Abstract
Background
Economic evidence relating to tobacco control is generally derived from the cost effectiveness of smoking-cessation programs or the economic impact of tobacco-induced disease, based on revealed-preference data. However, empirical estimates from stated-preference data on tobacco users’ preferences, smoking behaviour and smoking cessation aids using analytical techniques such as discrete-choice experiments (DCEs) could be important for policy decision making in tobacco control.
Objectives
Our objective was to review the practice and utility of DCE methodology across nicotine- and tobacco-related issues, particularly smoking and smoking-cessation behaviour, anti-smoking policies and preferences for smoking-cessation aids.
Methods
We searched the PubMed, MEDLINE and ECONLIT databases for full-text original research articles on tobacco-related issues published between January 2000 and April 2016 that used a DCE method. We summarised the evidence and methodological characteristics of DCEs according to Lancsar and Louviere, 2008.
Results
Our review of the 12 eligible studies showed that DCE methodology was used to elicit smoker preferences and to evaluate tobacco-control policies. The majority of the studies were published in the last 5 years. The areas of application were smoking cessation, smoking behaviour, electronic cigarette use, water-pipe smoking and tobacco packaging. Monetary attributes were the most influential attributes in all studies. The design of the DCEs varied.
Conclusion
DCE studies of tobacco-related issues were methodologically consistent with guidelines proposed for conducting health-related DCEs.
Electronic supplementary material
The online version of this article (doi:10.1007/s41669-017-0025-4) contains supplementary material, which is available to authorized users.
Key Points for Decision Makers
| Discrete-choice experiments (DCEs) can be used to assess tobacco-control policies, smoking behaviour and smoker preferences for cessation aids. |
| DCE-based evidence from low- and middle-income countries could address the research gaps regarding smoking-cessation behaviour and tobacco-control policies in these countries. |
| Studies showed that monetary attributes were the most influential factor in the fight against tobacco use. Price attributes dominated tobacco policies and behaviour. |
| Future research on tobacco issues using the DCE framework should combine preferences on initiation with cessation of tobacco products, smoking-cessation therapy options and types of tobacco products to ensure DCEs fit into economic evaluations. |
Background
The discrete-choice experiment (DCE) is an elicitation technique that provides stated-preference data for analysis. They are designed to elicit quantitative preferences for attributes of health products and programmes [1]. The technique is based on random utility theory, wherein individuals are asked to make a number of choices between health products and services. Each health product and service is defined by their attributes at different levels. Responses to the DCE questionnaire are then used to infer perceived utility: overall benefit and trade-offs between attributes [1–4].
The use of DCEs in the health sector is increasing. A review [5, 6] of health-related DCEs for the periods 1990–2000 and 2001–2008 reported that the study publication rate increased from a mean of 3 to 14 per year over this period. Wide adoption of DCEs by researchers in the UK, USA, Canada and Australia is evident in the literature. However, the increase in use of DCEs among researchers in low- and middle-income countries is slower [7]. Despite the dramatic increase in the use of DCEs in the health sector, only a few are applied to health-related behaviour. Recent examples of research using DCEs relating to health behaviour include studies on smoking [8], colorectal cancer screening [9] and immunisation behaviour [10].
Tobacco use and cigarette smoking contribute to a significant proportion of the world’s mortality and morbidity [11]. An analysis of global tobacco consumption reported 6 million premature deaths from tobacco use and exposure each year, accounting for 6% of all female and 12% of all male deaths [11]. Smoking-cessation programs are a cost-effective way to mitigate the economic and health consequences of smoking [12]. The implementation and exploration of alternative methods to encourage smoking cessation and discourage initiation are a high priority. However, smoking initiation and cessation involve complex behaviours associated with nicotine dependence. Evidence suggests that individual, social and psychological characteristics are the main determinants of cessation. These determinants can be modified to increase the likelihood of success [13, 14]. Pharmacy-based and behavioural-based methods of smoking cessation are probably the most widely used cessation methods in public health practice. Recently, alternative intervention methods such as smartphone-based and online-based support services have also been implemented. It is important to note that factors from various perspectives overlap to when cessation succeeds or relapses over time, as previous smokers may adopt another form of tobacco. Moreover, rates of long-term smoking abstinence after being nicotine dependent are low [14]. Research from the past 30 years suggests that a combination of strategies within complex systems such as demand reduction, pharmacotherapies, behavioural therapies and population-level policies need to be employed to predict smoking-cessation behaviour and thus increase the rates of effective cessation [15, 16]. These alternatives would provide a basis for choice-based studies to reduce tobacco epidemics.
Several key processes underlying tobacco-control interventions, such as initiation, cessation, relapse, policy process and cost, have been explored using mathematical and health behaviour models. Most of these models extrapolate prevalence, morbidity, mortality or economic consequences based on sensitive assumptions and uncertainties derived from past revealed-preference data. A recent review of 118 studies found that 18 different tobacco-control models had been tried; however, these are continuously changing with shifts in research focus—from explaining disease burden to economic consequences of tobacco use [17]. In contrast, DCEs can easily predict results of the tobacco-control interventions that are yet to be implemented and better reflect the influence of attributes over time. The use of DCE estimates such as cost, time, health risk and health outcomes could add precise parameter values to existing population mathematical models. Evidence from DCEs can provide high predictive value of behavioural responses that correspond to real-life situations [18]. For instance, an increase in tobacco price via taxation is an example of a population-level tobacco-control policy. Studies from Japan have shown that the pricing policy for smoking behaviour change could be the game changer in anti-tobacco campaigns [8, 19]. Yet, only a few studies have used such research designs [20].
DCEs that are predominantly used as econometric tools to assess healthcare interventions do not have a long history of application to behavioural problems such as smoking and smoking cessation [1, 4–6, 21]. Moreover, the theoretical literature has not consistently defined a precise application of DCEs for research on smoking, cessation behaviour, population-level policies and related preferences [8, 19]. In addition, empirical studies that have evaluated the relative influence of multiple variables and dimensions are also limited. Overall, DCE-based empirical literature often lacks consistency in supporting standardised applications for tobacco control. Therefore, this study aimed to review and compare the application of DCE methods in existing tobacco-control studies.
