Abstract
Background
This study aimed to explore the feasibility and efficacy of bone cement-augmented short-segmental pedicle screw fixation in treating Kümmell disease.
Material/Methods
From June 2012 to June 2015, 18 patients with Kümmell disease with spinal canal stenosis were enrolled in this study. Each patient was treated with bone cement-augmented short-segment fixation and posterolateral bone grafting, and posterior decompression was performed when needed. All patients were followed up for 12–36 months. We retrospectively reviewed outcomes, including the Oswestry disability index (ODI), visual analog scale (VAS) score, anterior and posterior heights of fractured vertebrae, kyphotic Cobb angle, and neurological function by Frankel classification.
Results
The VAS grades, ODI scores, anterior heights of affected vertebrae, and kyphotic Cobb angles showed statistically significant differences between pre- and postoperative and between preoperative and final follow-up values (P<0.05), whereas the differences between postoperative and final follow-up values were not statistically significant (P>0.05). The differences between posterior vertebral heights at each time point were not statistically significant (P>0.05). Improved neurological function was observed in 12 cases at final follow-up. Three cases had complications, including asymptomatic cement leakage in 2 patients and delayed wound infection in 1 patient.
Conclusions
Bone cement-augmented short-segment pedicle screw fixation is safe and effective for treating Kümmell disease, and can achieve satisfactory correction of kyphosis and vertebral height, with pain relief and improvement in neurological function, with few complications.
MeSH Keywords: Bone Cements, Bone Screws, Osteoporotic Fractures, Spine
Background
Kümmell disease as a complication of osteoporotic vertebral fracture (OVF) is increasingly common [1,2]. Although most OVFs can be treated conservatively with bed rest, analgesics, and use of a brace, approximately 10% or more develop nonunion [3,4]. This figure may not represent the true incidence because many asymptomatic or unrecognized cases are not included. Since Kümmell first described the condition in 1891, the literature has referred to Kümmell disease as delayed osteonecrosis after trauma [5–7],nonunion of compression fracture [1,8,9], delayed collapse of OVF [10,11], intravertebral pseudarthrosis [12,13], and vertebral vacuum sign [14,15]. Although the concept and diagnosis of Kümmell disease are ambiguous, more cases have been recognized with advances in radiographic evaluation of vertebral status, particularly with magnetic resonance imaging (MRI) [16].
No standard or single effective treatment for Kümmell disease exists. Nonsurgical treatment includes bed rest, lumbar traction, use of a brace, analgesics, drugs for osteoporosis, and osteoanabolic therapy. In general, conservative treatments have usually been less effective, and carry a risk for delayed neurological deficits [17,18]. Most surgeons have suggested that Kümmell disease should be treated by operative intervention. Various surgical options have been developed, including percutaneous kyphoplasty (PKP), percutaneous vertebroplasty (PVP), and anterior-only, posterior-only, and combined anterior and posterior procedures [19–22]. For stages I and II Kümmell disease, PKP and PVP have achieved good pain relief, vertebral body height restoration, and kyphosis deformity correction [23–25]. For stage III patients with spinal canal stenosis, particularly those with nerve damage, PKP or PVP are not effective, and have a high risk of cement leakage, with the potential risk of severe neurological damage. Traditional anterior or posterior decompression with bone grafting, and combined anterior and posterior procedures have been described, but the surgery is prolonged, with more blood loss and multiple complications [19–22]. Therefore, a safe, effective, and less invasive treatment approach for Kümmell disease is needed. Satisfactory results have been achieved with bone cement-augmented percutaneous short-segment screw fixation in patients with severe osteoporosis [26]. However, no study has investigated the efficacy of this procedure for Kümmell disease with spinal canal stenosis. This procedure is less traumatic than internal fixation surgery alone and may be very beneficial in elderly patients with comorbidities.
We report our experience of treatment for Kümmell disease using bone cement-augmented short-segment pedicle screw fixation. This study aimed to explore the clinical efficacy of the surgical procedure in treating Kümmell disease with spinal canal stenosis.
Material and Methods
Ethics statement
This retrospective study was approved by the Ethics Committee of Honghui Hospital Affiliated to Xi’an Jiaotong University. Written consents were obtained from all patients.
