Abstract
Objective
We assessed whether an automated Prescription Drug Monitoring Program (PDMP) intervention in emergency department (ED) settings was associated with reductions in opioid prescribing and quantities.
Methods
We performed a retrospective cohort study of ED visits by Medicaid beneficiaries. We assessed the staggered implementation (pre-post) of automated PDMP queries at 86 EDs in Washington State, Jan 1, 2013 to Sep 30, 2015. The outcomes included any opioid prescribed within 1 day of the index ED visit and total dispensed morphine milligram equivalents (MMEs). The exposure was the automated PDMP query intervention. We assessed effects of automated PDMP stratified by prior high-risk opioid use. We performed multiple sensitivity analyses, including restriction to pain related visits, restriction to visits with a confirmed PDMP query, and assessment of six specific opioid high risk indicators.
Results
The study included 1,187,237 qualifying ED visits (898,162 pre-intervention; 289,075 post-intervention). Compared to the pre-intervention period, automated PDMP queries were not significantly associated with reductions in the proportion of visits with opioid prescribing (5.8 per 1000 encounters, 95%CI: −0.11, 11.8) or the amount of prescribed MMEs (difference 2.66, 95%CI: −0.15, 5.48). There was no evidence of selective reduction in patients with prior high risk opioid use (1.2 per 1000 encounters, 95%CI: −9.5, 12.0; MMEs: 1.22, 95%CI: −3.39, 5.82). The lack of a selective reduction in high risk patients was robust to all sensitivity analyses.
Conclusions
An automated PDMP query intervention was not associated with reductions in ED opioid prescribing or quantities, even in patients with prior high-risk opioid use.
Introduction
Background
Drug overdoses have overtaken motor vehicle collisions as the leading cause of accidental mortality, and this epidemic has been fueled by prescription opioid abuse.1 Overdose deaths involving prescription opioids have quadrupled since 1999. From 1999 to 2015, more than 183,000 people have died in the U.S. from overdoses related to prescription opioids.2
EDs are a frequent source for prescriptions for controlled substances3 and represent particularly high risk settings for doctor shopping and drug diversion.4–7 Individuals predisposed towards the misuse or diversion of opioids may frequently seek prescriptions from EDs.7,8 Contributing factors include the episodic nature of emergency care, lack of a long-term physician-patient relationship, and until recently, the absence of integrated data systems about prior controlled substance use.
Prescription drug monitoring programs (PDMPs) represent one approach to addressing the prescription opioid epidemic. All but one state have adopted these electronic registries, which track dispensed controlled substances to unique patients.9 Information in the PDMP may help providers identify high-risk patients, such as those with high dosages of prescribed opioids, multiple prescribers and/or dispensers, and overlapping prescriptions for opioids or other controlled substances.
Importance
Information from PDMPs may result in more selective opioid prescribing.10,11 However, there are multiple logistical barriers to PDMP use by providers, including web pages that are difficult to navigate, frequent requirements for password updates, and time needed to access clinically useful information.12,13 As a result, there has been limited provider use of PDMPs in the absence of mandates.14–16
At least ten states require that health care providers perform a PDMP query prior to opioid prescribing.17 Recent evaluations suggest that the requirement for mandatory PDMP use is associated with reduced opioid prescribing to high-risk patients and less “shopping” behavior (multiple prescribers and/or pharmacies for controlled substances).17,18 Such mandates are controversial, as they impose significant logistical burdens on prescribers without addressing usability barriers. In addition, the perception of a coercive requirement may erode provider support for PDMP programs.19 Finally, such mandates could potentially encourage under-treatment of pain. Conversely, best available data suggest that voluntary PDMP use has limited impact on opioid prescribing behavior.17
One potential solution is the automation of PDMP queries that “push” clinically relevant data to providers at the time of a patient encounter.12 This approach is non-coercive and eliminates many of the logistical barriers related to PDMP use. Automated PDMP queries may be particularly appealing in ED settings, which are characterized by competing clinical demands and intense pressure to maximize patient throughput. Starting in November of 2014, Washington state hospital EDs began implementing an automated PDMP query on a staggered basis (eFigure 1). This natural policy experiment mitigates potential confounding by indication (i.e. providers selectively performing queries on patients at higher risk of opioid overdose or abuse) that may occur in the absence of automated queries. Understanding the impact of automated PDMP queries is particularly important for Medicaid beneficiaries, who have a six-fold higher risk of fatal prescription opioid overdose compared to non-Medicaid populations.20
Goal of This Investigation
Using data from a large cohort of Medicaid beneficiaries, we assessed whether an automated PDMP intervention in ED settings was associated with reductions in opioid prescribing and quantities. We were specifically interested in the impact of the intervention on patients with a prior history of high-risk controlled substance use.
Methods
Description of the Policy Intervention
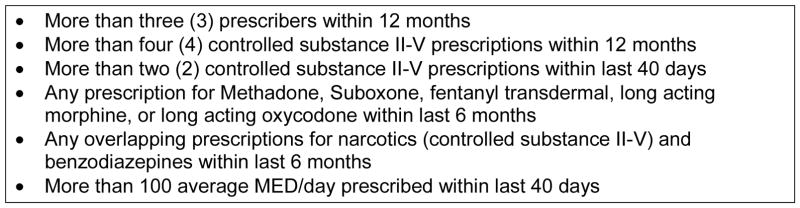
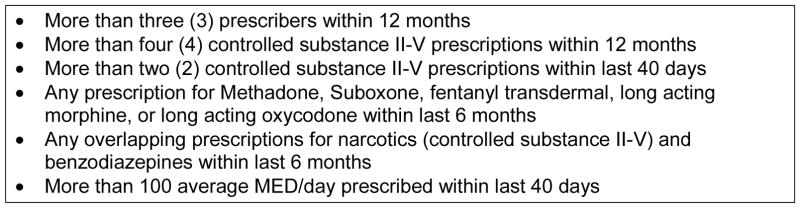
The Washington state PDMP became operational in October 2011. Beginning in November 2014, Washington state began implementation of an automated PDMP query into a pre-existing, statewide, Emergency Department Information Exchange (EDIE). EDIE is an electronic database that tracks information for unique patients and generates alerts for ED providers, including reports about care guidelines, security events, and ED visit history. An EDIE query occurs nearly instantaneously at the time of patient registration at all non-federal EDs in Washington state. The new initiative integrates an automated PDMP query using patient last name, first name, and date of birth as mandatory fields. If any of six high risk criteria established by the Washington state Department of Health are met when the PDMP is queried (Figure 1), then a complete PDMP report is generated and incorporated into the EDIE report. ED providers can access this EDIE-automated PDMP query information by clicking on an icon in their local electronic medical record systems. If the ED did not have an electronic medical record system, then a paper report was faxed to the ED. There is no requirement for providers to enter PDMP credentials to view query data. Providers may still perform a manual PDMP query, although there is no requirement to do so.
