Abstract
Background
Funding for graduate medical education is at risk despite the services provided by residents.
Objective
We quantified the potential monetary value of services provided by on-call orthopedic surgery residents.
Methods
We conducted a prospective, cross-sectional, multicenter cohort study design. Over a 90-day period in 2014, we collected data on consults by on-call orthopedic surgery residents at 4 tertiary academic medical centers in the United States. All inpatient and emergency department consults evaluated by first-call residents during the study period were eligible for inclusion. Based on their current procedural terminology codes, procedures and evaluations for each consult were assigned a relative value unit and converted into a monetary value to determine the value of services provided by residents. The primary outcome measures were the total dollar value of each consult and the percentage of resident salaries that could be funded by the generated value of the resident consult services.
Results
In total, 2644 consults seen by 33 residents from the 4 institutions were included for analysis. These yielded an average value of $81,868 per center for the 90-day study period, that is, $327,471 annually. With a median resident stipend of $53,992, the extrapolated average percentage of resident stipends that could be funded by these consult revenues was 73% of the stipends of the residents who took call or 36% of the stipends of the overall resident cohort.
Conclusions
The potential monetary value generated by on-call orthopedic surgery residents is substantial.
Introduction
The landscape of health care has changed dramatically with the passage of the Affordable Care Act.1,2 Funding of graduate medical education (GME) has also been a topic of intense public debate.2–8 A 2014 report from the Institute of Medicine proposed major changes to the way GME is funded, including transformational and performance-based funding.7
Residents provide services to the most at-risk populations by training disproportionately in medical centers serving urban and underserved patients.9 Their presence increases access to care for many of these patients.
In this study, we sought to quantify the potential monetary value of on-call orthopedic residents across 4 academic medical centers in terms of both work relative value units (wRVUs) and potential billable services in Medicare dollars. Prior studies examining this topic were either single site studies, at the fellow level, and/or limited to the outpatient setting.10–13
Methods
All consults evaluated by 1 of 33 on-call orthopedic surgery residents at each of the 4 urban academic institutions during a 90-day period between September and December 2014 were eligible for inclusion. Consults with incomplete information were excluded from analysis. Consult information was recorded, including date and day of the week of the consult, admission status, diagnosis, primary consulting orthopedic service, procedures performed by the on-call physician, and the patient's payer status.
The consult was assigned an encounter level based on current procedural terminology (CPT) for evaluation and management. Patients requiring a procedure by the on-call resident were assigned a CPT procedure code. Each CPT code and encounter level was then assigned a wRVU according to the January 2014 physician fee schedule.14 We coded procedures that would be followed up by another provider with the –54 modifier, with a reduction in the wRVU value included in the analysis. Total wRVUs per consult were calculated and converted to a dollar amount using the conversion factor ($35.82 per wRVU) in the fee schedule.14 This dollar value per consult was the primary outcome for each consult. We performed a descriptive analysis to evaluate consult characteristics and demographics.
Resident stipend information was obtained from the Association of American Medical Colleges published data.15 The average stipend per program was calculated using postgraduate year 1 (PGY-1) through PGY-5 values for the respective regions of participating programs. We calculated the percentage of the resident salaries that could be funded by the values generated by the value of the on-call residents' work, calculated by summing the 90-day value across the 4 institutions, multiplying it by 4 to annualize it, and dividing that value by an average resident stipend (across the years of training) multiplied by the overall number of residents in the analysis.
The Institutional Review Board at each of the 4 participating sites approved this study, and data use agreements between the centers were established.
