Abstract
Objectives. We aimed to summarize and critically evaluate the available evidence regarding the efficacy and safety of acupuncture for children with autism spectrum disorder (ASD). Methods. We searched 13 databases for studies published up to December 2016. Randomized controlled trials (RCTs) evaluating the efficacy of acupuncture for children with ASD were included. Outcome measures were the overall scores on scales evaluating the core symptoms of ASD and the scores for each symptom, such as social communication ability and skills, stereotypies, language ability, and cognitive function. Effect sizes were presented as mean differences (MD). Results. Twenty-seven RCTs with 1736 participants were included. Acupuncture complementary to behavioral and educational intervention significantly decreased the overall scores on the Childhood Autism Rating Scale (CARS) (MD −8.10, 95% CI −12.80 to −3.40) and the Autism Behavior Checklist (MD −8.92, 95% CI −11.29 to −6.54); however, it was unclear which of the ASD symptoms improved. Acupuncture as a monotherapy also reduced the overall CARS score. The reported adverse events were acceptable. Conclusions. This review suggests that acupuncture may be effective and safe for pediatric ASD. However, it is not conclusive due to the heterogeneity of the acupuncture treatment methods used in the studies.
1. Introduction
Autism spectrum disorder (ASD) is a neurodevelopmental disorder with an etiology that remains incompletely understood. The core symptoms of ASD include persistent deficits in social communication and interaction and restricted, repetitive patterns of behavior, interests, or activities [1]. The prevalence of ASD as reported in various studies ranges from as low as 1 in 500 to as high as 1 in 50 [2, 3].
Many types of treatments are available for ASD, but none have yet been developed that effectively treat the core symptoms. Conventional treatments for ASD include pharmacological therapy and behavioral and educational interventions (BEI). However, risperidone, a commonly used medication for the treatment of maladaptive behaviors in ASD, has adverse effects such as weight gain, fatigue, drowsiness, and tremors [4, 5]. Furthermore, the majorities of high quality BEI require 20 to 40 hours of treatment per week, and take a long time to show benefits [6–8].
The National Center for Complementary and Integrative Health describe “complementary” as a therapy used alongside conventional medicine, and “alternative” as a therapy used in place of conventional medicine [9]. Recent studies have reported that approximately 88% of a large, geographically diverse sample of children with ASD had used complementary and alternative medicine (CAM) such as gluten-free casein-free diets, melatonin, or music therapy in either the past or recently [10]. Families of children with ASD may choose CAM to treat a variety of symptoms, such as hyperactivity, inattention, gastrointestinal symptoms, or sleep disturbances [11], or due to concerns about the adverse effects of conventional treatments [12].
Acupuncture is one of the most popular forms of CAM [13]. As a form of Traditional Chinese Medicine (TCM), acupuncture is also widely used in Western countries [14]. In TCM, the pathogenesis of ASD is theorized to result from derangement or insufficiency of the brain and mind, and dysregulation of the heart, liver, spleen, and kidney after birth [15]. Acupuncture is used to correct the disharmony of organ systems and is theorized to address the symptoms of ASD by stimulating acupoints that are related to organs or viscera. The physiological mechanisms by which acupuncture works for ASD seem to be very complicated and remain unclear. The possible mechanisms by which acupuncture affects ASD include regulation of neurotransmitters [16, 17], which have been shown to be disturbed in many people with ASD [18], modulation of expression and activation of brain-derived neurotrophic factor (BDNF), which is involved in the pathophysiology of ASD [19], and so on.
Prior to 2011, systematic reviews [20, 21] concluded that there was no evidence for the use of acupuncture in ASD, because of the low total number and low methodological quality of the studies. Because of this lack of evidence, acupuncture treatment could not be recommended in existing clinical guidelines for the treatment of ASD. Since then, however, many studies of acupuncture for pediatric cases of ASD have been published. The objective of this study was to summarize and critically evaluate the updated evidence for the efficacy and safety of acupuncture for the treatment of ASD in pediatric patients.
2. Methods
This systematic review and meta-analysis was conducted according to the guidelines in the Cochrane Handbook for Systematic Reviews of Interventions [22]. Reporting was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [23]. The protocol of this review was registered in the International Prospective Register of Systematic Reviews, PROSPERO (CRD42017054544).
2.1. Search Strategy
Two authors (B. L. and J. L.) performed a comprehensive search of the following 13 electronic databases from their inception dates to 31 December 2016: six English databases (Cochrane Library, MEDLINE via EBSCO, EMBASE via Elsevier, AMED via EBSCO, CINAHL via EBSCO, and PsycARTICLES via ProQuest), two Chinese databases (Chinese National Knowledge Infrastructure (CNKI) and Wanfang Data), two Japanese databases (Japanese Institutional Repositories Online (JAIRO) and Citation Information by NII (CiNii)), and three Korean databases (Oriental Medicine Advanced Searching Integrated System (OASIS), Korean Traditional Knowledge Portal (KTKP), and KoreaMed). We also searched the reference lists of the relevant papers to identify additional trials. There was no restriction on language. In addition to the studies published in the journal, we also included grey literature, such as conference proceedings and degree theses.
The following search terms were used in MEDLINE: (autis∗ OR pervasive developmental disorder∗ OR childhood disintegrative disorder OR asperger∗ OR autism spectrum disorder OR child development disorders, pervasive) AND (acup∗ OR needl∗ OR trigger point OR body acupuncture OR scalp acupuncture OR tongue acupuncture OR auricular acupuncture OR pharmacopuncture OR bee OR acupuncture OR acupuncture therapy OR acupuncture points OR acupuncture, ear OR electroacupuncture). The details of search strategies used in all databases are presented in the Supplementary Material (Supplement 1).
2.2. Inclusion and Exclusion Criteria
2.2.1. Types of Studies
We included randomized controlled trials (RCTs) that evaluated the efficacy of acupuncture for children with ASD, including those using a quasi-random method such as alternate allocation or allocation by birth date. We included both parallel and crossover studies.
2.2.2. Types of Participants
We included patients with ASD under the age of 18 years, regardless of gender or race, diagnosed by standard criteria such as the Diagnostic and Statistical Manual of Mental Disorders (DSM) or the International Classification of Diseases (ICD). We accepted diagnoses by assessment tools such as the Autism Diagnostic Observation Scale (ADOS), Autism Diagnostic Interview-Revised (ADI-R), Childhood Autism Rating Scale (CARS), Chinese Classification of Mental Disorder (CCMD), and other validated tools. Studies on ASD were included even if they did not refer to the diagnostic criteria.
2.2.3. Types of Interventions
We included studies on acupuncture involving the insertion of needles into traditional acupoints or into nonmeridian points as experimental interventions, regardless of the acupuncture treatment method. Studies that did not involve skin penetration, such as those using acupressure, were excluded. Control interventions included pharmacological interventions, BEI, and CAM, including combinations of two or more therapy types. We also included sham acupuncture, which refers to a needle placed in an area close to but not into acupoints, as a control intervention. Studies in which the other treatments were applied to both experimental and control groups in the same manner were also included. We excluded trials that compared only different forms of acupuncture.
2.2.4. Types of Outcome Measures
The outcome measures were as follows: (1) the overall score on scales evaluating the core features of ASD, including CARS, the Autism Behavior Checklist (ABC1), the Aberrant Behavior Checklist (ABC2), the Autism Treatment Evaluation Checklist (ATEC), and the Ritvo-Freeman Real Life Rating Scale (RFRLRS); (2) social interaction skills, communication ability, or stereotypy, which are essential symptoms of ASD; and (3) language ability or cognitive function, which are associated features of ASD.
2.3. Study Selection and Data Extraction
After eliminating duplicate studies, two authors (B. L. and J. H. C.) independently screened the titles and abstracts of the searched studies to identify those that potentially met the inclusion criteria. Thereafter, the texts of the remaining articles were obtained and screened for eligibility by two authors (J. H. C. and H. K. S.).
One author (B. L.) extracted the data from the selected studies, and a different author (S. H. C.) reviewed the data. Discrepancies were resolved through discussion with a third author (G. T. C.). The extracted information included study design, country, demographic characteristics of the participants, diagnostic criteria, details of the experimental and control interventions, outcomes, adverse events, and information for assessing the risk of bias. We contacted the primary authors of the included studies via email if additional information was needed.
2.4. Quality Assessment
Two authors (J. H. C. and H. K. S.) independently evaluated the methodological quality of the included studies, using the Cochrane Collaboration's tool [22]. The following characteristics were assessed: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessments, incomplete outcome data, selective reporting, and other bias. Each domain was evaluated and categorized into three groups: “low risk,” “unclear,” or “high risk.” If the relevant information was not mentioned in the article, we evaluated the domain as “unclear.” Disagreements between the review authors over the risk of bias were resolved by discussion, with the participation of another author (J. L.).
2.5. Statistical Analysis
For studies using the same type of intervention, comparator, and outcome measure, quantitative synthesis was conducted by meta-analysis using the Review Manager software, version 5.3 (Cochrane, London, UK). Descriptive analysis was conducted when the number of reported studies was only one, or when it was considered that heterogeneity was too high for the results to be synthesized. For the meta-analyses, risk ratios (RR) and 95% CIs were calculated for dichotomous data, and mean differences (MD) and 95% CIs were used for continuous data. We used pre-post differences or end-point scores as outcome measures, presented for each included study. If among the included studies there were some measuring the change in a value, and others measuring the final value, of the same outcome measures, we planned to synthesize the data by calculating the final value as the initial value plus the change, if possible. We examined heterogeneity among the studies using the Higgins I2 test. We considered I2 ≥ 50% to be indicative of substantial heterogeneity, and I2 ≥ 75% to be indicative of serious heterogeneity. In the meta-analyses, a random effects model was used when the heterogeneity was significant, while a fixed effects model was used when the heterogeneity was not significant or the number of studies included in a meta-analysis was very small, in which case estimates of interstudy variance have poor accuracy [24].