Figure 1.
Washington State Controlled Substance High Risk Criteria
Study Design
We performed a retrospective cohort study of ED visits by Washington state Medicaid beneficiaries, from January 1, 2013 to September 30, 2015. The end of the study time frame was selected as the last day prior to nationwide transition from the ICD-9 to the ICD-10 system, to avoid confounding due to coding artifacts (e.g. for ED diagnoses and pre-existing co-morbidity codes).
Although all non-federal hospitals in Washington state agreed to participate in the automated PDMP initiative, implementation dates varied by hospital and were dependent on the completion of site-specific agreements with the state. We exploited the staggered implementation of automated PDMP queries while controlling for hospital specific effects and temporal trends on opioid prescribing. This approach allowed us to model variation from within-hospital changes over time and cross-hospital differences at a point in time. Of 86 eligible hospitals in Washington state, 65 completed implementation during the study period (eFigure 1).
The Washington State Health Care Authority provided enrollment information and medical claims for Medicaid beneficiaries, as well as PDMP dispense data linked at the beneficiary level. All pharmacies are required to report dispensing of controlled substances to the PDMP, regardless of payment source (including non-Medicaid co-insurers or cash). The Washington State Department of Health also provided data on provider queries of the PDMP system (queries are captured for patients with any prior PDMP record of a dispensed controlled substance). The Institutional Review Boards of Washington State and of Oregon Health & Science University approved this study.
Cohort Selection
We included Washington State Medicaid beneficiaries who were enrolled between Jan 1, 2013 and Sep 30, 2015. We excluded members with a prior history of cancer, as opioid treatment is accepted for cancer pain.21 We excluded beneficiaries who were also enrolled for Medicare, since Medicare data were unavailable to us. Children under 15 years of age were excluded. We excluded observations for members who were enrolled less than 3 months during the prior year to have sufficient data on pre-existing co-morbidities. Finally, we excluded patients who received hospice or nursing home care at any time during the study period, since opioid analgesics are a widely accepted treatment for hospice patients21, and institutional providers are likely responsible for medication management in nursing facilities.
We analyzed visits made by eligible beneficiaries to non-federal EDs in Washington State. ED visits were identified through an algorithm from the Healthcare Effectiveness Data and Information Set (HEDIS), that uses a combination of procedure, revenue, and place of service codes typically found on emergency department claims.22 We excluded ED visits that resulted in hospital admission or observation services and visits for which a unique treating ED provider could not be identified from claims data. We also excluded ED visits that were associated with >1,400 morphine milligram equivalents of prescribed opioids (equivalent to >280 tabs of 5mg oxycodone), as these likely represented erroneous data. Finally, we excluded visits to hospitals (n=3) with fewer than 100 eligible ED visits by Medicaid beneficiaries during the time frame.
Outcomes
The primary outcome was any outpatient dispensed Schedule II or III opioid prescription prescribed within 1 day of the index ED visit. We matched prescribing date to within one day after the ED index visit to account for encounters that spanned midnight. We included buprenorphine, butorphanol, codeine, dihydrocodeine, fentanyl, hydrocodone, hydromorphone, levomethadyl, levorphanol, meperidine, methadone, morphine, opium, oxycodone, oxymorphone, pentazocine, tapentadol, and tramadol.23 We included tablets, syrups/suspensions, films, and transdermal patches, and we excluded other formulations (e.g. powders, sprays).
A secondary outcome was the total outpatient dispensed morphine milligram equivalents (MME) prescribed within 1 day of the index ED visit. We used the following conversion factors to calculate MMEs: buprenorphine patch-12.6, buprenorphine tablet- 30; butorphanol-7, codeine-0.15, dihydrocodeine-0.25, fentanyl patch- 7.2, hydrocodone-1, hydromorphone-4, levomethadyl-8, levorphanol-11, meperidine-0.1, methadone-3, morphine-1, opium-1, oxycodone-1.5, oxymorphone-3, pentazocine-0.37, tapentadol-0.4, and tramadol-0.1.24–26
Exposure
The independent variable was the presence of the automated PDMP query. This was defined as a site specific binary indicator that corresponded to the time period either before (no exposure) or after (exposure present) implementation of the automated PDMP query system.
Measures
We included an expansive set of case-mix measures from claims data, evaluated during each calendar quarter. Demographics included age, sex, race-ethnicity, disability status, enrollment in Medicaid fee-for-service vs managed care programs, and enrollment in the Affordable Care Act expansion cohort. A one-year prior history of 17 physical health condition categories was evaluated using the Chronic Illness and Disability Payment System, which has been validated for use in Medicaid populations.27 Specific mental health diagnoses were identified through medical claims using the previously described Ettner classification system.28
We created ED visit-level measures from claims data. We collected data on the hospital site of service, and identified whether the ED visit was associated with any pain related discharge diagnosis (see eTable 1).29–31
We used linked PDMP dispense data to identify prior high risk use of controlled substances, as defined by the Washington State Department of Health (Figure 1). All PDMP “lookbacks” that define high risk use were performed from the date of the index ED visit.
