Abstract
Pituitary apoplexy is a rare clinical presentation caused by infarction of the pituitary gland or adenoma with or without hemorrhage. Although pituitary apoplexy is usually spontaneous, one of the predisposing factors is treatment with dopamine agonists, especially bromocriptine. The occurrence of apoplexy during cabergoline therapy is reported much less frequently. In this article, we report a 34-year-old man with macroprolactinomas who developed sudden visual deterioration due to pituitary apoplexy 1 year after initiation of cabergoline therapy. He was treated via endoscopic trans-sphenoidal surgery and his visual status recovered dramatically.
Keywords: Cabergoline, pituitary adenoma, pituitary apoplexy, prolactinoma
Introduction
Pituitary apoplexy is an acute clinical syndrome resulting from infarction of the pituitary adenoma with or without hemorrhage.[1] It is relatively uncommon presentation of pituitary adenomas that may lead to severe neurological morbidities and even death. Sudden onset of a headache, nausea, vomiting, deterioration of visual field and acuity and even blindness, diplopia, ophthalmoplegia, and altered mental status are the most common presentations.[2] Subclinical apoplexy may occur in 25% of cases and is more common than classical apoplexy. It is characterized by intratumoral hemorrhage and necrosis without the common presentations of apoplexy.[3]
Apoplexy may occur spontaneously or as a result of numerous predisposing factors, but the majority of patients do not have any specific cause.[1,4] Head trauma, diabetes mellitus, systemic arterial hypertension or hypotension, radiotherapy, pituitary dynamic tests, recent surgery, thrombocytopenia, coagulation disorders, and medications such as aspirin, estrogens, anticoagulant agents, and dopamine agonists (DAs) all have been reported as the predisposing factors of pituitary apoplexy.[1,2,3,4,5,6,7,8,9]
Bromocriptine is a DA commonly used as the primary therapy for prolactinomas. Cabergoline is a new DA that is proven to be more effective than bromocriptine in the treatment of prolactin-secreting adenomas while having fewer side effects.[5] Most of the reports of apoplexy in prolactinomas are related to treatment with bromocriptine, and there are very fewer reports of cabergoline-induced apoplexy.[4,5,6,7,8] We report a patient with macroprolactinoma who developed apoplexy about 1 year after cabergoline treatment and was successfully treated by endoscopic transsphenoidal surgery.
Case Report
A 34-year-old otherwise healthy man complained of a headache, sexual impotence, and visual loss and was diagnosed to have a macroprolactinoma from about 1 year ago [Figure 1].
Figure 1.
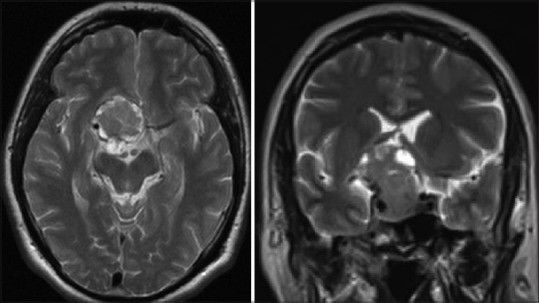
Coronal and Axial brain magnetic resonance imaging at the time of initial diagnosis
The pituitary hormonal assays were normal except an elevated serum prolactin level (358 ng/ml, with the normal range of 3–25 ng/ml).
Medical treatment with cabergoline was started on 1 mg twice a week and resulted in the decrease of the serum prolactin levels down to the normal range (21 ng/ml), and improvement of the visual status of the patient. Control magnetic resonance imaging (MRI) was planned, but the patient did not come for follow-up visits.
After about 1 year of cabergoline therapy, the patient presented to our Emergency Department with a severe headache and visual deterioration, especially in the right eye. Physical examination showed bilateral relative afferent papillary defect more severe on the right side (3+) and a visual acuity of count finger from 30 cm on the right side and 6/10 on the left.
Urgent brain MRI and computed tomography scan were done, which revealed massive intratumoral hemorrhage [Figure 2a–c]. The visual field study showed marked restriction of the visual field, more prominent on the right side [Figure 2d].
Figure 2.