3. Results
3.1. Study Description
3.1.1. Literature Search
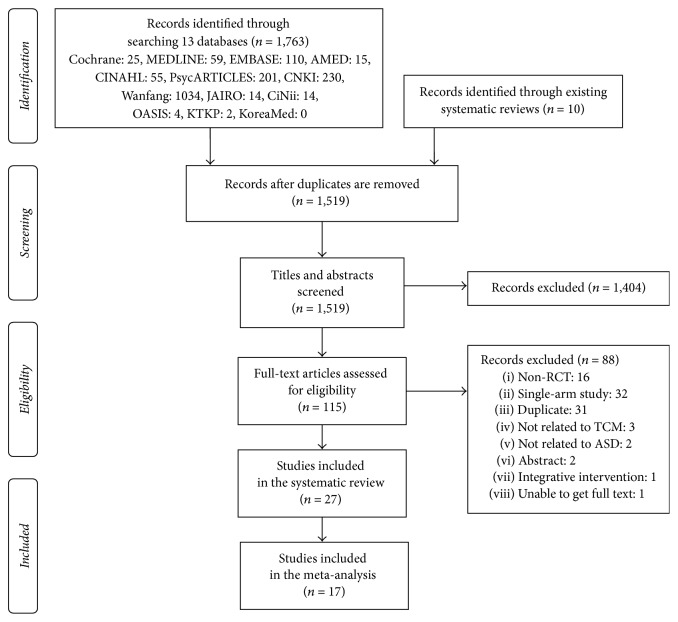
We identified 1763 records through a database search, and 10 additional records from the reference lists of relevant papers. After removing duplicates, 1519 records remained. A review of the titles and abstracts excluded 1404 records. After assessing the full text of the remaining 115 articles, we finally included 27 articles [25–51] in the systematic review and 17 articles [27, 29, 32–36, 38–43, 45–47, 49] in the meta-analysis (Figure 1).
Figure 1.
PRISMA flow chart of the literature screening and selection process.
3.1.2. Study Characteristics
Table 1 describes the characteristics of the included studies. The most common diagnostic reference was the DSM. Five studies [25, 40–43] received institutional review board approval before the study was conducted. Consent forms were obtained from research participants in 22 studies [25–30, 32, 34–43, 46–49, 51]. Only 4 studies [40–43] registered the protocol before the trial.
Table 1.
Summary of the studies included.
| Study (reference) |
Country | Sample size (A)/(B) | Mean age | Gender (M : F) |
Diagnostic criteria | (A) Experimental intervention | (B) Control intervention | Acupuncture points | Outcomes |
|---|---|---|---|---|---|---|---|---|---|
| Allam et al. 2008 [25] |
Egypt | 10/10 | 5.5 ± 1.22 y | (A) 7 : 3 (B) 5 : 5 |
DSM-IV ADI-R CARS ≥ 30 |
MA + (B) | Language therapy | GV20, GV26, GV17, 3 temple needles, YNSA cerebrum and aphasia points | Arabic language test |
| Chen et al. 2014 [26] |
China | 30/30 | 5.06 ± 1.32 y | 36 : 24 | CCMD-3 | MA + (B) | Cognitive behavior rehabilitation training | GV20, GV24, EX-HN3, HT7, SP6, HI3, head Anmian point | CSHQ, TER (CSHQ), PTQ |
| Fan and Li 2016 [27] |
China | 38/38 | (A) 5.21 ± 1.56 y (B) 4.98 ± 2.05 y |
(A) 22 : 16 (B) 20 : 18 |
NR | MA | Language therapy, guided education, cooperative exchanges, music therapy | Jin's three needle technique (Sishenzhen, Zhisanzhen, Naosanzhen, Niesanzhen, Shouzhizhen, Zuzhizhen, Shesanzhen, Xingshenzhen) | CARS, TER (language ability) |
| Gao 2015 [28] |
Mongolia | 50/50 | (A) 5.7 ± 0.8 y (B) 5.4 ± 0.7 y |
(A) 29 : 21 (B) 31 : 19 |
WHO | MA | Physical therapy, cognitive education, language education, behavior modification | Jin's three needle technique (Sishenzhen, Naosanzhen, Niesanzhen, Zuokeshangsanzhen, Dingshenzhen, Xingshenzhen, Shouzhizhen, Zuzhizhen, Shesanzhen) |
PEP |
| He 2006 [29] |
China | 30/30 | (A) 7.16 ± 4.26 y (B) 6.94 ± 3.86 y |
(A) 24 : 6 (B) 25 : 5 |
DSM-IV ICD-10 CCMD-2R |
EA + MA + (B) | Verbal communication training, social communication training, self-care training, cognitive training, motion training | EA (EX-HN1, EX-HN3, PC6, HT7, SP6, KI3), MA (LR3, AT3, TF4) | ABC2, CARS, ATEC |
| Li and Liu 2011 [30] |
China | 30/40 | NR | (A) 27 : 3 (B) 33 : 7 |
DSM-IV CCMD |
EA + (B) | Music therapy and structured teaching | Scalp points (Zhijiuzhen, emotional zone, heart and liver zone) | Clancy Autism Behavior Scale, CARS, ABC1, GDS |
| Li et al. 2011 [31] |
China | 19/19 | 42.75 ± 2.5 m | 36 : 2 | DSM-IV | MA + (B) | Behavioral educational intervention | Tongue points (Naozhongxue, Naoshuxue, Naoyuanxue, Bizhongxue) | PEP-revised |
| Li et al. 2015 [32] |
China | 53/53 | 5.1 ± 3.9 y | 82 : 24 | NR | MA + (B) | Intensive therapy, game therapy, sensory integration training | Jin's three needle technique (Shesanzhen, Zuzhizhen, Shouzhizhen, Xingshenzhen, Zhisanzhen, Naosanzhen, Niesanzhen, Dingshenzhen, Sishenzhen) |
CARS, ABC1 |
| Liao 2016 [33] |
China | 30/30 | (A) 9.24 ± 1.64 y (B) 9.51 ± 1.50 y |
(A) 19 : 11 (B) 18 : 12 |
NR | MA + (B) | ABA, language cognitive therapy, sensory integration training | Scalp temporal, frontal, suboccipital, occipital region | CARS, TER (CARS) |
| Liu and Yuan 2007 [34] |
China | 33/34 | 5.41 y | 60 : 7 | DSM-IV | MA | Sensory integration training | Jin's three needle technique (Sishenzhen, Niesanzhen, Zhisanzhen, Naosanzhen, Shesanzhen, Shouzhizhen, Zuzhizhen), Siguan | ABC1, CARS |
| J. G. Sun and X. R. Sun 2014 [35] |
Hong Kong | 42/42 | (A) 70 m (B) 65 m |
(A) 30 : 12 (B) 29 : 13 |
DSM-IV | EA + (B) | Behavior therapy, sensory integration training | Tongue points (Naozhongxue, Naoshuxue, Naoyuanxue, Bizhongxue) | CARS, TER (CARS) |
| Tang et al. 2013 [36] |
China | 20/18/18 | (A1) 4.526 ± 1.623 y (A2) 4.436 ± 1.520 y (B) 3.954 ± 1.572 y |
(A1) 14 : 6 (A2) 13 : 5 (B) 14 : 4 |
DSM-IV CCMD-2R CARS 36–41 |
(A1) doing (B) during retention of MA (A2) MA after (B) |
Educational training, behavior modification, sensory integration training, language therapy | Scalp areas according to symptoms | CARS, TER (CARS) |
| Wang et al. 2006 [37] |
China | 30/30 | NR | (A) 24 : 6 (B) 23 : 7 |
ICD-10 CCMD-3 |
EA + (B) | Behavior therapy | GV20, EX-HN1, GV24, GB13, EX-HN3, GV17, GB19, PC6, scalp speech areas 1, 2, 3 | Social adaptive quotient, TER (social adaptive quotient) |
| Wang et al. 2007 [38] |
China | 30/30 | (A) 5.14 ± 1.53 y (B) 5.46 ± 1.68 y |
(A) 24 : 6 (B) 23 : 7 |
ICD-10 CCMD-3 |
EA + (B) | Sensory integration training, auditory integration training, language therapy | GV20, EX-HN1, GV24, GB13, EX-HN3, GV17, GB19, PC6, scalp speech areas 1, 2, 3 | ABC1, TER (ABC1), PPVT |
| Wang et al. 2015 [39] |
China | 32/30 | (A) 5.12 ± 1.42 y (B) 5.10 ± 3.4 y |
(A) 18 : 14 (B) 15 : 15 |
NR | MA | Language therapy, guided education, ABA, music therapy | Jin's three needle technique (Sishenzhen, Zhisanzhen, Naosanzhen, Niesanzhen, Shouzhizhen, Zuzhizhen, Shesanzhen, Xingshenzhen) |
CARS, TER (language ability) |
| Wong 2008a [40] |
Hong Kong | 18/18 | (A) 7.40 ± 2.215 y (B) 7.62 ± 2.367 y |
(A) 17 : 1 (B) 17 : 1 |
DSM-IV ADI-R ADOS |
EA + MA + (B) | Conventional educational program | EA (GV20, EX-HN3, HT7, SP6), MA (AT3) | ADOS, ABC2, ATEC, RFRLRS, WeeFIM, CGI, SPT |
| Wong and Chen 2010 [41] |
Hong Kong | 30/25 | (A) 9.17 ± 4.12 y (B) 9.56 ± 4.22 y |
(A) 25 : 5 (B) 22 : 3 |
DSM-IV ADI-R ADOS |
EA, conventional educational program |
Sham EA, conventional educational program |
EX-HN1, EX-HN3, PC6, HT7, LR3, SP6, AT3, TF4 | WeeFIM, PEDI, Leiter-R, CGI, ABC2, RFRLRS, RDLS, a standardized parental report |
| Wong and Sun 2010 [42] |
Hong Kong | 25/25 | (A) 6.23 ± 1.8 y (B) 6 ± 1.99 y |
(A) 21 : 4 (B) 23 : 2 |
DSM-IV ADI-R CARS ≥ 30 |
MA, conventional educational and behavior model | Sham MA, conventional educational and behavior model | Tongue points (Runze, Guanzhu, Tianmen, Diyou) | GMDS, RFRLRS, RDLS, SPT, WeeFIM |
| Wong et al. 2014 [43] |
Hong Kong | 16/11 (12/9) |
(A) 10.167 ± 3.930 y (B) 8.750 ± 4.617 y |
(A) 16 : 0 (B) 11 : 0 |
DSM-IV ADI-R CARS ≥ 30 |
MA + (B) | Conventional educational and behavior model | Tongue points (Runze, Guanzhu, Tianmen, Diyou) | ATEC, RDLS, SPT, WeeFIM, CGI, Cerebral FDG metabolism by PET |
| Wu 2015 [44] |
China | 40/40 | (A) 6.5 ± 2.3 y (B) 6.2 ± 2.1 y |
(A) 28 : 12 (B) 30 : 10 |
DSM-5 | MA | Conventional intervention | Jin's three needle technique (NR) | Functional development scale |
| Xiong 2014 [45] |
China | 32/32 | (A) 7.48 ± 3.26 y (B) 7.56 ± 3.12 y |
(A) 18 : 14 (B) 17 : 15 |
CCMD-3 | MA + (B) | Educational training, sensory training, behavior modification, language therapy | Scalp frontal, temporal, occipital, suboccipital, parietal regions | CARS |
| Yang 2012 [46] |
China | 20/20 | (A) 5.6053 ± 2.2582 y (B) 4.2778 ± 1.8249 y |
(A) 16 : 4 (B) 14 : 6 |
DSM-IV | MA | Behavior therapy, sensory integration training | Jin's three needle technique (Sishenzhen, Dingshenzhen, Zhisanzhen, Yansanzhen, Naosanzhen, Shesanzhen, Shousanzhen, Shouzhizhen, Zusanzhen, Zuzhizhen), CV12, CV4, CV6, GV14, BL20, GV4 | CARS, TER (CARS), EEG, attention value |
