Key Points
Question
Does use of a cervical pessary reduce the rate of spontaneous delivery before 34 weeks of gestation among women with singleton pregnancies, short cervical length, and no prior spontaneous preterm birth?
Findings
In this randomized trial of 300 women, the rates of spontaneous preterm birth at less than 34 weeks were 7.3% with a cervical pessary compared with 15.3% without cervical pessary use, a significant difference.
Meaning
The use of a cervical pessary among women with singleton pregnancies, short cervical length, and no prior spontaneous preterm birth reduced the risk of spontaneous preterm birth at less than 34 weeks of gestation.
Abstract
Importance
Spontaneous preterm birth is a major cause of perinatal morbidity and mortality. It is unclear if a cervical pessary can reduce the risk of spontaneous preterm delivery.
Objective
To test whether in asymptomatic women with singleton pregnancies and no prior spontaneous preterm birth but with short cervical length on transvaginal ultrasound, use of a cervical pessary would reduce the rate of spontaneous preterm birth at less than 34 weeks of gestation.
Design, Setting, and Participants
Parallel-group, nonblinded, randomized clinical trial conducted from March 1, 2016, to May 25, 2017, at a single center in Italy. Asymptomatic women with singleton gestations, no previous spontaneous preterm births, and cervical lengths of 25 mm or less at 18 weeks 0 days to 23 weeks 6 days of gestation were eligible.
Interventions
Patients were randomized 1:1 to receive either cervical pessary (n = 150) or no pessary (n = 150). The pessary was removed between 37 weeks 0 days and 37 weeks 6 days of gestation or earlier if clinically indicated. The control group received standard care. For cervical length of 20 mm or shorter, women in both groups were prescribed vaginal progesterone, 200 mg/d, until 36 weeks 6 days of gestation. No bed rest or activity restriction was recommended.
Main Outcomes and Measures
The primary end point was spontaneous preterm birth at less than 34 weeks of gestation. Secondary outcomes were adverse events.
Results
Among 300 women who were randomized (mean age, 29 [SD, 6.3] years; mean gestational age, 22 [SD, 1.3] weeks), 100% completed the trial. The primary end point occurred in 11 women (7.3%) in the pessary group and 23 women (15.3%) in the control group (between-group difference, −8.0% [95% CI, −15.7% to −0.4]; relative risk, 0.48 [95% CI, 0.24-0.95]). During follow-up, the pessary group had a higher rate of increased or new vaginal discharge (86.7% vs 46.0%; between-group difference, +40.7% [95% CI, +30.1%-+50.3%]; relative risk, 1.88 [95% CI, 1.57-2.27]).
Results
Among 300 women who were randomized (mean age, 29 [SD, 6.3] years; mean gestational age, 22 [SD, 1.3] weeks), 100% completed the trial. The primary end point occurred in significantly fewer women in the pessary group. During follow-up, the pessary group had a higher rate of increased or new vaginal discharge.
| No. (%) | Between-Group Difference, % (95% CI) |
Relative Risk (95% CI) | ||
|---|---|---|---|---|
| Pessary Group (n = 150) |
Control Group (n = 150) |
|||
| Primary outcome | ||||
| Spontaneous preterm birth <34 wk | 11 (7.3) | 23 (15.3) | −8.0 (−15.7 to −0.4) | 0.48 (0.24-0.95) |
| Adverse events | ||||
| Vaginal discharge | 130 (86.7) | 69 (46.0) | 40.7 (30.1 to 50.3) | 1.88 (1.57-2.27) |
Conclusions and Relevance
Among women without prior spontaneous preterm birth who had asymptomatic singleton pregnancies and short transvaginal cervical length, use of a cervical pessary, compared with no pessary use, resulted in a lower rate of spontaneous preterm birth at less than 34 weeks of gestation. The results of this single-center, nonblinded study among selected pregnant women require confirmation in multicenter clinical trials.
Trial Registration
clinicaltrials.gov Identifier: NCT02716909
This randomized clinical trial compares the effect of use of a cervival pessary vs usual care on risk of spontaneous preterm birth among women with singleton pregnancies without prior spontaneous preterm birth but with short cervical length.
Introduction
Preterm birth, defined as delivery before 37 weeks of gestation, is a major cause of perinatal morbidity and mortality.1 About 15 million infants were born prematurely in 2015, causing 1.1 million deaths as well as short- and long-term disability in the survivors.2,3
Different strategies have been adopted for prevention of spontaneous preterm birth. The evidence supports use of vaginal progesterone in women with singleton pregnancy with a short cervix,4,5 while cervical cerclage seems to be beneficial only in the subgroup of singleton pregnancies with both prior spontaneous preterm birth and cervical length of 25 mm or less6 and not in women without prior spontaneous preterm birth,7 nor in women with multiple gestations.8 International guidelines recommend cervical cerclage for such high-risk women.4
The cervical pessary is a silicone device that has been used to prevent spontaneous preterm birth.9,10,11,12,13,14 The leading hypotheses for its mechanism of action are that the pessary helps keep the cervix closed and changes the inclination of the cervical canal so that the pregnancy weight is not directly above the internal os. The 4 randomized clinical trials (RCTs) in women with singleton pregnancy with a short cervix published so far provided contradictory results,9,10,11,12 and a meta-analysis by Saccone et al13 concluded that in this subset of women, the cervical pessary does not reduce the rate of spontaneous preterm delivery or improve perinatal outcome. However, clinical heterogeneity within the trials was high, and the studies included women both with and without prior preterm birth.13
The hypothesis of this trial was that in asymptomatic women with singleton pregnancy without prior spontaneous preterm birth but with short cervical length on transvaginal ultrasound, the insertion of a cervical pessary would reduce the rate of spontaneous preterm birth at less than 34 weeks of gestation.