Analysis
The unit of analysis was an ED visit. We used a multivariable logistic regression model to assess the association of automated PDMP queries with the primary outcome of any dispensed opioid. The independent variable of interest was a site- and time- specific binary indicator for implementation of the automated PDMP intervention. We adjusted for patient demographic and health characteristics, as well as presence of pain diagnoses. We included hospital fixed effects to control for any unobserved, time-invariant hospital confounders, and a linear time variable (quarter 1–11) to control for potential temporal trends. Because opioid prescribing practices over time may vary by hospital, we included an interaction term between hospital and time to account for site-specific temporal trends. We also used 3 indicator variables for calendar quarter to adjust for seasonality. Standard errors were clustered at the hospital level.
Because >80% of ED visits did not result in opioid prescribing, we restricted the analysis of total MMEs to ED visits with an opioid prescription. To account for the highly skewed distribution of MMEs, we used a generalized linear model with log link, and Wald variance family based on results of the modified Park test. Covariates included in the model were the same as those described above for the primary outcome of any opioid prescribing, and standard errors were clustered at the hospital level.
We dropped 0.67% of observations from the analysis due to missing core demographics (age and/or gender). Observations with missing race and ethnicity were categorized as “unknown” and included in the analysis. Comorbidities, disability status, and eligibility under the Affordable Care Act were coded as presence or absence of diagnosis codes and therefore had no missing values.
For both outcomes, we also assessed for potential effect modification by prior high risk use of controlled substances. Automated PDMP queries might have a selective effect on patients with any of the six indicators of high risk opioid use (Figure 1). We included an interaction term in models between the binary indicators of high-risk status (any of the six indicators) and automated PDMP query. We further refined this analysis by restricting to the population of patients who are more likely to receive an opioid prescription – those with a pain diagnosis recorded for their visit.
Several factors may have resulted in an invalid PDMP query, such as data entry errors of name/date of birth, technical problems such as temporary unavailability of the PDMP, or initial inability to verify the patient’s identity due to medical condition or intoxication. For this reason, we performed a sensitivity analysis focused on ED visits with evidence of a successful automated PDMP query, as determined by a PDMP query matching on a Medicaid beneficiary and performed on the day of a qualifying ED visit. ED visits occurring after implementation of automated queries were restricted to those where a successful query was completed, but all ED visits by eligible patients in the pre-implementation phase remained in the analysis. We restricted the sensitivity analyses to patients with any prior record of dispensed controlled substance, as the Washington State PDMP only captures queries on such patients.
Finally, we assessed whether there were selective effects by specific high risk factors, as concern for opioid misuse may vary across the six indicators (Figure 1). We included interaction terms in models between the binary indicator of automated PDMP queries and each of the six individual high risk factors. We performed this sensitivity analysis in the primary cohort of all ED visitors, as well as in the subgroup with a prior record of dispensed controlled substance as described above.
All results are presented as marginal effects (i.e. absolute risk difference attributable to the intervention). Data management and analyses were completed using R version 3.4.1 and Stata version 14.2.
Results
We identified 1,187,237 eligible ED visits during the study period (eFigure 2). ED visit level characteristics before and after site specific implementation of the automated PDMP queries are presented in Table 1. Compared to the ED visits occurring before policy implementation, ED visits after automated PDMP queries were more often made by beneficiaries who were non-White, male, and who qualified for Medicaid benefits due to expansion through the Affordable Care Act. There were otherwise no clinically important differences by age, prior history of physical or behavioral health conditions, prior markers of high risk opioid use, or pain related diagnoses.
Table 1.
Characteristics of ED Visitors Before and After Automated PDMP Queries
| Visits occurring before EDIE Integration (N= 898,162) | Visits occurring after EDIE Integration (N= 289,075) | |
|---|---|---|
| Patient characteristics | ||
| Age (years) – mean (SD) | 33.3 (12.7) | 33.9 (12.6) |
| Female sex – N (%) | 573,820 (63.9) | 175,577 (60.7) |
| Race/ethnicity – N (%) | ||
| White | 552,821 (61.6) | 163,022 (56.4) |
| Hispanic | 116,006 (12.9) | 38,972 (13.5) |
| Black | 78,180 (8.7) | 34,503 (11.9) |
| American Indian/Alaska Native | 37,414 (4.2) | 8,696 (3.0) |
| Hawaiian/Pacific Islander | 11,159 (1.2) | 5,465 (1.9) |
| Asian | 9,370 (1.0) | 4,824 (1.7) |
| Other/unknown | 93,212 (10.4) | 33,593 (11.6) |
| Qualify for Medicaid under expansion – N(%) | 111,534 (12.4) | 65,315 (22.6) |
| Coverage type – N(%) | ||
| Managed care | 794,876 (88.5) | 268,753 (93.0) |
| Fee-for-service | 103,286 (11.5) | 20,322 (7.0) |
| History of Physical Health Conditions1 – N (%) | ||
| Cardiovascular | 242,978 (27.1) | 81,497 (28.2) |
| Pulmonary | 238,265 (26.5) | 74,017 (25.6) |
| Skeletal & connective | 233,898 (26.0) | 71,977 (24.9) |
| Gastrointestinal | 210,638 (23.5) | 65,695 (22.7) |
