Abstract
During interprofessional intensive care unit (ICU) rounds each member of the interprofessional team is responsible for gathering and interpreting information from the electronic health records (EHR) to facilitate effective team decision-making. This study was conducted to determine how each professional group reviews EHR data in preparation for rounds and their ability to identify patient safety issues. Twenty-five physicians, 29 nurses, and 20 pharmacists participated. Individual participants were given verbal and written sign-out and then asked to review a simulated record in our institution’s EHR, which contained 14 patient safety items. After reviewing the chart, subjects presented the patient and the number of safety items recognised was recorded. About 40%, 30%, and 26% of safety issues were recognised by physicians, nurses, and pharmacists, respectively (p = 0.0006) and no item recognised 100% of the time. There was little overlap between the three groups with only 50% of items predicted to be recognised 100% of the time by the team. Differential recognition was associated with marked differences in EHR use, with only 3/152 EHR screens utilised by all three groups and the majority of screens used exclusively only by one group. There were significant and non-overlapping differences in individual profession recognition of patient safety issues in the EHR. Preferential identification of safety issues by certain professional groups may be attributed to differences in EHR use. Future studies will be needed to determine if shared decision-making during rounds can improve recognition of safety issues.
Keywords: Communication, interprofessional collaboration, interprofessional practice, quantitative method, simulation, team effectiveness
Introduction
Electronic health record (EHR) adoption by US hospitals has been increasing with up to 96.9% of hospitals employing a certified EHR. While there were many purported benefits of this technology, its application has also fostered significant unintended consequences, a term coined “e-iatrogenesis” (Buntin, Burke, Hoaglin, & Blumenthal, 2011; Chaudhry et al., 2006; Colpaert et al., 2006; Weiner, Kfuri, Chan, & Fowles, 2007). The intensive care unit (ICU) is especially susceptible to these unintended consequences as complex medical decision requires proficient navigation of the EHR to synthesise over 1,300 data points/patient/day (Manor-Shulman, Beyene, Frndova, & Parshuram, 2008). Successful use of an EHR is dependent upon its providers being able to efficiently find and integrate this large volume data for effective decision-making. Consequently, it is easy to envision how problems with data fragmentation and poor user interfaces can lead to significant issues with clinical cognition and pursuant errors. This was confirmed in our prior study, where residents and ICU fellows only recognised 40% of relevant patient safety issues in an EHR-based ICU simulation exercise (Stephenson, Gorsuch, Hersh, Mohan, & Gold, 2014). As cognitive factors are associated with up to 74% of diagnostic errors, the improvement of clinical cognition associated with the efficient extraction and synthesis of immense data from the EHR are critical in optimal patient care (Graber, Franklin, & Gordon, 2005; Roberson et al., 2014).
While the patient record is essential for providing patient care, it can also impede on effective interprofessional collaboration (Lingard et al., 2007). Others have acknowledged that the current EHR may not support the flow of information that is needed by the interprofessional team for patient-centred decision-making (Elias, Barginere, Berry, & Selleck, 2015). Attempts at improving EHR utilisation is complicated by the fact that the same software is used by multiple professions with differing workflows. This is especially apparent in the ICU where care teams are comprised of physicians, nurses, pharmacists, respiratory therapists, nutritionists, and social workers, all of whom use the EHR dissimilarly to input, gather, analyse, and communicate data. In spite of different workflows in employing the EHR, data are shared from all team members during daily Interprofessional (interprofessional) rounds (Collins, Bakken, Vawdrey, Coiera, & Currie, 2011a). However, a safe and conscientious care plan can only be generated if the data presented by all members of the interprofessional rounding team are reliable and accurate (Kim, Barnato, Angus, Fleisher, & Kahn, 2010). Consequently, it is imperative that any interventions to improve or modify EHR function accounts for all representative professional groups. This improvement begins with the observation and understanding of how the EHR is employed by the different professional groups.
Simulation-based training is a powerful tool that can be used to assess EHR usability and recognition of safety issues in critically ill patients without affording unnecessary risk whilst improving diagnostic accuracy (Ben-Assuli, Sagi, Leshno, Ironi, & Ziv, 2015; March et al., 2013; Weller, Nestel, Marshall, Brooks, & Conn, 2012). With reforms in medical education, there has been increasing emphasis on simulation training as it has been shown to increase knowledge and skills in invasive procedures as well as communication in a realistic environment (Wayne, Barsuk, O’Leary, Fudala, & McGaghie, 2008; Wayne, Didwania et al., 2008; Zendejas, Brydges, Wang, & Cook, 2013). Prior studies in EHR simulation have suggested EHR simulation promotes quality patient care as well as improvement in the identification of patient safety issues in critically ill patients (Landman et al., 2014; Milano, Hardman, Plesiu, Rdesinski, & Biagioli, 2014; Stephenson et al., 2014).