Patients
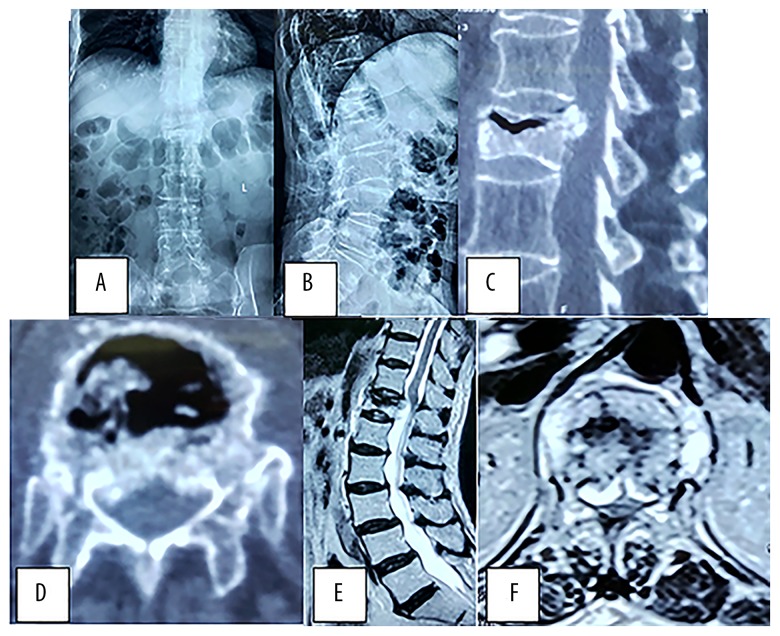
From June 2012 to June 2015, 18 patients with stage III Kümmell disease with posterior wall collapse and spinal canal stenosis were studied in our center. There were 7 men and 11 women, with a mean age of 71.7 years (range: 58 to 82 years). The patients had different degrees of osteoporosis, and the lumbar spine bone mineral density T score ranged from −2.7 to −4.5 standard deviation (SD), with mean of −3.6 SD. Fourteen cases had minor injuries (9 due to falls and 5 from lifting weights). The symptom duration in 18 patients ranged from 1 to 7 months, with a mean of 3.7 months. All had severe back pain relieved or aggravated by positional changes. All underwent conservative treatment for at least 1 month before admission. Twelve patients had a neurological deficit, with pain, numbness, or weakness of the lower limbs. Seven had hypertension, 3 had diabetes mellitus, and 2 had heart disease. The levels of diseased vertebrae were as follows: L2 (2 cases), L1 (3 cases), T12 (8 cases), T11 (3 cases), T10 (1 case), T9 (1 case). Each patient had only 1 affected vertebral body. Neurological function was divided into B (2 cases), C (4 cases), D (6 cases), and E grades (6 cases), based on the Frankel classification. The general patient data are shown in Table 1. All patients underwent X-ray, MRI, and computed tomography (CT) imaging preoperatively. Radiographs demonstrated burst fractures with a vacuum phenomenon in all patients (Figure 1A, 1B). An intravertebral vacuum cleft (IVC), sclerosis at the fracture edge, posterior wall breakage, and spinal canal stenosis were confirmed with CT (Figure 1C, 1D). MRI showed a limited fluid or gas signal and spinal cord compression (Figure 1E, 1F). The disease was diagnosed by combining the results of the clinical examination and radiologic findings. Patients with previous spine surgery, infection, or tumor were excluded.
Table 1.
General data of patients.
| Case | Gender | Age (Year) | Trauma History | Medical History (Month) | Duration of Follow-up (Month) | Damaged Segmet | BMD (T score) | Comorbidity |
|---|---|---|---|---|---|---|---|---|
| 1 | Female | 72 | Fall injury | 3 | 19 | T12 | −3.5 | Hypertension |
| 2 | Female | 69 | Fall injury | 1 | 24 | L1 | −2.9 | Hypertension |
| 3 | Male | 78 | Lifting weight | 4 | 13 | T11 | −4.2 | No |
| 4 | Female | 75 | No | 2 | 28 | T12 | −3.5 | Hypertension |
| 5 | Male | 64 | Lifting weight | 6 | 31 | L2 | −2.7 | Heart disease |
| 6 | Female | 80 | Fall injury | 3 | 16 | T9 | −3.7 | No |
| 7 | Female | 58 | Lifting weight | 5 | 36 | T12 | −3.2 | Diabetes mellitus |
| 8 | Female | 70 | Fall injury | 4 | 25 | T11 | −3.8 | Hypertension |
| 9 | Male | 73 | Fall injury | 3 | 18 | L1 | −4.3 | Hypertension |
| 10 | Male | 82 | No | 2 | 15 | T12 | −3.7 | No |
| 11 | Female | 67 | Lifting weight | 4 | 28 | L1 | −3.2 | Heart disease |
| 12 | Female | 74 | No | 5 | 21 | T10 | −4.5 | No |
| 13 | Male | 69 | Fall injury | 7 | 30 | T12 | −3.7 | Diabetes mellitus |
| 14 | Female | 72 | Fall injury | 1 | 27 | T11 | −3.5 | Hypertension |
| 15 | Male | 79 | No | 2 | 12 | L2 | −4.0 | No |
| 16 | Female | 64 | Fall injury | 6 | 36 | T12 | −3.4 | Diabetes mellitus |
| 17 | Female | 70 | Lifting weight | 3 | 24 | T12 | −2.9 | No |
| 18 | Male | 75 | Fall injury | 5 | 19 | T12 | −4.3 | Hypertension |
BMD – bone mineral density.