Methods
Study Design and Participants
This was a single-center, parallel-group RCT of women with asymptomatic singleton pregnancies without prior spontaneous preterm birth but with short cervical length on transvaginal ultrasound who were randomized to receive a cervical pessary (ie, intervention group) or no pessary (ie, control group) at the University of Naples Federico II (Naples, Italy) from March 1, 2016, to May 25, 2017.
The trial was approved by the local ethics committee. All participants in the trial provided written informed consent. The trial protocol is available in Supplement 1.
Eligible women were those referred to the institution for a diagnosis of short cervix during the routine anatomy scan. In Italy, the anatomy scan is a routine ultrasound examination primarily used to assess fetal anatomy and detect the presence of any fetal anomalies conducted between 18 weeks 0 days and 23 weeks 6 days of gestation. At the university, measurement of the cervix using transvaginal ultrasound was repeated and women found to have a cervical length of 25 mm or less were approached by the research staff and consented.
Inclusion criteria were age 18 to 50 years, singleton pregnancy, cervical length of 25 mm or less, and gestational age at randomization between 18 weeks 0 days and 23 weeks 6 days of gestation.
Exclusion criteria were multiple pregnancies, rupture of membranes at the time of randomization, lethal fetal structural abnormality, cerclage in situ, vaginal bleeding at the time of randomization, suspicion of chorioamnionitis, placenta previa or accreta, ballooning of membranes outside the cervix into the vagina, cervical length of 0 mm, painful and regular uterine contractions, or history of spontaneous preterm birth between 16 weeks 0 days and 36 weeks 6 days of gestation.
At the time of randomization, ethnicity of the women was assessed by clinician determination given the different baseline risk of preterm birth according to ethnicity.
Randomization and Masking
Eligible participants were randomly allocated in a 1:1 ratio to either the cervical pessary or the control group. Women were randomized by a web-based system using random blocks of 2, 4, and 6 to receive the Arabin pessary (Dr. Arabin GmbH & Co) or no pessary. Randomization was stratified by cervical length (<20 mm or ≥20 mm–≤25 mm). The randomization sequence was prepared by an independent statistician and implemented by use of a central telephone number. The recruiters and the trial coordinator did not have access to the randomization sequence. The allocation code was disclosed only after patient initials were confirmed. Clinicians did not have advance access to the randomization sequence.
Outcome assessors, data collectors, and data analysts were blinded to allocated treatment group. Assessment of the outcomes and outcome collection were made by clinicians not involved in the clinical trial and reported in a form with only the trial identification as the identifier. The data analyst was blinded until the entire analysis was completed.
Interventions
Cervical length was measured by operators with certification of competence in the technique (Fetal Medicine Foundation Certificate of Competence in Cervical Assessment), as described previously.15,16 The length of the cervix was measured with a transvaginal real-time ultrasound probe placed in the anterior fornix of the vagina. Endocervical canal length was measured as the distance between the internal and external os by using a straight line with calipers placed at the notches made by the internal os and external os. Three anatomic landmarks defined the appropriate sagittal view: the internal os, the external os, and the endocervical canal. The image was enlarged while visualizing the 3 landmarks simultaneously. This procedure was repeated 3 times. Only the shortest cervical length measurement was recorded. Each examination was performed during a minimum of 5 minutes.
At the time of randomization, all women in both groups underwent a speculum examination, and vaginal swabs were taken for bacteriological analysis. If the results showed infection, appropriate treatment was given without delaying the insertion of the pessary in the intervention group. The pessary was not removed if there was evidence of bacterial infection after device insertion.
All the cervical pessaries used in the trial were certified by European Conformity and were inserted by the attending physicians, who had received practical training in the placement of the device. Pessary insertion training consisted of a didactic session and a hands-on session. All staff were required to demonstrate competence in pessary placement on a live model. All cervical pessaries were purchased from the manufacturer.
In the intervention group, the cervical pessary was placed at the time of randomization and was removed during the 37th week (37 weeks 0 days–37 weeks 6 days) or earlier if clinically indicated. Reason for earlier removal included active vaginal bleeding, preterm labor with persistent contractions and advanced dilatation despite tocolysis, severe discomfort, or participant request.
Women in the control group received the same obstetrical care as those in the intervention group.
For cervical length of 20 mm or less, women in both groups were prescribed vaginal progesterone 200-mg suppositories daily until 36 weeks 6 days of gestation. No recommendation was made about bed rest, activity, or vaginal intercourse.
All participants were followed up in outpatient settings every month until delivery. In the pessary group, a digital examination was done at each monthly visit to ensure proper pessary placement. At each follow-up visit, women were asked whether they experienced any adverse events and about adherence to progesterone therapy. Specifically, women were asked about vaginal discharge, pelvic discomfort, and pelvic pain. Bleeding or lacerations during the insertion and the removal of the pessary were also recorded.
For women in both groups who presented after 26 weeks of gestation with symptoms of preterm labor, tocolytics and glucocorticoids were administrated for fetal lung maturation and hospitalization was offered.
Outcomes
The primary outcome was spontaneous preterm birth at less than 34 weeks of gestation.