| Skin | 173,464 (19.3) | 57,416 (19.9) |
| Pregnancy | 151,718 (16.9) | 43,257 (15.0) |
| Nervous system | 110,424 (12.3) | 33,183 (11.5) |
| Metabolic | 89,400 (10.0) | 30,507 (10.6) |
| Diabetes | 88,797 (9.9) | 27,419 (9.5) |
| Genital | 80,322 (8.9) | 24,796 (8.6) |
| Other infectious disease | 68,548 (7.6) | 22,663 (7.8) |
| Renal | 53,093 (5.9) | 17,097 (5.9) |
| Hematological | 29,250 (3.3) | 9,665 (3.3) |
| Eye | 18,931 (2.1) | 6,136 (2.1) |
| Cerebrovascular | 10,164 (1.1) | 2,849 (1.0) |
| HIV/AIDs | 7,388 (0.8) | 2,381 (0.8) |
| Developmental disability | 5,575 (0.6) | 1,681 (0.6) |
| History of Behavioral Health Conditions2 – N (%) | ||
| Any Ettner disorder | 648,154 (72.2) | 208,683 (72.2) |
| Anxiety disorder | 302,453 (33.7) | 96,665 (33.4) |
| Dysthymia or other depression | 249,502 (27.8) | 77,596 (26.8) |
| Major depression | 128,793 (14.3) | 41,586 (14.4) |
| Alcohol disorder | 121,956 (13.6) | 40,105 (13.9) |
| Bipolar disorder | 99,208 (11.0) | 29,145 (10.1) |
| Schizophrenia or other non-mood disorder | 70,587 (7.9) | 21,547 (7.5) |
| Disorders originating in childhood | 61,700 (6.9) | 19,006 (6.6) |
| Personality disorder | 27,489 (3.1) | 7,753 (2.7) |
| Adjustment disorder | 20,170 (2.2) | 5,494 (1.9) |
| Other disorder | 287,579 (32.0) | 97,910 (33.9) |
| Patient opioid use history3 – N(%) | ||
| Any high risk criteria | 173,336 (19.3) | 57,954 (20.0) |
| >4 prescriptions for controlled substances in past 12 mo. | 141,653 (15.8) | 48,893 (16.9) |
| Any overlapping prescriptions for controlled substances & benzodiazepines in past 6 mo. | 121,927 (13.6) | 37,869 (13.1) |
| >3 prescribers in past 12 mo. | 98,552 (11.0) | 36,433 (12.6) |
| >2 prescriptions for controlled substances in past 40 days | 45,617 (5.1) | 12,832 (4.4) |
| Any methadone, suboxone, transdermal fentanyl, long-acting morphine, or long-acting oxycodone in past 6 mo. | 19,918 (2.2) | 6,101 (2.1) |
| >100 average MED/day in past 40 days | 14,540 (1.6) | 4,544 (1.6) |
| Pain-related diagnoses at visit – N (%) | ||
| Any pain diagnosis | 366,044 (40.8) | 116,737 (40.4) |
| Injury | 187,969 (20.9) | 59,230 (20.5) |
| Arthritis/joint pain | 90,066 (10.0) | 30,841 (10.7) |
| Back pain | 68,780 (7.7) | 21,155 (7.3) |
| Non-traumatic dental | 37,411 (4.2) | 10,442 (3.6) |
| Neck pain | 23,916 (2.7) | 7,733 (2.7) |
| Headache/migraine | 15,857 (1.8) | 5,938 (2.1) |
| Kidney stone | 7,716 (0.9) | 2,690 (0.9) |
| Gallstone | 5,166 (0.6) | 1,683 (0.6) |
| Other4 | 28,136 (3.1) | 8,352 (2.9) |
Indicates whether the enrollee had a 1-year history of the condition of interest at the time when the visit occurred. Health condition categories were constructed using the Chronic Illness and Disability Payment System (CDPS).
Indicates whether the enrollee had a 1-year history of the condition of interest at the time when the visit occurred. Condition categories were constructed using Ettner classifications.
Controlled substances in this section include substances on schedules II–V
Including sickle cell with crisis, acute pancreatitis, pathological fracture, acute pain not otherwise specified, and pain related to HIV/AIDS
Table 2 displays the unadjusted percentage of ED visits that resulted in any opioid prescribing and the unadjusted average MME dispensed, before (17.5%, MME [median, IQR]: 75, 60–112.5) and after (18.2%, MME [median, IQR]: 75, 60–112.5) automated PDMP query implementation. Short acting hydrocodone and oxycodone were the two most commonly prescribed prescription opioids, both before and after the intervention (eTable 2). Unadjusted proportion of opioid prescribing and MME dispensed as a function of time are illustrated in eFigure 3.
Table 2.
Unadjusted Proportion of Opioid Prescribing, Before and After Implementation of Automated PDMP Queries
| Any opioid prescription N (%) |
Total dispensed MMEs* mean (SD) median [IQR] |
|||
|---|---|---|---|---|
|
| ||||
| Before | After | Before | After | |
|
|
||||
| Overall (N= 1,187,237 visits) | 157,004 (17.5) | 52,667 (18.2) | 111.7 (120.4) 75.0 [60.0 – 112.5] |
110.0 (115.5) 75.0 [60.0 – 112.5] |
| Not high-risk patient (N= 955,947 visits) | 102,739 (11.4) | 34,689 (12.0) | 97.5 (80.0) 75.0 [60.0 – 112.5] |
96.9 (75.1) 75.0 [60.0 – 100.0] |
| High-risk patient(N = 231,290 visits) | 54,265 (6.0) | 17,978 (6.2) | 138.5 (169.5) 90.0 [60.0 – 150.0] |
135.3 (165.0) 90.0 [60.0 – 150.0] |
| Pain diagnosis; Not high-risk patient (N = 370,704 visits) | 63,154 (17.3) | 21,511 (18.4) | 99.3 (79.3) 75.0 [60.0 – 112.5] |
98.9 (75.7) 75.0 [60.0 – 112.5] |
| Pain diagnosis; High-risk patient(N = 112,077 visits) | 34,051 (9.3) | 11,234 (9.6) | 137.7 (164.1) 90.0 [60.0 – 150.0] |
134.6 (161.5) 90.0 [60.0 – 150.0] |
IQR = interquartile range
Among patients with any opioid prescription
Table 3 describes the adjusted associations between implementation of automated PDMP queries and outcomes. Automated PDMP queries were not associated with significant changes in the proportion of visits with opioid prescribing (5.8 per 1000 encounters, 95%CI: −0.11, 11.8) or in the amount of MMEs prescribed at these visits (2.66, 95%CI: −0.15, 5.48). There was no evidence of selective effect on visits for patients with prior high risk opioid use, either for all ED visits (visits with any opioid: 1.2 per 1000 encounters, 95%CI: −9.5, 12.0; MMEs: 1.22, 95%CI: −3.39, 5.82) or for visits with a pain related diagnosis (visits with any opioid: −2.5 per 1000 encounters, 95%CI: −15.9, 10.8; MMEs: 1.20, 95%CI: −4.81, 7.21). Among patients without prior high risk opioid use who had a pain related diagnosis, automated PDMP queries were associated with a small increase in the proportion of visits with opioid prescribing (13.3 per 1000 encounters, 95%CI: 3.4, 23.1) relative to high risk patients. We did not find evidence of differential quantity of prescribed MMEs by prior history of high risk opioid use.