Figure 1.
Preoperative X-ray and CT show L1 burst fracture with intravertebral vacuum cleft, and MRI showed a limited low signal and spinal cord compression.
Surgical procedures
All patients were placed in a prone position on the operating table and underwent surgery under general anesthesia. Pillows were placed under the affected vertebral segment to enable spinal column hyperextension. This position was conducive to recovery of the vertebral height. A posterior midline approach was used to expose the spinous processes, lamina, and facet joint; 6 pedicle screws were inserted bilaterally into 1 level above, 1 level below, and the collapsed vertebra itself, and then 2 rods were used to obtain further recovery of the vertebral height. Wide decompressive laminectomy of the diseased vertebra was necessary for patients with neurological deficits, and intraoperative exploration showed no spinal cord compression. Polymethylmethacrylate bone cement was injected slowly when it became doughy and could stand at the tip of the bone cement inserter; this process was monitored under fluoroscopic control in the lateral plane. The cavity of the IVC was filled with cement postoperatively. Autogenous bone grafts or allografts were used to facilitate posterolateral fusion. A cross-link was used routinely in each patient. The incision was rinsed and hemostasis achieved. The wound was closed using a layer-to-layer suture.
Effectiveness evaluation
All patients underwent X-ray, MRI, and CT preoperatively, as well as anteroposterior and lateral X-rays postoperatively and during follow-up. Postoperative CT or MRI was performed selectively according to the patient’s condition. Kyphotic Cobb angles and anterior and posterior heights of fractured vertebrae were measured with a lateral X-ray. Back pain was assessed with the visual analog scale (VAS) score. Impact on the patient’s daily life was assessed using the Oswestry disability index (ODI). Neurological function was assessed with the Frankel classification. Preoperatively, one day after surgery, and at the final follow-up, the measurement of VAS score, ODI, anterior and posterior heights of fractured vertebrae, kyphotic Cobb angle, and neurological function were used to evaluate changes. Additionally, Intraoperative and postoperative complications were recorded.
Statistical analyses
All analyses were performed using IBM SPSS Statistics for Windows, version 19.0 (IBM Corp, USA). All data were expressed as mean ± SD. The paired t-test was performed to compare the differences in every index between 2 time points in this study. P<0.05 was considered statistically significant.
Results
All patients tolerated the procedure well. Follow-up was performed on every patient. The follow-up period ranged from 12 to 36 months, with a mean of 23.4 months. The mean operative time was 114.6 min (97–135), mean blood loss was 229.6 ml (203–272), mean volume of cement was 9.8 ml (8.5–11.5), and the mean hospital stay was 7.9 days (6–11).
The VAS grades, ODI scores, anterior heights of affected vertebrae, and kyphotic Cobb angles showed statistically significant differences between pre- and postoperative and between preoperative and final follow-up values (P<0.05; Table 2), whereas the differences between postoperative and final follow-up values were not statistically significant (P>0.05; Table 2). The differences between posterior vertebral heights at each time point were not statistically significant (P>0.05; Table 2).
Table 2.
Evaluation indexs at preoperation, postoperation, and final follow-up.
| VAS score | ODI score (%) | Anterior vertebral height (mm) | Posterior vertebral height (mm) | Kyphotic cobb angle (°) | |
|---|---|---|---|---|---|
| Preoperation | 8.1±0.6 | 84.1±6.1 | 11.6±1.7 | 20.5±2.0 | 29.9±1.8 |
| Postoperation | 2.7±0.4* | 31.0±3.1* | 20.1±2.0* | 20.7±1.7*** | 12.3±1.8* |
| Final Follow-up | 2.9±0.7*,** | 32.2±3.8*,** | 19.4±2.9*,** | 20.3±2.5**,**** | 12.9±2.7*,** |
P<0.05 vs. preoperation values;
P>0.05 vs. postoperation values;
P>0.05 vs. preoperation values;
P>0.05 vs. preoperation values.