Methods
Search Strategy
We conducted a literature search in the PubMed, MEDLINE and ECONLIT databases to identify original, peer-reviewed studies published between 1 January 2000 and 30 April 2016. We searched the free text, medical subject headings (MeSH) and index words related to tobacco and smoking cessation (Table 1), restricting the searches to papers published in the English language. We also manually searched the reference lists of each selected study. Duplicates were removed (by KR and NT) and titles, abstracts and methods were screened. The papers were selected based on the following eligibility criteria:
Subjects: The choice experiment was performed in adult smokers (aged ≥16 years) with the cognitive ability to perform choice tasks.
Study type: Economic evaluations, policy evaluations, preference measurements and predictive epidemiological studies with choice-based response formats.
Study design: Studies using the DCE framework in their experimental design. We included studies that clearly mentioned discrete-choice model-based analyses of preference data collected from tobacco users using choice-based response formats. We ensured that the experimental designs of the selected articles attempted to control for interactions between variables.
Table 1.
Search strategy
| Search focus | Keywords |
|---|---|
| Study design (Scope 1) | Discrete Choice Experiment OR Choice Model*OR Stated preference methods OR Preference OR Patient preference{MeSH} OR Choice behaviour {MeSH} |
| Tobacco-related issues (Scope 2) | Tobacco OR Nicotine OR Cigarettes OR Electronic cigarettes OR Water-pipe tobacco OR Tobacco Use OR Tobacco chewing OR Vaping OR Smoking behaviour OR Smoking OR Anti-tobacco policy OR Tobacco control OR Smoking regulation OR Health warnings OR Pricing policies OR Packaging OR plain packaging OR Branding |
| Treatment or outcomes (Scope 3) | Smoking cessation {MeSH} OR Tobacco Use cessation product {MeSH} OR smoking prevention OR smoking cessation therapy OR nicotine replacement therapy OR behavioural therapy OR pharmacotherapy |
| Final search [(Scope 1) AND (Scope 2) AND (Scope 3)] |
MeSH medical subject heading
* Indicates a wild card
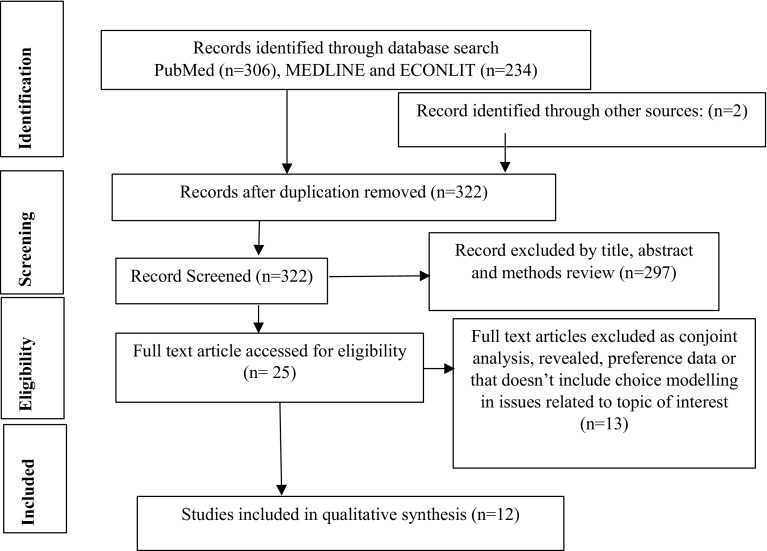
We excluded reviews, conference papers, commentaries, letters and studies that presented methodological issues or used conjoint analysis with rankings or ratings including best–worst scaling. The purpose of this exclusion was to achieve uniformity in the selected studies to facilitate a fairer comparison of the methods used to conduct the DCEs. The title, abstract and method sections of all potential articles meeting the inclusion criteria were independently studied by two authors (KR and NT). During the screening of selected articles, appropriate attention was given to synonyms of DCEs, such as stated-choice methods or choice-based conjoint analysis (Fig. 1).
Fig. 1.
Flow diagram of study selection
Data Extraction
Data from and characteristics of the selected studies were assessed using the guidelines of Lancsar and Louviere [22] to check the DCE method quality. We used an adapted version of the report format used by Mandeville et al. [23], which was also developed from the former guidelines, to assess the validity of each study. Reporting items included information on study design, selection of attributes, method of creating the choice set, questionnaire and sampling design, estimation method, and application to tobacco-related issues. Two reviewers (KR and NT) independently extracted data, and any dissimilarities were resolved through discussion. A kappa inter-rater agreement of 85% was achieved using SPSS version 16 [24].
Results
Details of Selected Discrete-Choice Experiment (DCE) Studies
Only one [25] of the 12 studies selected was conducted in a developing country (Lebanon). This study elicited preferences for a university-based smoking-cessation program. The other 11 studies were conducted in developed countries: Japan, USA, UK, Canada, Switzerland and Sweden. The majority of studies (8/12) were published in the last 5 years. We found a variety of areas of application within tobacco research: half of the studies focused on smoking cessation, two on smoking behaviour [8, 19], two on electronic cigarette use [26, 27], one on waterpipe smoking [28] and another on cigarette packaging issues [29]. Six studies were published in journals that focus on smoking addiction, and four were published in health economics journals. A single study each was published in a general public health and health technology assessment journal (Table 2).
Table 2.
Characteristics of included discrete-choice experiment studies
| Characteristic | Studies (n) |
|---|---|
| Country of origin | |
| Japan | 3 |
| Canada | 3 |
| USA | 2 |
| UK | 1 |
| Lebanon | 1 |
| Switzerland | 1 |
| Sweden | 1 |
| Year of publication | |
| 2001–2005 | 1 |
| 2006–2010 | 3 |
| 2011–2016 | 8 |
| Area of application | |
| Smoking cessation | 6 |
| Smoking behaviour | 2 |
| Electronic cigarettes | 2 |
| Water-pipe tobacco | 1 |
| Tobacco packaging | 1 |
| Source of publication | |
| Addiction/tobacco/nicotine-related journals | 6 |
| Health economics journal | 4 |
| Other public health/epidemiology journal | 1 |
| Health technology assessment journal | 1 |
Methodological Characteristics
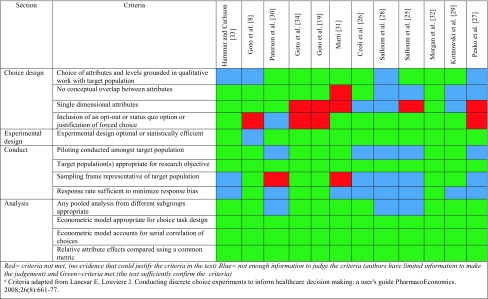
We examined the selected studies for the methodology used based on DCE stages: selection of attributes, experimental design and construction of the choice set, DCE questionnaire design, estimation method and applicability. Validity assessment is presented in Table 3 and methodological characteristics are presented in Table 4, and a summary of findings is presented in Table 5.