Table 3.
Adjusted Associations between Implementation of Automated PDMP Queries and Outcomes
|
Any opioid prescription1 per 1000 encounters [95% CI] |
Total dispensed MME2,3 estimate [95% CI] |
|
|---|---|---|
| Overall | 5.8 [−0.11, 11.8] | 2.66 [−0.15, 5.48] |
| Not high-risk patient | 7.2 [2.1, 12.3] | 2.98 [0.48, 5.49] |
| High-risk patient | 1.2 [−9.5, 12.0] | 1.22 [−3.39, 5.82] |
| Difference | 6.0 [−1.6, 13.5] | 1.77 [−1.88, 5.41] |
| Pain diagnosis; Not high-risk patient | 10.7 [2.5, 19.0] | 3.78 [1.47, 6.09] |
| Pain diagnosis; High-risk patient | −2.5 [−15.9, 10.8] | 1.20 [−4.81, 7.21] |
| Difference | 13.3 [3.4, 23.1] | 2.58 [−2.83, 7.99] |
For overall and high-risk vs not high-risk models, total observations were N= 1,187,237 visits. After restricting to visits with a pain diagnosis, total observations were N = 482,781 visits.
Among patients with any opioid prescription
For overall and high-risk vs not high-risk models, total observations were N= 209,668 visits. After restricting to visits with a pain diagnosis, total observations were N = 129,948 visits.
In the sub-cohort of beneficiaries with any prior dispense of a controlled substance, the proportion of validated PDMP queries associated with an ED visit were 4% before the intervention and 71% after the intervention. Table 4 describes the results of the sensitivity analysis that compared ED visits of this sub-cohort with a confirmed PDMP query in the post-intervention phase with all ED visits in the pre-intervention phase. There were small increases in both the proportion of visits with opioid prescribing (13.6 per 1000 encounters, 95%CI: 6.5, 20.7) and prescribed MMEs (4.10, 95%CI: 1.08, 7.13) associated with the intervention. There was no evidence of decreased opioid prescribing or MMEs in patients with prior high-risk opioid use. We did find the intervention resulted in relatively higher proportion of opioid prescribing in patients without a history of high-risk opioid use, compared to those who did have such a history for all diagnoses (differential prescribing proportion for all ED visits: 9.4 per 1000 encounters, 95%CI 2.4, 16.4; differential prescribing proportion for visits with a pain related diagnosis: 19.6 per 1000 encounters, 95%CI 10.5, 28.8). We did not find statistically significant evidence of differential quantity of prescribed MMEs by prior history of high risk opioid use.
Table 4.
Effect of Confirmed Automated PDMP Queries for Patients with Any Prior History of Controlled Substance Use
|
Any opioid prescription1 per 1000 encounters [95% CI] |
Total dispensed MME2,3 estimate [95% CI] |
|
|---|---|---|
| Overall | 13.6 [6.5, 20.7] | 4.10 [1.08, 7.13] |
| Not high-risk patient | 16.5 [10.1, 23.0] | 4.03 [1.31, 6.76] |
| High-risk patient | 7.1 [−3.4, 17.6] | 3.76 [−0.60, 8.12] |
| Difference | 9.4 [2.4, 16.4] | 0.27 [−3.01, 3.56] |
| Pain diagnosis; Not high-risk patient | 20.3 [10.3, 30.2] | 4.95 [2.29, 7.62] |
| Pain diagnosis; High-risk patient | 0.63 [−11.5,12.8] | 3.00 [−2.69, 8.69] |
| Difference | 19.6 [10.5, 28.8] | 1.95 [−2.93, 6.83] |
For overall and high-risk vs not high-risk models, total observations were N= 807,971 visits. After restricting to visits with a pain diagnosis, total observations were N = 340,785 visits.
Among patients with any opioid prescription
For overall and high-risk vs not high-risk models, total observations were N= 167,315 visits. After restricting to visits with a pain diagnosis, total observations were N = 103,685 visits.
Finally, there was no evidence of selective reductions in opioid prescribing or dispensed MMEs by specific opioid high risk indicators, either in the overall cohort (eTable 3) or in the sub-cohort with a confirmed PDMP query in the post-intervention phase (eTable 4).
Limitations
First, we focused on Medicaid beneficiaries in a single state, and the generalizability of our findings requires external validation. Second, we were unable to match opioid prescriptions by treating ED providers because of high frequency of missing prescriber data. However, our approach of attributing opioid prescriptions results in almost identical estimates compared to a national sample of ED visits using chart review to ascertain opioid prescribing.32 Third, although we exploited the staggered implementation of the automated PDMP to generate effect estimates, it is possible that our findings are confounded by unmeasured factors. Fourth, it is possible that providers did not check information in EDIE that was generated by the automated PDMP query. Fifth, the automated PDMP query would not have captured controlled substances dispensed in other states. Sixth, our sensitivity analysis of validated PDMP query was limited to patients with a prior PDMP record. However, we believe that ED providers are often unaware of prior controlled substance use, and we have no reason to believe that providers use PDMP data in a differential manner in patients with and without prior controlled substance use. Finally, our findings may be unique to the ED setting due to the challenges of acute pain management and episodic care. Automated PDMP queries may have different efficacy in outpatient settings.
