153. doi: 10.1089/lgbt.2014.0131. [DOI] [PubMed] [Google Scholar]
- 26.Munson S, Cook C. Lesbian and bisexual women’s sexual healthcare experiences. J Clin Nurs. 2016;25(23–24):3497–3510. doi: 10.1111/jocn.13364. [DOI] [PubMed] [Google Scholar]
- 27.Roller CG, Sedlak CA, Draucker Burke C, et al. Managing the conversation: how sexual minority women reveal sexual orientation. J Nurse Pract. 2016;12(6):e259–e266. [Google Scholar]
- 28.Sherman MD, Kauth MR, Shipherd JC, Street RL. Communication between VA providers and sexual and gender minority veterans: a pilot study. Psychol Serv. 2014;11(12):235–242. doi: 10.1037/a0035840. [DOI] [PubMed] [Google Scholar]
- 29.Stein GL, Bonuck KA. Physician–patient relationships among the lesbian and gay community. J Gay Lesbian Med Assoc. 2001;5(3):87–93. [Google Scholar]
- 30.Venetis MK, Meyerson BE, Friley LB, et al. Characterizing sexual orientation disclosure to health care providers: lesbian, gay, and bisexual perspectives. Health Commun. 2017;32(5):578–586. doi: 10.1080/10410236.2016.1144147. [DOI] [PubMed] [Google Scholar]
- 31.Bjorkman M, Malterud K. Lesbian women’s experiences with health care: a qualitative study. Scand J Prim Health Care. 2009;27(4):238–243. doi: 10.3109/02813430903226548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Boehmer U, Case P. Physicians don’t ask, sometimes patients tell: disclosure of sexual orientation among women with breast carcinoma. Cancer. 2004;101(8):1882–1889. doi: 10.1002/cncr.20563. [DOI] [PubMed] [Google Scholar]
- 33.Fish J, Williamson I. Exploring lesbian, gay, and bisexual patients’ accounts of their experiences of cancer care in the UK. Eur J Cancer Care (Engl) 2016 doi: 10.1111/ecc.12501. [DOI] [PubMed] [Google Scholar]
- 34.Law M, Mathai A, Veinot P, et al. Exploring lesbian, gay, bisexual, and queer (LGBQ) people’s experiences with disclosure of sexual identity to primary care physicians: a qualitative study. BMC Fam Pract. 2015;16:175. doi: 10.1186/s12875-015-0389-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mulligan E, Heath M. Seeking open minded doctors — how women who identify as bisexual, queer, or lesbian seek quality health care. Aust Fam Physician. 2007;36(6):469–471. [PubMed] [Google Scholar]
- 36.Politi MC, Clark MA, Armstrong G, et al. Patient–provider communication about sexual health among unmarried middle-aged and older women. J Gen Intern Med. 2009;24(4):511–516. doi: 10.1007/s11606-009-0930-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rose D, Ussher JM, Perz J. Let’s talk about gay sex: gay and bisexual men’s sexual communication with healthcare professionals after prostate cancer. Eur J Cancer Care (Engl) 2017;26(1) doi: 10.1111/ecc.12469. [DOI] [PubMed] [Google Scholar]
- 38.Sharek DB, McCann E, Sheerin F, et al. Older LGBT people’s experiences and concerns with healthcare professionals and services in Ireland. Int J Older People Nurs. 2015;10(3):230–240. doi: 10.1111/opn.12078. [Epub 2014]. [DOI] [PubMed] [Google Scholar]
- 39.Underhill K, Morrow KM, Colleran C, et al. A qualitative study of medical mistrust, perceived discrimination, and risk behavior disclosure to clinicians by US male sex workers and other men who have sex with men: implications for biomedical HIV prevention. J Urban Health. 2015;92(4):667–686. doi: 10.1007/s11524-015-9961-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bjorkman M, Malterud K. Being lesbian — does the doctor need to know? Scand J Prim Health Care. 2007;25(1):58–62. doi: 10.1080/02813430601086178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Daley AE. Becoming seen, becoming known: lesbian women’s self-disclosures of sexual orientation to mental health service providers. J Gay Lesbian Ment Health. 2012;16(3):215–234. [Google Scholar]
- 42.Quinn GP, Sutton SK, Winfield B, et al. Lesbian, gay, bisexual, transgender, queer/questioning (LGBTQ) perceptions and health care experiences. J Gay Lesbian Soc Serv. 2015;27(2):246–261. doi: 10.1080/10538720.2015.1022273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wanyenze RK, Musinguzi G, Matovu JK, et al. ‘If you tell people that you had sex with a fellow man, it is hard to be helped and treated’: barriers and opportunities for increasing access to HIV services among men who have sex with men in Uganda. PLoS One. 2016;11(1):e0147714. doi: 10.1371/journal.pone.0147714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Biddix JM, Fogel CI, Perry Black B. Comfort levels of active duty gay/bisexual male service members in the military healthcare system. Mil Med. 2013;178(12):1335–1440. doi: 10.7205/MILMED-D-13-00044. [DOI] [PubMed] [Google Scholar]