Table 3.
Validity assessment of the included studiesa
Table 4.
Discrete-choice experiment methodology in tobacco-control research
| References | Design | Design plan | Design source | Method of creating choice set | Number of choice sets | Questionnaire | Estimation method |
|---|---|---|---|---|---|---|---|
| Marti [31] | Fractional factorial | Main effects only and interactions | Website | Orthogonal array | 10 | Interviewer administered | All models comparison |
| Goto et al. [8] | Factorial | Main effects only with interaction | N-Logit Version 3 | Orthogonal planning method | 8 | Unclear | Mix logit model and simulation |
| Pesko et al. [27] | Balanced | Interaction with all variables | Unclear | D-efficient design D-efficiency |
12 | Unclear | Linear probability model with sensitivity analysis |
| Goto et al. [19] | Fractional factorial | Main effect only with interactions | N-Logit version 4.0 and Stata 11 | Orthogonal planning method | 8 | Unclear | Random parameter logit model |
| Paterson et al. [30] | Fractional factorial | Unclear | Expert panel | Orthogonal design | 4 | Internet | Random parameter logit |
| Czoli et al. [26] | Balance incomplete block | Main effect only with interactions | SAS v. 9.4 | Orthogonal design | 20 | Online/internet | Multinomial logit regression |
| Salloum et al. [28] | Fractional factorial | Main effects with interaction | SAS v. 9.4 | Unclear | 9 | Internet-based (tablet) | Multinomial logit regression, nested logit model |
| Salloum et al. [25] | Fractional factorial | Main effect and alternative | SAS v. 9.3 | Unlear | 8 | Interviewer | Conditional logit models |
| Goto et al. [34] | Fractional factorial | Time risk preference: survival analysis | NLOGIT 3.0 | Orthogonal planning method | 8 | Interviewer administered | Mixed logit model with simulation |
| Morgan et al. [32] | Fractional factorial | Main effect and subgroup analysis | SAS v. 9.1.2 | D efficient design (co-variance matrix) | 24 | Web-based online | Conditional logit regression model |
| Kotnowski et al. [29] | Fractional factorial | Main analysis and interaction | SAS v. 9.3 (D-efficiency 98%) | Orthogonal and balanced choice set | 10 | Web-based online | Multinomial logic model |
| Hammar and Carlsson [33] | Fractional factorial | Main analysis | SAS | D-optimal design | 4 | Unclear | Standard random effects binary Probit model |
Table 5.
Study limitations, main findings and policy decisions offered
| References | Attributes and choice scenarios | Outcome measurements | Main findings | Strengths/limitations | Policy decision offered |
|---|---|---|---|---|---|
| Marti [31] | Price efficacy, side effects, weight gains and availability (location of cessation service) | WTP for improving cessation service | Smokers are willing to pay for higher efficacy, less-frequent side effects and prevention of weight gain | Non-random non-representative sample, no measure of preference heterogeneity, discussed hypothetical bias | High demand for improved cessation service |
| Goto et al. [8] | Price, penalty, mortality, rest, passive risk of cancer | Influence in behaviour | Price has greater effect on smoker with low nicotine dependence | Use of stratified random sampling, no consideration of interaction within attributes and heterogeneity, measure goodness of fit | Nicotine dependence and individual factors emphasized in smoking-cessation counselling |
| Pesko et al. [27] | Brand, price, flavour, warning label | Measure heterogeneity in policy response | Price responsiveness was higher among adult smokers who vape. Strong warning labels reduced smoking by about 5% | Internal and theoretical validity maintained, studied only current smokers, non-random sampling | Tax increase and strong warning label encouraged switch to electronic nicotine delivery system |
| Goto et al. [19] | Price per pack, fine, mortality risk, short-term risk, health risk to others | Attitude change due to anti-smoking policies | Price consistently influenced smokers of all dependence levels to attempt to quit; risk information and a smoking ban were effective only for low-dependence smokers | Test of internal validity assumed based on design | Anti-tobacco pricing policies changes smoker’s attitude |
| Paterson et al. [30] | Frequency of dose, availability of cessation service, duration of use, success rate, total cost | Heterogeneity in preference for smoking cessation service, WTP | Systematic preference heterogeneity and random heterogeneity for therapy types by dose, light smokers were willing to pay more for 40% of success rate | Pretesting of choices, non-random sampling | Increasing success rate should be the primary focus of smoking-cessation programs |
| Czoli et al. [26] | Flavour, nicotine content, health warning, price | Preference for electronic cigarettes | Both flavour (36%) and health warnings (35%) significantly predicted perceptions of product harm; heterogeneity in consumers’ trade-offs with respect to e-cigarette product characteristics | Cross-validation of the study findings across other design, convenience sampling | Health warnings and flavour need to be targeted for e-cigarette regulation |
| Salloum et al. [28] | Flavour, nicotine content, price of waterpipe tobacco | Impact on consumer choice of attributes and between-subject assignment of health warnings | More females preferred flavoured product than males, health warning prompt subject to opt out, fruit-flavoured products were chosen most | Convenience sampling and no systematic effort to control sampling factors | Water pipe-specific regulation should limit the availability of flavoured water pipe tobacco and require accurate labelling of constituents |
