Abstract
Background
Physicians need to rapidly and effectively facilitate patient-centered, shared decision-making (SDM) conversations, but little is known about how residents or attending physicians acquire this skill.
Objective
We explored emergency medicine (EM) attending physicians' use of SDM in the context of their experience as former residents and current educators and assessed the implications of these findings on learning opportunities for residents.
Methods
We used semistructured interviews with a purposeful sample of EM physicians. Interviews were transcribed verbatim, and 3 research team members performed iterative, open coding of transcripts, building a provisional codebook as work progressed. We analyzed the data with a focus on participants' acquisition and use of skills required for SDM and their use of SDM in the context of resident education.
Results
Fifteen EM physicians from academic and community practices were interviewed. All reported using SDM techniques to some degree. Multiple themes noted had negative implications for resident acquisition of this skill: (1) the complex relationships among patients, residents, and attending physicians; (2) residents' skill levels; (3) the setting of busy emergency departments; and (4) individual attending factors. One theme was noted to facilitate resident education: the changing culture—with a cultural shift toward patient-centered care.
Conclusions
A constellation of factors may diminish opportunities for residents to acquire and practice SDM skills. Further research should explore residents' perspectives, address the modifiable obstacles identified, and examine whether these issues generalize to other specialties.
Introduction
Shared decision-making (SDM), the process by which clinicians and patients collectively make decisions, based on clinical evidence and patient preferences and values, has been called “the pinnacle of patient-centered care.”1 It has been promoted for its potential to engage patients, increase patients' knowledge, and decrease the use of care resources.2–5 The National Guideline Clearinghouse recognizes more than 360 current practice guidelines (from 48 specialties) that recommend the utilization of SDM for a range of medical problems.6 Despite the widespread promotion of SDM, implementation remains challenging, and there is no consensus on how to teach and foster SDM skills in trainees.7–9
Prior studies across multiple specialties have demonstrated that interventions to teach SDM skills can be both necessary and effective.10–14 However, for SDM to be integrated into routine clinical care, those skills need to be taught and modeled routinely during training.9 While residency programs have been reevaluating how physicians-in-training can gain the necessary skills for SDM, little is known about how contextual factors of residency or the perspectives of attending physicians affect residents' opportunities to practice these skills.15,16 Little research exists regarding barriers residents face in learning SDM skills, and several studies report lack of formal education, lack of familiarity with SDM as a concept, and lack of feedback on communication skills.17–20 While several studies encompassed multiple specialties, all are limited by small sample sizes and heterogeneous designs.
In our initial investigation of attending emergency physician (EP) attitudes and practices regarding their use of SDM, we discovered generally positive attitudes toward SDM, along with growing recognition of barriers to its routine use in the emergency department.21 In this analysis, we examined emergency medicine (EM) faculty's experiences with acquisition of SDM skills and teaching these skills to residents. The goal was to improve our understanding of how clinicians acquire and teach SDM skills to facilitate and promote this patient-centered practice.
In this research summary, we focus on the emergent themes regarding factors that affect training, education, and the opportunities to practice and use SDM during residency.