VAS – visual analog scale, ODI – Oswestry Disability Index.
No neurological deterioration occurred postoperatively. Preoperatively, neurological function was divided into B (2 cases), C (4 cases), D (6 cases), and E grades (6 cases), based on the Frankel classification. Postoperatively, neurological function was divided into B (1 case), C (3 cases), D (5 cases), and E grades (9 cases). At the final followup, 2, 2, and 14 patients were classified as grades C, D, and E, respectively (Table 3). Improved neurological function was observed in 12 patients at the final follow-up.
Table 3.
Number of patients by Frankel classification at different times.
| Frankel classification | |||||
|---|---|---|---|---|---|
| A | B | C | D | E | |
| Preopreation | 0 | 2 | 4 | 6 | 6 |
| Postoperation | 0 | 1 | 3 | 5 | 9 |
| Final Follow-up | 0 | 0 | 2 | 2 | 14 |
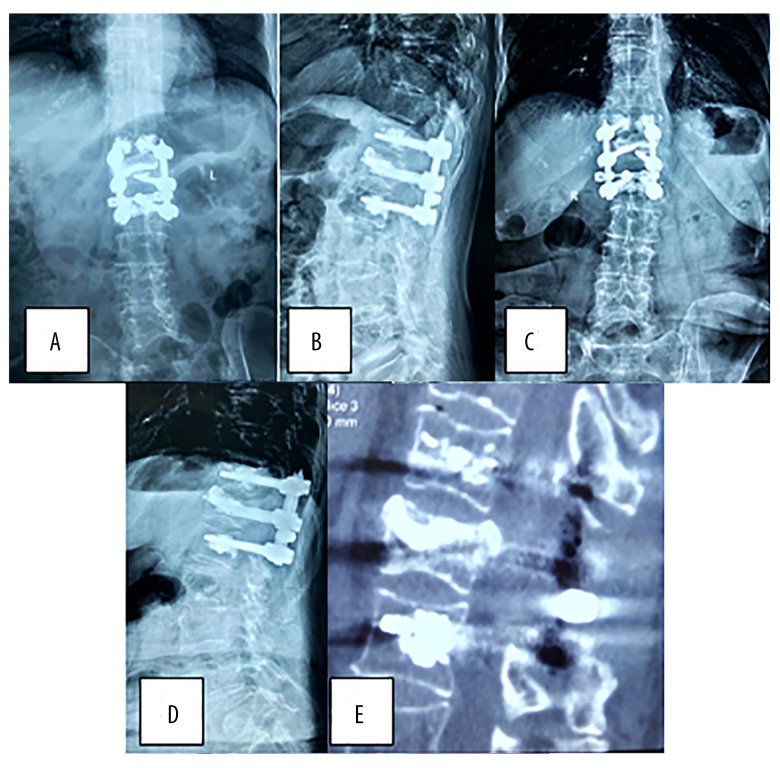
As shown in Figure 2, the postoperative and final follow-up reviews revealed good internal fixation position and satisfactory posterior decompression. No serious intra- or postoperative complications were observed, such as renal failure and cardiopulmonary complications. A small amount of cement leakage occurred in 2 patients, but they were asymptomatic postoperatively. One patient had delayed wound infection, and was cured with conservative treatment. No obvious bone cement displacement occurred at the final follow-up. No loosening, displacement, or fracture of internal fixation occurred by the end of follow-up.
Figure 2.
The postoperative and final follow-up reviews revealed good internal fixation position and satisfactory posterior decompression.
Discussion
Diagnosis of Kümmell disease
Kümmell disease is an uncommon condition, occurring in adults older than 50 years, and mostly in women. The thoracolumbar junction, particularly the T12 vertebra, is the most commonly affected vertebral segment [6,27]. Tsujio reported that the incidence of nonunion was 13.5% after 6 months of conventional conservative treatment and revealed a series of significant risk factors for nonunion, including the presence of a vertebral fracture in the thoracolumbar spine, presence of a middle-column injury, and a confined high-intensity or a diffuse low-intensity area in the fractured vertebrae on T2-weighted MR images [8]. Patients often have a history of minor trauma, or even no trauma history. The etiology and pathology are unclear. Most authors have suggested that Kümmell disease is secondary to ischemic necrosis of the vertebral body, and that vascular injury is responsible for impaired bone healing [5–7,27].