Spontaneous preterm birth included either spontaneous onset of preterm labor or preterm premature rupture of membranes. Iatrogenic (medically indicated) preterm deliveries were not included in the primary end point as they are due to fetal or maternal conditions such as fetal distress or maternal preeclampsia and cannot be modified by use of a pessary.
The prespecified secondary outcomes were spontaneous preterm birth at less than 37, 32, and 28 weeks of gestation, gestational age at delivery, latency (time from randomization to delivery), preterm premature rupture of membranes at less than 34 weeks of gestation, mode of delivery, maternal adverse events (vaginal discharge and pelvic discomfort), chorioamnionitis (inflammation of the chorion and amnion by histopathological assessment after delivery), and neonatal outcomes including birth weight, admission to a neonatal intensive care unit, neonatal death (death of a live-born infant within the first 28 days of life) and perinatal death (either fetal death, defined as intrauterine fetal death after 20 weeks of gestation, or neonatal death), and a composite of adverse perinatal outcomes, defined as at least 1 of the following: necrotizing enterocolitis, intraventricular hemorrhage grade 3 or 4, respiratory distress syndrome, bronchopulmonary dysplasia, retinopathy of prematurity requiring therapy, blood culture–proven sepsis, and neonatal death.
Post hoc exploratory outcomes included preterm birth (spontaneous and iatrogenic) at less than 37 weeks, 34 weeks, 32 weeks, and 28 weeks of gestation; iatrogenic preterm birth at less than 34 weeks; birth weight less than 2500 g or less than 1500 g; and the components of the composite of adverse perinatal outcomes.
Data on pregnancy outcomes were obtained from hospital maternity records. In case of preterm birth, records were examined to determine whether the delivery was medically indicated (iatrogenic preterm birth) or spontaneous.
Sample Size Calculation
Calculation of the sample size was based on the following considerations: a prevalence of cervical length 25 mm or less of about 1% to 2% in women with singleton gestation,15 an incidence of preterm birth at less than 34 weeks of gestation of about 25% in women with singleton pregnancy using vaginal progesterone for cervical length 20 mm or less, and a decrease in spontaneous preterm birth by 50% using a cervical pessary.11 We determined that a sample size of 300 patients (150 per group) would provide a power of 80% to detect a 50% relative reduction in the primary outcome from a baseline risk of 25%, with a 2-sided type I error of .05.
Statistical Analysis
Data are shown as means or as numbers and percentages. Univariate comparisons of dichotomous data were performed using the χ2 test with continuity correction. Comparisons between groups were performed with the use of the t test to test group means by assuming equal within-group variances.
The primary analysis was an intention-to-treat comparison of the treatment assigned at randomization. The effect of pessary use on the cumulative incidence of each outcome was quantified in 2 ways: first as the difference between treatment groups in cumulative incidence of the outcome with 95% confidence intervals and second as the unadjusted relative risk and its 95% confidence interval. Ninety-five percent confidence intervals were assessed using the bootstrap method. Original prespecified analysis included the use of the odds ratio instead of the unadjusted relative risk (Supplement 1). However, given that relative risks are easier to interpret, we decided to quantified the incidence of the primary outcome by using the unadjusted relative risk.
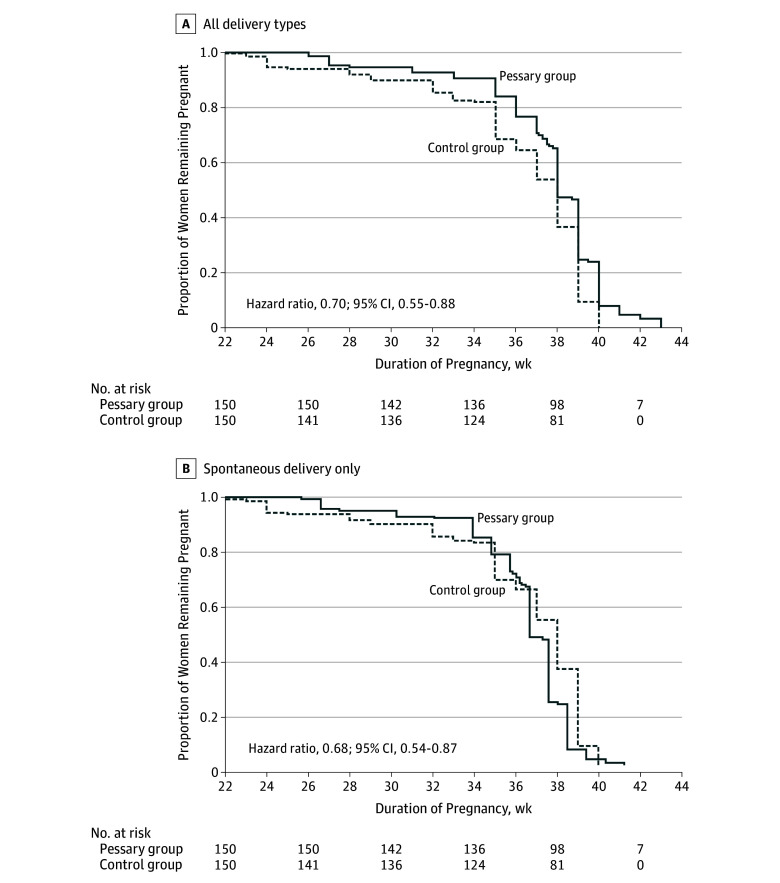
The frequency of spontaneous preterm birth at less than 34 weeks of gestation in relation to gestational age was assessed by Kaplan-Meier analysis. Two different panels was assessed for this analysis: one with any type of delivery (spontaneous and iatrogenic) as the event and one with only spontaneous delivery as the event. Hazard ratios were estimated using the Cox proportional hazards model.