Specifically, our group has employed high-fidelity EHR-based simulation to understand physician clinical decision-making and recognition of patient safety issues in critically ill patients (March et al., 2013). To accomplish this, we created a clone of our institution’s EHR environment (EpicCare, Epic Systems, Inc., Madison, WI, USA) which contained full functionality and all user-specific customisations. Our institution has been using EpicCare for over 7 years. The EHR was populated with a high-fidelity medical ICU (MICU) case which included 5 days of clinical data including vital signs, intake/output reports, laboratory results, full medication administration report (MAR), all relevant nursing documentation, and progress notes from all relevant professional groups. One of our previously validated cases which we employed in this study is a 74-year-old woman who is admitted with septic shock, acute renal failure, and acute respiratory distress syndrome. A total of 14 safety issues were built into the case and were categorised into 3 groups: (1) dangerous trends in the patient’s condition, (2) medication errors, and (3) failure to adhere to critical care best practices (March et al., 2013; Stephenson et al., 2014). The goal of this study was to utilise a high-fidelity EHR-based simulation to understand the workflow of the different members of the interprofessional ICU rounding team and the ability of team members from each professional group to recognise safety issues in a critically ill patient.
Methods
Study design
The study employed a quasi-experimental cross-sectional design to examine interprofessional ICU rounding issues related to whether clinical staff could recognise safety issues associated with critically ill patients.
Intervention
Housestaff (interns, residents, and fellows) rotating through the MICU as well as MICU nurses and pharmacists were eligible for enrolment. All simulations were held in our institution’s MICU, which is a closed ICU. To simulate each of the professional group’s workflows, physicians were provided a written sign-out, then given 10 minutes to review the EHR as if assuming care for the patient in preparation for daily rounds. Participants were not instructed to look for safety issues in the EHR. Simulating the pharmacist’s workflow, a member of the study team read a scripted oral presentation which included subjective and objective data. During this oral presentation, the pharmacist had an opportunity to review the EHR. In mirroring the nurse’s workflow, nurses were given a written sign-out with typical information that would be passed along verbally during shift change. Nurses were then allotted 10 minutes to review the EHR. At the end of each participant’s review of the EHR, the patient was presented to a member of the study team.
Data collection
Each participant was scored on the number of safety issues identified during their presentation and was also provided an immediate debriefing of the safety issues at the conclusion of their respective report. Screen capture of the subjects’ navigation were accurately recorded in real time with Tobii Studio (Tobii Systems, Danderyd Municipality, Sweden) as previously described (Gold, Stephenson, Gorsuch, Parthasarathy, & Mohan, in press) to facilitate comprehension of EHR usability by the individual professional groups.
Data analysis
All analyses were performed using Graph Pad Prism (GraphPad, La Jolla, CA, USA) and a p-value of <0.05 was considered statistically significant. Differences between multiple groups were analysed using Kruskal-Wallis test. Correlations were analysed via Spearman’s test.
Ethical considerations
This study was approved by the Oregon Health and Science University Institutional Review Board. This project received assistance from the National Center for Interprofessional Practice and Education at the University of Minnesota, Twin Cities campus.
Results
We enrolled 25 physicians, 29 nurses, and 20 pharmacists. Of the physicians, there were 10 interns, 11 residents, and 4 fellows. Of the 14 safety issues created in the case, the average recognition of these issues was 32.2% (4.5/14). On average 39.7% (5.6/14) of safety issues were identified by the physicians, 29.8% (4.2/14) by nurses, and 26.4% (3.7/14) by pharmacists (p = 0.0006). Regarding imminent safety issues, the clinical diagnosis of recurrent sepsis was only recognised by 20% (15/74) of participants, while worsening trends in hemodynamics were recognised by 38% (28/74) of participants.