| Zeng et al. 2014 [47] |
China | 30/25 | (A) 3.51 ± 1.48 y (B) 3.49 ± 1.47 y |
(A) 18 : 12 (B) 14 : 11 |
ICD-10 | MA + (B) | ABA, TEACCH, PCI, sensory integration training, auditory integration training, language cognitive therapy | Jin's three needle technique (Sishenzhen, Naosanzhen, Niesanzhen, Zhisanzhen, Shesanzhen, Dingshenzhen, Shouzhizhen, Zuzhizhen) | TER (CARS), TER (PEP) |
| Zeng et al. 2016 [48] |
China | 60/25 | (A) 3.62 ± 1.36 y (B) 3.60 ± 1.52 y |
(A) 36 : 24 (B) 16 : 9 |
ICD-10 | MA + (B) | ABA, TEACCH, PCI, sensory integration training, language cognitive therapy, music therapy | Jin's three needle technique (Naosanzhen, Niesanzhen, Zhisanzhen, Shesanzhen, Dingshenzhen, Shouzhizhen, Zuzhizhen) | TER (CARS), TER (PEP3) |
| Zhao et al. 2015 [49] |
China | 30/30 | NR | NR | ICD-10 | EA + (B) | Special education | Group 1: GV20, Sishenzhen, GV24, GB13 Group 2: ST8, GV23, Dingshenzhen, GV17, GB19; use group 1 or 2 alternately every other week |
ABC1, TER (ABC1) |
| Zhao et al. 2015 [50] |
China | 35/30 | (A) 3.5 y (B) 3.2 y |
(A) 28 : 7 (B) 25 : 5 |
DSM-IV ICD-10 |
MA + (B) | Risperidone 0.5–2 mg/d | Jin's three needle technique (Dingshenzhen, Zhisanzhen, Sishenzhen, Niesanzhen), GV17, transport point mainly pericardium, heart, or liver meridian | TER (improvement of abnormal behavior) |
| Zhen and Jin 2016 [51] |
China | 68/68 (63/65) |
(A) 4.2 y (B) 4.5 y |
(A) 56 : 12 (B) 53 : 15 |
DSM-IV | MA + (B) | Speech training and structured teaching | Jin's three needle technique (Esanzhen, Niesanzhen, Zhensanzhen), EX-HN1 | PEP-3 |
ABA, Applied Behavior Analysis; ABC1, Autism Behavior Checklist; ABC2, Aberrant Behavior Checklist; ADI-R, Autism Diagnostic Interview-Revised; ADOS, Autism Diagnostic Observation Scale; ATEC, Autism Treatment Evaluation Checklist; CARS, Childhood Autism Rating Scale; CCMD, Chinese Classification of Mental Disorder; CGI, Clinical Global Impression; CSHQ, Children's Sleep Habits Questionnaire; DSM, Diagnostic and Statistical Manual of Mental Disorders; EA, electroacupuncture; EEG, electroencephalography; FDG, fluorodeoxyglucose; GDS, Gesell Development Schedules; GMDS, Griffiths Mental Developmental Scale; ICD, International Classification of Diseases; MA, manual acupuncture; NR, not recorded; PCI, Play and Cultural Intervention; PEDI, Pediatric Evaluation of Disability Inventory; PEP, Psychoeducational Profile; PET, positron emission tomography; PPVT, Peabody Picture and Vocabulary Test; PTQ, Parent Temperament Questionnaire; RDLS, Reynell Developmental Language Scales; RFRLRS, Ritvo-Freeman Real Life Rating Scale; SPT, Symbolic Play Test; TEACCH, Treatment and Education of Autistic and Related Communication Handicapped Children; TER, Total Effective Rate; WeeFIM, Functional Independence Measure for Children; WHO, World Health Organization; YNSA, Yamamoto New Scalp Acupuncture; acrossover trial. The rest are parallel studies.
Experimental interventions involved manual acupuncture in 19 trials [25–28, 31–34, 36, 39, 42–48, 50, 51], electroacupuncture in 6 trials [30, 35, 37, 38, 41, 49], and both manual acupuncture and electroacupuncture in 2 trials [29, 40]. The most frequently used acupoints were GV20 [25, 26, 37, 38, 40, 49] and EX-HN3 [26, 29, 37, 38, 40, 41], used in six trials each. The depth of insertion ranged from 0.3 cm to 1.5 cun, and the heterogeneity was high, depending on the location of the acupoints. (Cun, a traditional Chinese unit of length, corresponds to 3.0303030 cm [52].) The most commonly used needle retention time was 30 minutes; the most frequent number of treatment sessions was 120; the most commonly used frequency and duration of acupuncture treatment were 5 times/week and 8 weeks. There was no follow-up study after treatment in any of the studies. Details of the acupuncture treatment methods used can be found in Table 2.
Table 2.
Details of acupuncture treatment methods.
| Study (reference) |
Depth of insertion | Deqi | Needle stimulation | Needle retention time | Number of treatment sessions | Frequency of treatment | Duration of treatment |
|---|---|---|---|---|---|---|---|
| Allam et al. 2008 [25] |
0.5–1 cun∗ | O | Rapid manual stimulation upon insertion and removal of the needles | 20 min | NR | Twice per week | 9 months |
| Chen et al. 2014 [26] |
NR+ | NR | Han's acupoint nerve stimulator | 30 min | NR | 5 times per week | 2 months |
| Fan and Li 2016 [27] |
NR | NR | Twirling every 30 min | Head: 1 h, others: 30 min |
20 | 5 times per week | NR |
| Gao 2015 [28] |
NR | NR | Twirling every 5 min | 45 min | NR | 6 times per week | 20 weeks |
| He 2006 [29] |
NR | NR | Electrical stimulation (10 V, wave of rarefaction) | NR | 24 | 3 times per week | 8 weeks |
| Li and Liu 2011 [30] | 0.5–1 cun | NR | Electrical stimulation (1.25 Hz, wave of condensation and rarefaction, 15 min), twirling | 2–4 h | 60 | 6 times per week | NR |
| Li et al. 2011 [31] | NR | NR | Twirling, lifting, thrusting | No retention | NR | 1–5 times per week | 6 weeks |
| Li et al. 2015 [32] |
NR | NR | Twirling every 10 min | 30 min | NR | 6 times per week | 3 months |
| Liao 2016 [33] |
10–15 mm | NR | Twirling every 30 min | 3-4 h | NR | NR | NR |
| Liu and Yuan 2007 [34] |
Head: 0.5–0.8 cun, tongue, limbs: 0.2–0.8 cun | NR | Twirling every 10 min | 30 min | 72 | 6 times per week | 12 weeks |
| J. G. Sun and X. R. Sun 2014 [35] |
NR | NR | Electrical and thermal stimulation | 20 min | NR | 3 times per day | 2 months |
| Tang et al. 2013 [36] |
10–15 mm | NR | Twirling | 6–8 h | NR | 6 times per week | 25 weeks |
| Wang et al. 2006 [37] |
GV20, EX-HN1: 0.5–0.8 cun | O | Electrical stimulation (1.25 Hz, wave of condensation and rarefaction) | 50 min | NR | 5 times per week | 4 months |
| Wang et al. 2007 [38] |
GV20: 15–20 mm, EX-HN1: 1.5–20 mm | O | Electrical stimulation (75 Hz) | 50 min | NR | 5 times per week | 4 months |
| Wang et al. 2015 [39] |
NR | NR | Twirling | Head: 1 h, limbs: 30 min | 20 | 5 times per week | NR |
| Wong 2008a [40] | GV20, EX-HN3, HT7, SP6: 13–25 mm, AT3: 5–10 mm | O | Electrical stimulation (25–75 Hz, continuous wave) | 30 min | 24 | 3 times per week | 8 weeks |
| Wong and Chen 2010 [41] |
NR | NR | Electrical stimulation | 30 min | 12 | 3 times per week | 4 weeks |
| Wong and Sun 2010 [42] |
Runze: 1 cm, Guanzhu: 0.3 cm, Tianmen: 0.5–1 cm, Diyou: 0.5 cm | NR | Quick and accurate insertion into acupoints | <15 s | 40 | 5 times per week | 8 weeks |
| Wong et al. 2014 [43] |
Runze: 1 cm, Guanzhu: 0.3 cm, Tianmen: 0.5–1 cm, Diyou: 0.5 cm | NR | Quick and accurate insertion into acupoints | <15 s | 40 | 5 times per week | 8 weeks |
| Wu 2015 [44] |
NR | NR | NR | NR | 120 | 6 times per week | NR |
| Xiong 2014 [45] |
10–15 mm | NR | Twirling every 1 h | 6–8 h | NR | NR | NR |
| Yang 2012 [46] |
Trunk: 0.1–0.3 cun, head: 0.5–0.8 cun | NR | Twirling every 20 min | 60 min, trunk: no retention | 120 | 5 times per week | NR |
| Zeng et al. 2014 [47] |
NR | NR | Twirling every 15 min | 1 h | 120 | 5 times per week | 6 months |
| Zeng et al. 2016 [48] |
Head: 15–20 mm, tongue, limbs: 5–15 mm |
O | Twirling every 15 min | 1 h | 120 | 5 times per week | 6 months |
| Zhao et al. 2015 [49] |
25 mm | NR | Electrical stimulation (1–100 Hz, continuous wave, ≤50 mA, 30 min) | 2 h | NR | 6 times per week | 3 months |
| Zhao et al. 2015 [50] |
1–1.5 cun | NR | Twirling 200 times per min for 2-3 min | Scalp: 1 h, others: no retention | NR | 6 times per week | 3 months |
| Zhen and Jin 2016 [51] |
NR | NR | Lifting and thrusting | 30 min | NR | 5 times per week | 3 months |
∗1 cun = 3.0303030 cm; +NR: not recorded. aCrossover trial. The rest are parallel studies.