No interim analyses were planned. No adjustment for multiple comparisons was made, so the findings of the secondary outcomes should be considered exploratory. No patients were lost to follow-up and no data were missing. A 2-sided P.05 was considered statistically significant. Statistical analysis was performed using SPSS version 19.0 (IBM Inc).
Post hoc subgroup analyses were performed to examine the effect of a cervical pessary according to progesterone therapy (yes vs no), and cervical length (≤10 mm vs >10 mm). P values for the interaction between subgroup and treatment were calculated using the Wald test.
Results
Trial Population
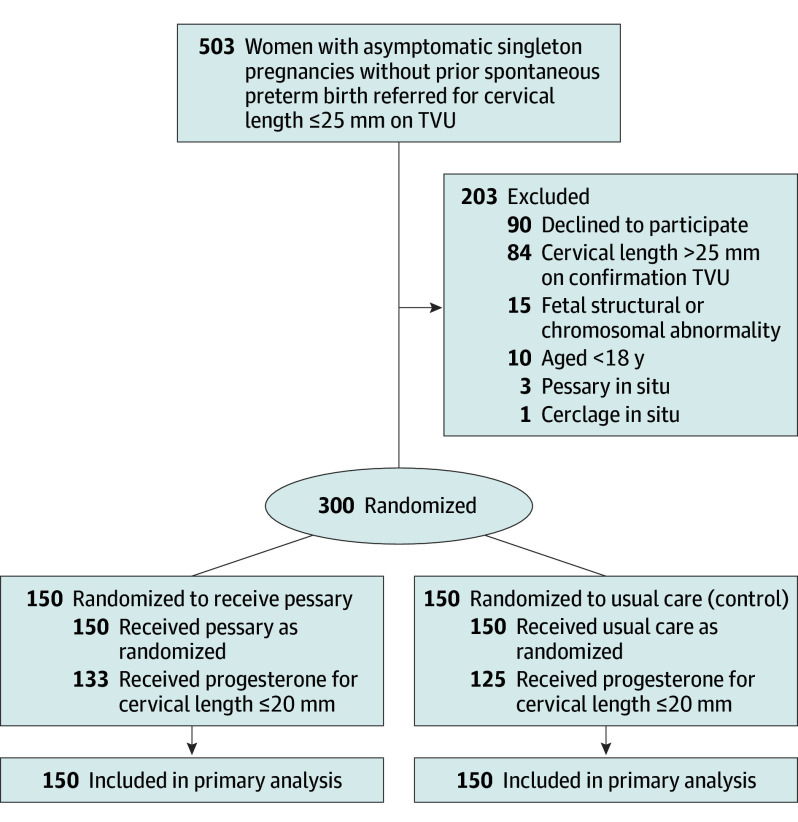
From March 2016 to May 2017, of the 503 women referred for short cervical length, 300 asymptomatic women with singleton pregnancies without prior spontaneous preterm birth but with a transvaginal ultrasound cervical length of 25 mm or less between 18 weeks 0 days and 23 weeks 6 days of gestation agreed to take part in the study, underwent randomization, and were enrolled and followed up.
Of the randomized women, 150 (50%) were randomized to the cervical pessary group and 150 (50%) to the control group. No women were excluded after randomization or lost to follow-up (Figure 1). No women in the intervention group had the pessary removed by request or for severe discomfort.
Figure 1. Flow of Participants in a Trial of the Effect of Cervical Pessary Use on Spontaneous Preterm Birth in Women With Singleton Pregnancies and Short Cervical Length.
TVU indicates transvaginal ultrasound.
Table 1 shows the baseline demographic and clinical characteristics for each group. There were 133 women (88.7%) in the pessary group and 125 (83.3%) in the control group who had a cervical length of 20 mm or less and received vaginal progesterone; 33 (22.0%) in the pessary group and 38 (25.3%) in the control group received antibiotics because of positive cultures from a vaginal swab at the time of randomization. Use of antibiotic therapy among women with positive vaginal cultures is shown in eTable 1 in Supplement 2.
Table 1. Participant Characteristics.
| Characteristics | Pessary Group (n = 150) |
Control Group (n = 150) |
|---|---|---|
| Age, mean (SD), y | 28.5 (6.2) | 28.9 (6.5) |
| Race, No. (%) | ||
| White | 133 (88.7) | 135 (90.0) |
| Asian | 10 (6.7) | 10 (6.7) |
| Black | 7 (4.7) | 5 (3.3) |
| Body mass index, mean (SD)a | 26.7 (6.2) | 26.4 (6.3) |
| Smoking, No. (%) | 19 (12.7) | 20 (13.3) |
| Nulliparous, No. (%) | 104 (69.3) | 105 (70.0) |
| Parous, No. (%) | 46 (30.7) | 45 (30.0) |
| Prior cervical surgery, No. (%) | ||
| Loop excision of transformation zone | 5 (3.3) | 4 (2.7) |
| Cone biopsy | 2 (1.3) | 1 (0.7) |
| Gestation time at randomization, mean (SD), wk | 22.3 (1.4) | 22.4 (1.1) |
| Cervical length, mean (SD), mm | 11.5 (5.7) | 12.5 (5.9) |
| ≤20, No. (%) | 133 (88.7) | 125 (83.3) |
| ≤15, No. (%) | 122 (81.3) | 115 (76.7) |
| ≤10, No. (%) | 56 (37.3) | 42 (28.0) |
| ≤5, No. (%) | 16 (10.7) | 12 (8.0) |
| Vaginal progesterone, No. (%) | 133 (88.7) | 125 (83.3) |
| Positive vaginal swab culture at randomization, No. (%) | 36 (24.0) | 41 (27.3) |
| Antibiotics for positive vaginal culture, No. (%) | 33 (22.0) | 38 (25.3) |
Calculated as weight in kilograms divided by height in meters squared.