The diagnostic criteria for Kümmell disease remain unclear. Kümmell disease was first diagnosed by Maldague in 1978 as a sign of vertebral collapse, characterized by a gas-density cleft within a transverse separation of the vertebral body [28]. The IVC is a typical manifestation of Kümmell disease on imaging. Of the available imaging techniques, radiographs are the least sensitive for detecting an IVC, CT with coronal and sagittal reconstructed views is better, and MRI is the most sensitive method, as it demonstrates soft tissue characteristics, including marrow edema and fluid within the IVC [9]. Moreover, visualization of an IVC with MRI depends on whether the cleft is filled with gas or fluid. However, some reports suggested that IVC is not a specific sign of Kümmell disease, because a few patients with myeloma and infections also had an IVC [4,29]. The development of Kümmell disease mainly occurs in 3 stages. First, spinal vertebral bodies are slightly injured by minor trauma, and sometimes even with no trauma. Second, vertebral bodies experience dynamic instability in the cleft area, and then fracture and bone collapse occur. In the last stage, the compressed, fractured vertebral body compresses the posterior spinal cord, leading to continuous back pain and other neurologic symptoms [30]. Clinically, Kümmell disease is diagnosed by delayed collapse of the vertebra and dynamic instability, and ultimately progresses to kyphosis with long-term back pain or nerve injury, combined with evidence of an IVC on MRI.
Treatment of Kümmell disease
The treatment of Kümmell disease has been controversial [18,25]. Although the standard treatments require further study, some are accepted by the majority of surgeons. The treatment strategy mainly depends on several factors: age, comorbidities, bone quality, presence of neurological deficits, severity of kyphotic deformity, and pain severity [18,31,32]. For stage I and II patients without spinal canal stenosis, the purpose of the operation is to prevent abnormal movement at the diseased site and restore the sagittal sequence of the spine. The role of PVP and PKP in achieving pain relief, restoring the vertebral body height, and correcting deformity has been widely accepted [23–25]. Because persistent pain in Kümmell disease derives from motion in the IVC, excellent pain relief can be attained when the cleft is stabilized by filling with cement. In contrast, a small number of researchers suggested that vertebroplasty should be carefully considered, because the destructive process may further progress after surgery, with a theoretical risk of secondary displacement of the cement [27,33–35]. Stage III Kümmell disease is characterized by the collapse of the posterior vertebral body wall and the formation of spinal canal stenosis and dural sac compression. However, the progression to cord compression is often slow, and most early cases may not have symptoms of spinal cord injury. For stage III patients with mild stenosis of the spinal canal and without neurological symptoms, the goal of treatment is to relieve back pain and prevent further collapse of the affected vertebra and delayed neurological deficits. However, few reports have discussed treatment for this presentation. PVP or PKP is probably unsuitable, because the surrounding vertebral cortex has already been compromised. The deficit of the posterior vertebral body wall in stage III Kümmell disease is very dangerous, as inserted cement can easily leak out. Internal fixation seems to be necessary in this condition. For stage III patients with severe stenosis of the spinal canal and neurological symptoms, the objective of surgery is to relieve cord compression, eliminate spinal instability, and restore the sagittal balance of the spine [18,25]. Many fixation procedures have been developed to treat this presentation, including anterior-only, posterior-only, and combined anterior and posterior procedures [19–22]. However, these are technically demanding and are associated with multiple complications, which are very dangerous in elderly patients with comorbidities [35].
Techniques in this study
It is often difficult for patients with Kümmell disease to tolerate complex surgeries, because adults older than 50 years are usually affected, and may have many comorbidities or severe osteoporosis. Moreover, fixation surgery and body reconstruction have high complication rates in patients with severe osteoporosis. Therefore, a safe, effective, and less invasive treatment for Kümmell disease is needed. Short-segment, pedicle screw fixation combined with bone cement augmentation and posterolateral bone graft fusion can effectively eliminate intravertebral instability and segment motion. Many reports have suggested that the main factor in delayed neurological deficits following vertebral collapse in the osteoporotic spine is instability of the spinal column at the fracture site, rather than mechanical compression of the spinal cord by bone fragments [36–38]. Second, posterior screw stress is markedly reduced because of the anterior support provided by the intravertebral cement, which can reduce the risk of internal fixation failure. Third, screw loosening or displacement rarely occurs, because bone cement-augmented screws have a strong grip. Fourth, the retention effect of screws can reduce the risk of delayed bone cement displacement. Fifth, the cement leakage rate is visibly decreased; this greatly reduces the potential for nerve injury. Finally, short-segment fixation is not more invasive than instrumentation alone, and provides a shorter operative time and less blood loss, which is particularly important in the elderly with comorbidities. Many fixation procedures have been proposed to reverse the nerve damage in Kümmell disease with spinal canal stenosis. However, these often have high complication rates [31,39]. Three complications were observed in this study, including asymptomatic cement leakage in 2 patients, and delayed wound infection in 1 patient. Compared with other surgical procedures, bone cement-augmented short-segment pedicle screw fixation had fewer complications.