Results
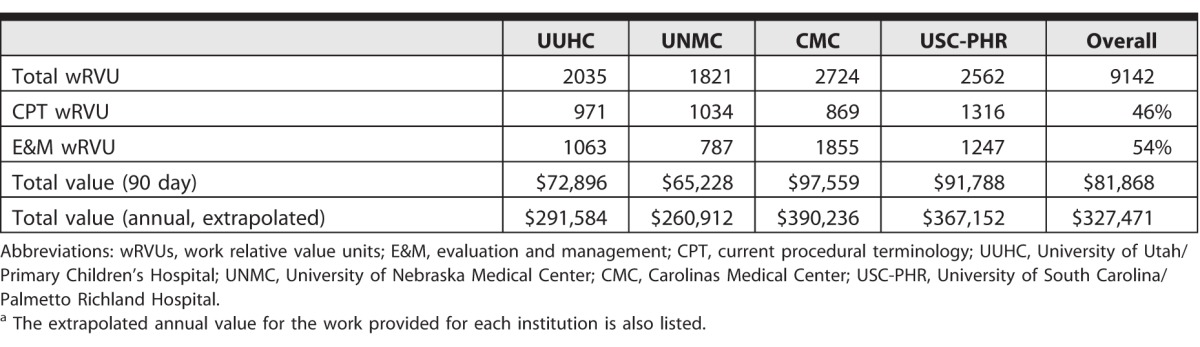
Across the 4 programs, 33 of 80 residents (41%) were in the on-call pool during the study period. During the 90-day period, these residents evaluated 2644 consults, of which 37 (1.4%) did not have complete information and were excluded from the analysis (Table 1). The average number of wRVUs per consult was 3.45. Private insurance (38%, 1004 of 2644), Medicare (21%, 555 of 2644), and Medicaid (15%, 397 of 2644) were the most common payers. Consults showed little variation based on day of the week. Over the 90-day study period, the average value generated per center was $81,868 (range, $65,228–$97,559; Table 2), and the overall average financial value per resident was $39,455. This amount represents 73% of the stipends of the resident group who took call and an average of 36% of the total amount for the stipends for all residents in the 4 programs (range, 21%–70%).15
Table 1.
Demographics of Consult by Institution and in Aggregate
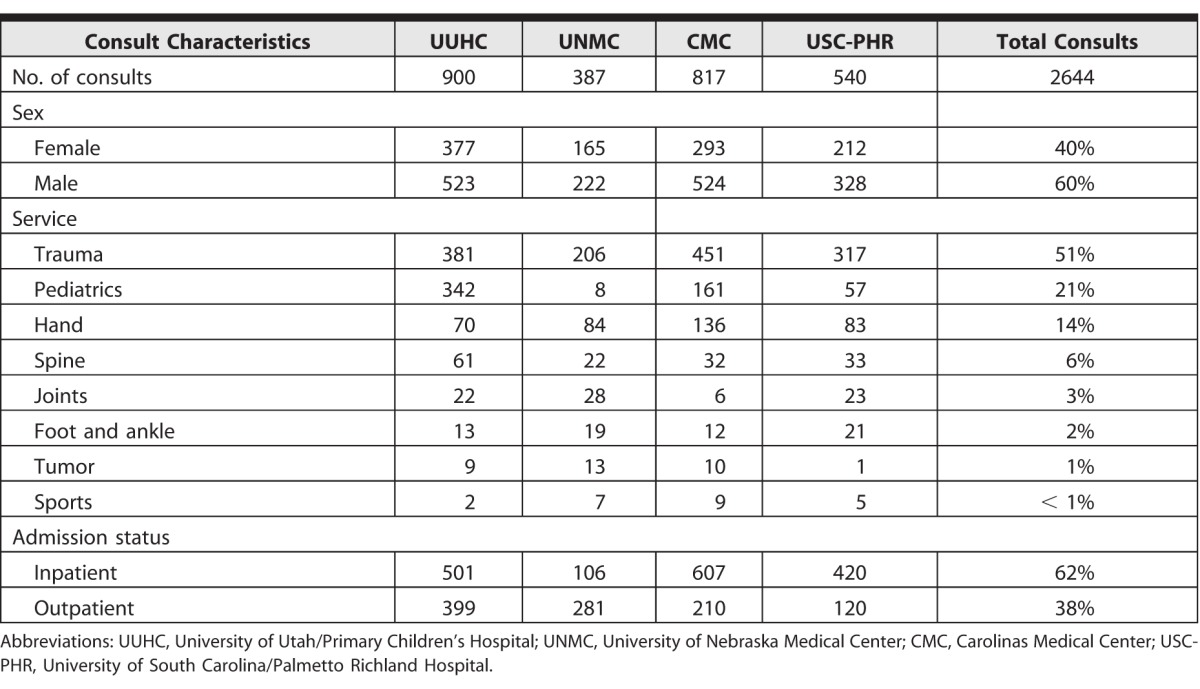
Table 2.
