Abstract
Craniopharyngiomas usually involve the sella and suprasellar space. Their occurrence in the posterior fossa without extension to the suprasellar region is uncommon with only 16 cases reported in the literature. We report a case of a primary posterior fossa craniopharyngioma that was managed by complete excision with a good recovery. Our case was unique in that the craniopharyngioma occurred in the fourth ventricle and extended downward to the level of C1, a manifestation that was reported only twice in the past. The literature on the topic is reviewed.
Keywords: Cerebellopontine angle craniopharyngioma, de novo craniopharyngioma, ectopic craniopharyngioma, fourth ventricular craniopharyngioma, primary posterior fossa craniopharyngioma
Introduction
Craniopharyngiomas are benign extra-axial partially cystic slow growing epithelial tumors. They account for 1.2–4.6% of all intracranial tumors.[1,2,3] They typically develop in the infundibulohypophysial axis and frequently occupy the suprasellar/parasellar region between the sella and hypothalamus, either anterior or posterior to optic chiasm. They are postulated to arise from the remnants of Rathke's pouch. Although the tumor is most commonly suprasellar in location, small numbers of craniopharyngiomas are located in the intrasellar region, infrasellar region, or the anterior, middle, and posterior cranial fossa.
Extension of craniopharyngiomas to the posterior cranial fossa occurs in 4–5.9% of cases.[2] Posterior fossa craniopharyngiomas may occur either as recurrence/extension or primary tumor (de novo). The latter is extremely rare with only 16 cases reported in literature up to date.[4,5] Pure fourth ventricle craniopharyngiomas are even rarer with only two cases reported in the literature.[6,7] In this article, the authors report a rare case of a de novo fourth ventricle craniopharyngioma that extended down to the foramen magnum, which was managed by complete excision. The aim is to provide documentation of the third case of craniopharyngioma in this location and to review the literature on the topic in an effort to increase neurosurgeons’ awareness of this rare occurrence.
Case Report
A previously healthy 24-year-old male presented to the Emergency Department in our hospital with 1-day history of altered conscious level. He had suffered from headache and difficulty walking for 3 weeks before his presentation. The headache was continued and progressive in nature, located in the occipital region, and was associated with nausea, vomiting, and diplopia. On examination, his Glasgow Coma Scale was 12/15. He had left sixth cranial nerve palsy with no papilledema, facial paralysis, or other neurological deficits. Computerized topography of the brain showed a large posterior fossa nonenhancing fourth ventricular lesion containing hemorrhage and calcification and causing obstructive hydrocephalus [Figure 1]. The patient's conscious level deteriorated rapidly necessitating the insertion of the emergency cerebrospinal fluid external ventricular drain (EVD) as the first procedure. Magnetic resonance imaging (MRI) of the brain showed a midline posterior fossa cystic lesion measuring 7.2 cm in the craniocaudal plane and 5.5 cm × 4.1 cm in the axial plane [Figure 2a and b]. The lesion appeared to have two components; an anterior portion located within the fourth ventricle and a posterior portion adjacent to the vermis extending downward through the foramen magnum reaching the level of C1. The lesion was purely intraventricular and causing a significant mass effect on the medulla and pons. Following the EVD, the patient regained consciousness and his condition stabilized. On the following day, he underwent posterior fossa craniectomy and total excision of the tumor. The posterior cystic component of the lesion contained yellowish turbid fluid. It had a thin wall which extended down to the level of the C1 but was easily removable. The anterior portion was partly calcified and partly solid containing muddy-like material. Although its wall was slightly adherent to the floor of the fourth ventricle, it was excised completely.
Figure 1.
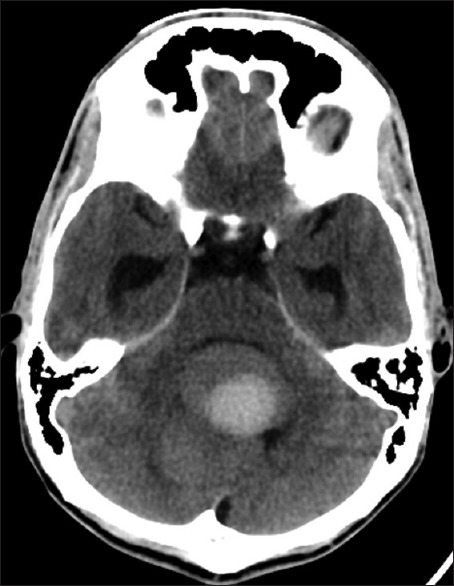
Computed tomography scan (axial with or without contrast): A large midline posterior fossa lesion occupying the fourth ventricle with evidence of calcification in the periphery
Figure 2.