As outcome measures, CARS was evaluated in 11 trials [27, 29, 30, 32–36, 39, 45, 46], ABC1 was evaluated in 5 trials [30, 32, 34, 38, 49], and ABC2 [29, 40, 41], ATEC [29, 40, 43], and RFRLRS [40–42] were each evaluated in 3 trials. Social interaction skills were assessed in 9 studies [29, 38, 40–43, 46, 48, 49], communication skills in 6 [29, 40, 41, 43, 46, 48], stereotypy in 2 [40, 41], language skills in 13 [25, 27, 28, 30, 38–43, 47–49], and cognitive function in 9 [28, 29, 31, 40–43, 47, 48], using a variety of outcome measures.
3.2. Quality Assessment
Of the 27 trials included, only 3 [25, 41, 46] used sealed or opaque envelopes and were rated as having “low risk” of bias in allocation concealment. A further 6 studies [30, 39, 48–51] were rated as “high risk” because they did not use appropriate concealment methods, and the remaining 18 studies [26–29, 31–38, 40, 42–45, 47] were evaluated as “unclear” due to lack of information. Nine studies [25, 26, 29, 36, 40–43, 46] used adequate methods of random sequence generation, using a randomization table or computer-generated randomization number. Because it is difficult to blind participants and therapists to acupuncture manipulation procedures, all studies were evaluated as “high risk” in the performance bias category. Only five trials [29, 40–43] reported the blinding of outcome assessment, and the remaining studies [25–28, 30–39, 44–51] were evaluated as “unclear” due to lack of information. Twenty studies [25–27, 29, 30, 33–40, 42, 45–50] had “low risk” of attrition bias, but five [31, 32, 41, 44, 51] were “unclear” because they did not provide statistical methods to deal with missing values. In two studies [28, 43], there were also dropouts, but they were rated “high risk” because of statistical methods using per-protocol analysis. Twenty-four studies [25–43, 45, 46, 49–51] were assessed as “low risk” in reporting bias, while two [47, 48] reported only effective rates without presenting raw data, and one [44] did not report all scheduled results. We contacted the primary authors of the studies [47, 48] to obtain the raw data via email, but did not receive the data. Except for the eight studies [25, 26, 30–34, 44] with possible baseline imbalances among participants in the experimental and control groups, the remaining studies [27–29, 35–43, 45–51] were evaluated as “low risk” in the other bias domain. Methodological assessments for each included study are presented in Figure 2.
Figure 2.
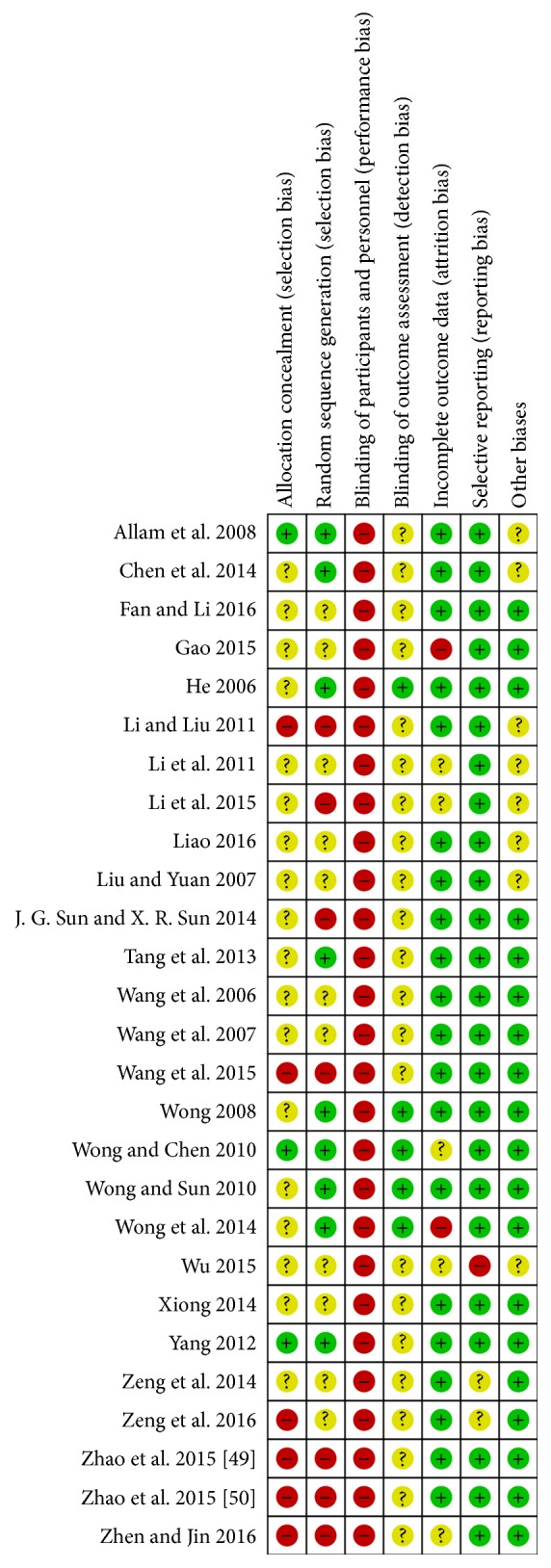
Summary of risk of bias in all included studies; “+” low risk; “?” unclear risk; “−” high risk.
3.3. Efficacy of Acupuncture as a Complementary Therapy
3.3.1. Complementary Therapy to BEI
Sixteen studies [25, 26, 29, 31–33, 35–38, 40, 43, 45, 47, 49, 51] compared acupuncture plus BEI to BEI alone.
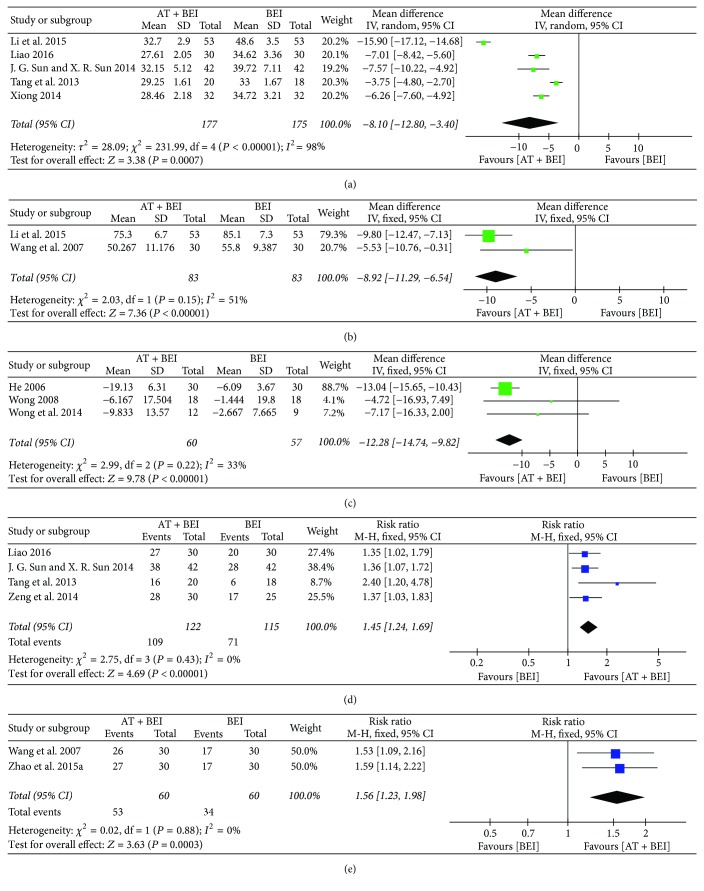
(1) Overall Scores on Scales Evaluating the Core Features of ASD. When acupuncture was added to BEI, the meta-analyses showed that reductions of the overall CARS [32, 33, 35, 36, 45], ABC1 [32, 38], and ATEC scores [29, 40, 43] were higher after treatment than for BEI alone (CARS, MD −8.10, 95% CI −12.80 to −3.40, I2 = 98%; ABC1, MD −8.92, 95% CI −11.29 to −6.54, I2 = 51%; ATEC, MD −12.28, 95% CI −14.74 to −9.82, I2 = 33%). Meta-analyses showed higher values in the acupuncture plus BEI groups than in the control groups in the studies that evaluated improvements in CARS [33, 35, 36, 47] and ABC1 [38, 49] scores using the total effective rate (TER) (CARS-TER, RR 1.45, 95% CI 1.24 to 1.69, I2 = 0%; ABC1-TER, RR 1.56, 95% CI 1.23 to 1.98, I2 = 0%) (Figure 3).