Methods
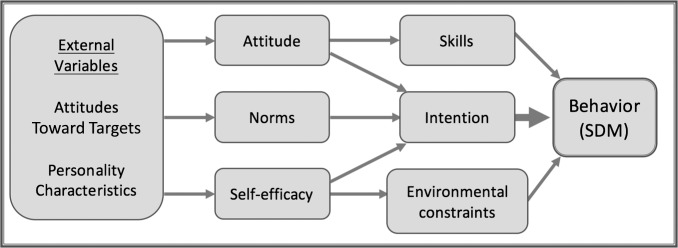
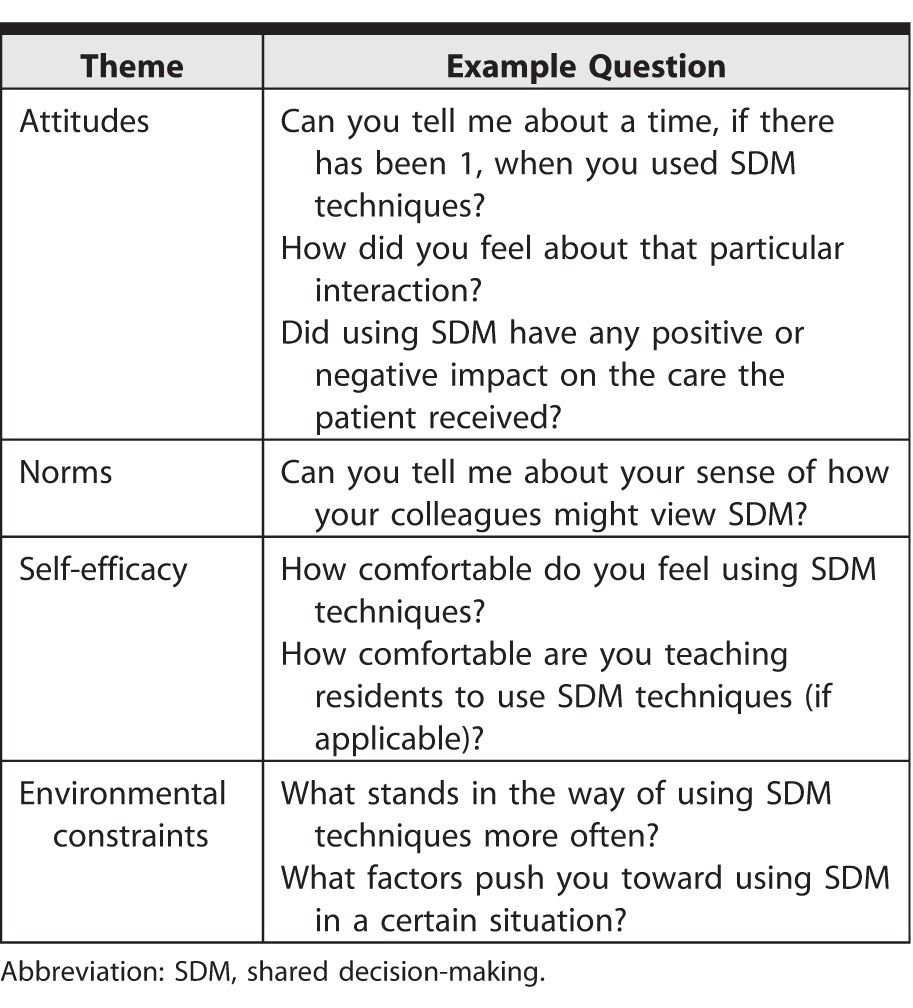
The theory of planned behavior provides a framework for exploring the relationships among beliefs, attitudes, intentions, and behaviors (such as SDM).22 Social cognitive theory adds dimensions of personal and environmental factors and recognizes their dynamic relationship with behaviors.22 These 2 theories provide a more complete framework for organizing the factors (concrete experiences, reflective observation, abstract conceptualization, and active experimentation) that may influence the performance of SDM (Figure 1).22 Table 1 explains how our framework led to the development of the interview guide.21,22
Figure 1.
Theoretical Framework (Integrative Model: Social Cognitive Theory and Theory of Planned Behavior22) Demonstrating How Various Factors May Influence a Behavior (Shared Decision-Making)
Table 1.
How the Theoretical Framework Shaped the Interview Guide
To explore how the theory of planned behavior and social cognitive theory influence SDM, we conducted semistructured interviews with practicing EPs. We chose a purposeful sample of EM physicians based on sex, years in practice, region, employment setting (rural/suburban/urban), academic versus community practice setting, and location of training.23
Data Collection
Interviewers were practicing EM physicians who knew many of the participants. The research goals were stated prior to the semistructured interview, and it was made clear that the interviewers sought frank responses (interview guide provided as online supplemental material). The 3 coders included an EM attending, an EM resident, and a nonphysician researcher with experience with qualitative methods.