Discussion
In this large cohort of ED visits by Medicaid beneficiaries, an automated PDMP query intervention was not associated with reductions in opioid prescribing or quantities, even in patients with objective evidence of prior high-risk opioid use. These findings were robust to multiple sensitivity analyses, including restriction to pain related visits, restriction to visits with a confirmed PDMP query in the post period, and assessment of six specific opioid high risk indicators. We did note a small increase in opioid prescribing in patients without evidence of prior high-risk opioid use. These findings suggest limited efficacy of the policy to reduce opioid prescribing in emergency department settings. Paradoxically, the intervention may have increased the willingness of clinicians to prescribe opioids to patients without prior high-risk opioid use.
These findings are unexpected. The low proportion of PDMP usage in the pre-intervention period is consistent with other reports14–16, and the intervention did markedly improve the proportion of ED visits with a validated PDMP query. Several state-level evaluations suggest that PDMP implementation is associated with reductions in doctor shopping, pharmacy shopping, and prescription drug overdose17,23,33–35, although these findings are not universal.36,37 Features such as mandatory registration35, mandatory use17,18,38, and active monitoring of suspicious prescribing, dispensing, or purchasing activity18 may increase the efficacy of PDMPs. Several studies also suggest that providers alter prescribing behavior when given unsolicited PDMP data.10,39,40
There are several potential explanations for our findings. Although the automated PDMP initiative was designed to minimize user burden by incorporating queries into the pre-existing EDIE system, it is possible that providers did not access these data. It is possible that providers were unaware that a PDMP report had been generated, did not think that PDMP data would change their management, or that they ignored reports due to “alert fatigue.”41
We noted that 71% of ED visits in the post-implementation period had verified queries. Mismatches may be attributable to invalid queries (e.g. data entry errors, unable to obtain identifying information due to patient condition) and may have attenuated the effect of the automated query. However, we found no changes in our findings in sensitivity analyses that focused on patients with a validated PDMP query.
The automated PDMP initiative was implemented in the context of multiple Washington state policies aimed at inappropriate opioid prescribing in use over the past decade.42 The state legislature enacted several mandates specifically targeting EDs in 2012, including the adoption of strict ED opioid prescribing guidelines and mandatory PDMP registration of all ED providers.43 It is possible that these prior interventions altered ED opioid prescribing habits and attenuated the effect of the automated PDMP intervention. However, the observed proportion of opioid prescribing in our current study (i.e. after the 2012 mandates) are virtually identical to those reported from national data32, and we previously demonstrated a minimal impact of the hospital mandates on ED opioid prescribing.44
The Washington state initiative generated a PDMP report for eligible encounters, but there was no accompanying recommendations or clinical decision support. Despite strict opioid prescribing guidelines that were in place during the study period45, ED providers may have been unaware of guidelines or unclear about how to apply them to specific patient encounters in the context of PDMP information. For example, a prior survey of 515 ED providers in Florida suggested that 35% were unaware of opioid prescribing guidelines, and that 24% were aware but did not follow such guidelines.16
Finally, acute pain treatment in the ED is fundamentally different from chronic pain management in outpatient settings. In some cases it may be appropriate to treat acute conditions (e.g. bone fracture) or exacerbation of chronic pain with opioid analgesics. The default approach for some ED providers may be to provide opioid pain control, and the value of the PDMP may be to justify this approach in patients without flags for prior high risk use. Our study found evidence of small increases in opioid prescribing to patients without high risk flags. Supportive findings have been reported from two smaller studies which assessed how PDMP data impacted opioid prescribing by emergency physicians. In a study of 179 ED visits, PDMP data resulted in reduced opioid prescribing in 25% of encounters and increased opioid prescribing in 16% of encounters.10 In another study of 544 ED visits, PDMP data decreased opioid prescribing in 3% and increased prescribing in 6% of encounters.46
Our findings have important policy implications, as the automated PDMP initiative requires monetary and staff resources. Automated PDMP queries may need to be combined with provider education and/or decision support, although further studies are required to assess the efficacy of multi-modal interventions. Automated queries may be less effective than PDMP use mandates in changing ED provider behavior.
In summary, an automated PDMP query intervention in ED settings was not associated with reductions in opioid prescribing or quantities, even in patients with objective evidence of prior high-risk opioid use. Additional policies, including provider education and clinical decision support, may be required to alter ED prescribing patterns.
Supplementary Material
Acknowledgments
Grant Support
This study was supported by National Institutes of Health (NIH) grant R01DA036522.
The funding organization had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. The contents do not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflicts of Interest: None
Author Contributions Statement
BCS, KJM, and HK designed the study. BCS and KJM obtained funding for this study. CJC, NLM, and JIY were responsible for data management and data analysis. BCS drafted the manuscript. All authors contributed substantially to manuscript revisions. BCS takes responsibility for the paper as a whole. CJC, NLM, and JIY had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors approved the final report for submission.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.NCHS Data Brief. [Accessed October 10, 2012];Drug Poisoning Deaths in the United States, 1980–2008. 2011 :81. http://www.cdc.gov/nchs/data/databriefs/db81.htm. [PubMed]
- 2.CDC. [Accessed Apr 20, 2017];Prescription opioid overdose data. 2016 https://www.cdc.gov/drugoverdose/data/overdose.html.