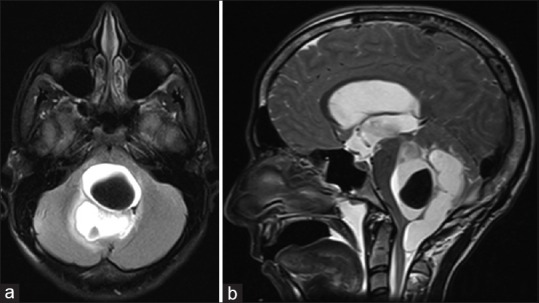
Magnetic resonance imaging scan (T2-weighted axial (a) and sagittal (b)): Midline posterior fossa cystic tumor lesion occupying the fourth ventricle and extending down to C1 and pushing the brainstem anteriorly. The lesion has two components: Anterior and posterior
Histopathology showed a cystic lesion lined by squamous epithelium (varies from flat, simple to stratified) with focal peripheral palisading. The wall shows extensive fibrosis, chronic inflammation, cholesterol clefts, and cystic changes, with calcification and focal osteoid formation. Wet keratin was identified. Focal cerebellar tissues with reactive gliosis were seen. These features were diagnostic of adamantinomatous type craniopharyngioma [Figure 3a–c]. Postoperatively, the patient made a good recovery with no neurological focal deficits apart from the left sixth nerve palsy which recovered only partially. The EVD was removed and no permanent shunting was required. Postoperative MRI showed no evidence of tumor residual and no hydrocephalus. At 2-year follow-up, the patient remains asymptomatic with no evidence of a recurrence.
Figure 3.
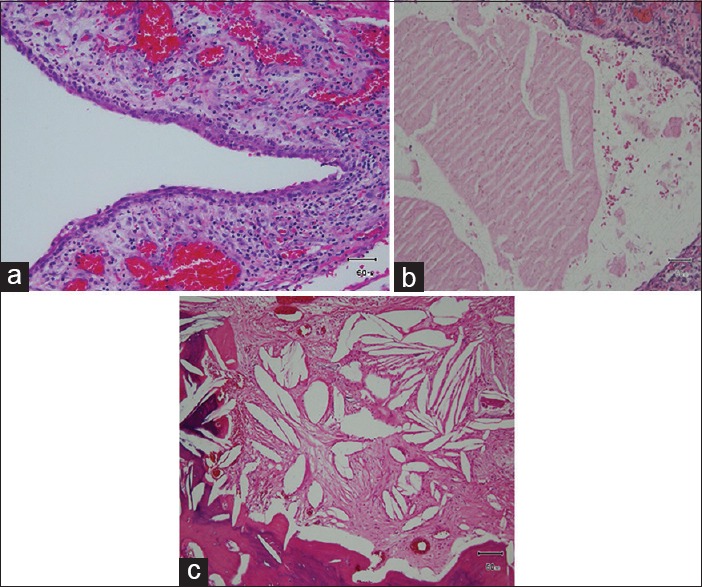
Histopathological specimen (H and E stain): A cyst wall lined by flat, simple to stratified squamous with peripheral palisaded cells, fibrosis and chronic inflammation (a). The attenuated central keratinizing epithelium is giving rise to squamoid cell ghosts referred to as “wet keratin” (b). The cyst wall shows cholesterol clefts and ossification/calcification (c)
Discussion
Craniopharyngiomas are relatively rare neoplasms that arise from squamous rests located at any point along the invagination of the primitive stomodeum of Rathke's pouch along a line from the nasopharynx to the hypothalamus.[8] They comprise 6–13% of brain tumors in children with an annual incidence of 5.25 cases per million. They are equally common in males and females with no variance by race.[3] Distribution by age is bimodal with the peak incidence in children at 5–14 years and in adults at the fifth and sixth decades of life.[3,9]
Craniopharyngiomas are most commonly located extra-axially in the sellar or suprasellar area in 90% of cases.[10] They can extend to the infrasellar region (5% of cases) and anterior (2–5%), middle (2%), or posterior (1–4%) cranial fossa.[11] Rarely, craniopharyngiomas arise primarily in unusual locations, such as the nasopharynx, sphenoid bone, third ventricle, pineal gland, sylvian fissure, and cerebellopontine angle (CPA).