The mean gestational age at randomization was 22.3 (SD, 1.4) weeks vs 22.4 (SD, 1.1) weeks and the mean cervical length was 11.5 mm (SD, 5.7 mm) vs 12.5 mm (SD, 5.9 mm) in the pessary and control groups, respectively.
Primary Outcome
Spontaneous preterm birth at less than 34 weeks of gestation occurred in 11 women (7.3%) in the pessary group and 23 women (15.3%) in the control group (between-group difference, −8.0%; 95% CI, −15.7% to −0.4%) (Table 2). In the survival analysis to 34 weeks of gestation, the incidence of spontaneous preterm birth was significantly lower in the pessary group compared with the control group (hazard ratio, 0.36; 95% CI, 0.54-0.87) (Figure 2).
Table 2. Primary and Secondary Outcomes in the Pessary and Control Groups.
| Outcomes | Pessary Group (n = 150) |
Control Group (n = 150) |
Between-Group Difference in % or Mean (95% CI) | Relative Risk (95% CI) | P Value |
|---|---|---|---|---|---|
| Primary Outcome | |||||
| Spontaneous preterm birth <34 wk, No. (%) | 11 (7.3) | 23 (15.3) | −8.0 (−15.7 to −0.4)a | 0.48 (0.24-0.95)a | .04 |
| Secondary Outcomes b | |||||
| Spontaneous preterm birth, No. (%) | |||||
| <37 wk | 30 (20.0) | 49 (32.7) | −12.7 (−22.9 to −2.3)a | 0.61 (0.41-0.91)a | .02 |
| <32 wk | 10 (6.7) | 14 (9.3) | −2.6 (−4.1 to 9.4) | 0.71 (0.33-1.56) | .52 |
| <28 wk | 6 (4.0) | 9 (6.0) | −2.0 (−3.5 to 7.7) | 0.67 (0.24-1.83) | .60 |
| Gestational age at delivery, mean (95% CI), wk | 37.6 (37.1-38.2) | 36.2 (35.5-36.9) | 1.4 (0.6 to 2.3)a | .001 | |
| Time from randomization to delivery, mean (95% CI), d | 107.0 (102.1-113.2) | 97.0 (91.7-103.3) | 10.0 (3.8 to 16.2)a | .002 | |
| Preterm premature rupture of membranes <34 wk, No. (%) | 2 (1.3) | 2 (1.3) | 0 (−3.6 to 3.6) | 1.00 (0.14-7.01) | >.99 |
| Cesarean delivery, No. (%) | 45 (30.0) | 57 (38.0) | −8.0 (−3.2 to 19.0) | 0.79 (0.57-1.09) | .18 |
| Operative vaginal delivery, No. (%) | 5 (3.3) | 10 (6.7) | −3.4 (−2.1 to 9.1) | 0.50 (0.18-1.43) | .29 |
| Spontaneous vaginal delivery, No. (%) | 100 (66.7) | 83 (55.3) | 11.4 (−0.1 to 22.6) | 1.20 (1.00-1.45) | .06 |
| Maternal Adverse Effects b | |||||
| Vaginal discharge, No. (%) | 130 (86.7) | 69 (46.0) | 40.7 (30.1 to 50.3)a | 1.88 (1.57-2.27)a | <.001 |
| Pelvic discomfort, No. (%) | 5 (3.3) | 1 (0.6) | 2.7 (−1.0 to 7.0) | 5.00 (0.59-42.29) | .22 |
| Chorioamnionitis, No. (%) | 5 (3.3) | 7 (4.7) | −1.4 (−3.7 to 6.6) | 0.71 (0.23-2.20) | .77 |
| Neonatal Outcomes b | |||||
| Birth weight, mean (95% CI), g |
2889.9 (2770.3-3009.6) | 2644.6 (2513.5-2775.7) | 245.3 (69.2 to 421.4)a | .006 | |
| Neonatal intensive care unit, No. (%) | 15 (10.0) | 28 (18.7) | −8.7 (−17.1 to −0.3)a | 0.54 (0.30-0.96)a | .04 |
| Neonatal death, No. (%)c | 1 (0.7) | 3 (2.0) | −1.3 (−2.1 to 5.1) | 0.33 (0.04-3.17) | .61 |
| Perinatal death, No. (%)d | 2 (1.3) | 4 (2.7) | −1.4 (−2.5 to 5.6) | 0.50 (0.09-2.69) | .68 |
| Composite perinatal outcome, No. (%)e | 22 (14.7) | 48 (32.0) | −17.3 (−27.0 to −7.3)a | 0.46 (0.29-0.72)a | .01 |
Statistically significant.
No adjustment for multiple comparisons was made, so the findings of the secondary outcomes should be considered exploratory.
Neonatal death is death of a live-born infant within the first 28 days of life.
Perinatal death is intrauterine fetal death after 20 weeks of gestation or neonatal death.