- 3.National Center for Health Statistics. Medication Therapy in ambulatory medical care: United States, 2003–2004. [Accessed October 10, 2012];Vital and Health Statistics. 2006 series 13, Number 163. http://www.cdc.gov/nchs/data/series/sr_13/sr13_163.pdf#page=26#page=26. [PubMed]
- 4.Zechnich AD, Hedges JR. Community-wide emergency department visits by patients suspected of drug-seeking behavior. Academic emergency medicine: official journal of the Society for Academic Emergency Medicine. 1996 Apr;3(4):312–317. doi: 10.1111/j.1553-2712.1996.tb03443.x. [DOI] [PubMed] [Google Scholar]
- 5.Geiderman JM. Keeping lists and naming names: habitual patient files for suspected nontherapeutic drug-seeking patients. Annals of emergency medicine. 2003 Jun;41(6):873–881. doi: 10.1067/mem.2003.210. [DOI] [PubMed] [Google Scholar]
- 6.Graber MA, Gjerde C, Bergus G, Ely J. The use of unofficial “problem patient” files and interinstitutional information transfer in emergency medicine in Iowa. The American journal of emergency medicine. 1995 Sep;13(5):509–511. doi: 10.1016/0735-6757(95)90158-2. [DOI] [PubMed] [Google Scholar]
- 7.Hansen GR. The drug-seeking patient in the emergency room. Emergency medicine clinics of North America. 2005 May;23(2):349–365. doi: 10.1016/j.emc.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 8.Cantrill SV, Brown MD, Carlisle RJ, et al. Clinical policy: critical issues in the prescribing of opioids for adult patients in the emergency department. Annals of emergency medicine. 2012 Oct;60(4):499–525. doi: 10.1016/j.annemergmed.2012.06.013. [DOI] [PubMed] [Google Scholar]
- 9.Gugelmann HM, Perrone J. Can prescription drug monitoring programs help limit opioid abuse? JAMA: the journal of the American Medical Association. 2011 Nov 23;306(20):2258–2259. doi: 10.1001/jama.2011.1712. [DOI] [PubMed] [Google Scholar]
- 10.Baehren DF, Marco CA, Droz DE, Sinha S, Callan EM, Akpunonu P. A statewide prescription monitoring program affects emergency department prescribing behaviors. Annals of emergency medicine. 2010 Jul;56(1):19–23. e11–13. doi: 10.1016/j.annemergmed.2009.12.011. [DOI] [PubMed] [Google Scholar]
- 11.Green TC, Mann MR, Bowman SE, et al. How does use of a prescription monitoring program change medical practice? Pain Med. 2012 Oct;13(10):1314–1323. doi: 10.1111/j.1526-4637.2012.01452.x. [DOI] [PubMed] [Google Scholar]
- 12.Greenwood-Ericksen MB, Poon SJ, Nelson LS, Weiner SG, Schuur JD. Best Practices for Prescription Drug Monitoring Programs in the Emergency Department Setting: Results of an Expert Panel. Annals of emergency medicine. 2016 Jun;67(6):755–764. e754. doi: 10.1016/j.annemergmed.2015.10.019. [DOI] [PubMed] [Google Scholar]
- 13.Poon SJ, Greenwood-Ericksen MB, Gish RE, et al. Usability of the Massachusetts Prescription Drug Monitoring Program in the Emergency Department: A Mixed-methods Study. Academic emergency medicine: official journal of the Society for Academic Emergency Medicine. 2016 Apr;23(4):406–414. doi: 10.1111/acem.12905. [DOI] [PubMed] [Google Scholar]
- 14.Feldman L, Williams KS, Coates J, Knox M. Awareness and utilization of a prescription monitoring program among physicians. Journal of pain & palliative care pharmacotherapy. 2011;25(4):313–317. doi: 10.3109/15360288.2011.606292. [DOI] [PubMed] [Google Scholar]
- 15.Barrett K, Watson A. Physician perspectives on a pilot prescription monitoring program. Journal of pain & palliative care pharmacotherapy. 2005;19(3):5–13. [PubMed] [Google Scholar]
- 16.Young HW, 2nd, Tyndall JA, Cottler LB. The current utilization and perceptions of prescription drug monitoring programs among emergency medicine providers in Florida. International journal of emergency medicine. 2017 Dec;10(1):16. doi: 10.1186/s12245-017-0140-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Buchmueller TC, Carey C. NBER Papers. Feb, 2017. The Effect of Prescription Drug Monitoring Programs on Opioid Utilization in Medicare. [Google Scholar]
- 18.Pardo B. Do more robust prescription drug monitoring programs reduce prescription opioid overdose? Addiction. 2016 Dec 23; doi: 10.1111/add.13741. [DOI] [PubMed] [Google Scholar]
- 19. [Accessed Feb 2, 2017];Should California doctors be required to use drug monitoring database? 2015 https://ww2.kqed.org/stateofhealth/2015/08/13/should-california-doctors-be-required-to-use-drug-monitoring-database/
- 20.CDC. Overdose deaths involving prescription opioids among medicaid enrollees - Washington, 2004–2007. [Accessed March 7, 2016];MMWR Weekly. 2009 58(42):1171–1175. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5842a1.htm. [PubMed] [Google Scholar]
- 21.Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain-United States, 2016. JAMA: the journal of the American Medical Association. 2016 Mar 15; [Google Scholar]
- 22.NCQA HEDIS. [Accessed March 16, 2016];Technical Specifications for Health Plans. 2014 www.ncqa.org/HEDISQualityMeasurement/HEDISMeasures/HEDIS2014.aspx.
- 23.Bao Y, Pan Y, Taylor A, et al. Prescription Drug Monitoring Programs Are Associated With Sustained Reductions In Opioid Prescribing By Physicians. Health Aff (Millwood) 2016 Jun 01;35(6):1045–1051. doi: 10.1377/hlthaff.2015.1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Paulozzi LJ, Kilbourne EM, Desai HA. Prescription drug monitoring programs and death rates from drug overdose. Pain Med. 2011 May;12(5):747–754. doi: 10.1111/j.1526-4637.2011.01062.x. [DOI] [PubMed] [Google Scholar]
- 25.Oregon Health & Science University. [Accessed March 16, 2016];Guideline for Safe Chronic Opioid Therapy Prescribing For Patients with Chronic Non-cancer Pain. 2014 http://www.ohsu.edu/gim/epiclinks/opioidresources/OHSU_Opioid%20Guideline_1%2014.pdf.