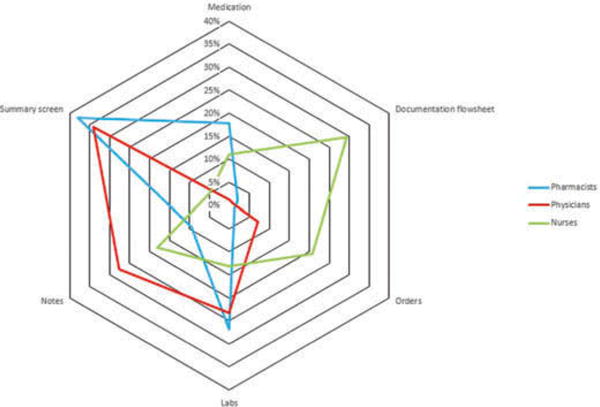
There were significant differences in the individual safety issues recognised by the professional groups (Figure 1). Overall, physicians were more likely to report issues related to clinical changes to the patient’s condition such as recurrent fever, hypotension, tachycardia, and identification of recurrent sepsis. In contrast, pharmacists were more likely to report issues related to medications and nurses were more likely to report issues related to ICU best practices (Vincent, 2005). None of the safety issues were recognised 100% of the time by any individual professional group (Figure 1).
Figure 1.
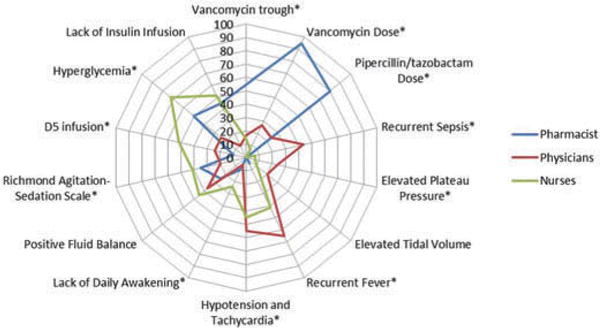
Differences in recognition of the safety issues by each professional group. Twenty-five physicians (red), 20 pharmacists (blue), and 29 nurses (green) underwent electronic health record simulation. Each item in the case is represented by a “spoke” in the plot and the recognition rate represented by the concentric rings. *Highest recognition by a professional group compared with remaining two groups combined was significant (p = 0.039).
Electronic health record utilisation
While there was no difference in the number of total and unique individual screens utilised by the three professional groups (Figure 2), there were significant differences in the relationship between screen use and performance between the groups. For physicians, performance on the simulation correlated with the number of unique screens visited (p = 0.01), while for pharmacists, performance correlated inversely with the ratio of unique to total screens visited (p = 0.006) (Figure 3), suggesting toggling between a low number of unique screens improves scores. Interestingly, for nurses there was no association between screen utilisation and performance (not shown).
Figure 2.
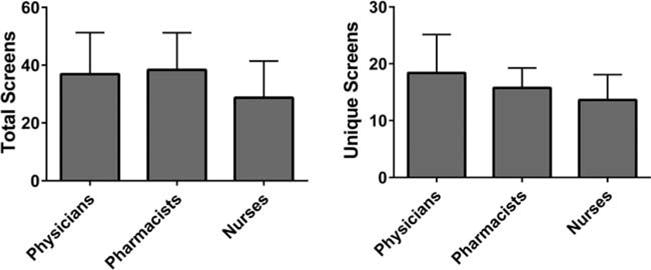
Total and unique screen utilisation by professional teams. Twenty-five physicians, 20 pharmacists, and 29 nurses underwent electronic health record simulation and total number of screens (left panel) and number of unique screens (right panel) was measured. There were no statistically significant differences between the three groups in either total or unique screens visited (p > 0.05).
Figure 3.
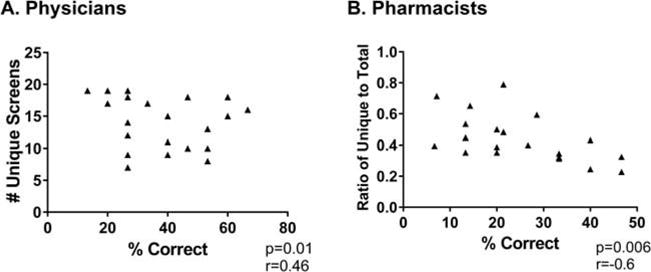
Relationship between screen use and performance. Recognition of safety issues correlated with the number of unique screens visited for physicians (r = 0.46, left panel). Recognition of safety issues correlated with unique/total screens visited for pharmacists (r = −0.6, right panel). There was no association between screen utilisation and performance (not shown).