Total wRVUs Listed for Each Institution for E&M and CPT Codesa
Discussion
In this study of 4 centers, orthopedic residents provided considerable patient services while on call. When quantified into a monetary value based on Medicare reimbursement rates, the value of these services represented a sizable percentage of residents' salaries.
Our data demonstrated that orthopedic residents provide a significant amount of financially quantifiable services to patients. We used conservative measures in our analysis. While Medicare is the chief payer for GME, residents provide services to patients with private and public insurance as well as those who lack coverage. In our cohort, 38% of patients were privately funded, and these payers often reimburse at higher rates than the Medicare wRVU multiplier we used. We also did not include potential downstream revenue generated by orthopedic residents (eg, splint/cast charges, facility fees for procedures), which would further increase the value generated by the residents. Adjusting the value with the –54 modifier for procedures performed by the on-call residents for which follow-up care would be performed by another physician decreased the value by 30%. At the same time, we likely overestimated the potential revenue, as 15% (397 of 2644) of patients were funded by Medicaid, 17% (449 of 2644) were self-pay, and 4% (106 of 2644) had no known insurer.
Studies on this topic have been performed in other specialties. A study in the pediatrics outpatient setting found that residents had a substantial amount of average annual wRVU production per resident, increasing from 548 as a PGY-1 to 893 as a PGY-3.11 Another study in pediatric surgery estimated that a fellow generated 703 wRVUs, which converted to just under $26,000 annually.12 This is lower than the annualized amount of $327,471 in our study of orthopedic resident services. Our findings are comparable to a study of plastic surgery consultations, which found a potential of greater than 10 000 wRVUs for work performed by plastic surgery residents over a 1-year period.13
Alternatives to resident physician coverage for orthopedic consultations do exist, including advanced practice providers. The national average salary for an orthopedic advanced practice provider is approximately double that of a resident physician.15,16 At some facilities, orthopedic attending physicians cover orthopedic consultations. Their salary is substantially higher than that of resident physicians, and they bill at a higher rate. Considering these costs, and comparing them to the cost and value of resident physicians, is important for a complete understanding of the financial value of on-call residents.
The billing practices for resident physicians' services vary. None of the institutions in this study bills for services attending physicians did not directly supervise. Thus, our calculations of billable services are theoretical.
Our study has limitations. We only examined the work performed by orthopedic residents, a procedure-based specialty, and the findings may not be generalizable to other specialties. We chose a 90-day study period, which does not reflect volume over an entire year. Despite this being a multicenter study, our results may not be generalizable to orthopedic programs in different settings or regions. Furthermore, wRVU calculations may not reflect the actual value of reimbursement received by participating institutions. Finally, we did not calculate the value of resident services in the outpatient clinic, the operating room, and rounding on patients, nor did we account for the cost impact of the presence of residents beyond their salaries.
With the continued at-risk status of GME funding, research utilizing this methodology in other specialties may be beneficial to hospitals, tax payers, and policy makers to make more informed decisions about the value of on-call residents.
Conclusion
In this study of 4 academic medical centers with orthopedic residency programs, on-call residents provided services that represented substantial potential monetary value. The value of services represented approximately 73% of their stipend using average published relative value and rates and data on resident stipends.
Footnotes
Funding: The authors report no external funding source for this study.
Conflict of interest: The authors declare they have no competing interests.
These data were presented at the Southern Orthopaedic Association Annual Meeting, Naples, Florida, July 27–30, 2016; the South Carolina Orthopaedic Association & South Carolina Association of Orthopaedic Executives Annual Meeting, Kiawah Island, South Carolina, August 4–6, 2016; and the American Academy of Orthopaedic Surgeons Annual Meeting, San Diego, California, March 14–18, 2017.