| Salloum et al. [25] | Treatment type, risk of side effect, cessation support service, distance travelled, cost | Attribute of most importance for cessation, WTP | Respondents were willing to give up $US70 to avoid an additional 10% risk of minor side effects and $US12 to avoid an addition km of travel to the nearest pharmacy | Convenience sampling | Young students are willing to trade-off to be smoke free |
| Goto et al. [34] | Reward, time delayed | Time discount rate, risk aversion, duration of smoking cessation | Time and risk parameters significantly predicted the success attempts of those who had already quit for up to 1 month at baseline | Follow-up design to measure time risk, over-estimation, purposive selection | Time and risk preference determine long-term quit |
| Morgan et al. [32] | First meeting with expert adviser, frequency of meeting, support method, incentive, quitting pal | Likelihood of quitting, subgroup analysis | Incentives of >£20–80 per month are required to increase the likelihood of quitting. Daily initial telephone or text support and a quitting pal increased their likelihood of quitting | Qualitative study and pre-test before deciding the attributes | Incentives increases quit likelihood among pregnant women |
| Kotnowski et al. [29] | Pack structure, brand, branding, warning label size, price | Impact on consumer choice | Price (23%) and branding (18%) were weighted as important in trial intent decisions, warning label size (23%) and brand (17%) were weighted important when judging product harm | Non-representative sample, limited attributes, underestimation | Standardized cigarette packaging decreases demand and misleading perceptions about product harm among females |
| Hammar and Carlsson [33] | Price, subsidy and regulation | Effectiveness of different smoking policies on smokers’ expectations to quit smoking | On average, respondents expected to quit smoking in 53% of the choice situations | Discussion on potential errors, overestimation | Restricted availability, increased cigarette prices, cessation subsidies and regulations at restaurants, increase probability of smoking cessation |
WTP willingness to pay
Selection and Level of Attributes
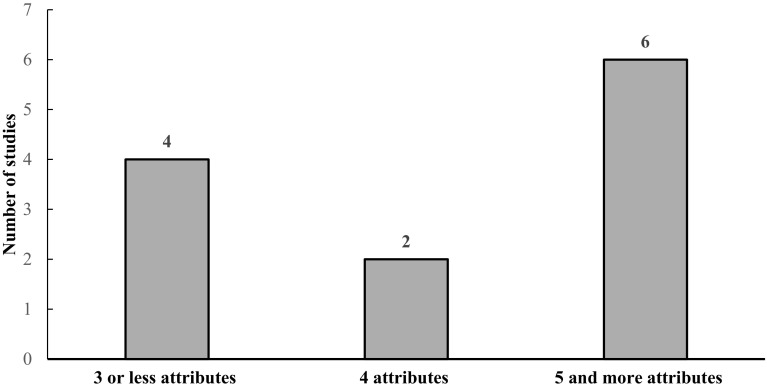
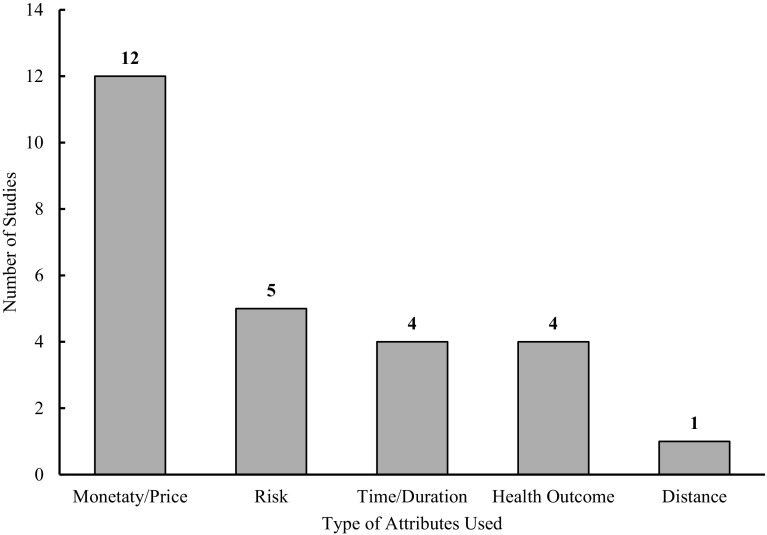
The reporting of how attributes and their respective levels were selected was consistent in most studies. Half of the studies (n = 6) selected attributes based on a literature review. Four other studies [8, 26, 30, 31] reported a literature review followed by qualitative studies such as consulting experts or focus groups. Similarly, one study [29] used a literature review and observation of market practice, and another study used comparative meta-analysis followed by a qualitative study [32]. The method of defining attribute levels was relatively inconsistent. Studies using literature reviews to define attributes tended to use qualitative techniques such as interviews [29], expert consultation [19, 26, 30], focus group rankings and pilot tests [25, 33]. Two studies [8, 34] confirmed attribute levels using a pre-test technique only, and another study [27] did not report their method clearly. Half of the studies included five or more attributes, four studies [27, 29, 33, 34] used three or fewer attributes and only two studies [25, 30] included four attributes to define utility or preference (Fig. 2). All studies included a monetary attribute in the form of an incentive, price or cost of the service. Four studies [25, 30, 32, 34] included a time attribute representing the time taken to obtain any service or the duration of travel to get there. Five articles included short- or long-term health risks [8, 19, 25, 28, 31] (Fig. 3).
Fig. 2.
Number of attributes used in studies
Fig. 3.
Types of attributes used in studies
Experimental Design and Construction of Choice Set
Ten studies followed fractional factorial design, and two studies [26, 27] applied balanced and incomplete block designs. For ten of the studies, the design plan was only to estimate the main effect and its interactions with covariates, whereas two recently published studies presented the main effect along with subgroup analysis [32] and interaction effects with all variables [27]. Half of the studies used the Statistical Analysis System (SAS; Cary, NC, USA) and three studies [8, 19, 34] used NLOGIT econometric software to design the orthogonal arrays. The method used to create choices varied among the studies. The majority (7/12) used orthogonal planning methods, and others used the D-efficient design [27], D-efficient with covariance matrix [32] or orthogonal balanced design [26].
DCE Sampling Design and Questionnaire Administration
Four of the studies used pretesting and pre-used questionnaires to make them user friendly [19, 31–33]. Three studies [8, 19, 33] used probability sampling, but the majority incorporated some form of non-probability sampling. Studies using non-probability sampling tended to pool subjects from heterogeneous subgroups and extrapolate the findings to certain groups of smokers. Eight studies administered questionnaires via the internet using web-based technology or email, and the remaining four [19, 25, 31, 34] administered interviews. Non-response rates varied from 40% [33] to 80% [34]. The number of choice sets per respondent ranged from four to 24. Only one study reported using forced choice methods [32].
Method of Estimation
The objective-oriented method of estimation was used across studies. One study presented all model comparisons [31], three [26, 28, 29] used multinomial logit models and only two studies used mixed logit models [8, 34]. The oldest study [33] used a standard random-effect binary probit model, whereas the studies conducted after 2010 [25, 26, 28, 29, 32] used mixed, multinomial or a combination of other model designs.
