Dear Editor,
Onychomycosis, a persistent fungal infection of the nail bed, matrix, or plate is the most common nail disorder in adults, accounting for up to 50% of all ungual pathologies. High prevalence of the disease together with the limited efficacy of conventional therapies, has stimulated the development of new and more effective approaches in treating the disease.[1]
Due to their minimally invasive nature and potential to restore clear nail growth with relatively few sessions, lasers have become a popular option in the treatment of onychomycosis.
A middle-aged male, otherwise healthy, presented with severe distal subungual onychomycosis of the toenail recalcitrant to all treatment modalities. He was treated with three cycles of itraconazole and amorolfine nail lacquer without much improvement. We tried Q-switched neodymium-doped yttrium aluminum garnet (Nd-Yag) lasers for his nail fungus out of desperation as the patient was frustrated for the past 5 years or more with all kinds of medical therapies available. The laser protocol included 3 sessions with an interval of 2 weeks. Laser fluence of 500 mj was applied with a 1.5-mm spot size. Two passes across the nail plate were performed with a minute pause between each pass. The lateral and proximal nail folds were also treated. After 3 sittings, the patient was more than happy with the treatment, and there were no noticeable side effects. Figure 1 and 2 show before and after 3 sessions of Q switched Neodymium-doped yttrium aluminium garnet laser and the video shows the laser pass being given over the affected nail plate. Clinically, the patient improved and the follow-up mycology was negative There were no signs of recurrence after a follow-up of 3 months (Video 1: showing laser pass being given over the affected nail).
Figure 1.
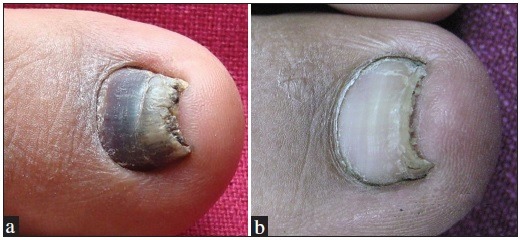
(a) Distal subungal onychomycosis of toe nail (b) Clearance of onychomycosis after 3 sessions of Q switched Neodymium-doped yttrium aluminium garnet laser
Figure 2.

(a) Distal subungual onychomycosis of toenail. (b) Clearance of onychomycosis after 3 sessions of Q-switched neodymium-doped yttrium aluminum garnet laser
Laser or light systems that have been investigated for onychomycosis include the carbon dioxide, Nd-Yag, 870/930-nm combination, and femtosecond infrared 800 nm lasers in addition to photodynamic and ultraviolet light therapy.[2]
The various light sources used for the treatment of onychomycosis have the potential to destroy dermatophytes by a variety of methods including photothermal and photochemical effects.[3] Photothermal effects include selective photothermolysis and nonselective bulk heating of dermatophytes.[4] Photochemical effects include PDT or selective alteration of metabolic or structural function with specific wavelengths.
The photothermal effects of lasers can be selective or nonselective. In both cases, the laser creates heat to destroy the target; however, in the case of selective photothermolysis, the heat is preferentially absorbed by the target. This allows for more precise, thermally confined laser surgery. Since selective heating of dermatophytes is quite challenging, currently, most laser systems target dermatophytes through nonspecific bulk heating.[3]
If laser and light-based devices act through nonspecific bulk heating of dermatophytes, there is a high risk of heating and destroying surrounding normal tissue while attempting to eradicate dermatophytes. This would produce unacceptable side effects such as ulceration, dyspigmentation, and scar.[3] In case of nonspecific bulk heating of dermatophytes, direct laser elimination of onychomycosis is not successful due to difficulties in selectively delivering laser energy to the deeper levels of the nail plate without collateral damage. Thus, selective photothermolysis of dermatophytes, while sparing the surrounding structures, is preferable.[3]
The Q-switched Nd-Yag laser provides a selective, both photothermal and photomechanical effect on the fungus. It is postulated that denaturing one or more of the molecules within the pathogen may deactivate the fungi.
It has been proposed that the 532 nm Nd-Yag laser may be better at targeting the endogenous pigment xanthomegnin, which has peak absorption between 406 and 555 nm.[2,3,4,5] The 1064 nm setting is beyond the absorption spectrum of xanthomelanin, but its effectiveness is due to another absorbing chromophobe, perhaps melanin, which is present in the fungal cell wall.[2] Since it is a longer wavelength, it is able to more deeply penetrate tissue and efficiently target fungal overgrowth in the nail bed.[2]
The exact mechanism of laser therapy is still under investigation, but it may combine direct fungicidal effects of the laser with induced modifications in the immune system or changes in the local microenvironment.[6]
Due to minimally invasive nature and less likely adverse effects, Q-switched Nd-Yag laser appears to be a promising treatment for onychomycosis. The laser may be combined with topical and oral antifungals in patients with onychomycosis recalcitrant to treatment.
Laser treatment for onychomycosis is still incipient, and thus, further efforts toward the establishment of standard treatment schedules, as well as the best pulse characteristics with regards to fluency, length and format, are still required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Video Available on: www.jcasonline.com
REFERENCES
- 1.Morais OO, Costa IM, Gomes CM, Shinzato DH, Ayres GM, Cardoso RM. The use of the Er:YAG 2940nm laser associated with amorolfine lacquer in the treatment of onychomycosis. An Bras Dermatol. 2013;88:847–9. doi: 10.1590/abd1806-4841.20131932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ledon JA, Savas J, Franca K, Chacon A, Nouri K. Laser and light therapy for onychomycosis: A systematic review. Lasers Med Sci. 2014;29:823–9. doi: 10.1007/s10103-012-1232-y. [DOI] [PubMed] [Google Scholar]
- 3.Ortiz AE, Avram MM, Wanner MA. A review of lasers and light for the treatment of onychomycosis. Lasers Surg Med. 2014;46:117–24. doi: 10.1002/lsm.22211. [DOI] [PubMed] [Google Scholar]
- 4.Carney C, Cantrell W, Warner J, Elewski B. Treatment of onychomycosis using a submillisecond 1064-nm neodymium:yttrium-aluminum-garnet laser. J Am Acad Dermatol. 2013;69:578–82. doi: 10.1016/j.jaad.2013.04.054. [DOI] [PubMed] [Google Scholar]
- 5.Kawai K, Akita T, Nishibe S, Nozawa Y, Ogihara Y, Ito Y. Biochemical studies of pigments from a pathogenic fungus microsporum cookei. III. Comparison of the effects of xanthomegnin and O-methylxanthomegnin on the oxidative phosphorylation of rat liver mitochondria. J Biochem. 1976;79:145–52. doi: 10.1093/oxfordjournals.jbchem.a131041. [DOI] [PubMed] [Google Scholar]
- 6.Gupta A, Simpson F. Device-based therapies for onychomycosis treatment. Skin Therapy Lett. 2012;17:4–9. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.