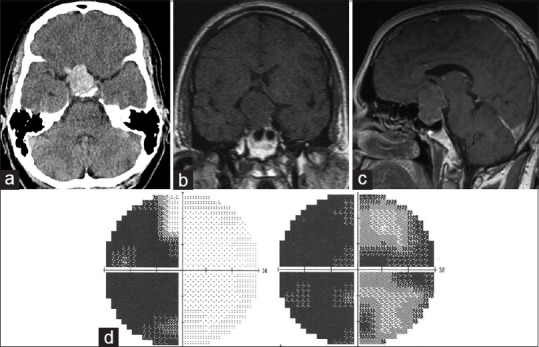
(a) Brain computed tomography scan. (b and c) Sagittal and coronal brain magnetic resonance imaging showing intra-tumoral hemorrhage and re-expansion of the tumor capsule. (d) The preoperative visual perimetry that shows bilateral visual loss with the right eye prominence
The patient did not have any precipitating factors except the cabergoline usage. Replacement therapy with stress dose of steroid and thyroid hormone was started in the Emergency Department and the patient transferred to the operating theater for trans-sphenoidal evacuation of hematoma and tumor resection. The tumor was soft and reddish with both solid and grossly hemorrhagic components and was gently removed by suction and ring curettes under endoscopic view using 0° and 30° lenses. The patient visual field and acuity improved dramatically just after the surgery [Figure 3] and the postoperative course was uneventful.
Figure 3.
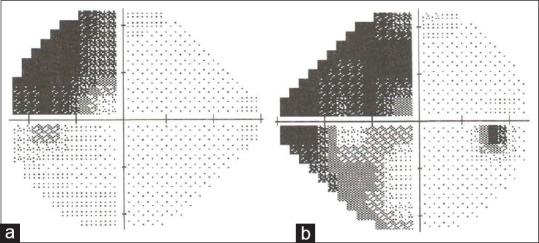
Left (a) and right (b) postoperative perimetry depicting remarkable improvement of the visual fields
An early postoperative brain MRI confirmed radical tumor removal and decompression of the optic nerves [Figure 4]. The patient's pituitary axis hormones remained normal, and the replacement therapy was tapered. The histopathologic evaluation reported hemorrhagic pituitary adenoma that proved to be prolactinoma after immunohistochemical staining for pituitary hormones. Until now (3 months after the operation), the serum prolactin level stayed in the normal range while receiving cabergoline 0.5 mg/week.
Figure 4.
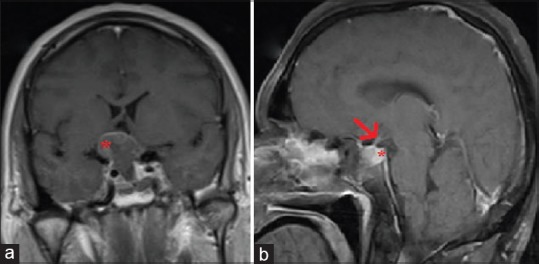
(a) Coronal view of the gadolinium-enhanced early postoperative brain magnetic resonance imaging. There is a small shell of tumor remnant (a: asterix) at the floor of the third ventricle abutting the hypothalamus. (b) Sagittal section of the left side of the sellar region showing that the pituitary stalk (b: arrow) and gland (b: asterix) have been well preserved
Discussion
Infarction of pituitary adenoma is the product of an imbalance between their high rate of demand for nutrientsin adenomas and their inherently limited blood supply that makes them vulnerable to infarction. Hypermetabolism of pituitary adenomas has been documented by the high uptake of metabolic tracers such as glucose by the micro and macroadenomasin fluorodeoxyglucose-positron emission tomography scan. Furthermore, there is limited angiogenesis and reduced vessel density with in pituitary adenomas that combined with the high intratumoral pressure, reduce the perfusion of the tumor and enhance the susceptibility to ischemia and infarction.[1]
Administration of DAs is one of the known risk factors for pituitary apoplexy. DAs promote inhibition of prolactin release. In addition, DA promotes tumor regression due to lactotroph cell size reduction and degenerative and necrotic changes in tumor cells. The bromocriptine-induced degenerative and necrotic changes of tumor cells with subsequent fibrosis raise the possibility of the influence of bromocriptine in the development of intratumoral hemorrhage and consequent pituitary apoplexy.[6] This association has been extensively described for bromocriptine. Cabergoline acts in the same way as bromocriptine to shrink prolactinomas by causing apoptosis of lactotroph cells.
In a systematic review by Carija and Vucina,[6] it was reported that apoplexy appears to be more frequent in among macroprolactinomas than microprolactinomas and also within the first 1½ year from the beginning of treatment with DA. Nevertheless, the clinically manifested pituitary tumor apoplexy appears in a relatively small percentage of prolactinomas treated with DA.