Posterior fossa craniopharyngiomas have been categorized into three distinct groups.[3,4,12,13] The first group is the large craniopharyngiomas that extend from the suprasellar region to the posterior fossa. The second group is the craniopharyngiomas that recur in the posterior fossa after surgical resection of sellar or parasellar tumors and the third group are the craniopharyngiomas that arise de novo in the posterior fossa. Within the latter group, two different locations reported are the CPA and the fourth ventricle. The de novo origin of posterior fossa craniopharyngioma can be explained by two main hypotheses.[5] The embryogenic theory relates to the transformation of the remnant cells of the craniopharyngial duct and the involuted Rathke's pouch along a line that extends from the vomer through the midline sphenoid bone to the floor of sella turcica. The alternative metaplastic theory relates to the residual squamous epithelium that may undergo metaplasia. These cells are derived from stomodeum and are normally part of adenohypophysis.[4,5,6]
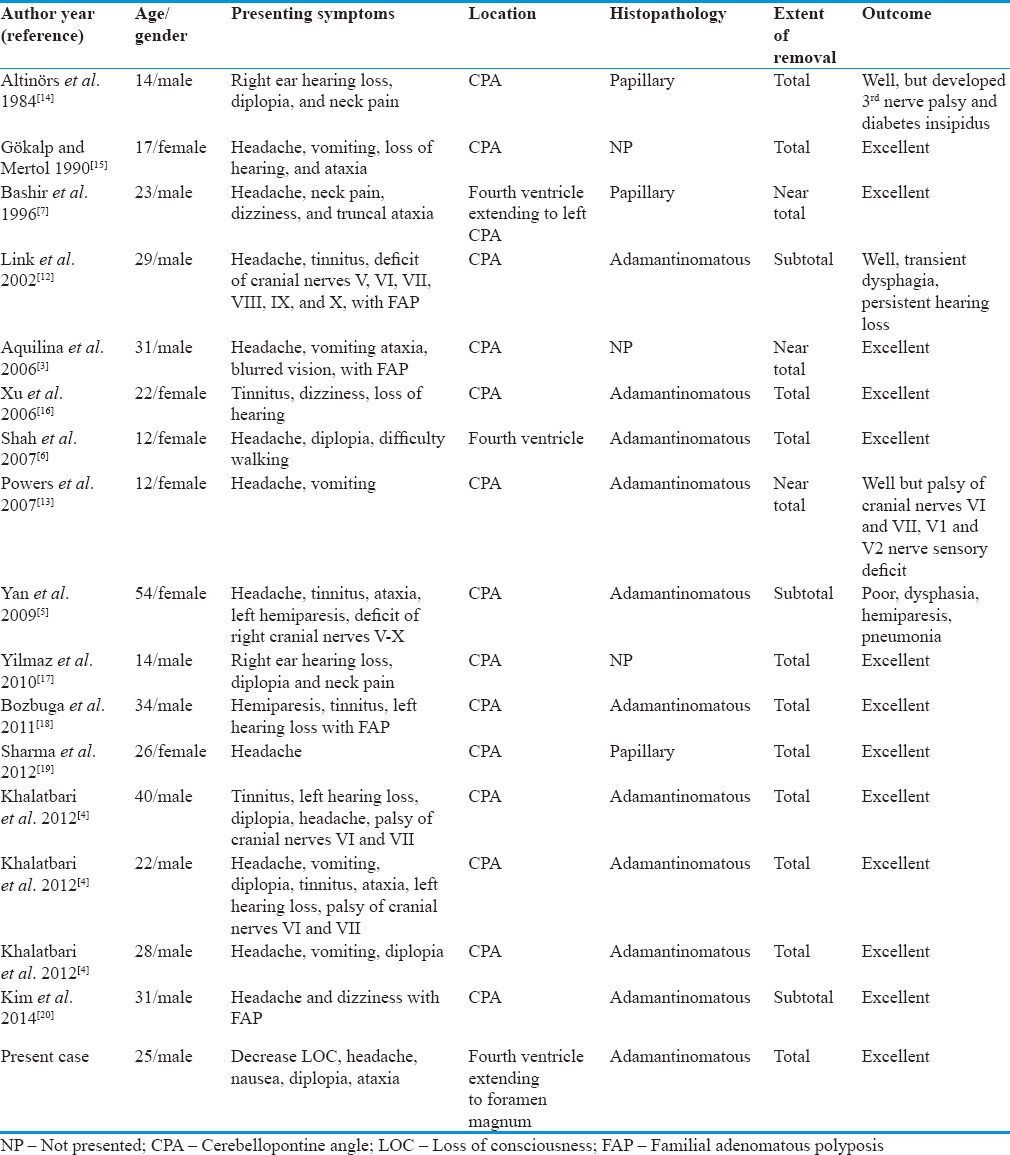
A review of the 16 reported cases of primary posterior fossa craniopharyngioma in addition to our case is summarized in Table 1. Males were slightly more affected than females (11 vs. 6) cases and the age range was 12–54 (median 25 years). Craniopharyngiomas in any location can present with raised intracranial pressure features but tumors in the posterior fossa (compared to the more common suprasellar lesions) are more likely to present with cerebellar disturbances and cranial palsies. The most common surgical approach used was suboccipital technique (16 cases including ours). The excision was total in 11 cases and subtotal in six cases. The pathology of the craniopharyngioma was adamantinomatous of 11 cases, papillary in three cases, and undocumented in three cases. The outcome of surgery was excellent with full recovery of neurological function reported in 13 cases. Transient cranial neuropathies and dysphagia were reported in three cases, and the outcome was considered poor due to motor deficits and pneumonia in only one out of the 17 cases. Follow-up information was only mentioned in eight cases with a follow-up period ranging from 9 weeks to 5 years. None of the reported cases showed evidence of recurrence even in those cases where complete excision was not achieved. Although the number of cases reported was few, we observed a better outcome of the fourth ventricular cases compared to CPA craniopharyngiomas.