Participants provided written, informed consent and filled out a demographics form. The interview team consisted of 2 academic EPs (E.M.S. and T.R.E.) who trained and piloted interviews under a senior investigator with qualitative experience (S.L.G.). All interviews were recorded and transcribed verbatim. Data collection was concluded when thematic saturation was reached, and 3 consecutive transcripts yielded no new concepts,24 and was designed to comply with standards for qualitative research.25,26
Interviews were semistructured and included questions about participants' training in SDM and their interactions with residents in the context of using SDM. The interview guide was modified as interviews progressed, to encourage more detail in responses.
Trained interviewers took field notes during interviews. Participants were asked to compare their use of SDM in the different settings, elaborating on why they used SDM more in some settings than in others, and their responses were included in the coded transcripts. To evaluate trustworthiness, we performed member checking by providing participants with a summary of major points discussed, and asking them for their agreement, disagreement, or comments.27
The study was granted exempt status by our Institutional Review Board.
Data Analysis
Transcripts were entered into Dedoose qualitative data management and analysis software version 7.0.18 (SocioCultural Research Consultants LLC, Manhattan Beach, California). Initial coding was performed concurrently with interviews and was performed by 3 research team members (E.M.S., E.R.K., K.E.P.) with qualitative research experience or recent training in coding. The codebook was developed using a directed approach to content analysis; we combined a priori codes drawn from previous literature and our theoretical framework with emergent codes that came from the line-by-line coding of transcripts.25,28 Coding was iterative, meaning transcripts were recoded as the codebook was refined. Each transcript was coded at least twice by at least 2 coders. Disagreements were discussed until consensus was reached. The codebook is provided as online supplemental material.
Results
We interviewed 15 EM faculty members between June and November 2015. Interviews lasted 20 to 45 minutes. Participants had completed residency training from 1 to 30 years prior to the interview. In the year prior to the interviews, participants worked at 14 different community and academic emergency departments, with nearly one-half having worked at more than 1 site. Sites included academic, academic-affiliated, and community settings.
Interviewees commented on factors that have implications for training residents in SDM. Those factors were derived deductively and inductively and were categorized as barriers or facilitators. Themes around barriers fell into 4 categories, and we identified 1 facilitator theme (Table 2).
Table 2.