- 26.Centers for Medicare and Medicaid Services. [Accessed March 8, 2016];Opioid Morphine Equivalent Conversion Factors. 2015 https://www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovContra/Downloads/Opioid-Morphine-EQ-Conversion-Factors-March-2015.pdf.
- 27.Kronick R, Gilmer T, Dreyfus T, Lee L. Improving health-based payment for Medicaid beneficiaries: CDPS. Health care financing review. 2000 Spring;21(3):29–64. [PMC free article] [PubMed] [Google Scholar]
- 28.Ettner SL, Frank RG, McGuire TG, Hermann RC. Risk adjustment alternatives in paying for behavioral health care under Medicaid. Health services research. 2001 Aug;36(4):793–811. [PMC free article] [PubMed] [Google Scholar]
- 29.Sullivan MJ, Adams H, Tripp D, Stanish WD. Stage of chronicity and treatment response in patients with musculoskeletal injuries and concurrent symptoms of depression. Pain. 2008 Mar;135(1–2):151–159. doi: 10.1016/j.pain.2007.05.021. [DOI] [PubMed] [Google Scholar]
- 30.Logan J, Liu Y, Paulozzi L, Zhang K, Jones C. Opioid prescribing in emergency departments: the prevalence of potentially inappropriate prescribing and misuse. Medical care. 2013 Aug;51(8):646–653. doi: 10.1097/MLR.0b013e318293c2c0. [DOI] [PubMed] [Google Scholar]
- 31.Sun BC, Chi DL, Schwarz E, et al. Emergency department visits for nontraumatic dental problems: a mixed-methods study. American journal of public health. 2015 May;105(5):947–955. doi: 10.2105/AJPH.2014.302398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kea B, Fu R, Lowe RA, Sun BC. Interpreting the National Hospital Ambulatory Medical Care Survey: United States Emergency Department Opioid Prescribing, 2006–2010. Academic emergency medicine: official journal of the Society for Academic Emergency Medicine. 2016 Feb;23(2):159–165. doi: 10.1111/acem.12862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Patrick SW, Fry CE, Jones TF, Buntin MB. Implementation Of Prescription Drug Monitoring Programs Associated With Reductions In Opioid-Related Death Rates. Health Aff (Millwood) 2016 Jul 01;35(7):1324–1332. doi: 10.1377/hlthaff.2015.1496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moyo P, Simoni-Wastila L, Griffin BA, et al. Impact of prescription drug monitoring programs (PDMPs) on opioid utilization among Medicare beneficiaries in 10 US States. Addiction. 2017 May 12; doi: 10.1111/add.13860. [DOI] [PubMed] [Google Scholar]
- 35.Wen H, Schackman BR, Aden B, Bao Y. States With Prescription Drug Monitoring Mandates Saw A Reduction In Opioids Prescribed To Medicaid Enrollees. Health Aff (Millwood) 2017 Apr 01;36(4):733–741. doi: 10.1377/hlthaff.2016.1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yarbrough CR. Prescription Drug Monitoring Programs Produce a Limited Impact on Painkiller Prescribing in Medicare Part D. Health services research. 2017 Jan 18; doi: 10.1111/1475-6773.12652. [DOI] [PMC free article] [PubMed]
- 37.Nam YH, Shea DG, Shi Y, Moran JR. State prescription drug monitoring programs and fatal drug overdoses. The American journal of managed care. 2017 May;23(5):297–303. [PubMed] [Google Scholar]
- 38.Brown R, Riley MR, Ulrich L, et al. Impact of New York prescription drug monitoring program, I-STOP, on statewide overdose morbidity. Drug and alcohol dependence. 2017 Sep 01;178:348–354. doi: 10.1016/j.drugalcdep.2017.05.023. [DOI] [PubMed] [Google Scholar]
- 39.Young LD, Kreiner PW, Panas L. Unsolicited Reporting to Prescribers of Opioid Analgesics by a State Prescription Drug Monitoring Program: An Observational Study with Matched Comparison Group. Pain Med. 2017 Apr 04; doi: 10.1093/pm/pnx044. [DOI] [PubMed] [Google Scholar]
- 40.Gonzalez AM, Kolbasovsky A. Impact of a managed controlled-opioid prescription monitoring program on care coordination. The American journal of managed care. 2012 Sep;18(9):516–524. [PubMed] [Google Scholar]
- 41.Agency for Healthcare Research and Quality. [Accessed August 16, 2017];Alert Fatigue. 2017 https://psnet.ahrq.gov/primers/primer/28/alert-fatigue.
- 42.Franklin G, Sabel J, Jones CM, et al. A comprehensive approach to address the prescription opioid epidemic in Washington State: milestones and lessons learned. American journal of public health. 2015 Mar;105(3):463–469. doi: 10.2105/AJPH.2014.302367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Washington Health Care Authority. [Accessed October 10, 2012];Best Practices for Hospitals to Reduce Unnecesary Use of the Emergency Room by Medicaid Clients. 2012 http://www.wsha.org/files/Attestation%20and%20Best%20Practices%20ER%20April%2016.pdf.
- 44.Sun BC, Lupulescu-Mann N, Charlesworth CJ, et al. Impact of Hospital “Best Practice” Mandates on Prescription Opioid Dispensing After an Emergency Department Visit. Academic emergency medicine: official journal of the Society for Academic Emergency Medicine. 2017 Aug;24(8):905–913. doi: 10.1111/acem.13230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Washington State Medical Association. [Accessed June 18, 2015];Washington Emergency Department Opioid Prescribing Guidelines. http://www.maineacep.org/uploadedFiles/Maine/edopioidabuseguidelinesfinal.pdf.
- 46.Weiner SG, Griggs CA, Mitchell PM, et al. Clinician impression versus prescription drug monitoring program criteria in the assessment of drug-seeking behavior in the emergency department. Annals of emergency medicine. 2013 Oct;62(4):281–289. doi: 10.1016/j.annemergmed.2013.05.025. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.