However, some reports have suggested that the improvement in vertebral height and kyphosis angle gradually reverse after surgery, with a risk of further kyphotic deformity because of aggravated osteoporosis [27,32,35]. Compared with the findings on the first postoperative day, a small loss in kyphosis angle and height of the affected vertebra at the final follow-up was observed in this study, but the differences had no statistical significance (P>0.05). This may be related to the short follow-up time; hence, further observation is needed. Furthermore, previous studies also suggested that the severity of back pain might be unrelated to the severity of the kyphosis or the vertebral height loss [21,40,41].
This study has some limitations. First, this was a retrospective, single-center study, and no method was adopted to ensure unbiased randomization. Second, the sample size was small, and long-term clinical outcomes and complications were not clear due to insufficient follow-up duration. Third, a prospective, randomized controlled study would better assess the feasibility and efficacy of bone cement-augmented short-segment screw fixation for Kümmell disease.
Conclusions
Bone cement-augmented short-segment pedicle screw fixation is a safe and effective operation for Kümmell disease, and can achieve satisfactory correction of kyphosis and vertebral height, with pain relief and improvement of neurological function, with few complications. This procedure is less traumatic than traditional fixation surgery, and can be very beneficial in elderly patients with comorbidities. However, the long-term clinical outcomes and radiological results require further evaluation.
Footnotes
Source of support: This study was supported by the National Natural Science Foundation of China (No. 81472098)
Conflicts of interest
None.
References
- 1.Li D, Huang Y, Yang H, et al. Short-segment pedicle instrumentation with transpedicular bone grafting for nonunion of osteoporotic vertebral fractures involving the posterior edge. Eur J Orthop Surg Traumatol. 2013;23:21–26. doi: 10.1007/s00590-011-0928-1. [DOI] [PubMed] [Google Scholar]
- 2.Kim YC, Kim YH, Ha KY. Pathomechanism of intravertebral clefts in osteoporotic compression fractures of the spine. Spine J. 2014;14:659–66. doi: 10.1016/j.spinee.2013.06.106. [DOI] [PubMed] [Google Scholar]
- 3.Toyone T, Toyone T, Tanaka T, et al. Changes in vertebral wedging rate between supine and standing position and its association with back pain: A prospective study in patients with osteoporotic vertebral compression fractures. Spine (Phila Pa 1976) 2006;31:2963–66. doi: 10.1097/01.brs.0000247802.91724.7e. [DOI] [PubMed] [Google Scholar]
- 4.Feng SW, Chang MC, Wu HT, et al. Are intravertebral vacuum phenomena benign lesions? Eur Spine J. 2011;20:1341–48. doi: 10.1007/s00586-011-1789-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Benedek TG, Nicholas JJ. Delayed traumatic vertebral body compression fracture; Part II: Pathologic features. Semin Arthritis Rheum. 1981;10:271–77. doi: 10.1016/0049-0172(81)90004-4. [DOI] [PubMed] [Google Scholar]
- 6.Young WF, Brown D, Kendler A, Clements D. Delayed post-traumatic osteonecrosis of a vertebral body (Kümmell’s disease) Acta Orthop Belg. 2002;68:13–19. [PubMed] [Google Scholar]
- 7.Lee GW, Yeom JS, Kim HJ, Suh BG. A therapeutic efficacy of the transpedicular intracorporeal bone graft with short-segmental posterior instrumentation in osteonecrosis of vertebral body: A minimum 5-year follow-up study. Spine (Phila Pa 1976) 2013;38:E244–50. doi: 10.1097/BRS.0b013e31827efef2. [DOI] [PubMed] [Google Scholar]
- 8.Tsujio T, Nakamura H, Terai H, et al. Characteristic radiographic or magnetic resonance images of fresh osteoporotic vertebral fractures predicting potential risk for nonunion: A prospective multicenter study. Spine (Phila Pa 1976) 2011;36:1229–35. doi: 10.1097/BRS.0b013e3181f29e8d. [DOI] [PubMed] [Google Scholar]