We next examined whether there were differences in the type of screens utilised by the professional groups. A total of 152 unique screens were utilised by the cohort as a whole. Twenty-three screens were used by all 3 professional groups, 101 screens were used exclusively by 1 professional group, and only 1 screen was utilised by all participants. When we looked at the 10 most frequently used screens by each group, only 3 were used by all 3 groups (Figure 4); these screens included the results review, review of progress notes, and the input/output screen. The majority of screens employed by each group were used at an extremely low frequency by the other professional groups.
Figure 4.
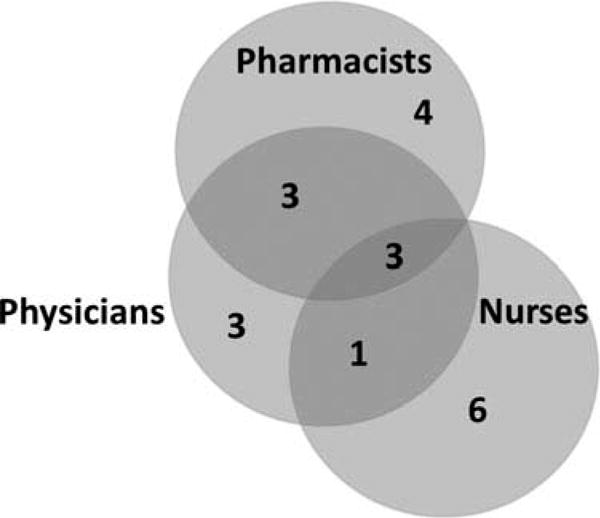
Similarities and differences in the top 10 unique screens visited by each professional group. Total 152 unique screens were visited by the cohort. Only 3 of the top 10 screens were used by all 3 professional groups.
We next classified each of the 152 unique screens used by our participants into 10 macro-categories based on content type (Appendix). When all participants were combined, 95% of the time reviewing the EHR was spent in six categories (Figure 5): medication review (8%), orders review (11%), data entry (12%), lab results (20%), review of notes (20%), and summary screens (24%). Review of screens for input/output, vital signs, non-laboratory test results, and use of non-EHR software accounted for less than 5% of the total time.
Figure 5.
Differences in time spent on screen types. The 152 unique screens visited by the cohort of physicians (red), pharmacist (blue), and nurses (green) were classified into 10 macro-categories. Six of the 10 macro-categories account for 95% of the time used in the simulation and are represented by a “spoke.” Non-lab tests, non-electronic health record programmes, input/output, and vitals screens account for less than 5% of time and are not included in the figure.
Pattern of EHR use varied significantly between the professional groups with three distinct patterns emerging, clustered around each professional group (Figure 6). Total 85% of pharmacists began their review on a medication screen and ultimately spent 38% of their time on summary screens and 27% of time reviewing laboratory data. Similarly, physicians spent a lot of time on summary screens (34%) and reviewing laboratory data (23%), but also spent substantial time reviewing notes (28%). All nurses began their review of the EHR by reviewing orders. They spend a large percentage of time reviewing and toggling to and from data entry screens (29%) compared with physicians and pharmacists who spend less than 2% of their time on these screens. Since data entry was not a part of our simulation, it can be inferred that nurses were utilising the data entry screens for data extraction, while physicians and pharmacists preferred visiting other screens for data gathering.
Figure 6.
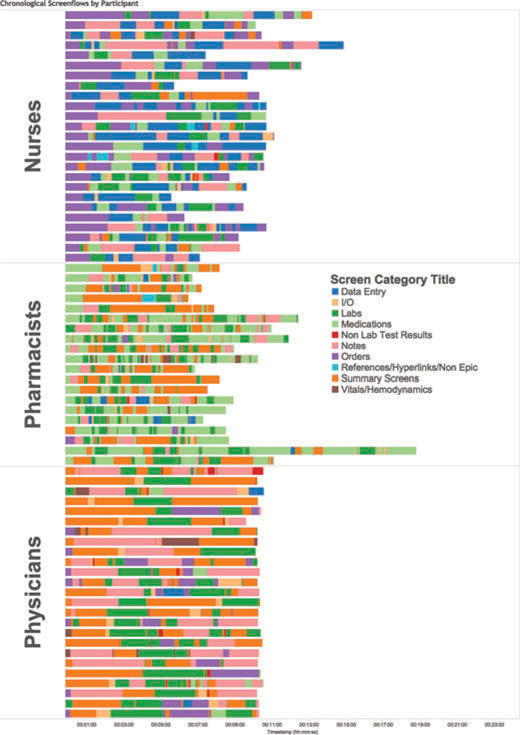
Pattern of screen use classified by macro-categories. Each row represents a participant and each colour represents one of 10 screen macro-categories. The width of a bar represents the time spent on a screen category. Pattern of electronic health record use varies between and within professions.