Figure 3.
Forest plots for comparison of acupuncture plus BEI versus BEI alone. (a) Overall CARS score. (b) Overall ABC 1 score. (c) Overall ATEC score. (d) TER based on CARS score. (e) TER based on ABC score. ABC1, Autism Behavior Checklist; AT, acupuncture treatment; ATEC, Autism Treatment Evaluation Checklist; BEI, behavioral and educational interventions; CARS, Childhood Autism Rating Scale; TER, total effective rate.
One study [29] found that the total ABC2 scores were improved in the acupuncture plus BEI group compared with the BEI group (P < 0.01), but in another study [40] the differences were not significant (P = 0.205). One study [29] did not present the standard deviation, thus quantitative synthesis could not be performed. In one study [40], which evaluated the overall RFRLRS score, no significant difference was found between the two groups (P = 0.752).
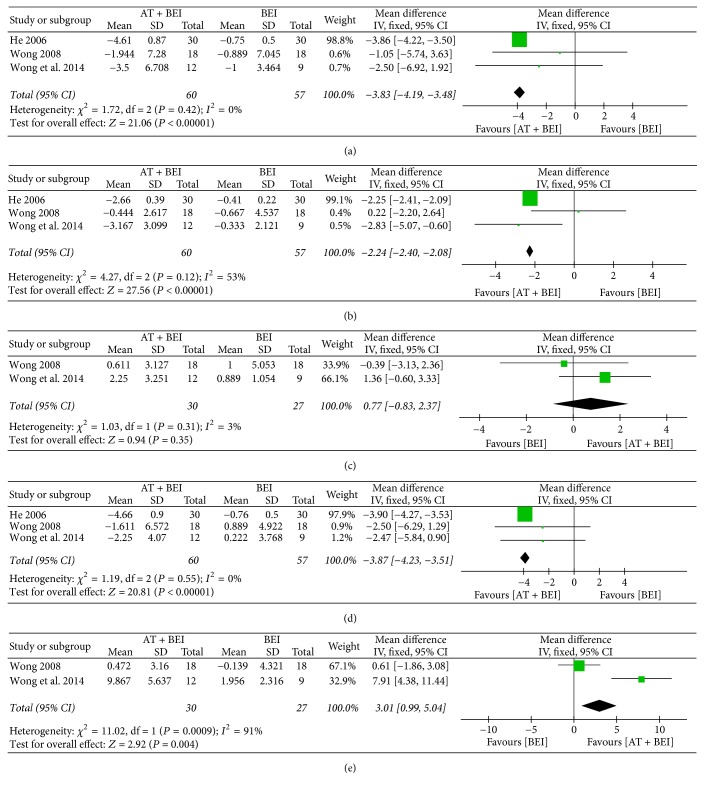
(2) Social Interaction Skills. Five studies [29, 38, 40, 43, 49] assessed social interaction skills, among which three [29, 40, 43] used a subscale of the ATEC and showed improvements when acupuncture was additionally used (MD −3.83, 95% CI −4.19 to −3.48, I2 = 0%) (Figure 4).
Figure 4.
Forest plots for comparison of acupuncture plus BEI versus BEI alone. (a) Social interaction skill (ATEC). (b) Communication ability (ATEC). (c) Language ability (SPT). (d) Cognitive function (ATEC). (e) Cognitive function (WeeFIM). AT, acupuncture treatment; ATEC, Autism Treatment Evaluation Checklist; BEI, behavioral and educational interventions; SPT, Symbolic Play Test; WeeFIM, Functional Independence Measure for Children.
Of the two studies [38, 49] that assessed social interaction skills using ABC1, Zhao et al. [49] found significant improvement in the acupuncture group compared with the controls (P = 0.019), while no such effect was found by Wang et al. [38] (P > 0.05). We could not do a meta-analysis because of considerable baseline variations between the studies. Wong [40] reported that there were no significant differences between the two groups when social interaction was assessed by a subscale of the ADOS (P = 0.987) or RFRLRS (P = 0.268).
(3) Communication Ability. Three studies [29, 40, 43] evaluated communication skills assessed with a subscale of the ATEC and reported improvements in the acupuncture plus BEI groups compared with the BEI groups (MD −2.24, 95% CI −2.40 to −2.08, I2 = 53%) (Figure 4).
There was no difference between the two groups in one study [40], in which subscales of the ABC2 and ADOS were used to assess communication skills (P = 0.183, P = 0.604; resp.).
(4) Stereotypy. There was no difference between the two groups in one study [40] in which a subscale of the ABC2 was used to assess stereotypy (P = 0.484).
(5) Language Ability. Six studies [25, 38, 40, 43, 47, 49] assessed language ability. Two studies [40, 43] evaluated it using the Symbolic Play Test (SPT), and found no significant difference (MD 0.77, 95% CI −0.83 to 2.37, I2 = 3%) (Figure 4).
Two studies [38, 49] evaluated language ability using a subscale of the ABC1, one of which [49] showed a significant improvement in the acupuncture plus BEI group compared with the controls (P < 0.05), while the other [38] did not (P > 0.05). We could not conduct a meta-analysis due to the heterogeneity of the baseline values. Zeng et al. [47] found a significant improvement in language ability in the acupuncture group compared with the controls, when assessed with TER calculated using the Psychoeducational Profile (PEP) (P < 0.05), while no significant difference was found in other studies evaluated with the Arabic language test [25], Peabody Picture Vocabulary Test [38], Reynell Developmental Language Scales (RDLS) [43], and RFRLRS [40].
(6) Cognitive Function. Five studies [29, 31, 40, 43, 47] measured cognitive function, among which three [29, 40, 43] used a subscale of the ATEC and showed significant improvements in the acupuncture plus BEI group compared with the BEI group (MD −3.87, 95% CI −4.23 to −3.51, I2 = 0%). The pooled results assessing cognitive function with the Functional Independence Measure for Children (WeeFIM) [40, 43] showed a comparative benefit of using acupuncture in conjunction with BEI (MD 3.01, 95% CI 0.99 to 5.04, I2 = 91%) (Figure 4).
Two studies [31, 47] reported greater improvements in cognitive function, evaluated by the PEP-revised and TER of the PEP, respectively, in the acupuncture plus BEI group than in the control group (P = 0.05, P = 0.02; resp.).
3.3.2. Complementary Therapy to Pharmacotherapy
One study [50] compared acupuncture plus pharmacotherapy to pharmacotherapy alone, and descriptive analysis was performed. The study showed that the addition of acupuncture to risperidone improved abnormal behaviors, including stereotypy assessed by the TER, compared with risperidone alone (P < 0.05).
3.3.3. Complementary Therapy to BEI Combined with Music Therapy
Two studies [30, 48] compared acupuncture plus a combination therapy including both BEI and music therapy, which is a form of CAM, to the combination therapy. Only descriptive analysis was performed, because of the difference in the outcome measures evaluated in the two studies.
(1) Overall Scores on Scales Evaluating the Core Features of ASD. Li and Liu [30] reported that the total CARS and ABC1 scores were lower when acupuncture was added to the combination therapy (both P < 0.01). Zeng et al. [48] reported that the TER calculated using the CARS was higher in the acupuncture group (P = 0.008).
(2) Social Interaction Skills. One study [48] reported that social interaction skills were not significantly different between the two groups, when assessed by subscales of the PEP3 (P > 0.05).
(3) Communication Ability. Zeng et al. [48] reported that communication abilities were not significantly different between the two groups, when assessed by subscales of the PEP3 (P > 0.05).
(4) Language Ability. Both studies measured language ability, using either a subscale of the PEP3 [48] or the Gesell Developmental Schedules [30], and both showed a significant improvement in the acupuncture group compared to the control group (P < 0.05, P < 0.01; resp.).
(5) Cognitive Function. One study [48] reported that cognitive function was higher in the acupuncture group compared with the control group, when assessed by subscales of the PEP3 (P = 0.0005).
3.4. Efficacy of Acupuncture as an Alternative Therapy
3.4.1. Alternative Therapy to BEI
Four studies [28, 34, 44, 46] compared acupuncture with BEI.
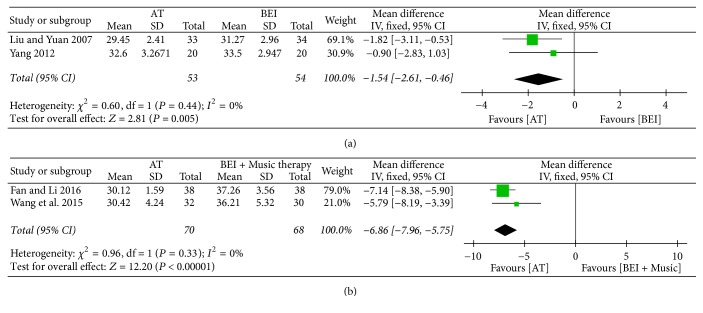
(1) Overall Scores on Scales Evaluating the Core Features of ASD. Two studies [34, 46] found greater improvement in the overall CARS score after treatment in the acupuncture group than in the BEI group (MD −1.54, 95% CI −2.61 to −0.46, I2 = 0%) (Figure 5).
Figure 5.
Forest plots for the outcome “overall CARS score”. (a) Acupuncture versus BEI. (b) Acupuncture versus BEI and music therapy. AT, acupuncture treatment; BEI, behavioral and educational interventions; CARS, Childhood Autism Rating Scale.
The ABC1 [34], and the TER calculated with the CARS [46], also showed a significant improvement in the acupuncture group compared to the control group (both P < 0.05).
(2) Social Interaction Skills. Yang [46] measured social interaction skills using a subscale of the CARS but found no significant difference between the two groups (P > 0.05).