Validity
Validity and reliability reporting were inconsistent. However, studies reported adjusting and discussing potential errors [33] or follow-up strategies [34], discussed hypothetical bias [31], goodness-of-fit measurements [8], and pretesting of choice and cross-validation with other designs [26, 30] to maintain validity and reliability. Three studies [8, 33, 34] discussed the risks of over-estimation when comparing findings from revealed behavioural studies. Only one study [32] triangulated the findings of a DCE with revealed-preference data. Overall, the validity assessment revealed that the validity criteria in the studies were not met or could not be judged for choice design and conduct of DCEs (Table 3).
Application to Tobacco and Smoking
Half of the DCE studies evaluated preferences for various aspects of cessation services. Three studies [25, 30, 31] reported marginal willingness-to-pay (WTP) estimates. In general, studies reported that smokers were willing to trade for personalised cessation support, to increase the success rate of smoking-cessation aids and to reduce side effects from smoking-cessation medication. Three studies [27, 30, 31] investigated the existence of preference heterogeneity. Only one study [29] comprehensively illustrated the influence of tobacco packaging, marketing and branding, including the size of warning labels; however, two studies included health warnings, and both concluded they had a substantial influence on users. Two studies [26, 27] applied the DCE technique to elicit preferences for electronic cigarettes.
Tobacco-Cessation Preferences Evaluated
The two studies [26, 28] that evaluated client choices for tobacco products predicted that price, availability, tobacco packet design and health warnings (in terms of risk) were the most influential attributes. In people who intended to quit smoking, the efficacy of alternatives and treatment success rates were the most influential factors, as the study showed an increase in WTP when there were decreased chances of side effects [30] and relapse [25]. For a vulnerable group such as pregnant women, incentives significantly altered the preference for, and success of, quitting. One study [30] investigated provider-related preferences, such as the drug-distribution setting (prescription or over the counter) and fear of weight gain and concluded that those factors did not influence cessation. However, two recent studies [25, 32] revealed a strong preference for quitting associated with peer pressure, incentives and counselling frequency.
Policy Decisions
One-third of the studies reported on the effects of price trade-offs in encouraging smoking cessation in terms of WTP for improved cessation services [25, 30, 31] and investigated the influence of incentives on vulnerable populations such as pregnant women [32]. All studies reported the significant influence of monetary attributes by contextual perspective. Four studies found pricing policies to be effective, as they shifted the preferences of smokers who intended to stop smoking [8, 19], and a proposed tax increase decreased consumption [27, 34]. Two studies [30, 31] reported that increasing the availability of cessation services or drugs predicted a higher demand for cessation services and increased success rates in clinical settings. One study [29] on branding and tobacco packaging reported that standardised cigarette packaging was the most influential policy, whereas studies investigating other policy decisions such as regulating flavour in electronic cigarettes [26, 27] and use of proper warning labels [26, 27, 29] found them to be less influential (Table 5).
Discussion
Tobacco use continues to be an important public health challenge worldwide, and econometric analysis of smoking behaviour and cessation therapies is a health research priority. This paper reviewed the application of DCEs to investigate smoking-cessation interventions and tobacco control policies. We found that researchers have adopted the DCE methodology to quantify behaviour, elicit future preferences and policy options and measure policy impacts. To the best of our knowledge, this is one of the first reviews to explore how DCE techniques have been designed and used globally in this area. In addition, price attributes were dominant in all studies, the reporting of design plans was inconsistent, and studies explicitly used non-random sampling techniques.
Along with DCE studies, subject-specific reviews on the utility of DCEs in the health literature is also increasing. The existing reviews investigated the use of DCEs in pharmacy practice [35], human resources for health [23] and healthcare decision making [36]. We found a limited number of tobacco-control studies adopting DCEs, perhaps because they often require skills in advanced statistical and design techniques [37]. A majority of smoking-related DCEs were published by researchers from developed countries. Indeed, DCEs have been regularly used in health economics studies in high-income countries [6]. Only a limited number of studies have used DCEs in resource-limited settings, and the results they produce may differ from those conducted in developed countries [7]. The trend for an increase in the number of DCE-based studies on tobacco-related issues over time is similar to the trend in the use of DCEs in healthcare research [6]. Furthermore, choice modelling requires multidisciplinary skills in research design, economic theory, experimental design and, most importantly, rigorous statistical analysis, which all consume large amounts of resources and expertise [37].
In addition, as well as finding monetary attribute effects in all studies, we also found other attributes such as risk, time and health outcomes. Only a few attribute levels, such as duration of service provision and the process of getting smoking-cessation medication, were set from the perspective of health service providers at smoking-cessation clinics. More research on preference assessment from the viewpoint of the smoking-cessation service provider is needed to combine their preferences with those of tobacco users. In general, smoking-related DCEs focused particularly on price and risk attributes from the tobacco user’s perspective, which contrasts with other health-related DCEs that particularly emphasize health outcomes and the health service’s perspective [6]. Most included studies used monetary attributes as the most dominant attribute for making policy decisions based on smoker behaviour or response. Nevertheless, caution is necessary as the dominant preference effect is valid for smokers with strong preferences [3].
The validity of DCEs and their implications is still under investigation in health economics. Different types of attributes and the design of the DCE itself pose a threat to validity. In fact, evidence from environmental economics recommends the routine integration of tests of validity and reliability into a DCE framework [38]. The studies included in our review reported using a preparatory study such as expert consultation or focus group discussion when establishing attributes, in addition to the literature review. A preparatory study helps identify the appropriate attribute levels and ease in interpreting choices, thus maintaining internal validity [39, 40]. We found most studies used opportunistic or non-probability sampling. Overall, generalisability was weak; however, the objective of DCE studies is to measure weighted preferences [4]. Fractional factorial designs were the most common, adopted in nine studies; however, the design plans only included interactions with covariates such as age, sex and educational background. Furthermore, combining stated-preference and observed-preference data or comparing a DCE result with methods such as contingent valuation can only maintain external validity in choice experiments [9, 38, 41]. None of our studies reported any tests of external validity. Prior assumption of external validity was used in most studies, as suggested by some methodological studies [18, 40, 42]. The practice of assuming external validity is concurrent with a review of DCEs use in pharmacy practice [35]. A limited number of choices and attributes can provide much-needed external validity [1, 4, 43]. Furthermore, studies on complex and multifaceted health behaviours, such as smoking and smoking cessation, should use hierarchical information integration to test their theory and validity; these are considered less favourable and practical to implement but become evident with well-designed DCEs [44].