Discussion
A high-fidelity EHR-based simulation experience was created to assess the use of EHR by the different members of our MICU interprofessional team. This study highlights how poor physicians, nurses, and pharmacists are at identifying dangerous trends and safety issues in the EHR, confirming our prior work with physicians (Stephenson et al., 2014). When safety issues are recognised, professional groups tend to identify these safety issues in certain predictable domains. These professional differences may be ascribed to substantial differences in workflows, expectations of narrowly defined clinical rounding roles, EHR screen design, and EHR utilisation (Makowsky et al., 2009). However, while differences in workflow may explain the marked interprofessional differences in recognition of safety issues, they do not explain the persistent intraprofessional variation in recognition of safety issues. Examples include only 80% recognition of under dosing of vancomycin by pharmacists, less than 50% recognition of recurrent sepsis by physicians and less than 50% recognition of a D5 (5% dextrose) infusion in a patient with hyperglycaemia and hypervolemia by nurses. This variation of both intra-and interprofessional recognition implies an average interprofessional team from our cohort could miss as much as 50% of safety issues supporting the persistence of patient safety issues during the theoretical safety net of interprofessional rounds (Arora, Patel, Engell, & LaRosa, 2013; Kim et al., 2010; Reason, 2000). Further, while it is likely that the worsening hemodynamics might have been caught by the average interprofessional rounding team, this study suggests that the imminent diagnosis of recurrent sepsis would be under-recognised, thus compromising the creation of an appropriate care plan for this patient.
The incorporation of screen tracking provided some insight into the aetiology of the professional differences in recognition of safety issues. Both pharmacists and physicians spend the majority of their time utilising EHR screens designed for data review (as opposed to data entry). The categories of safety issues recognised by these two professions correlates with the type of information viewed on the screens visited. Further, there was a direct correlation for physicians between unique screens visited and performance, and an indirect correlation between unique/total screens visited for pharmacists. This supports our prior studies and suggests, at least within our EHR, effective use is not necessarily equated with improved efficiency per se. Rather, due to usability and probable fragmentation issues with the EHR (evidenced by the number of screens used), the ability to rapidly scan and process information is associated with expert use (Gold et al., in press).
In contrast, the lack of association in frequency of screens visited with performance for nurses was surprising. One potential explanation for this is the perceived notion that the EHR may be viewed by our nurses as a tool for data entry as opposed to data extraction. This is supported by the high frequency of use of data entry screens by nurses when compared with other groups. Another potential explanation is that nurses do not trust the information in the EHR. Indeed a prior study suggested that nurses preferentially depend on either bedside information or verbal communication (Collins, Bakken, Vawdrey, Coiera, & Currie, 2011b; Gregory, Tan, Tilrico, Edwardson, & Gamm, 2014). This is also supported by another study that demonstrated nursing students are more likely to report incorrect vital signs that were conveyed to them at the bedside by medical students. This was in part due to the belief that the information in the EHR may be incomplete and therefore potentially unreliable for decision-making (Collins et al., 2011b; Kaba & Beran, 2016). Additional qualitative studies will be required to better elucidate which, if any, of these factors are responsible. Finally, the significant differences in EHR use patterns between nurses and the other professional groups highlight the fact that objective/quantitative measures of EHR usability will need to be created and validated for each professional group individually.
Our results highlight the markedly different patterns in EHR navigation between and within professional groups. There was little overlap in screen use between the professional groups, with a large number of screens utilised by only one of the professional groups. This is not unexpected given the role each professional group often has in customising interfaces to facilitate their own professional workflow, usually in isolation from the development processes of the other professional groups. However, even when we re-categorised screens based on general functionality, significant variations between the professional groups persisted. This confirms the results from prior surveys and a recent study highlighting differences between physician and nursing EHR navigation during creation of discharge summaries (Helleso & Sogstad, 2014; Penoyer et al., 2014). While intended to improve the performance of each group, it is likely the siloed approach to customisation has resulted in a slow evolutionary divergence in EHR usability between the groups. These results argue for a unit-specific, patient-centric interprofessional approach to EHR customisation to minimise any potential gaps in data visualisation between groups. Optimally, use of a high-fidelity simulation exercise with context-specific cases, such as the one created for this study, will allow for a more complete evaluation of these customisations prior to deployment.