Table 1.
Reported surgical cases of primary posterior fossa craniopharyngioma
Conclusion
Primary posterior fossa craniopharyngioma is a rare entity with only 16 cases published in the literature up to date. It is even rarer for craniopharyngioma to originate from the fourth ventricle. We report the third such case in the literature. Craniopharyngioma should be included in differential diagnosis of CPA and fourth ventricular tumors in adolescent and adult patients. Early diagnosis and total resection are associated with favorable outcome.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Kuratsu J, Ushio Y. Epidemiological study of primary intracranial tumors in childhood. A population-based survey in Kumamoto Prefecture, Japan. Pediatr Neurosurg. 1996;25:240–6. doi: 10.1159/000121132. [DOI] [PubMed] [Google Scholar]
- 2.Bunin GR, Surawicz TS, Witman PA, Preston-Martin S, Davis F, Bruner JM. The descriptive epidemiology of craniopharyngioma. J Neurosurg. 1998;89:547–51. doi: 10.3171/jns.1998.89.4.0547. [DOI] [PubMed] [Google Scholar]
- 3.Aquilina K, O’Brien DF, Farrell MA, Bolger C. Primary cerebellopontine angle craniopharyngioma in a patient with Gardner syndrome. Case report and review of the literature. J Neurosurg. 2006;105:330–3. doi: 10.3171/jns.2006.105.2.330. [DOI] [PubMed] [Google Scholar]
- 4.Khalatbari MR, Borghei-Razavi H, Samadian M, Moharamzad Y, Schick U. Isolated primary craniopharyngioma in the cerebellopontine angle. J Clin Neurosci. 2012;19:1516–9. doi: 10.1016/j.jocn.2011.09.029. [DOI] [PubMed] [Google Scholar]
- 5.Yan Y, Tang WY, Yang G, Zhong D. Isolated cerebellopontine angle craniopharyngioma. J Clin Neurosci. 2009;16:1655–7. doi: 10.1016/j.jocn.2009.02.029. [DOI] [PubMed] [Google Scholar]
- 6.Shah GB, Bhaduri AS, Misra BK. Ectopic craniopharyngioma of the fourth ventricle: Case report. Surg Neurol. 2007;68:96–8. doi: 10.1016/j.surneu.2006.11.073. [DOI] [PubMed] [Google Scholar]
- 7.Bashir EM, Lewis PD, Edwards MR. Posterior fossa craniopharyngioma. Br J Neurosurg. 1996;10:613–5. doi: 10.1080/02688699646970. [DOI] [PubMed] [Google Scholar]
- 8.Russel DS, Rubinstein LJ. Neoplasms of the sellar region. In: McLendon RE, editor. Pathology of Tumors of the Nervous System. 7th ed. London: Arnold; 2006. pp. 663–764. [Google Scholar]