- 9.Chen GD, Lu Q, Wang GL, et al. Percutaneous kyphoplasty for Kümmell disease with severe spinal canal stenosis. Pain Physician. 2015;18:E1021–28. [PubMed] [Google Scholar]
- 10.Kim KT, Suk KS, Kim JM, Lee SH. Delayed vertebral collapse with neurological deficits secondary to osteoporosis. Int Orthop. 2003;27:65–69. doi: 10.1007/s00264-002-0418-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nakashima H, Imagama S, Yukawa Y, et al. Comparative study of 2 surgical procedures for osteoporotic delayed vertebral collapse: Anterior and posterior combined surgery versus posterior spinal fusion with vertebroplasty. Spine (Phila Pa 1976) 2015;40:E120–26. doi: 10.1097/BRS.0000000000000661. [DOI] [PubMed] [Google Scholar]
- 12.Jang JS, Kim DY, Lee SH. Efficacy of percutaneous vertebroplasty in the treatment of intravertebral pseudarthrosis associated with noninfected avascular necrosis of the vertebral body. Spine (Phila Pa 1976) 2003;28:1588–92. [PubMed] [Google Scholar]
- 13.Kim HS, Heo DH. Percutaneous pedicle screw fixation with polymethylmethacrylate augmentation for the treatment of thoracolumbar intravertebral pseudoarthrosis associated with Kümmell’s osteonecrosis. Biomed Res Int. 2016;2016:3878063. doi: 10.1155/2016/3878063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pappou IP, Papadopoulos EC, Swanson AN, et al. Osteoporotic vertebral fractures and collapse with intravertebral vacuum sign (Kümmel’s disease) Orthopedics. 2008;31:61–66. doi: 10.3928/01477447-20080101-35. [DOI] [PubMed] [Google Scholar]
- 15.He D, Yu W, Chen Z, et al. Pathogenesis of the intravertebral vacuum of Kümmell’s disease. Exp Ther Med. 2016;12:879–82. doi: 10.3892/etm.2016.3369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen B, Fan S, Zhao F. Percutaneous balloon kyphoplasty of osteoporotic vertebral compression fractures with intravertebral cleft. Indian J Orthop. 2014;48:53–59. doi: 10.4103/0019-5413.125498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fabbriciani G, Pirro M, Floridi P, et al. Osteoanabolic therapy: A non-surgical option of treatment for Kümmell’s disease? Rheumatol Int. 2012;32:1371–74. doi: 10.1007/s00296-010-1408-3. [DOI] [PubMed] [Google Scholar]
- 18.Li H, Liang CZ, Chen QX. Kümmell’s disease, an uncommon and complicated spinal disorder: A review. J Int Med Res. 2012;40:406–14. doi: 10.1177/147323001204000202. [DOI] [PubMed] [Google Scholar]
- 19.Kanayama M, Ishida T, Hashimoto T, et al. Role of major spine surgery using Kaneda anterior instrumentation for osteoporotic vertebral collapse. J Spinal Disord Tech. 2010;23:53–56. doi: 10.1097/BSD.0b013e318193e3a5. [DOI] [PubMed] [Google Scholar]
- 20.Yang DL, Yang SD, Chen Q, et al. The treatment evaluation for osteoporotic Kümmell disease by modified posterior vertebral column resection: Minimum of one-year follow-up. Med Sci Monit. 2018;24:606–12. doi: 10.12659/MSM.902669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang F, Wang D, Tan B, et al. Comparative study of modified posterior operation to treat Kümmell’s disease. Medicine (Baltimore) 2015;94:e1595. doi: 10.1097/MD.0000000000001595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Suk SI, Kim JH, Lee SM, et al. Anterior-posterior surgery versus posterior closing wedge osteotomy in posttraumatic kyphosis with neurologic compromised osteoporotic fracture. Spine (Phila Pa 1976) 2003;28:2170–75. doi: 10.1097/01.BRS.0000090889.45158.5A. [DOI] [PubMed] [Google Scholar]
- 23.Huang Y, Peng M, He S, et al. Clinical efficacy of percutaneous kyphoplasty at the hyperextension position for the treatment of osteoporotic Kümmell disease. Clin Spine Surg. 2016;29:161–66. doi: 10.1097/BSD.0000000000000259. [DOI] [PubMed] [Google Scholar]
- 24.Matsuura M, Fujimoto Y, Yamada K, Nakamae T. Percutaneous vertebroplasty versus balloon kyphoplasty for osteoporotic vertebral fracture with intravertebral cleft. Spine J. 2014;14:S123. [Google Scholar]