It is important to acknowledge the limitations of this study. First, this study was a single-centre study done with one EHR in a critical care setting and thus it is not clear if our results can be generalised to other EHR systems or other clinical settings. Second, while we attempted to reproduce the daily workflow of the different professions, the simulations were done in isolation after a full complement of morning rounds and participants were not asked to present their data to a full interprofessional team. It is possible that the presence of shared decision-making by all members of the interprofessional team would increase recognition of safety issues by the team as a whole. We anticipate this data to form the basis for full interprofessional rounding simulations and will be the subject of subsequent studies. Third, we only incorporated three professional groups. Indeed, the lowest recognition rate in our study was related to ventilators; this argues for the importance of having a respiratory therapist during interprofessional rounds, which has previously been shown to improve communication of ventilator data, increase in ventilator-free days, and an accurate assessment of the patient’s changing respiratory status (Cohen et al., 1991; King, Conrad, & Ahmed, 2013). Fourth, given the limitations of a simulation and the lack of an actual patient, workflows could not be perfectly replicated. As an initiative for best practice, nurses give verbal report at the bedside during their sign-out which may promote identification of patient safety issues. Physicians may also anticipate gathering additional ventilator data as well as assessing sedation and daily awakenings at the patient’s bedside, thus not routinely using the EHR for this type of data collection. While this may be true, it does not take away from the fact that we are still poor at recognising safety issues in the EHR. In addition, since physicians were not asked to generate a progress note, they may have avoided cognitive processing that occurs with this task (Weir et al., 2003). Lastly, all participants were aware this was a simulation and thus a significant Hawthorne effect could exist and overestimate our results.
Concluding comments
Through the use of a high-fidelity simulation of a critically ill patient, we have demonstrated that the different members of the interprofessional team are relatively poor at identifying safety issues in our institution’s EHR. There were significant silos in which an interprofessional team’s expertise and workflow may have increased recognition of safety issues in certain domains. Our study captures the disparate ways the EHR is used to serve the purposes of the different professions. We are continuing our study on EHR usability and recognition of safety issues with full rounding simulations to see if teamwork and shared decision-making facilitate improvement in recognition of safety issues.
Acknowledgments
Funding
This project was funded by a grant from the Agency for Healthcare Research and Quality (RO1HS023793, R18HS021637) and the Donaghue Foundation.
Appendix
Description of screen categories and examples of each
| Screen category | Description |
|---|---|
| Data entry | Screens which are only used for data entry |
| For example, Doc Flowsheets | |
| I/O | Screens which only display input (e.g. fluids, medication volume, feeds, etc.) and output (e.g. urine, stool, drain, vomit, etc.) data |
| For example, Input/Output screen | |
| Labs | Screens which only display laboratory data |
| For example, Results Review | |
| Medications | Screens which only display medications with or without administration times |
| For example, Medication Administration Record (MAR) or Medications | |
| Non-lab test results | Screens which display non-laboratory results |
| For example, reviewing echocardiogram results or chest X-ray results | |
| Notes | Screens which display any of the interprofessional notes |
| For example, reviewing daily progress notes | |
| Orders | Screens which display active, completed, or discontinued orders |
| For example, Orders Manager | |
| References/hyperlink/non-epic | Use of non-EHR software |
| For example, use of a web browser to visit online.lexi.com | |
| Summary screens | Screens which contain data elements from various domains (e.g. vitals, labs, medications) |
| For example, ICU Accordion | |
| Vitals/hemodynamics | Screens which only display vital signs and hemodynamics |
| For example, Vital Signs |
Footnotes