Orthogonal designs have been the most frequently used in health economics, followed by D-Optimal designs [45]. In our review, these designs were frequently reported as a method of constructing the choice set. The efficient design of DCEs is influenced by the choice-making behaviour of the study participants, and smokers and tobacco users are no exception [46]. Although the use of statistically efficient designs and statistical software is increasing [6], only one study [31] used websites to construct a choice set. Similarly, we found that the results of weighted preferences and welfare estimates varied along with the DCE framework. The recent studies used more advanced econometric analyses for valuation [10, 47]. One study assessed time and risk preferences and their relation to smoking cessation using a DCE technique and concluded that smokers with a high time discount rate were more likely to relapse. We consider this finding to be a novel application of DCEs as it extends the scope of predictors of smoking cessation. This finding also supports quasi-hyperbolic discounting, a tendency to choose current benefits over future gains in prediction [48]. One potential explanation for risk attributes explaining long-term relapse could be the behavioural nature of self-selection, which is applicable to smoking cessation but not to smoking initiation [49].
The major strengths of this study include the rigorous database search, the validity assessment of the selected studies and the outlining of policy decision options. This is a subject-specific review of the application of DCEs within the field of tobacco use. Furthermore, the study presented the progressive application of DCEs for informed econometric decision making for tobacco control.
The review also has some limitations. Our exclusion of grey literature may have neglected some relevant work within this field. However, our efforts in reference tracing from the selected articles and methodological research meant our search strategy was comprehensive and systematic. The review focussed more on a critique of methods than the results of the studies. It is not possible to answer how the results of welfare estimates can be used by policy makers. Future methodological studies and studies on generalising the findings of DCEs are recommended. Standardising the reporting and ‘method’ of approaching the question, justification and design of the study could be the first step to generating quantitative evidence from the evaluation of all tobacco-control efforts.
Implications for Practice and Research
The analysis of stated-preference data on health promotion or health behaviour change interventions from DCEs can adequately predict actual health behaviour [18]. Therefore, the application of DCEs to explain smoking or cessation behaviour has the potential to establish new interventions for tobacco control. DCEs were found that elicited preferences for electronic cigarettes and the marketing or branding of cigarettes. Electronic cigarettes and cigarette brand design are tobacco-control issues that have only recently emerged and for which limited research has been conducted [50]. The DCE framework can appropriately fit into such emerging behaviours and interventions that regularly inform policy makers and researchers. One possible benefit of using DCE techniques is that it can bring about triangulation in research findings. It promotes the estimation of the degree of effects that induce changes in smoking behaviour and the environment, as outlined by tobacco-control policies, for example, determining the effects of incentives to avert smoking in pregnancy, measuring possible changes in smokers’ attitudes and behaviours after the introduction of tobacco prohibition in public places and tobacco tax increases. Furthermore, DCEs can also help inform the design of trials to test interventions in real-life settings [32]. The elicitation of smoker preferences as well as economic evaluations for new tobacco products such as e-cigarettes, and their appropriate cessation methods, can inform decision makers who implement changes to serve smokers who are willing to quit.
Conclusions
The DCE methodology adopted in nicotine- and tobacco-related studies were consistent with the guidelines for conducting health-related DCEs. However, we observed heterogeneity in the distribution of attributes, which included price, risk, time, distance and health outcomes. Price attributes had dominant effects on tobacco policies and behaviour. Perspectives from both tobacco users and tobacco-cessation service providers could be incorporated into DCE attributes. Prominent methodological issues identified included using fewer attributes, conducting a literature review followed by qualitative techniques to confirm the choice set and good explanation of DCE theory. Moreover, designs and design plans were reported inconsistently and is a key area for improvement. We suggest standardising the reporting and ‘method’ of approaching the question, justification and design of the study. Future studies could combine preference evaluations for tobacco products, smoker’s behavioural options and cessation intervention or service providers to incorporate DCE results in an economic evaluation framework that can ease tobacco-control decision making.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors acknowledge Dharma Nand Bhatta, PhD, Faculty of Medicine, Epidemiology Unit, Prince of Songkla University, Songkhla, Thailand, for his feedback on the manuscript. Our sincere gratitude goes to Professor Hiroaki Hayakawa, UBD School of Business and Economics, for providing advice on theories of behavioural economics, the economics of tobacco use and comments on the manuscript. We thank Katie Smyth and Professor Graeme Henderson for English editing.
Author contributions
KR designed the review, searched for studies, extracted data, analyzed findings, and drafted the manuscript. DK validated the data extraction and wrote some sections of the manuscript and revised and proofread the manuscript. ST helped to write the review, interpreted the results, and performed a technical edit of the manuscript. NT contributed to the design of the study, to article screening and the final edit of the manuscript.
Compliance with Ethical Standards
Data availability statement
All data generated or analysed during this study are included in this published article (its supplementary information files).
Conflicts of interest
KR, DK, ST and NT have no conflicts of interest.
Funding
No financial assistance was received to conduct this study.
Footnotes
Electronic supplementary material
The online version of this article (doi:10.1007/s41669-017-0025-4) contains supplementary material, which is available to authorized users.
Contributor Information
Kabindra Regmi, Phone: 97761534620, Email: regmi.kabindra@gmail.com, Email: 15m4014@ubd.edu.bn.
Dinesh Kaphle, Email: dinesh.kaphle@gmail.com.
Sabina Timilsina, Email: sabina.timilsina@mail.ugm.ac.id.
Nik Annie Afiqah Tuha, Email: anni.mohamad@ubd.edu.bn.