(3) Communication Ability. Yang [46] evaluated communication skills using subscales of the CARS. There were no significant differences in nonverbal communication abilities between the two groups (P > 0.05), but verbal communication abilities were significantly different in favour of the acupuncture group (P < 0.05).
(4) Language Ability. Gao [28] reported that language ability was significantly improved in the acupuncture group compared with the BEI group (P < 0.05), when measured by a subscale of the PEP.
(5) Cognitive Function. In one study [28], there was no difference between interventions when cognitive function was evaluated by a subscale of the PEP (P > 0.05).
3.4.2. Alternative Therapy to BEI Combined with Music Therapy
Two studies [27, 39] compared acupuncture with a combination therapy consisting of both BEI and music therapy. Both studies showed improved total CARS scores in the acupuncture group compared with the control group, after treatment (MD −6.86, 95% CI −7.96 to −5.75, I2 = 0%) (Figure 5).
3.5. Acupuncture versus Sham Acupuncture
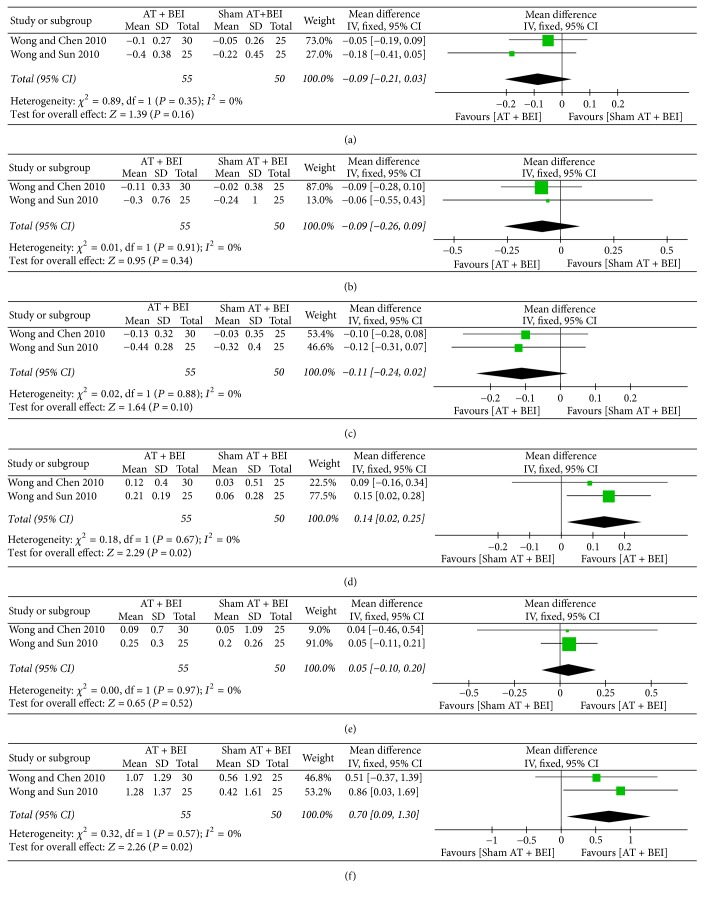
Two studies [41, 42] compared acupuncture plus BEI with sham acupuncture plus BEI.
(1) Overall Scores on Scales Evaluating the Core Features of ASD. Both studies [41, 42] measured the total RFRLRS scores, which showed no significant differences between the two groups (MD −0.09, 95% CI −0.21 to 0.03, I2 = 0%) (Figure 6).
Figure 6.
Forest plots for comparison of acupuncture versus sham acupuncture. (a) Overall RFRLRS score. (b) Social interaction skill (RFRLRS). (c) Language ability (RFRLRS). (d) Language ability-comprehension age (RDLS). (e) Language ability-expression age (RDLS). (f) Cognitive function (WeeFIM). AT, acupuncture treatment; BEI, behavioral and educational interventions; RDLS, Reynell Developmental Language Scales; RFRLRS, Ritvo-Freeman Real Life Rating Scale; WeeFIM, Functional Independence Measure for Children.
(2) Social Interaction Skills. Social interaction skills were assessed using a subscale of the RFRLRS [41, 42] and the Pediatric Evaluation of Disability Inventory (PEDI) [41], but there were no significant differences between the groups (RFRLRS, MD −0.09, 95% CI −0.26 to 0.09, I2 = 0%; PEDI, P = 0.959) (Figure 6).
(3) Communication Ability. One study [41] reported that there was no difference between the two groups when assessing communication ability using subscales of the ABC2 (P = 0.849).
(4) Stereotypy. One study [41] evaluated stereotypy using subscales of the ABC2 and found no difference between the two groups (P = 0.629).
(5) Language Ability. There were no significant differences in language abilities between the two groups when evaluated using subscales of the RFRLRS [41, 42], RDLS [41, 42], and SPT [42] (RFRLRS, MD −0.11, 95% CI −0.24 to 0.02, I2 = 0%; RDLS-comprehension age, MD 0.14, 95% CI 0.02 to 0.25, I2 = 0%; RDLS-expression age, MD 0.05, 95% CI −0.10 to 0.20, I2 = 0%; SPT, P = 0.092) (Figure 6).
(6) Cognitive Function. Both studies [41, 42] measured cognitive function using a subscale of the WeeFIM, which showed differences in favour of the acupuncture group (MD 0.70, 95% CI 0.09 to 1.30, I2 = 0%) (Figure 6).
3.6. Other Effects of Acupuncture in ASD
In addition to the above-mentioned outcome measures, acupuncture has other potential effects on ASD. First, acupuncture might improve social adaptation. Li and Liu [30] found that participants who received acupuncture showed improved ability for social adaptation, as measured by the Gesell Developmental Schedules, compared to those who did not receive acupuncture (P < 0.01). Wang et al. [37] found that the social adaptive quotient and TER calculated were higher when acupuncture was added to BEI than for BEI alone (both P < 0.05).
Second, acupuncture might improve sleeping habits. In a study that evaluated the TER using the Children's Sleep Habits Questionnaire [26], the rate for the acupuncture plus BEI group was higher than that of the BEI-alone group (P = 0.001).
3.7. Safety
Six RCTs with 306 participants [35, 40–43, 49] provided data on adverse events associated with acupuncture (Table 3). Four trials [35, 42, 43, 49] reported that no adverse events occurred during the interventions. Wong and Chen [41] reported that some participants experienced minor superficial bleeding, crying, or irritability during acupuncture. Another study [40] reported one case of a worsening sleep pattern and one case of increased hyperactivity and ritualistic behavior.
Table 3.
Adverse events in included studies.
| Study (reference) | Sample size (E/C) |
Adverse events |
|---|---|---|
| J. G. Sun and X. R. Sun 2014 [35] |
42/42 | None |
| Wong 2008 [40] |
18/18 | E: 1 (worsening of sleep pattern; sleeping late at night), 1 (worsening of hyperactivity and ritualistic behavior) Parents thought that the negative changes were minor and did not affect the participant's functioning |
| Wong and Chen 2010 [41] |
30/25 | E: minor superficial bleeding or crying, and irritability during acupuncture was experienced by some |
| Wong and Sun 2010 [42] |
25/25 | None. Initial crying in fear and possible minor pain occurred in the first few sessions, but patients adapted easily and tolerated the procedure well |
| Wong et al. 2014 [43] |
12/9 | None. Initial crying in fear and possible minor pain occurred in first few sessions, but patients adapted easily and tolerated the procedure well |
| Zhao et al. 2015 [49] |
30/30 | None |
C, control group; E, experimental group.
4. Discussion
In the present study, we conducted a systematic review of 27 RCTs with 1736 participants, to evaluate the efficacy of acupuncture for children with ASD. The outcome assessment of our review was summarized in two aspects: improvement of overall symptoms of ASD (evaluated with the overall scores on scales such as CARS, ABC1, ABC2, ATEC, and RFRLRS, which are specific outcome measures for ASD) and improvement in each of the major symptom categories of ASD (including social interaction skills, communication ability, stereotypy, language ability, and cognitive function).
When acupuncture was added to BEI, our pooled results indicated that reductions in the overall scores on the CARS, ABC1, and ATEC, and TERs based on the overall scores on the CARS and ABC1, were significantly higher compared with the BEI-alone group. Acupuncture was not demonstrably effective in reducing the overall ABC2 and RFRLRS scores as an adjunctive therapy, but the results were unreliable because only a very small number of studies evaluated this. As a complementary therapy for BEI, acupuncture therapy provided inconsistent results in improving the individual symptoms of ASD. This may have been a result of evaluating each symptom using nonspecific scales for ASD, such as the SPT or WeeFIM. There were many studies that evaluated the total scores on ASD-specific outcome measures, but the scores on the subscales that evaluated each individual ASD symptom were rarely presented. Therefore, the number of studies evaluating each major symptom of ASD was insufficient for assessing statistical validity. The effect of acupuncture as a complementary therapy alongside pharmacotherapy, or as an adjunctive therapy to music therapy combined with BEI, could not be assessed because there were only one or two studies available.
When acupuncture was used as an alternative therapy for BEI, or for BEI plus music therapy, the total CARS scores of the acupuncture group showed greater improvement than those of the control groups. There was only one study evaluating the efficacy of acupuncture for each of the ASD symptoms, such as social interaction skills, communication ability, language ability, and cognitive function. Therefore, the results concerning the efficacy of acupuncture as a monotherapy for each symptom of ASD should be interpreted with caution.
Our review found that acupuncture had no significantly different effect on any outcome compared to sham acupuncture. In addition, while the results indicate that acupuncture might improve social adaptability and sleeping habits, these results cannot be confirmed because of the limited number of studies.