- 25.Yang H, Pan J, Wang G. A review of osteoporotic vertebral fracture nonunion management. Spine (Phila Pa 1976) 2014;39:B4–6. doi: 10.1097/BRS.0000000000000538. [DOI] [PubMed] [Google Scholar]
- 26.Park SJ, Kim HS, Lee SK, Kim SW. Bone cement-augmented percutaneous short segment fixation: An effective treatment for Kümmell’s disease? J Korean Neurosurg Soc. 2015;58:54–59. doi: 10.3340/jkns.2015.58.1.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Laredo JD. Expert’s comment concerning Grand Rounds case entitled “Kümmell’s disease: Delayed post-traumatic osteonecrosis of the vertebral body” (by R. Ma, R. Chow, F. H. Shen) Eur Spine J. 2010;19:1071–72. doi: 10.1007/s00586-009-1204-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Maldague BE, Noel HM, Malghem JJ. The intravertebral vacuum cleft: A sign of ischemic vertebral collapse. Radiology. 1978;129:23–29. doi: 10.1148/129.1.23. [DOI] [PubMed] [Google Scholar]
- 29.Malghem J, Maldague B, Labaisse MA, et al. Intravertebral vacuum cleft: Changes in content after supine positioning. Radiology. 1993;187:483–87. doi: 10.1148/radiology.187.2.8475295. [DOI] [PubMed] [Google Scholar]
- 30.Ito Y, Hasegawa Y, Toda K, Nakahara S. Pathogenesis and diagnosis of delayed vertebral collapse resulting from osteoporotic spinal fracture. Spine J. 2002;2:101–6. doi: 10.1016/s1529-9430(01)00165-6. [DOI] [PubMed] [Google Scholar]
- 31.Lee SH, Cho DC, Sung JK. Catastrophic intramedullary hematoma following Kümmell’s disease with large intravertebral cleft. Spine J. 2008;8:1007–10. doi: 10.1016/j.spinee.2007.07.397. [DOI] [PubMed] [Google Scholar]
- 32.Lee SH, Kim ES, Eoh W. Cement augmented anterior reconstruction with short posterior instrumentation: A less invasive surgical option for Kümmell’s disease with cord compression. J Clin Neurosci. 2011;18:509–14. doi: 10.1016/j.jocn.2010.07.139. [DOI] [PubMed] [Google Scholar]
- 33.Wagner AL, Baskurt E. Refracture with cement extrusion following percutaneous vertebroplasty of a large interbody cleft. Am J Neuroradiol. 2006;27:230–31. [PMC free article] [PubMed] [Google Scholar]
- 34.Wang HS, Kim HS, Ju CI, Kim SW. Delayed bone cement displacement following balloon kyphoplasty. J Korean Neurosurg Soc. 2008;43:212–14. doi: 10.3340/jkns.2008.43.4.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhang GQ, Gao YZ, Zheng J, et al. Posterior decompression and short-segmental pedicle screw fixation combined with vertebroplasty for Kümmell’s disease with neurological deficits. Exp Ther Med. 2013;5:517–22. doi: 10.3892/etm.2012.833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sudo H, Ito M, Kaneda K, et al. Anterior decompression and strut graft versus posterior decompression and pedicle screw fixation with vertebroplasty for osteoporotic thoracolumbar vertebral collapse with neurologic deficits. Spine J. 2013;13:1726–32. doi: 10.1016/j.spinee.2013.05.041. [DOI] [PubMed] [Google Scholar]
- 37.Verlaan JJ. Stabilizing osteoporotic thoracolumbar fractures through an anterior or posterior approach: What works best? Spine J. 2013;13:1733–35. doi: 10.1016/j.spinee.2013.07.029. [DOI] [PubMed] [Google Scholar]
- 38.Nakamae T, Fujimoto Y, Yamada K, Matsuura M. The cause of delayed neurologic deficits following osteoporotic vertebral pseudoarthrosis. Spine J. 2014;14:S97. [Google Scholar]
- 39.Nguyen HV, Ludwig S, Gelb D. Osteoporotic vertebral burst fractures with neurologic compromise. J Spinal Disord Tech. 2003;16:10–19. doi: 10.1097/00024720-200302000-00003. [DOI] [PubMed] [Google Scholar]
- 40.Chen L, Dong R, Gu Y, Feng Y. Comparison between balloon kyphoplasty and short-segmental fixation combined with vertebroplasty in the treatment of Kümmell’s disease. Pain Physician. 2015;18:373–81. [PubMed] [Google Scholar]
- 41.Chen C, Chen L, Gu Y, et al. Kyphoplasty for chronic painful osteoporotic vertebral compression fractures via unipedicular versus bipedicular approachment: A comparative study in early stage. Injury. 2010;41:356–59. doi: 10.1016/j.injury.2009.09.021. [DOI] [PubMed] [Google Scholar]