Relevant Themes and Supporting Quotes
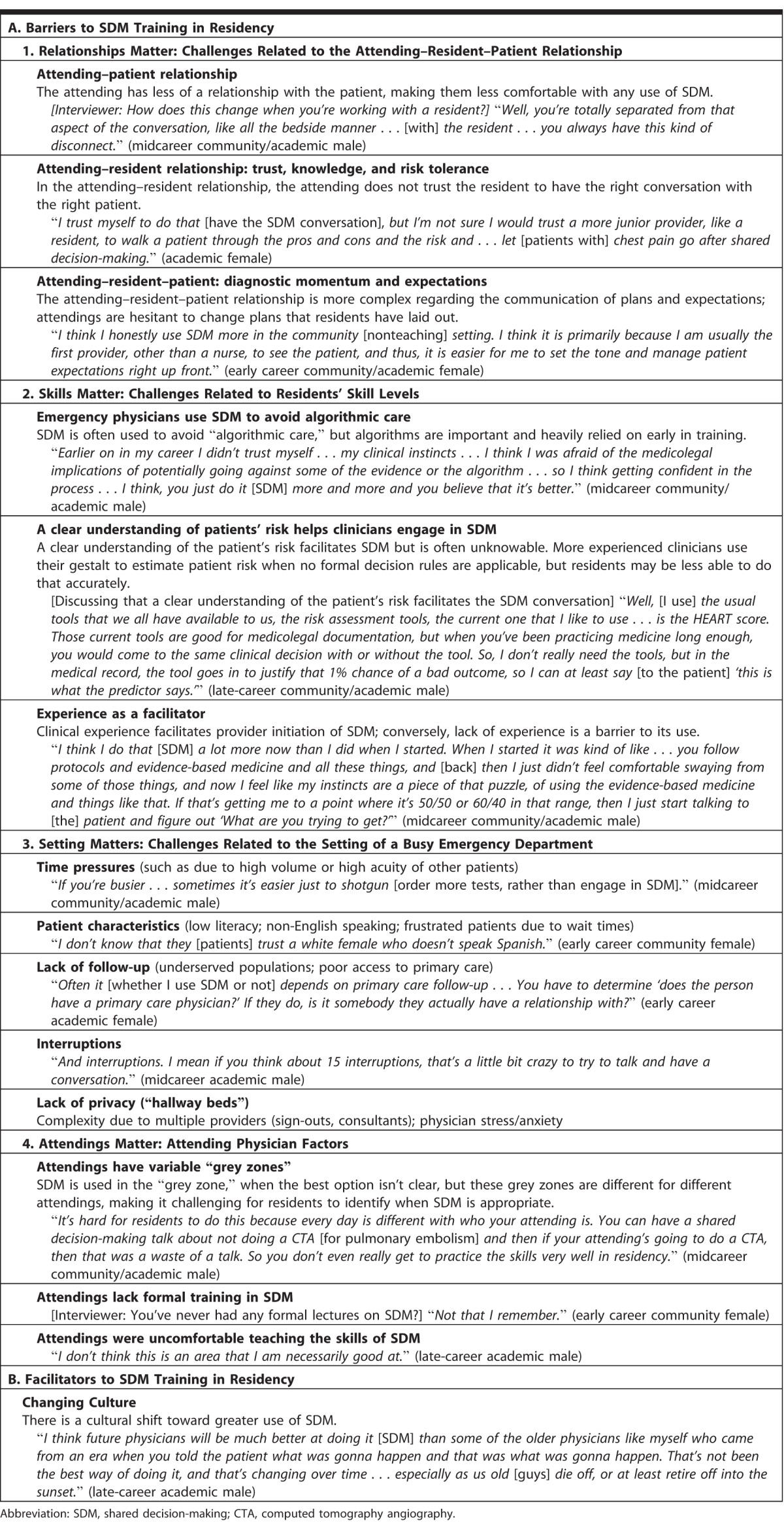
Barriers to SDM Training During Residency
Relationships Matter:
When asked how the presence of residents altered their ability or motivation to initiate SDM conversations, EM physicians' responses were overwhelmingly negative and often focused on the difficulties in the attending–resident–patient triad compared with the attending–patient dyad. Respondents noted that a good patient relationship allowed them to elicit patient preferences in clinical decision-making discussions, which facilitated SDM. In contrast, when they supervised residents, respondents did not feel they had a sufficiently close relationship with the patient to employ SDM. Interviewees noted they are often the last provider to see the patient, and since the residents often conveyed the diagnosis and treatment plan to the patient, that made making a change or the addition of SDM difficult.
Skills Matter:
The EM faculty noted they often used SDM to diverge from “algorithmic” care, when they felt that a particular course of care might not be best for a patient. However, they noted that residents relied, and they, as residents, had relied on care algorithms.
Several noted that as their clinical skills improved, they understood the nuances of clinical care and were more willing to accept and invite patient involvement in decision-making. Many noted they did not always trust the residents to have the right conversation with the patient. This led us to conclude that lack of clinical experience may be a major barrier to the use of SDM within residency and in the years following residency. Similarly, a number of interviewees noted that when they had a solid understanding of patient risk, they felt more comfortable engaging in SDM.29 One educator opined that junior residents probably should not engage in SDM, as they have not yet developed the clinical acumen needed to use it appropriately. These comments suggest that residents and early career physicians may be less comfortable engaging in SDM.
Setting Matters:
Interviewees mentioned a number of setting-related barriers, including time constraints; high-acuity patients competing for physician time and attention; lack of access to follow-up care; low health literacy; language barriers; lack of privacy; and frequent interruptions. Interviewees indicated they were less likely to offer SDM at facilities with more of these types of barriers.
Attendings Matter:
Participants noted there is variation in practice among attending physicians, and this poses a challenge to resident education. Trainees may be encouraged to use SDM in 1 clinical scenario, only to find that the next day, another attending disagrees with the use of SDM. None of our participants had formal training in SDM, and while all felt they could comfortably engage patients, some expressed concerns about their ability to effectively teach SDM skills to residents.