Colour versions of one or more of the figures in the article can be found online at www.tandfonline.com/ijic.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- Arora N, Patel K, Engell CA, LaRosa JA. The effect of interdisciplinary team rounds on urinary catheter and central venous catheter days and rates of infection. American Journal of Medical Quality. 2013;29:329–334. doi: 10.1177/1062860613500519. [DOI] [PubMed] [Google Scholar]
- Ben-Assuli O, Sagi D, Leshno M, Ironi A, Ziv A. Improving diagnostic accuracy using EHR in emergency departments: A simulation-based study. Journal of Biomedical Informatics. 2015;55:31–40. doi: 10.1016/j.jbi.2015.03.004. [DOI] [PubMed] [Google Scholar]
- Buntin MB, Burke MF, Hoaglin MC, Blumenthal D. The benefits of health information technology: A review of the recent literature shows predominantly positive results. Health Affairs. 2011;30:464–471. doi: 10.1377/hlthaff.2011.0178. [DOI] [PubMed] [Google Scholar]
- Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, Shekelle PG. Systematic review: Impact of health information technology on quality, efficiency, and costs of medical care. Annals of Internal Medicine. 2006;144:742–752. doi: 10.7326/0003-4819-144-10-200605160-00125. doi: 0000605-200605160-00125. [DOI] [PubMed] [Google Scholar]
- Cohen IL, Bari N, Strosberg MA, Weinberg PF, Wacksman RM, Millstein BH, Fein IA. Reduction of duration and cost of mechanical ventilation in an intensive care unit by use of a ventilatory management team. Critical Care Medicine. 1991;19:1278–1284. doi: 10.1097/00003246-199110000-00010. [DOI] [PubMed] [Google Scholar]
- Collins SA, Bakken S, Vawdrey DK, Coiera E, Currie L. Model development for EHR interdisciplinary information exchange of ICU common goals. International Journal of Medical Informatics. 2011a;80:e141–e149. doi: 10.1016/j.ijmedinf.2010.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins SA, Bakken S, Vawdrey DK, Coiera E, Currie L. Clinician preferences for verbal communication compared to EHR documentation in the ICU. Applied Clinical Informatics. 2011b;2:190–201. doi: 10.4338/ACI-2011-02-RA-0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colpaert K, Claus B, Somers A, Vandewoude K, Robays H, Decruyenaere J. Impact of computerized physician order entry on medication prescription errors in the intensive care unit: A controlled cross-sectional trial. Critical Care. 2006;10:R21. doi: 10.1186/cc3983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elias B, Barginere M, Berry PA, Selleck CS. Implementation of an electronic health records system within an interprofessional model of care. Journal of Interprofessional Care. 2015;29:551–554. doi: 10.3109/13561820.2015.1021001. [DOI] [PubMed] [Google Scholar]
- Gold JA, Stephenson LE, Gorsuch A, Parthasarathy K, Mohan V. Feasibility of utilizing a commercial eye tracker to assess electronic health record use during patient simulation. Health Informatics Journal. doi: 10.1177/1460458215590250. in press. [DOI] [PubMed] [Google Scholar]
- Graber ML, Franklin N, Gordon R. Diagnostic error in internal medicine. Archives of Internal Medicine. 2005;165:1493–1499. doi: 10.1001/archinte.165.13.1493. [DOI] [PubMed] [Google Scholar]
- Gregory S, Tan D, Tilrico M, Edwardson N, Gamm L. Bedside shift reports: What does the evidence say? Journal of Nursing Administration. 2014;44:541–545. doi: 10.1097/NNA.0000000000000115. [DOI] [PubMed] [Google Scholar]
- Helleso R, Sogstad MK. Hospital nurses’ and physicians’ use of information sources during their production of discharge summaries: A cross-sectional study. Studies in Health Technology and Informatics. 2014;201:335–341. [PubMed] [Google Scholar]
- Kaba A, Beran TN. Impact of peer pressure on accuracy of reporting vital signs: An interprofessional comparison between nursing and medical students. Journal of Interprofessional Care. 2016;30:116–122. doi: 10.3109/13561820.2015.1075967. [DOI] [PubMed] [Google Scholar]
- Kim MM, Barnato AE, Angus DC, Fleisher LA, Kahn JM. The effect of multidisciplinary care teams on intensive care unit mortality. Archives of Internal Medicine. 2010;170:369–376. doi: 10.1001/archinternmed.2009.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King AE, Conrad M, Ahmed RA. Improving collaboration among medical, nursing and respiratory therapy students through interprofessional simulation. Journal of Interprofessional Care. 2013;27:269–271. doi: 10.3109/13561820.2012.730076. [DOI] [PubMed] [Google Scholar]