Participants with the composite perinatal outcome had at least 1 of the following: necrotizing enterocolitis, intraventricular hemorrhage grade 3 or 4, respiratory distress syndrome, bronchopulmonary dysplasia, retinopathy of prematurity requiring therapy, blood culture–proven sepsis, or neonatal death.
Figure 2. Kaplan-Meier Plot of the Probability of Continued Pregnancy Without Delivery in the Cervical Pessary and Control Groups.
Prespecified Secondary Outcomes
The cervical pessary was associated with a significantly lower rate of spontaneous preterm birth at less than 37 weeks of gestation, longer gestational age at delivery and latency from randomization to delivery, higher birth weight, lower rate of admission to a neonatal intensive care unit, and lower incidence of adverse composite perinatal outcome compared with the control group. There was no significant between-group difference in the incidence of spontaneous preterm birth at less than 32 weeks or 28 weeks, but the trial was not powered for these outcomes (Table 2).
Post Hoc Outcomes
The cervical pessary was associated with a significantly lower rate of preterm birth at less than 37 weeks and 34 weeks of gestation. The cervical pessary was also associated with significantly lower rates of respiratory distress syndrome and retinopathy of prematurity vs controls and with nonsignificantly lower rates of necrotizing enterocolitis, intraventricular hemorrhage grade 3 or 4, bronchopulmonary dysplasia, and blood culture–proven sepsis (eTable 2 in Supplement 2).
Adverse Events
During follow-up, the pessary group had a higher rate than the control group of increased or new vaginal discharge (86.7% vs 46.0%; between-group difference, 40.7%; 95% CI, 30.1% to 50.3%), but no significant differences in pelvic discomfort were reported (Table 2).
No cases of maternal death or serious injuries during insertion or removal of the pessary were reported.
Post Hoc Subgroup Analyses
The tests of interaction for the post hoc subgroup analyses for receipt of concomitant therapy with vaginal progesterone and by cervical length of 10 mm or less vs greater than 10 mm were not significant (P=.56 and P=.46 for interaction, respectively) (eTable 3 in Supplement 2).
Discussion
This RCT showed that in asymptomatic women with singleton pregnancies without prior spontaneous preterm birth but with a transvaginal ultrasound cervical length of 25 mm or less, use of a cervical pessary resulted in a statistically significantly lower rate of spontaneous preterm birth than no pessary. Cervical pessary was also associated with a significant difference in the secondary outcomes of longer gestational age at delivery, longer latency, and a lower incidence of a composite of adverse neonatal outcomes but with a higher rate of vaginal discharge.
This study did not support earlier findings of a meta-analysis of 3 RCTs that showed no beneficial effect of a cervical pessary in reducing spontaneous preterm birth in women with a singleton gestation and a cervical length of 25 mm or less.13 None of the included studies9,10,11 were blinded for outcome assessors, data collectors, or data analysts. Moreover, the higher rate of preterm birth in the control group in 1 of the trials (26.8%)11 is not concordant with those of the control groups of the other 2 trials (5.5% and 11.3%).9,10 More than half of the women included in the meta-analysis (932/1420) came from 1 large trial by Nicolaides et al,9 which drives the summary statistics. This trial was methodologically very different from our study. Nicolaides et al included both women without prior preterm birth and those with prior preterm birth, and the study included multiple sites, some of which did not enroll many participants, raising the possibility of lesser experience with pessary placement and management.9 The current study’s trial protocol included hands-on training and a requirement for all staff to demonstrate pessary insertion competence on a live model, while Nicolaides et al9 did not include this type of training. The median cervical length at randomization was lower in this study compared with the trial by Nicolaides et al (approximately 12 mm vs 20 mm) and the rate of very short cervix was higher (79% vs 29% for cervical length ≤15 mm). The different results between the trials raises the question of whether a cervical pessary can be effective only at very low cervical length cutoffs, although there was no effect modification by cervical length in the current study.
The results of the current study are consistent with those of the trial by Goya et al,11 which concluded that a cervical pessary could prevent preterm birth in a population of appropriately selected at-risk women previously screened for cervical length assessment on transvaginal ultrasound at the midtrimester visit. There were more women with prior preterm birth in the trial by Nicolaides et al9 (154/932 [16.5%]) compared with the trial by Goya et al11 (41/380 [10.8%]). This raises the question of whether a cervical pessary can be effective only in women with a short cervix but without prior preterm birth.
Different strategies have been adopted for prevention of preterm birth, including progesterone use,5,17,18,19 cerclage,6,7,8,20,21 cervical pessary use,9,10,11,12,13,14 and lifestyle modifications such as smoking cessation,22 diet,23 aerobic exercise,24,25 and nutritional supplements.26,27,28,29,30 Cervical cerclage is an invasive technique requiring anesthesia and an operating room.31 Therefore, increasing interest has focused on use of a pessary for prevention of preterm birth. A cervical pessary is relatively noninvasive, is easy to use, does not require anesthesia, can be used in an outpatient clinic setting, and is easily removed when necessary.32 The exact mechanism of the possible efficacy of a cervical pessary to prevent spontaneous preterm birth in women with short cervical length is not completely clear. Vitsky33 first suggested in 1961 that the incompetent cervix is aligned centrally, with no support except the nonresistant vagina. A cervical pessary would change the inclination of the cervical canal, directing it more posteriorly. In doing so, the weight of the pregnancy would be more on the anterior lower segment.32 Another proposed mechanism is that the pessary could strengthen the immunological barrier between the chorioamnion-extraovular space and the vaginal microbiological flora, as cerclage has been postulated to do.34
The strengths of the current study included blinding of the outcome assessors, data collectors, and data analysts as well as the 100% follow-up obtained because all women included in the trial delivered at the study institution.