References
- 1.Ryan M. Discrete choice experiments in health care. BMJ. 2004;328(7436):360–361. doi: 10.1136/bmj.328.7436.360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stalmeier PFM, Goldstein MK, Holmes AM, Lenert L, Miyamoto J, Stiggelbout AM, et al. What should be reported in a methods section on utility assessment? Med Decis Mak. 2001;21(3):200–207. doi: 10.1177/02729890122062497. [DOI] [PubMed] [Google Scholar]
- 3.Scott A. Identifying and analysing dominant preferences in discrete choice experiments: an application in health care. J Econ Psychol. 2002;23(3):383–398. doi: 10.1016/S0167-4870(02)00082-X. [DOI] [Google Scholar]
- 4.Ryan M, Netten A, Skåtun D, Smith P. Using discrete choice experiments to estimate a preference-based measure of outcome—an application to social care for older people. J Health Econ. 2006;25(5):927–944. doi: 10.1016/j.jhealeco.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 5.Ryan M, Gerard K. Using discrete choice experiments to value health care programmes: current practice and future research reflections. Appl Health Econ Health Policy. 2003;2(1):55–64. [PubMed] [Google Scholar]
- 6.de Bekker-Grob EW, Ryan M, Gerard K. Discrete choice experiments in health economics: a review of the literature. Health Econ. 2012;21(2):145–172. doi: 10.1002/hec.1697. [DOI] [PubMed] [Google Scholar]
- 7.Mangham LJ, Hanson K, McPake B. How to do (or not to do) … Designing a discrete choice experiment for application in a low-income country. Health Policy Plann. 2009;24(2):151–158. doi: 10.1093/heapol/czn047. [DOI] [PubMed] [Google Scholar]
- 8.Goto R, Nishimura S, Ida T. Discrete choice experiment of smoking cessation behaviour in Japan. Tob Control. 2007;16(5):336–343. doi: 10.1136/tc.2006.019281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marshall DA, Johnson FR, Kulin NA, Özdemir S, Walsh JME, Marshall JK, et al. How do physician assessments of patient preferences for colorectal cancer screening tests differ from actual preferences? A comparison in Canada and the United States using a stated-choice survey. Health Econ. 2009;18(12):1420–1439. doi: 10.1002/hec.1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hall J, Kenny P, King M, Louviere J, Viney R, Yeoh A. Using stated preference discrete choice modelling to evaluate the introduction of varicella vaccination. Health Econ. 2002;11(5):457–465. doi: 10.1002/hec.694. [DOI] [PubMed] [Google Scholar]
- 11.Bilano V, Gilmour S, Moffiet T, d’Espaignet ET, Stevens GA, Commar A, et al. Global trends and projections for tobacco use, 1990-2025: an analysis of smoking indicators from the WHO Comprehensive Information Systems for Tobacco Control. Lancet. 2015;385(9972):966–976. doi: 10.1016/S0140-6736(15)60264-1. [DOI] [PubMed] [Google Scholar]
- 12.Ekpu VU, Brown AK. The economic impact of smoking and of reducing smoking prevalence: review of evidence. Tob Use Insights. 2015;8:1–35. doi: 10.4137/TUI.S15628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lennox A. Determinants of outcome in smoking cessation. Br J Gen Pract. 1992;42(359):247–252. [PMC free article] [PubMed] [Google Scholar]
- 14.Yudkin P, Hey K, Roberts S, Welch S, Murphy M, Walton R. Abstinence from smoking eight years after participation in randomised controlled trial of nicotine patch. BMJ. 2003;327(7405):28–29. doi: 10.1136/bmj.327.7405.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mamoun M, Bergen AW, Shieh J, Wiggins A, Brody AL. Biomarkers of response to smoking cessation pharmacotherapies: progress to date. CNS Drugs. 2015;29(5):359–369. doi: 10.1007/s40263-015-0243-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Feirman S, Donaldson E, Pearson J, Zawistowski G, Niaura R, Glasser A et al. Mathematical modelling in tobacco control research: protocol for a systematic review. BMJ Open. 2015;5(4). doi:10.1136/bmjopen-2014-007269. [DOI] [PMC free article] [PubMed]
- 17.Feirman SP, Donaldson E, Glasser AM, Pearson JL, Niaura R, Rose SW, et al. Mathematical modeling in tobacco control research: initial results from a systematic review. Nicotine Tob Res. 2016;18(3):229–242. doi: 10.1093/ntr/ntv104. [DOI] [PubMed] [Google Scholar]
- 18.Salampessy BH, Veldwijk J, Jantine Schuit A, den Brekel-Dijkstra K, Neslo REJ, Ardine de Wit G, et al. The predictive value of discrete choice experiments in public health: an exploratory application. Patient. 2015;8(6):521–529. doi: 10.1007/s40271-015-0115-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goto R, Takahashi Y, Ida T. Changes in smokers’ attitudes toward intended cessation attempts in Japan. Value Health. 2011;14(5):785–791. doi: 10.1016/j.jval.2010.12.010. [DOI] [PubMed] [Google Scholar]
- 20.Lambooij MS, Harmsen IA, Veldwijk J, de Melker H, Mollema L, van Weert YWM, et al. Consistency between stated and revealed preferences: a discrete choice experiment and a behavioural experiment on vaccination behaviour compared. BMC Med Res Methodol. 2015;15:19. doi: 10.1186/s12874-015-0010-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ryan M, Amaya-Amaya M. ‘Threats’ to and hopes for estimating benefits. Health Econ. 2005;14(6):609–619. doi: 10.1002/hec.949. [DOI] [PubMed] [Google Scholar]
- 22.Lancsar E, Louviere J. Conducting discrete choice experiments to inform healthcare decision making: a user’s guide. Pharmacoeconomics. 2008;26(8):661–677. doi: 10.2165/00019053-200826080-00004. [DOI] [PubMed] [Google Scholar]
- 23.Mandeville KL, Lagarde M, Hanson K. The use of discrete choice experiments to inform health workforce policy: a systematic review. BMC Health Serv Res. 2014;14(1):1–14. doi: 10.1186/1472-6963-14-367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leech NL, Barrett KC, Morgan GA. IBM SPSS for intermediate statistics: use and interpretation. Howe: Routledge; 2014. [Google Scholar]
- 25.Salloum RG, Abbyad CW, Kohler RE, Kratka AK, Oh L, Wood KA. Assessing preferences for a university-based smoking cessation program in Lebanon: a discrete choice experiment. Nicotine Tob Res. 2015;17(5):580–585. doi: 10.1093/ntr/ntu188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Czoli CD, Goniewicz M, Islam T, Kotnowski K, Hammond D. Consumer preferences for electronic cigarettes: results from a discrete choice experiment. Tob Control. 2016;25(e1):e30–e36. doi: 10.1136/tobaccocontrol-2015-052422. [DOI] [PubMed] [Google Scholar]