The authors would like to thank the following people for their contribution to data collection and study coordination: Eric Forney, third-year medical student, Paul Johnson, MD, Lisa Lepper, Shawn Malan, third-year medical student, Ryan Miller, MD, Osita Obi, fourth-year medical student, Derek Parshall, fourth-year medical student, and Rachael Seymour, PhD.
References
- 1. . Protection P, Act AC. HR 3590. 111th Congress. 2010;2. https://www.gpo.gov/fdsys/pkg/PLAW-111publ148/pdf/PLAW-111publ148.pdf. Accessed November 14, 2017.
- 2. . Iglehart JK. . The uncertain future of Medicare and graduate medical education. N Engl J Med. 2011; 365 14: 1340– 1345. [DOI] [PubMed] [Google Scholar]
- 3. . Grover A, Slavin PL, Willson P. . The economics of academic medical centers. N Engl J Med. 2014; 370 25: 2360– 2362. [DOI] [PubMed] [Google Scholar]
- 4. . Bowles E, Simpson A. . The Moment of Truth: Report of the National Commission on Fiscal Responsibility and Reform. Washington, DC: White House; 2010. [Google Scholar]
- 5. . Iglehart JK. . Financing graduate medical education-mounting pressure for reform. N Engl J Med. 2012; 366 17: 1562– 1563. [DOI] [PubMed] [Google Scholar]
- 6. . Medical Payment Advisory Commission. Report to the Congress: reforming the delivery system. September 16, 2008. https://www2.lawrence.edu/fast/finklerm/Miller%20Medpac%20report%202008.pdf. Accessed November 14, 2017.
- 7. . Institute of Medicine; Board on Health Care Services; Committee on the Governance and Financing of Graduate Medical Education, et al. Graduate Medical Education that Meets the Nation's Health Needs. Washington, DC: National Academies Press; 2014. [PubMed] [Google Scholar]
- 8. . Iglehart JK. . Institute of Medicine report on GME—a call for reform. N Engl J Med. 2015; 372 4: 376– 381. [DOI] [PubMed] [Google Scholar]
- 9. . Association of American Medical Colleges. Academic medicine: where patients turn for hope. https://members.aamc.org/eweb/upload/Academic%20Medicine%20Where%20Patients%20Turn%20for%20Hope.pdf. Accessed November 14, 2017.
- 10. . Jackson JB III, Huntington WP, Frick SL. . Assessing the value of work done by an orthopedic resident during call. J Grad Med Educ. 2014; 6 3: 567– 570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. . Ng M, Lawless ST. . What if pediatric residents could bill for their outpatient services? Pediatrics. 2001; 108 4: 827– 834. [DOI] [PubMed] [Google Scholar]
- 12. . St Peter SD, Calkins CM, Holcomb GW III, et al. . Financial impact of in-house attending surgeon: a prospective study. J Pediatr Surg. 2008; 43 6: 994– 997. [DOI] [PubMed] [Google Scholar]
- 13. . Drolet BC, Tandon VJ, Sargent R, et al. . Revenue generation and plastic surgery training programs: 1-year evaluation of a plastic surgery consultation service. Plast Reconstr Surg. 2016; 138 3: e539– e542. [DOI] [PubMed] [Google Scholar]
- 14. . Centers for Medicare & Medicaid Services, US Department of Health and Human Services. Medicare program; revisions to payment policies under the physician fee schedule, clinical laboratory fee schedule and other revisions to Part B for CY 2014. Final rule with comment period. Fed Regist. 2013; 78: 74229– 74823. [PubMed] [Google Scholar]
- 15. . Association of American Medical Colleges. Survey of resident/fellow stipends and benefits report 2014–2015. November 2014. https://www.aamc.org/download/412558/data/2014stipendsurveyreportfinal.pdf. Accessed November 14, 2017.
- 16. . Vaidya A. . 9 things to know about orthopedic PA salary. Becker's Spine Review. https://www.beckersspine.com/orthopedic-spine-practices-improving-profits/item/31478-9-things-to-know-about-orthopedic-pa-salary.html. Accessed November 14, 2017.