According to TCM's holistic approach, stimulating the acupoints related to various organs or viscera of the human body through meridians corrects the disharmony and dysregulation of organ systems. In TCM, the pathogenesis of ASD is considered to be related to disharmony of the five viscera, six bowels, and meridians, mainly dysregulation of the heart, liver, spleen, kidney, and brain [15]. Dysregulation and disharmony of the organs associated with ASD may have been corrected through acupuncture treatment, and this may have resulted in an improvement in overall scores on ASD-specific outcome measures, such as the CARS and ABC1. On a scientific basis, the pathogenesis of ASD is incompletely understood. Acupuncture can modulate neurotrophic factors [19] and neurotransmitter systems such as serotonin [53], GABA [17], and glutamate [16], which are considered strong candidates for roles in ASD [18], and this could lead to improvement in the symptoms of ASD. Further investigations should be conducted to clarify the specific mechanisms of acupuncture in treating ASD, and to examine which core symptoms of ASD can be improved by acupuncture.
We did not find strong evidence to show that acupuncture is associated with any serious adverse events. However, only six RCTs (22.22%) reported acupuncture safety data. Therefore, we could not draw a firm conclusion about the safety of acupuncture for ASD.
Two systematic reviews regarding acupuncture for ASD [20, 21] have been published during the last few years. Compared with the previous systematic reviews [20, 21], which included 10 and 11 articles, respectively, our review included many additional published RCTs. In other words, by including 27 RCTs and 1736 participants, this is the most comprehensive and recent review of acupuncture for patients with pediatric ASD. Unlike previous studies, which referred to the treatment used in the control group as “conventional treatment,” we analyzed the interventions used in the controls by classifying them as pharmacological interventions, BEI, and CAM. We could confirm that acupuncture as a complementary therapy improved the total CARS and ABC1 scores, which are tools for measuring the key symptoms of ASD, but could not specifically determine the symptoms that improved. The total CARS scores before and after treatment were reported in ten studies [27, 30, 32–36, 39, 45, 46], but there was only one study [46] that showed the scores on subscales evaluating each symptom. Meanwhile, we did not find much improvement in the low methodological quality of the included studies. Furthermore, owing to the heterogeneity of the acupuncture methods used in each study, we could not draw any other conclusions.
4.1. Limitations
This review has several limitations, and each should be considered seriously. First, we found that significant heterogeneity existed for several of the outcomes. This may have been caused by the heterogeneity of the recruited participants with ASD, as ASD comprises a range of symptoms and associated problems. Moreover, unlike other clinical trials, acupuncture clinical trials involve various factors that cause heterogeneity, such as selection of acupoints, frequency and duration of treatments, depths of insertion, and needle retention times. Although the treatments used in the control groups were classified in this review as pharmacological interventions, BEI, or CAM, the variety of BEI treatments may have caused heterogeneity. Second, the low methodological quality of some studies remains a challenge. Many studies showed performance bias, because acupuncture therapy is difficult to blind. The low methodological quality of some studies can lead to overestimation of the effects of acupuncture on ASD. Additionally, although we searched the literature regardless of language, most of the included studies were conducted in China (74.07%), which suggests a potential for location bias and limits the generality of this review. We intended to estimate publication bias with a funnel plot, but none of the outcome measures were used in more than 10 studies. Accordingly, we could not assess publication bias in this review.
4.2. Implications for Future Research
After the publication of the DSM-5 in 2013 [1], a single diagnosis of “ASD” has replaced previous subtypes. ASD is a highly heterogeneous disorder that involves various symptoms. Therefore, it is necessary to identify the subgroups of ASD children that can benefit from acupuncture. To resolve this in detail, subscales as well as total scores on the indicators evaluating ASD, such as the CARS, ABC1, and ABC2, should be measured and presented to distinguish the symptoms that might be improved by acupuncture. Only four of the studies included in this review [25, 36, 42, 43] used CARS scores as diagnostic criteria to specify the severity of the symptoms. In future studies, the severity of ASD should be specified in participants via appropriate inclusion criteria.
Since there were variations in the types of acupuncture used, and a lack of standardization in the selection of acupoints, future research must standardize and generalize acupuncture treatment for ASD. In the studies included in this review, GV20 and EX-HN3 were frequently used. The most frequent needle retention time was 30 minutes, the number of treatment sessions was 120, the frequency of treatment was 5 times/week, and the duration of treatment was 8 weeks. To accumulate evidence, we should select specific acupuncture treatment methods based on existing studies. Additionally, the included studies did not conduct follow-ups after the treatment ended. We suggest long-term clinical trials with longer follow-up periods that include serial measurements of outcomes to determine the effects of acupuncture over time.
To improve the methodological quality, a strict protocol should be planned prior to future trials. Moreover, we expect rigorous, well-designed clinical trials in full compliance with the Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA) recommendations [54]. In this review, only six studies reported adverse events related to acupuncture, and all events were mild. To draw clear conclusions about the safety of acupuncture for pediatric ASD, future studies should measure and report all adverse events using guidelines such as the CONSORT for Harms Data Recommendations [55]. Moreover, parents of children with ASD experience considerable levels of stress [56]; therefore, we suggest that the quality of life of parents of children with ASD should be considered as an additional important outcome measure in future clinical trials.
5. Conclusion
The results of this systematic review indicated that acupuncture may improve the overall symptoms of ASD. The reported adverse events associated with acupuncture were mild and acceptable. However, due to heterogeneities among the trials and the low methodological quality of some of the studies, additional rigorous, well-designed RCTs with larger sample sizes should be performed to confirm these results.
Acknowledgments
This study was supported by the Traditional Korean Medicine R&D program funded by the Ministry of Health & Welfare through the Korea Health Industry Development Institute (KHIDI) (no. HB16C0075).
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this article.
Authors' Contributions
All authors were responsible for the study concept and design: Boram Lee and Jihong Lee participated in the literature search; Boram Lee, Jihong Lee, Jin-Hong Cheon, Hyun-Kyung Sung, and Seung-Hun Cho were responsible for the analysis and interpretation of the data; Boram Lee drafted the paper; Gyu Tae Chang supervised the study and critically reviewed the paper; all authors approved the final paper.
Supplementary Materials
Supplementary Material includes the search terms for each database described in Methods. Supplement 1: search strategy used in all databases.
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th. Arlington, Va, USA: American Psychiatric Association; 2013. (DSM-5). [DOI] [Google Scholar]
- 2.Fombonne E. Epidemiology of pervasive developmental disorders. Pediatric Research. 2009;65(6):591–598. doi: 10.1203/pdr.0b013e31819e7203. [DOI] [PubMed] [Google Scholar]
- 3.Zablotsky B., Black L. I., Maenner M. J., Schieve L. A., Blumberg S. J. Estimated Prevalence of Autism and Other Developmental Disabilities Following Questionnaire Changes in the 2014 National Health Interview Survey. National Health Statistics Reports. 2015;(87):1–20. [PubMed] [Google Scholar]
- 4.McVoy M., Findling R. Child and Adolescent Psychopharmacology Update. Psychiatric Clinics of North America. 2009;32(1):111–133. doi: 10.1016/j.psc.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 5.McCracken J. T., McGough J., Shah B., et al. Risperidone in children with autism and serious behavioral problems. The New England Journal of Medicine. 2002;347(5):314–321. doi: 10.1056/nejmoa013171. [DOI] [PubMed] [Google Scholar]
- 6.Howlin P., Magiati I., Charman T. Systematic review of early intensive behavioral interventions for children with autism. American Journal on Intellectual and Developmental Disabilities. 2009;114(1):23–41. doi: 10.1352/2009.114:23-41. [DOI] [PubMed] [Google Scholar]
- 7.Virués-Ortega J. Applied behavior analytic intervention for autism in early childhood: meta-analysis, meta-regression and dose-response meta-analysis of multiple outcomes. Clinical Psychology Review. 2010;30(4):387–399. doi: 10.1016/j.cpr.2010.01.008. [DOI] [PubMed] [Google Scholar]
- 8.Spreckley M., Boyd R. Efficacy of applied behavioral intervention in preschool children with autism for improving cognitive, language, and adaptive behavior: a systematic review and meta-analysis. Journal of Pediatrics. 2009;154(3):338–344. doi: 10.1016/j.jpeds.2008.09.012. [DOI] [PubMed] [Google Scholar]
- 9.NCCIH Publication No. D347. Complementary, Alternative, or Integrative Health: What’s In a Name? 2016, https://nccih.nih.gov/health/integrative-health.