- Landman AB, Redden L, Neri P, Poole S, Horsky J, Raja AS, Poon EG. Using a medical simulation center as an electronic health record usability laboratory. Journal of the American Medical Informatics Association. 2014;21:558–563. doi: 10.1136/amiajnl-2013-002233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lingard L, Conn LG, Russell A, Reeves S, Miller KL, Kenaszchuk C, Zwarenstein M. Interprofessional information work: Innovations in the use of the chart on internal medicine teams. Journal of Interprofessional Care. 2007;21:657–667. doi: 10.1080/13561820701731817. [DOI] [PubMed] [Google Scholar]
- Makowsky MJ, Schindel TJ, Rosenthal M, Campbell K, Tsuyuki RT, Madill HM. Collaboration between pharmacists, physicians and nurse practitioners: A qualitative investigation of working relationships in the inpatient medical setting. Journal of Interprofessional Care. 2009;23:169–184. doi: 10.1080/13561820802602552. [DOI] [PubMed] [Google Scholar]
- Manor-Shulman O, Beyene J, Frndova H, Parshuram CS. Quantifying the volume of documented clinical information in critical illness. Journal of Critical Care. 2008;23:245–250. doi: 10.1016/j.jcrc.2007.06.003. [DOI] [PubMed] [Google Scholar]
- March CA, Steiger D, Scholl G, Mohan V, Hersh WR, Gold JA. Use of simulation to assess electronic health record safety in the intensive care unit: A pilot study. BMJ Open. 2013;3(4):e002549–e002549. doi: 10.1136/bmjopen-2013-002549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milano CE, Hardman JA, Plesiu A, Rdesinski RE, Biagioli FE. Simulated electronic health record (Sim-EHR) curriculum: Teaching EHR skills and use of the EHR for disease management and prevention. Academic Medicine. 2014;89:399–403. doi: 10.1097/ACM.0000000000000149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penoyer DA, Cortelyou-Ward KH, Noblin AM, Bullard T, Talbert S, Wilson J, Briscoe JG. Use of electronic health record documentation by healthcare workers in an acute care hospital system. Journal of Healthcare Management. 2014;59:130–144. [PubMed] [Google Scholar]
- Reason J. Human error: Models and management. The Western Journal of Medicine. 2000;172:393–396. doi: 10.1136/ewjm.172.6.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberson D, Connell M, Dillis S, Gauvreau K, Gore R, Heagerty E, Schwartz M. Cognitive complexity of the medical record is a risk factor for major adverse events. The Permanente Journal. 2014;18:4–8. doi: 10.7812/TPP/12-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephenson LS, Gorsuch A, Hersh WR, Mohan V, Gold JA. Participation in EHR based simulation improves recognition of patient safety issues. BMC Medical Education. 2014;14:224. doi: 10.1186/1472-6920-14-224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vincent JL. Give your patient a fast hug (at least) once a day. Critical Care Medicine. 2005;33:1225–1229. doi: 10.1097/01.ccm.0000165962.16682.46. doi:00003246-200506000-00005[pii] [DOI] [PubMed] [Google Scholar]
- Wayne DB, Barsuk JH, O’Leary KJ, Fudala MJ, McGaghie WC. Mastery learning of thoracentesis skills by internal medicine residents using simulation technology and deliberate practice. Journal of Hospital Medicine. 2008;3:48–54. doi: 10.1002/jhm.268. [DOI] [PubMed] [Google Scholar]
- Wayne DB, Didwania A, Feinglass J, Fudala MJ, Barsuk JH, McGaghie WC. Simulation-based education improves quality of care during cardiac arrest team responses at an academic teaching hospital: A case-control study. Chest. 2008;133:56–61. doi: 10.1378/chest.07-0131. [DOI] [PubMed] [Google Scholar]
- Weiner JP, Kfuri T, Chan K, Fowles JB. “e-Iatrogenesis”: The most critical unintended consequence of CPOE and other HIT. Journal of the American Medical Informatics Association: JAMIA. 2007;14:387–388. doi: 10.1197/jamia.M2338. discussion 389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weir CR, Hurdle JF, Felgar MA, Hoffman JM, Roth B, Nebeker JR. Direct text entry in electronic progress notes. An evaluation of input errors. Methods of Information in Medicine. 2003;42:61–67. doi: 10.1267/METH03010061. [DOI] [PubMed] [Google Scholar]
- Weller JM, Nestel D, Marshall SD, Brooks PM, Conn JJ. Simulation in clinical teaching and learning. The Medical Journal of Australia. 2012;196:594. doi: 10.5694/mja10.11474. [DOI] [PubMed] [Google Scholar]
- Zendejas B, Brydges R, Wang AT, Cook DA. Patient outcomes in simulation-based medical education: A systematic review. Journal of General Internal Medicine. 2013;28:1078–1089. doi: 10.1007/s11606-012-2264-5. [DOI] [PMC free article] [PubMed] [Google Scholar]