- 9.Haupt R, Magnani C, Pavanello M, Caruso S, Dama E, Garrè ML. Epidemiological aspects of craniopharyngioma. J Pediatr Endocrinol Metab. 2006;19(Suppl 1):289–93. [PubMed] [Google Scholar]
- 10.Carmel PW, Antunes JL, Chang CH. Craniopharyngiomas in children. Neurosurgery. 1982;11:382–9. doi: 10.1227/00006123-198209000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Sener RN, Kismali E, Akyar S, Selcuki M, Yalman O. Large craniopharyngioma extending to the posterior cranial fossa. Magn Reson Imaging. 1997;15:1111–2. doi: 10.1016/s0730-725x(97)00137-9. [DOI] [PubMed] [Google Scholar]
- 12.Link MJ, Driscoll CL, Giannini C. Isolated, giant cerebellopontine angle craniopharyngioma in a patient with Gardner syndrome: case report. Neurosurgery. 2002;51:221–5. doi: 10.1097/00006123-200207000-00033. [DOI] [PubMed] [Google Scholar]
- 13.Powers CJ, New KC, McLendon RE, Friedman AH, Fuchs HE. Cerebellopontine angle craniopharyngioma: Case report and literature review. Pediatr Neurosurg. 2007;43:158–63. doi: 10.1159/000098394. [DOI] [PubMed] [Google Scholar]
- 14.Altinörs N, Senveli E, Erdogan A, Arda N, Pak I. Craniopharyngioma of the cerebellopontine angle. Case report. J Neurosurg. 1984;60:842–4. doi: 10.3171/jns.1984.60.4.0842. [DOI] [PubMed] [Google Scholar]
- 15.Gökalp HZ, Mertol T. Cerebellopontine angle craniopharyngioma. Neurochirurgia (Stuttg) 1990;33:20–1. doi: 10.1055/s-2008-1053548. [DOI] [PubMed] [Google Scholar]
- 16.Xu F, Liu X, Xu ZA. A case of ectopic craniopharyngioma. Chin J Neurosurg. 2006;21:762. [Google Scholar]
- 17.Yilmaz C, Altinors N, Sonmez E, Gulsen S, Caner H. Rare lesions of the cerebellopontine angle. Turk Neurosurg. 2010;20:390–7. doi: 10.5137/1019-5149.JTN.2961-10.0. [DOI] [PubMed] [Google Scholar]
- 18.Bozbuga M, Turan Suslu H, Hicdonmez T, Bayindir C. Primary cerebellopontine angle craniopharyngioma in a patient with Gardner syndrome. J Clin Neurosci. 2011;18:300–1. doi: 10.1016/j.jocn.2010.06.006. [DOI] [PubMed] [Google Scholar]
- 19.Sharma M, Mally R, Velho V, Hrushikesh K. Primary isolated cerebellopontine angle papillary craniopharyngioma. Neurol India. 2012;60:438–9. doi: 10.4103/0028-3886.100727. [DOI] [PubMed] [Google Scholar]
- 20.Kim MS, Kim YS, Lee HK, Lee GJ, Choi CY, Lee CH. Primary intracranial ectopic craniopharyngioma in a patient with probable Gardner's syndrome. J Neurosurg. 2014;120:337–41. doi: 10.3171/2013.10.JNS131401. [DOI] [PubMed] [Google Scholar]