- 27.Pesko MF, Kenkel DS, Wang H, Hughes JM. The effect of potential electronic nicotine delivery system regulations on nicotine product selection. Addiction. 2016;111(4):734–744. doi: 10.1111/add.13257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Salloum RG, Maziak W, Hammond D, Nakkash R, Islam F, Cheng X, et al. Eliciting preferences for waterpipe tobacco smoking using a discrete choice experiment: implications for product regulation. BMJ Open. 2015;5(9):e009497. doi: 10.1136/bmjopen-2015-009497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kotnowski K, Fong GT, Gallopel-Morvan K, Islam T, Hammond D. The impact of cigarette packaging design among young females in canada: findings from a discrete choice experiment. Nicotine Tob Res. 2015;18(5):1348–1356. doi: 10.1093/ntr/ntv114. [DOI] [PubMed] [Google Scholar]
- 30.Paterson RW, Boyle KJ, Parmeter CF, Neumann JE, De Civita P. Heterogeneity in preferences for smoking cessation. Health Econ. 2008;17(12):1363–1377. doi: 10.1002/hec.1336. [DOI] [PubMed] [Google Scholar]
- 31.Marti J. Assessing preferences for improved smoking cessation medications: a discrete choice experiment. Eur J Health Econ. 2012;13(5):533–548. doi: 10.1007/s10198-011-0333-z. [DOI] [PubMed] [Google Scholar]
- 32.Morgan H, Hoddinott P, Thomson G, Crossland N, Farrar S, Yi D, et al. Benefits of Incentives for Breastfeeding and Smoking cessation in pregnancy (BIBS): a mixed-methods study to inform trial design. Health Technol Assess. 2015;19(30):1–522, vii–viii. doi:10.3310/hta19300. [DOI] [PMC free article] [PubMed]
- 33.Hammar H, Carlsson F. Smokers’ expectations to quit smoking. Health Econ. 2005;14(3):257–267. doi: 10.1002/hec.923. [DOI] [PubMed] [Google Scholar]
- 34.Goto R, Takahashi Y, Nishimura S, Ida T. A cohort study to examine whether time and risk preference is related to smoking cessation success. Addiction. 2009;104(6):1018–1024. doi: 10.1111/j.1360-0443.2009.02585.x. [DOI] [PubMed] [Google Scholar]
- 35.Naik-Panvelkar P, Armour C, Saini B. Discrete choice experiments in pharmacy: a review of the literature. Int J Pharm Pract. 2013;21(1):3–19. doi: 10.1111/ijpp.12002. [DOI] [PubMed] [Google Scholar]
- 36.Whitty JA, Lancsar E, Rixon K, Golenko X, Ratcliffe J. A systematic review of stated preference studies reporting public preferences for healthcare priority setting. Patient. 2014;7(4):365–386. doi: 10.1007/s40271-014-0063-2. [DOI] [PubMed] [Google Scholar]
- 37.Mühlbacher A, Johnson FR. Choice experiments to quantify preferences for health and healthcare: state of the practice. Appl Health Econ Health Policy. 2016;14(3):253–266. doi: 10.1007/s40258-016-0232-7. [DOI] [PubMed] [Google Scholar]
- 38.Rakotonarivo OS, Schaafsma M, Hockley N. A systematic review of the reliability and validity of discrete choice experiments in valuing non-market environmental goods. J Environ Manag. 2016;183 Part 1:98–109. doi:10.1016/j.jenvman.2016.08.032. [DOI] [PubMed]
- 39.Kenny P, Hall J, Viney R, Haas M. Do participants understand a stated preference health survey? A qualitative approach to assessing validity. Int J Technol Assess Health Care. 2003;19(04):664–681. doi: 10.1017/S026646230300062X. [DOI] [PubMed] [Google Scholar]
- 40.Howard K, Salkeld G. Does attribute framing in discrete choice experiments influence willingness to pay? Results from a discrete choice experiment in screening for colorectal cancer. Value Health. 2009;12(2):354–363. doi: 10.1111/j.1524-4733.2008.00417.x. [DOI] [PubMed] [Google Scholar]
- 41.Ben-Akiva M, Bradley M, Morikawa T, Benjamin J, Novak T, Oppewal H, et al. Combining revealed and stated preferences data. Mark Lett. 1994;5(4):335–349. doi: 10.1007/BF00999209. [DOI] [Google Scholar]
- 42.Krucien N, Gafni A, Pelletier-Fleury N. Empirical testing of the external validity of a discrete choice experiment to determine preferred treatment option: the case of sleep apnea. Health Econ. 2015;24(8):951–965. doi: 10.1002/hec.3076. [DOI] [PubMed] [Google Scholar]
- 43.Erdem S, Campbell D, Hole AR. Accounting for attribute-level non-attendance in a health choice experiment: does it matter? Health Econ. 2015;24(7):773–789. doi: 10.1002/hec.3059. [DOI] [PubMed] [Google Scholar]
- 44.van Helvoort-Postulart D, Dellaert BGC, van der Weijden T, von Meyenfeldt MF, Dirksen CD. Discrete choice experiments for complex health-care decisions: does hierarchical information integration offer a solution? Health Econ. 2009;18(8):903–920. doi: 10.1002/hec.1411. [DOI] [PubMed] [Google Scholar]
- 45.Carlsson F, Martinsson P. Design techniques for stated preference methods in health economics. Health Econ. 2003;12(4):281–294. doi: 10.1002/hec.729. [DOI] [PubMed] [Google Scholar]
- 46.Flynn TN, Bilger M, Malhotra C, Finkelstein EA. Are efficient designs used in discrete choice experiments too difficult for some respondents? A case study eliciting preferences for end-of-life care. Pharmacoeconomics. 2015;34(3):273–284. doi: 10.1007/s40273-015-0338-z. [DOI] [PubMed] [Google Scholar]
- 47.Viney R, Savage E, Louviere J. Empirical investigation of experimental design properties of discrete choice experiments in health care. Health Econ. 2005;14(4):349–362. doi: 10.1002/hec.981. [DOI] [PubMed] [Google Scholar]
- 48.Ida T. A quasi-hyperbolic discounting approach to smoking behavior. Health Econ Rev. 2014;4:5. doi:10.1186/s13561-014-0005-7. [DOI] [PMC free article] [PubMed]
- 49.Lahiri K, Song JG. The effect of smoking on health using a sequential self-selection model. Health Econ. 2000;9(6):491–511. doi: 10.1002/1099-1050(200009)9:6<491::AID-HEC541>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 50.Correa JB, Ariel I, Menzie NS, Brandon TH. Documenting the emergence of electronic nicotine delivery systems as a disruptive technology in nicotine and tobacco science. Addict Behav. 2017;65:179–184. doi: 10.1016/j.addbeh.2016.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analysed during this study are included in this published article (its supplementary information files).