- 10.Owen-Smith A. A., Bent S., Lynch F. L., et al. Prevalence and predictors of complementary and alternative medicine use in a large insured sample of children with Autism Spectrum Disorders. Research in Autism Spectrum Disorders. 2015;17:40–51. doi: 10.1016/j.rasd.2015.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Klein N., Kemper K. J. Integrative approaches to caring for children with autism. Current Problems in Pediatric and Adolescent Health Care. 2016;46(6):195–201. doi: 10.1016/j.cppeds.2015.12.004. [DOI] [PubMed] [Google Scholar]
- 12.Hanson E., Kalish L. A., Bunce E., et al. Use of complementary and alternative medicine among children diagnosed with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2007;37(4):628–636. doi: 10.1007/s10803-006-0192-0. [DOI] [PubMed] [Google Scholar]
- 13.Tindle H. A., Davis R. B., Phillips R. S., Eisenberg D. M. Trends in use of complementary and alternative medicine by us adults: 1997–2002. Alternative Therapies in Health and Medicine. 2015;11(1):42–49. [PubMed] [Google Scholar]
- 14.Zhang Y., Xing J. J., Li J., Zeng B. Y., Liang F. R. International Review of Neurobiology. chapter 1. Vol. 111. Elsevier; 2013. History of acupuncture research; pp. 1–23. [DOI] [PubMed] [Google Scholar]
- 15.Chen W.-X., Wu-Li L., Wong V. C. N. Electroacupuncture for children with autism spectrum disorder: Pilot study of 2 cases. The Journal of Alternative and Complementary Medicine. 2008;14(8):1057–1065. doi: 10.1089/acm.2007.0823. [DOI] [PubMed] [Google Scholar]
- 16.Lee G. J., Yin C. S., Choi S. K., Yang J. S., Lee H., Park H. K. Acupuncture attenuates extracellular glutamate level in global ischemia model of rat. Neurological Research. 2010;32(supplement 1):79–83. doi: 10.1179/016164109X12537002794200. [DOI] [PubMed] [Google Scholar]
- 17.Xu Q., Yang J.-W., Cao Y., et al. Acupuncture improves locomotor function by enhancing GABA receptor expression in transient focal cerebral ischemia rats. Neuroscience Letters. 2015;588:88–94. doi: 10.1016/j.neulet.2014.12.057. [DOI] [PubMed] [Google Scholar]
- 18.Toma C., Hervás A., Balmaña N., et al. Neurotransmitter systems and neurotrophic factors in autism: Association study of 37 genes suggests involvement of DDC. The World Journal of Biological Psychiatry. 2013;14(7):516–527. doi: 10.3109/15622975.2011.602719. [DOI] [PubMed] [Google Scholar]
- 19.Li L. Y., Jiang N., Zhao Y. Could acupuncture have a role in the treatment of autism spectrum disorder via modulation of BDNF expression and activation? Acupuncture in Medicine. 2014;32(6):503–505. doi: 10.1136/acupmed-2014-010602. [DOI] [PubMed] [Google Scholar]
- 20.Cheuk D. K., Wong V., Chen W. X. Acupuncture for autism spectrum disorders (ASD) The Cochrane Database of Systematic Reviews. 2011;(9) doi: 10.1002/14651858.CD007849.pub2.CD007849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee M. S., Choi T.-Y., Shin B.-C., Ernst E. Acupuncture for children with autism spectrum disorders: a systematic review of randomized clinical trials. Journal of Autism and Developmental Disorders. 2012;42(8):1671–1683. doi: 10.1007/s10803-011-1409-4. [DOI] [PubMed] [Google Scholar]
- 22.Higgins J. P. T., Green S. Cochrane handbook for systematic reviews of interventions. version 5.1.0, 2011.
- 23.Moher D., Liberati A., Tetzlaff J., Altman D. G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Medicine. 2009;6(7) doi: 10.1371/journal.pmed.1000097.e1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Borenstein M., Hedges L. V., Higgins J. P. T., Rothstein H. R. A basic introduction to fixed- effect and random-effects models for meta-analysis. Research Synthesis Methods. 2010;1(2):97–111. doi: 10.1002/jrsm.12. [DOI] [PubMed] [Google Scholar]
- 25.Allam H., Eldine N. G., Helmy G. Scalp acupuncture effect on language development in children with autism: a pilot study. The Journal of Alternative and Complementary Medicine. 2008;14(2):109–114. doi: 10.1089/acm.2007.0508. [DOI] [PubMed] [Google Scholar]
- 26.Chen S. Q., Fang J. Q., Wang Y., et al. Clinical observation of Han's acupoint nerve stimulator (HANS) in the treatment of somnipathy of autistic children. Medical Innovation of China. 2014;11(15):124–127. [Google Scholar]
- 27.Fan J., Li M. Efficacy observation of Jin's three needling therapy on autism children with language development disorders. Bao Jian Wen Hui. 2016;3(5):p. 79. [Google Scholar]
- 28.Gao X. Clinical curative effect observation of Jin's three needling therapy for 50 cases of children with autism. Journal of the Chinese Medical Association. 2015;31(31):75–77. [Google Scholar]
- 29.He J. Theoretical and clinical study on treatment of autism with acupuncture. Hunan University of Chinese Medicine; 2006. [Google Scholar]
- 30.Li N., Liu Z. Clinical study on activating brain and opening orifices scalp acupuncture therapy in the treatment of children with autism. Proceedings of the The 5th Beijing International Rehabilitation Forum; 2011; pp. 382–387. [Google Scholar]
- 31.Li L., Jiao Y., Liu L.-Y., Huang C. Analysis of the effect that tongue acupuncture combining with comprehensive intervention to children with autism. Chinese Journal of Child Health Care. 2011;19(5):477–479. [Google Scholar]
- 32.Li T., Li H., Zhao Y. Clinical evaluation of acupuncture treatment for children with autism. Chinese Journal of Modern Drug Application. 2015;9(16):260–261. [Google Scholar]
- 33.Liao J. Clinical analysis of scalp acupuncture combined with rehabilitation training in the treatment of children with autism spectrum disorder. China Practical Medicine. 2016;11(22):268–269. [Google Scholar]
- 34.Liu G., Yuan L. X. Clinical observe of acupuncture treat autism. Chinese Archives of Traditional Chinese Medicine. 2007;25(12):2497–2498. [Google Scholar]
- 35.Sun J. G., Sun X. R. Encephalopathy therapeutic tongue acupoint apparatus (ETTAA) for 42 cases of autism. Chinese acupuncture & moxibustion. 2014;34(1):96–98. [PubMed] [Google Scholar]
- 36.Tang Q., Zhang C., Wang Y., Xiang D., Zhang Y. Clinical observation on treatment of moderate autistic children with combination of scalp point needling and rehabilitation training. Chinese Journal of Rehabilitation Medicine. 2013;28(3):251–253. [Google Scholar]
- 37.Wang C. N., Shang S. Y., Wei X. H. The influence of electroacupuncture plus behavior therapy on social adaptive behavior ability in autism children. Shanghai Journal of Acupuncture and Moxibustion. 2006;25(12):p. pp. [Google Scholar]
- 38.Wang C. N., Liu Y., Wei X. H., Li L. X. Effects of electroacupuncture combined with behavior therapy on intelligence and behavior of children of autism. Chinese acupuncture & moxibustion. 2007;27(9):660–662. [PubMed] [Google Scholar]
- 39.Wang J., Li J., Mei X. Observation and treatment of children with autism language development disorders efficacy Jin three-needle. China Continuing Medical Education. 2015;7(22):159–160. [Google Scholar]
- 40.Wong C. L. Acupuncture and autism spectrum disorders: an assessor-blinded randomized controlled trial. Hong Kong University of Philosophy; 2008. [Google Scholar]
- 41.Wong V. C. N., Chen W. X. Randomized controlled trial of electro-acupuncture for autism spectrum disorder. Alternative Medicine Review. 2010;15(2):136–146. [PubMed] [Google Scholar]
- 42.Wong V. C. N., Sun J. G. Randomized controlled trial of acupuncture versus sham acupuncture in autism spectrum disorder. The Journal of Alternative and Complementary Medicine. 2010;16(5):545–553. doi: 10.1089/acm.2007.0768. [DOI] [PubMed] [Google Scholar]
- 43.Wong V. C., Sun J., Yeung D. W. Randomized control trial of using tongue acupuncture in autism spectrum disorder. Journal of Traditional Chinese Medical Sciences. 2014;1(1):62–72. doi: 10.1016/j.jtcms.2014.11.005. [DOI] [Google Scholar]
- 44.Wu S. Observation of the clinical effect of acupuncture treatment of 80 cases of children with autism. China Health Standard Management. 2015;6(10):p. 246. [Google Scholar]
- 45.Xiong Y. Clinical observation of head acupuncture combined with rehabilitation training in the treatment of moderate autism. Asia-Pacific Traditional Medicine. 2014;10(6):95–96. [Google Scholar]
- 46.Yang Y. The clinical research on autism children with treatment of acupuncture on TiaoRentongDu theory. Guangzhou University of Chinese Medicine; 2012. [Google Scholar]
- 47.Zeng H., Chen S., Yang X., Huang X., Zeng X., Luo Q. Clinical observation on 30 cases of pediatric autism co-treated with Jin triple-needle therapy. Journal of Pediatrics of Traditional Chinese Medicine. 2014;10(2):47–50. [Google Scholar]
- 48.Zeng H., Huang X., Yang X., et al. Clinical study of Jin triple-needle therapy combined with rehabilitation training on childhood autism. Journal of Pediatrics of Traditional Chinese Medicine. 2016;12(5):69–75. [Google Scholar]
- 49.Zhao N. X., Gao F., Jiao W. T., et al. Clinical study of the intervention on abnormal behavior in the children with autism treated with head electroacupuncture and special education. World Journal of Integrated Traditional and Western Medicine. 2015;10(8):1104–1107. [Google Scholar]
- 50.Zhao N., Zhang N., Jiao W., Gao F. Observations on the efficacy of acupuncture plus Risperidone in improving the abnormal behavior of autistic children. Shaanxi Journal of Traditional Chinese Medicine. 2015;36(8):1070–1071. [Google Scholar]
- 51.Zhen F., Jin Y. Clinical efficacy of scalp acupuncture therapy in rehabilitating the language barrier in children with autism. Journal of Pediatrics of Traditional Chinese Medicine. 2016;12(3):68–70. [Google Scholar]
- 52.Korea Research Institute of Standards and Science. The International System of Units (SI) conversion. http://www.kriss.re.kr/standard/view.do?pg=explanation_tab_06.
- 53.Cabyoglu M. T., Ergene N., Tan U. The mechanism of acupuncture and clinical applications. International Journal of Neuroscience. 2006;116(2):115–125. doi: 10.1080/00207450500341472. [DOI] [PubMed] [Google Scholar]
- 54.Macpherson H., Altman D. G., Hammerschlag R., et al. Revised Standards for reporting interventions in clinical trials of acupuncture (STRICTA): Extending the CONSORT Statement. Acupuncture and Related Therapies. 2015;3(4):35–46. [Google Scholar]
- 55.Ioannidis J. P. A., Evans S. J. W., Gøtzsche P. C., et al. Better reporting of harms in randomized trials: an extension of the CONSORT statement. Annals of Internal Medicine. 2004;141(10):781–788. doi: 10.7326/0003-4819-141-10-200411160-00009. [DOI] [PubMed] [Google Scholar]
- 56.Davis N. O., Carter A. S. Parenting stress in mothers and fathers of toddlers with autism spectrum disorders: associations with child characteristics. Journal of Autism and Developmental Disorders. 2008;38(7):1278–1291. doi: 10.1007/s10803-007-0512-z. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material includes the search terms for each database described in Methods. Supplement 1: search strategy used in all databases.