This study has several limitations. First, the open-label nature of the trial could have affected medical decision making, such as the timing of the removal of the pessary when a participant presented with contractions. However, outcome assessors and data analysts were blinded. Second, the exploratory nature of the secondary outcomes and the numerous secondary end points with no adjustment for multiple comparisons could have led to type I error. Third, the single-center nature of the trial raises the question of the external generalizability of the findings. Fourth, all women in both groups underwent vaginal swabs for bacteriological analysis. The practice of screening and treating for vaginal infections during pregnancy is a subject of debate and is not currently recommended.
Conclusions
Among women without prior spontaneous preterm birth who had asymptomatic singleton pregnancies and short transvaginal cervical length, use of a cervical pessary, compared with no pessary use, resulted in a lower rate of spontaneous preterm birth at less than 34 weeks of gestation. The results of this single-center, nonblinded study among selected pregnant women require confirmation in multicenter clinical trials.
Trial Protocol
eTable 1. Results of Vaginal Swabs at Randomization
eTable 2. Post Hoc Secondary Outcomes
eTable 3. Subgroup Analyses for Spontaneous Preterm Birth at Less Than 34 Weeks
References
- 1.Martin JA, Hamilton BE, Osterman MJ, Driscoll AK, Mathews TJ. Births: final data for 2015. Natl Vital Stat Rep. 2017;66(1):1. [PubMed] [Google Scholar]
- 2.Rysavy MA, Li L, Bell EF, et al. ; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network . Between-hospital variation in treatment and outcomes in extremely preterm infants. N Engl J Med. 2015;372(19):1801-1811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patel RM, Kandefer S, Walsh MC, et al. ; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network . Causes and timing of death in extremely premature infants from 2000 through 2011. N Engl J Med. 2015;372(4):331-340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American College of Obstetricians and Gynecologists . ACOG practice bulletin No.142: cerclage for the management of cervical insufficiency. Obstet Gynecol. 2014;123(2 pt 1):372-379. [DOI] [PubMed] [Google Scholar]
- 5.Society for Maternal-Fetal Medicine Publications Committee . Progesterone and preterm birth prevention: translating clinical trials data into clinical practice. Am J Obstet Gynecol. 2012;206(5):376-386. [DOI] [PubMed] [Google Scholar]
- 6.Berghella V, Rafael TJ, Szychowski JM, Rust OA, Owen J. Cerclage for short cervix on ultrasonography in women with singleton gestations and previous preterm birth: a meta-analysis. Obstet Gynecol. 2011;117(3):663-671. [DOI] [PubMed] [Google Scholar]
- 7.Berghella V, Ciardulli A, Rust OA, et al. Cerclage for sonographic short cervix in singleton gestations without prior spontaneous preterm birth: systematic review and meta-analysis of randomized controlled trials using individual patient-level data. Ultrasound Obstet Gynecol. 2017;50(5):569-577. [DOI] [PubMed] [Google Scholar]
- 8.Saccone G, Rust O, Althuisius S, Roman A, Berghella V. Cerclage for short cervix in twin pregnancies: systematic review and meta-analysis of randomized trials using individual patient-level data. Acta Obstet Gynecol Scand. 2015;94(4):352-358. [DOI] [PubMed] [Google Scholar]
- 9.Nicolaides KH, Syngelaki A, Poon LC, et al. A randomized trial of a cervical pessary to prevent preterm singleton birth. N Engl J Med. 2016;374(11):1044-1052. [DOI] [PubMed] [Google Scholar]
- 10.Hui SY, Chor CM, Lau TK, Lao TT, Leung TY. Cerclage pessary for preventing preterm birth in women with a singleton pregnancy and a short cervix at 20 to 24 weeks: a randomized controlled trial. Am J Perinatol. 2013;30(4):283-288. [DOI] [PubMed] [Google Scholar]
- 11.Goya M, Pratcorona L, Merced C, et al. ; Pesario Cervical para Evitar Prematuridad (PECEP) Trial Group . Cervical pessary in pregnant women with a short cervix (PECEP): an open-label randomised controlled trial. Lancet. 2012;379(9828):1800-1806. [DOI] [PubMed] [Google Scholar]
- 12.Karbasian N, Sheikh M, Pirjani R, Hazrati S, Tara F, Hantoushzadeh S. Combined treatment with cervical pessary and vaginal progesterone for the prevention of preterm birth: a randomized clinical trial. J Obstet Gynaecol Res. 2016;42(12):1673-1679. [DOI] [PubMed] [Google Scholar]
- 13.Saccone G, Ciardulli A, Xodo S, et al. Cervical pessary for preventing preterm birth in singleton pregnancies with short cervical length: a systematic review and meta-analysis. J Ultrasound Med. 2017;36(8):1535-1543. [DOI] [PubMed] [Google Scholar]
- 14.Saccone G, Ciardulli A, Xodo S, et al. Cervical pessary for preventing preterm birth in twin pregnancies with short cervical length: a systematic review and meta-analysis. J Matern Fetal Neonatal Med. 2017;30(24):2918-2925. [DOI] [PubMed] [Google Scholar]