Facilitators to SDM Training During Residency
Despite challenges noted, interviewees pointed out the positive effects of the culture of patient-centered care, and many perceived a cultural shift toward increased use of SDM.
Discussion
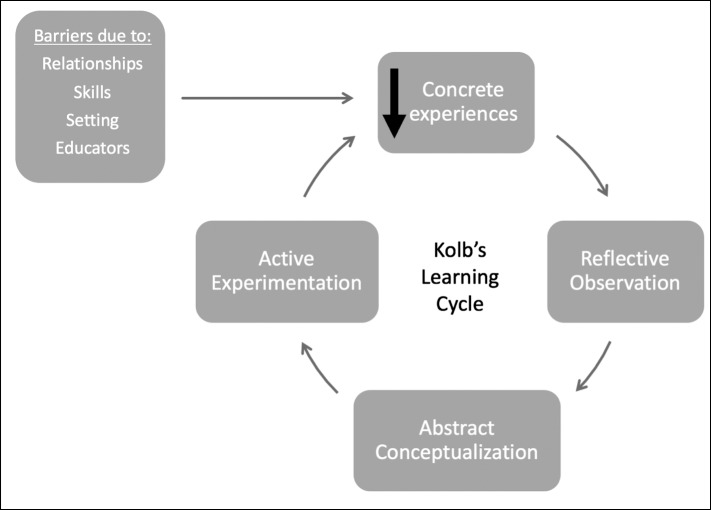
Our results highlight challenges to residents learning and practicing SDM, as well as a single facilitator. Medical education has been conceptualized as a “community of practice” where a network of individuals develops and shares a knowledge base, set of beliefs, values, history, and experiences.30,31 Within that community, experiential learning often predominates, and educators are expected to provide authentic experiences for trainees. According to Kolb,32 these concrete experiences lead to reflective observation, abstract conceptualization, active experimentation, and back to experiences. Authentic experiences are an important part of learning a new skill. Unfortunately, many of the barriers we found limit opportunities for residents to have concrete SDM experiences (Figure 2). By limiting learning opportunities during residency, many barriers are perpetuated: first, because less experience often leads to lower confidence and hesitancy,33 and residents may be less likely to seek out opportunities to use SDM; and second, because residents lacking the skills to perform SDM become attendings with marginal skills and experience.
Figure 2.
Conceptual Framework Regarding How Noted Barriers May Impede Skill Acquisition for Residents by Decreasing Opportunities for Concrete Experiences32
Many barriers noted are clearly not unique to EM. A recent study reported that internal medicine residents felt that “gaps in their clinical skills” were a barrier to effective SDM,18 and a study examining the same issues in surgical residents noted numerous “missed opportunities” for teaching communication skills, supporting the generalizability of some of our findings.34
Another finding relates to the barriers categorized under “setting.” While some of those, such as the difficulties of engaging in SDM when a patient is in a “hallway bed,” are specific to EM, many apply to clinical contexts across specialties and are more likely present in settings in which residents are trained. For example, compared with nonteaching hospitals, teaching hospitals provide a disproportionate amount of medical care for indigent and medically underserved populations, have high patient volumes, and have patients with high severity of illness.35–37 It follows that the barriers we identified—poor follow-up, low health literacy, language barriers, and high volumes—may disproportionately burden teaching hospitals, suggesting that both patients and trainees at those settings are less likely to have the opportunity to participate in SDM. That finding is particularly concerning in light of evidence that suggests disadvantaged patients may benefit more from SDM than patients with higher literacy and socioeconomic status.38 As many teaching hospitals cite “improving the health of their communities” at the heart of their mission statements,35 increasing SDM opportunities should be viewed not only as a benefit to trainees but also as a benefit to the communities served.
Participants' comments suggest some solutions for overcoming potential barriers: physicians were all comfortable initiating SDM conversations in the scenarios in which they deemed it appropriate. Therefore, attendings could be encouraged to model those conversations if they are uncomfortable letting the resident proceed unsupervised. However, that degree of comfort may not exist for all specialties: a large, multispecialty study of residents and educators concluded that risk communication, an essential part of SDM, may not be receiving enough attention during graduate education.39 Our results and the current literature39–41 suggest that more training, for both residents and attendings, is likely warranted.