- 45.Legere LE, MacDonnell JA. Meaningful support for lesbian and bisexual women navigating reproductive cancer care in Canada: an exploratory study. J Res Nurs. 2016;21(3):163–174. [Google Scholar]
- 46.Barbara AM, Quandt SA, Anderson RT. Experiences of lesbians in the health care environment. Women Health. 2001;34(1):45–62. [Google Scholar]
- 47.Furlotte C, Gladstone JW, Cosby RF, Fitzgerald KA. ‘Could we hold hands?’ Older lesbian and gay couples’ perceptions of long-term care homes and home care. Can J Aging. 2016;35(4):432–446. doi: 10.1017/S0714980816000489. [DOI] [PubMed] [Google Scholar]
- 48.Clover D. Overcoming barriers for older gay men in the use of health services: a qualitative study of growing older, sexuality, and health. Health Edu J. 2006;65(1):41–52. [Google Scholar]
- 49.Wirtz AL, Kamba D, Jumbe V, et al. A qualitative assessment of health seeking practices among and provision practices for men who have sex with men in Malawi. BMC Int Health Hum Rights. 2014;14:20. doi: 10.1186/1472-698X-14-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.McDonald C. Lesbian disclosure: disrupting the taken for granted. Can J Nurs Res. 2006;38(1):42–57. [PubMed] [Google Scholar]
- 51.Neville S, Henrickson M. Perceptions of lesbian, gay, and bisexual people of primary healthcare services. J Adv Nurs. 2006;55(4):407–415. doi: 10.1111/j.1365-2648.2006.03944.x. [DOI] [PubMed] [Google Scholar]
- 52.Durso LE, Meyer IH. Patterns and predictors of disclosure of sexual orientation to healthcare providers among lesbians, gay men, and bisexuals. Sex Res Social Policy. 2013;10(1):35–42. doi: 10.1007/s13178-012-0105-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bernstein KT, Liu KL, Begier EM, et al. Same-sex attraction disclosure to health care providers among New York City men who have sex with men: implications for HIV testing approaches. Arch Intern Med. 2008;168(13):1458–1464. doi: 10.1001/archinte.168.13.1458. [DOI] [PubMed] [Google Scholar]
- 54.Petroll AE, Mosack KE. Physician awareness of sexual orientation and preventive health recommendations to men who have sex with men. Sex Transm Dis. 2011;38(1):63–67. doi: 10.1097/OLQ.0b013e3181ebd50f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Johnson CV, Mimiaga MJ, Reisner SL, et al. Health care access and sexually transmitted infection screening frequency among at-risk Massachusetts men who have sex with men. Am J Public Health. 2009;99(Suppl 1):S187–S192. doi: 10.2105/AJPH.2007.127464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kamen CS, Smith-Stoner M, Heckler CE, et al. Social support, self-rated health, and lesbian, gay, bisexual, and transgender identity disclosure to cancer care providers. Oncol Nurs Forum. 2015;42(1):44–51. doi: 10.1188/15.ONF.44-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cochran SD, Mays VM. Disclosure of sexual preference to physicians by black lesbian and bisexual women. West J Med. 1988;149(5):616–619. [PMC free article] [PubMed] [Google Scholar]
- 58.Hirsch O, Löltgen K, Becker A. Lesbian womens’ access to healthcare, experiences with and expectations towards GPs in German primary care. BMC Fam Pract. 2016;17:162. doi: 10.1186/s12875-016-0562-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Klitzman RL, Greenberg JD. Patterns of communication between gay and lesbian patients and their health care providers. J Homosex. 2002;42(4):65–75. doi: 10.1300/J082v42n04_04. [DOI] [PubMed] [Google Scholar]
- 60.Coleman TA, Bauer GR, Pugh D, et al. Sexual orientation disclosure in primary care settings by gay, bisexual, and other men who have sex with men in a Canadian city. LGBT Health. 2017;4(1):42–54. doi: 10.1089/lgbt.2016.0004. [DOI] [PubMed] [Google Scholar]
- 61.Obedin-Maliver J, Goldsmith ES, Stewart L, et al. Lesbian, gay, bisexual, and transgender-related content in undergraduate medical education. JAMA. 2011;306(9):971–977. doi: 10.1001/jama.2011.1255. [DOI] [PubMed] [Google Scholar]
- 62.Parameshwaran V, Cockbain BC, Hillyard M, Price JR. Is the lack of specific lesbian, gay, bisexual, transgender, and queer/questioning (LGBTQ) health care education in medical school a cause for concern? Evidence from a survey of knowledge and practice among UK medical students. J Homosex. 2017;64(3):367–381. doi: 10.1080/00918369.2016.1190218. [DOI] [PubMed] [Google Scholar]