- 15.Iams JD, Goldenberg RL, Meis PJ, et al. ; National Institute of Child Health and Human Development Maternal Fetal Medicine Unit Network . The length of the cervix and the risk of spontaneous premature delivery. N Engl J Med. 1996;334(9):567-572. [DOI] [PubMed] [Google Scholar]
- 16.Saccone G, Simonetti B, Berghella V. Transvaginal ultrasound cervical length for prediction of spontaneous labour at term: a systematic review and meta-analysis. BJOG. 2016;123(1):16-22. [DOI] [PubMed] [Google Scholar]
- 17.Saccone G, Khalifeh A, Elimian A, et al. Vaginal progesterone vs intramuscular 17α-hydroxyprogesterone caproate for prevention of recurrent spontaneous preterm birth in singleton gestations: systematic review and meta-analysis of randomized controlled trials. Ultrasound Obstet Gynecol. 2017;49(3):315-321. [DOI] [PubMed] [Google Scholar]
- 18.Suhag A, Saccone G, Berghella V. Vaginal progesterone for maintenance tocolysis: a systematic review and metaanalysis of randomized trials. Am J Obstet Gynecol. 2015;213(4):479-487. [DOI] [PubMed] [Google Scholar]
- 19.Saccone G, Suhag A, Berghella V. 17-alpha-hydroxyprogesterone caproate for maintenance tocolysis: a systematic review and metaanalysis of randomized trials. Am J Obstet Gynecol. 2015;213(1):16-22. [DOI] [PubMed] [Google Scholar]
- 20.Suhag A, Reina J, Sanapo L, et al. Prior ultrasound-indicated cerclage: comparison of cervical length screening or history-indicated cerclage in the next pregnancy. Obstet Gynecol. 2015;126(5):962-968. [DOI] [PubMed] [Google Scholar]
- 21.Ehsanipoor RM, Seligman NS, Saccone G, et al. Physical examination-indicated cerclage: a systematic review and meta-analysis. Obstet Gynecol. 2015;126(1):125-135. [DOI] [PubMed] [Google Scholar]
- 22.Chamberlain C, O’Mara-Eves A, Oliver S, et al. Psychosocial interventions for supporting women to stop smoking in pregnancy. Cochrane Database Syst Rev. 2013;(10):CD001055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ota E, Hori H, Mori R, Tobe-Gai R, Farrar D. Antenatal dietary education and supplementation to increase energy and protein intake. Cochrane Database Syst Rev. 2015;(6):CD000032. [DOI] [PubMed] [Google Scholar]
- 24.Magro-Malosso ER, Saccone G, Di Mascio D, Di Tommaso M, Berghella V. Exercise during pregnancy and risk of preterm birth in overweight and obese women: a systematic review and meta-analysis of randomized controlled trials. Acta Obstet Gynecol Scand. 2017;96(3):263-273. [DOI] [PubMed] [Google Scholar]
- 25.Di Mascio D, Magro-Malosso ER, Saccone G, Marhefka GD, Berghella V. Exercise during pregnancy in normal-weight women and risk of preterm birth: a systematic review and meta-analysis of randomized controlled trials. Am J Obstet Gynecol. 2016;215(5):561-571. [DOI] [PubMed] [Google Scholar]
- 26.Saccone G, Saccone I, Berghella V. Omega-3 long-chain polyunsaturated fatty acids and fish oil supplementation during pregnancy: which evidence? J Matern Fetal Neonatal Med. 2016;29(15):2389-2397. [DOI] [PubMed] [Google Scholar]
- 27.Saccone G, Berghella V. Omega-3 supplementation to prevent recurrent preterm birth: a systematic review and metaanalysis of randomized controlled trials. Am J Obstet Gynecol. 2015;213(2):135-140. [DOI] [PubMed] [Google Scholar]
- 28.Saccone G, Berghella V. Omega-3 long chain polyunsaturated fatty acids to prevent preterm birth: a systematic review and meta-analysis. Obstet Gynecol. 2015;125(3):663-672. [DOI] [PubMed] [Google Scholar]
- 29.Saccone G, Berghella V. Folic acid supplementation in pregnancy to prevent preterm birth: a systematic review and meta-analysis of randomized controlled trials. Eur J Obstet Gynecol Reprod Biol. 2016;199:76-81. [DOI] [PubMed] [Google Scholar]
- 30.De-Regil LM, Palacios C, Lombardo LK, Peña-Rosas JP. Vitamin D supplementation for women during pregnancy. Cochrane Database Syst Rev. 2016;(1):CD008873. [DOI] [PubMed] [Google Scholar]
- 31.Berghella V, Ludmir J, Simonazzi G, Owen J. Transvaginal cervical cerclage: evidence for perioperative management strategies. Am J Obstet Gynecol. 2013;209(3):181-192. [DOI] [PubMed] [Google Scholar]
- 32.Arabin B, Halbesma JR, Vork F, Hübener M, van Eyck J. Is treatment with vaginal pessaries an option in patients with a sonographically detected short cervix? J Perinat Med. 2003;31(2):122-133. [DOI] [PubMed] [Google Scholar]
- 33.Vitsky M. Simple treatment of the incompetent cervical os. Am J Obstet Gynecol. 1961;81:1194-1197. [DOI] [PubMed] [Google Scholar]
- 34.Jones G, Clark T, Bewley S. The weak cervix: failing to keep the baby in or infection out? Br J Obstet Gynaecol. 1998;105(11):1214-1215. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
eTable 1. Results of Vaginal Swabs at Randomization
eTable 2. Post Hoc Secondary Outcomes
eTable 3. Subgroup Analyses for Spontaneous Preterm Birth at Less Than 34 Weeks