Our study has limitations. We did not interview residents about these issues. In a recent article, a current resident suggested that trainees are an “untapped resource in furthering pediatric SDM” because they have more time than attendings to talk to patients and families.41 Second, although our participants received their medical training at geographically varied sites, all were practicing in New England, which may have limited the heterogeneity of the responses, and it is possible that attending physicians in other specialties would identify other issues. Despite those limitations, we found that the themes participants expressed were both compelling and widespread and were of particular importance to those seeking to promote, teach, or study SDM.
Further research is warranted to clarify the importance and magnitude of each of the issues identified here and to examine the issues from the point of view of the residents, since they are likely to have important insights into these challenges as well as possible solutions.
Conclusion
Our qualitative study suggests that several potentially modifiable factors limit the number of opportunities that EM residents have to learn and practice the skills needed for SDM. Our findings may generalize to residents from other specialties.
Supplementary Material
Footnotes
Editor's Note: The online version of this article contains a semistructured interview guide and a master codebook.
Funding: This study was funded by grant number 1R03HS024311-01 from Agency for Healthcare Research and Quality. The project described was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, award number UL1TR001064. Dr Lindenauer is supported by grant number K24 HL132008: Research and Mentoring in Comparative Effectiveness and Implementation Science.
Conflict of interest: The authors declare they have no competing interests.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
What was known and gap
Shared decision-making has important positive consequences for patients and health care delivery, yet little is known about barriers to teaching and modeling this approach in residency settings.
What is new
Structured interviews with emergency medicine faculty revealed 4 barriers and 1 facilitator for teaching shared decision-making.
Limitations
Limited interview study; resident perspectives were not sampled.
Bottom line
Faculty report significant, yet potentially modifiable barriers that may diminish opportunities for residents to acquire and practice this important skill.
References
- 1. . Barry MJ, Edgman-Levitan S. . Shared decision making—pinnacle of patient-centered care. N Engl J Med. 2012; 366 9: 780– 781. [DOI] [PubMed] [Google Scholar]
- 2. . Kanzaria HK, Brook RH, Probst MA, et al. Emergency physician perceptions of shared decision-making. Acad Emerg Med. 2015; 22 4: 399– 405. [DOI] [PubMed] [Google Scholar]
- 3. . Elwyn G, Tilburt J, Montori VM. . The ethical imperative for shared decision-making. Eur J Pers Cent Healthc. 2013; 1 1: 129– 131. [Google Scholar]
- 4. . Hess EP, Grudzen CR, Thomson R, et al. Shared decision-making in the emergency department: respecting patient autonomy when seconds count. Acad Emerg Med. 2015; 22 7: 856– 864. [DOI] [PubMed] [Google Scholar]
- 5. . Hess EP, Knoedler MA, Shah ND, et al. The chest pain choice decision aid: a randomized trial. Circ Cardiovasc Qual Outcomes. 2012; 5 3: 251– 259. [DOI] [PubMed] [Google Scholar]
- 6. . Agency for Healthcare Research and Quality. National guideline clearinghouse. https://www.guideline.gov. Accessed December 7, 2017. [DOI] [PubMed]
- 7. . Légaré F, Politi MC, Drolet R, et al. Training health professionals in shared decision-making: an international environmental scan. Patient Educ Couns. 2012; 88 2: 159– 169. [DOI] [PubMed] [Google Scholar]
- 8. . Légaré F, Moumjid-Ferdjaoui N, Drolet R, et al. Core competencies for shared decision making training programs: insights from an international, interdisciplinary working group. J Contin Educ Health Prof. 2013; 33 4: 267– 273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. . Chen EH, Kanzaria HK, Itakura K, et al. The role of education in the implementation of shared decision making in emergency medicine: a research agenda. Acad Emerg Med. 2016; 23 12: 1362– 1367. [DOI] [PubMed] [Google Scholar]