In 2004, Knoepfelmacher et al.[5] reported a case of apoplexy 12 months after initiation of cabergoline treatment as, a rare late manifestation following tumor mass reduction. In 2007 Balarini Lima et al.[4] reported three cases of cystic prolactin-secreting macroadenomas, who developed pituitary apoplexy 7, 12 and 32 weeks after beginning of treatment with cabergoline. Although a greater incidence of pituitary apoplexy in cystic adenomas comparing to solid adenomas has not been reported, these cystic areas may reflect previous intratumoral hemorrhage and thus, may alarm a higher likelihood of occurrence of overt apoplexy in the future.
In this article, we reported a rare case of pituitary apoplexy occurring more than 1 year after treatment with cabergoline was started. In our case, there was no cystic appearance of the tumor in previous imaging studies. Despite presenting with dramatic loss of visual field and acuity, the visual status of our patient recovered markedly following endoscopic trans-sphenoidal surgery. In contrary to some previous reports of successful conservative management of pituitary apoplexy, this report may highlight the merits of timely surgical decompression in the restoration of visual status after apoplexy of pituitary adenomas even the prolactinoma subtype.[3,5]
Conclusion
Pituitary adenomas undergo infarction-pituitary apoplexy-mainly because of their inherent physiology and intrinsic features. Nevertheless, there are some known risk factors for apoplexy and DA administration is one of them. Because of high mortality and morbidity rate of apoplexy, it should be kept in mind that close follow-up is required when treatment with bromocriptine or cabergoline is attempted for prolactinoma. On occurrence of clinically overt apoplexy we recommend timely surgical decompression as the best therapeutic option for the patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Jahangiri A, Clark AJ, Han SJ, Kunwar S, Blevins LS Jr, Aghi MK. Socioeconomic factors associated with pituitary apoplexy. J Neurosurg. 2013;119:1432–6. doi: 10.3171/2013.6.JNS122323. [DOI] [PubMed] [Google Scholar]
- 2.Chng E, Dalan R. Pituitary apoplexy associated with cabergoline therapy. J Clin Neurosci. 2013;20:1637–43. doi: 10.1016/j.jocn.2013.02.027. [DOI] [PubMed] [Google Scholar]
- 3.Singh P, Singh M, Cugati G, Singh AK. Bromocriptine or cabergoline induced pituitary apoplexy: Rare but life-threatening catastrophe. J Hum Reprod Sci. 2011;4:59. doi: 10.4103/0974-1208.82367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Balarini Lima GA, Machado Ede O, Dos Santos Silva CM, Filho PN, Gadelha MR. Pituitary apoplexy during treatment of cystic macroprolactinomas with cabergoline. Pituitary. 2008;11:287–92. doi: 10.1007/s11102-007-0046-6. [DOI] [PubMed] [Google Scholar]
- 5.Knoepfelmacher M, Gomes MC, Melo ME, Mendonca BB. Pituitary apoplexy during therapy with cabergoline in an adolescent male with prolactin-secreting macroadenoma. Pituitary. 2004;7:83–7. doi: 10.1007/s11102-005-5349-x. [DOI] [PubMed] [Google Scholar]
- 6.Carija R, Vucina D. Frequency of pituitary tumor apoplexy during treatment of prolactinomas with dopamine agonists: A systematic review. CNS Neurol Disord Drug Targets. 2012;11:1012–4. doi: 10.2174/1871527311211080011. [DOI] [PubMed] [Google Scholar]
- 7.Oldfield EH, Merrill MJ. Apoplexy of pituitary adenomas: The perfect storm. J Neurosurg. 2015;122:1444–9. doi: 10.3171/2014.10.JNS141720. [DOI] [PubMed] [Google Scholar]
- 8.Singh TD, Valizadeh N, Meyer FB, Atkinson JL, Erickson D, Rabinstein AA. Management and outcomes of pituitary apoplexy. J Neurosurg. 2015;122:1450–7. doi: 10.3171/2014.10.JNS141204. [DOI] [PubMed] [Google Scholar]
- 9.Turgut M, Ozsunar Y, Basak S, Güney E, Kir E, Meteoglu I. Pituitary apoplexy: An overview of 186 cases published during the last century. Acta Neurochir (Wien) 2010;152:749–61. doi: 10.1007/s00701-009-0595-8. [DOI] [PubMed] [Google Scholar]