- 10. . Yuen JK, Mehta SS, Roberts JE, et al. A brief educational intervention to teach residents shared decision making in the intensive care unit. J Palliat Med. 2013; 16 5: 531– 536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. . Stacey D, Samant R, Pratt M, et al. Feasibility of training oncology residents in shared decision making: a pilot study. J Cancer Educ. 2012; 27 3: 456– 462. [DOI] [PubMed] [Google Scholar]
- 12. . Simmons L, Leavitt L, Ray A, et al. Shared decision making in common chronic conditions: impact of a resident training workshop. Teach Learn Med. 2016; 28 2: 202– 209. [DOI] [PubMed] [Google Scholar]
- 13. . Sepucha KR, Simmons LH, Barry MJ, et al. Ten years, forty decision aids, and thousands of patient uses: shared decision making at Massachusetts General Hospital. Health Aff (Millwood). 2016; 35 4: 630– 636. [DOI] [PubMed] [Google Scholar]
- 14. . Bieber C, Nicolai J, Hartmann M, et al. Training physicians in shared decision-making—who can be reached and what is achieved? Patient Educ Couns. 2009; 77 1: 48– 54. [DOI] [PubMed] [Google Scholar]
- 15. . Han PKJ, Joekes K, Elwyn G, et al. Development and evaluation of a risk communication curriculum for medical students. Patient Educ Couns. 2013; 94 1: 43– 49. [DOI] [PubMed] [Google Scholar]
- 16. . Hoppe RB, King AM, Mazor KM, et al. Enhancement of the assessment of physician–patient communication skills in the United States Medical Licensing Examination. Acad Med. 2013; 88 11: 1670– 1675. [DOI] [PubMed] [Google Scholar]
- 17. . Caldwell JG. . Evaluating attitudes of first-year residents to shared decision making. Med Educ Online. 2008; 13: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. . Simmons L, Leavitt L, Ray A, et al. Shared decision making in common chronic conditions: impact of a resident training workshop. Teach Learn Med. 2016; 28 2: 202– 209. [DOI] [PubMed] [Google Scholar]
- 19. . Loureiro E, Severo M, Ferreira MA. . Attitudes of Portuguese medical residents' towards clinical communication skills. Patient Educ Couns. 2015; 98 8: 1039– 1043. [DOI] [PubMed] [Google Scholar]
- 20. . Samant R, Aivas I, Bourque JM, et al. Oncology residents' perspectives on communication skills and shared decision making. J Cancer Educ. 2010; 25 4: 474– 477. [DOI] [PubMed] [Google Scholar]
- 21. . Schoenfeld EM, Goff SL, Elia TR, et al. The physician-as-stakeholder: an exploratory qualitative analysis of physicians' motivations for using shared decision making in the emergency department. Acad Emerg Med. 2016; 23 12: 1417– 1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. . National Cancer Institute. Theory at a glance: a guide for health promotion practice. 2nd ed. 2005. NIH Publication No. 05-3896. http://www.sbccimplementationkits.org/demandrmnch/wp-content/uploads/2014/02/Theory-at-a-Glance-A-Guide-For-Health-Promotion-Practice.pdf. Accessed December 7, 2017.
- 23. . Miles MB, Huberman AM, Saldana J. . Qualitative Data Analysis: A Methods Sourcebook. 3rd ed. Los Angeles, CA: SAGE Publications Inc; 2013. [Google Scholar]
- 24. . Guest G, Bunce A, Johnson L. . How many interviews are enough? An experiment with data saturation and variability. Field Methods. 2006; 18 1: 59– 82. [Google Scholar]
- 25. . Tong A, Sainsbury P, Craig J. . Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007; 19 6: 349– 357. [DOI] [PubMed] [Google Scholar]
- 26. . O'Brien BC, Harris IB, Beckman TJ, et al. Standards for reporting qualitative research. Acad Med. 2014; 89 9: 1245– 1251. [DOI] [PubMed] [Google Scholar]
- 27. . Creswell JW. . Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. Los Angeles, CA: SAGE Publications Inc; 2014. [Google Scholar]
- 28. . Hsieh HF. . Three approaches to qualitative content analysis. Qual Health Res. 2005; 15 9: 1277– 1288. [DOI] [PubMed] [Google Scholar]
- 29. . Backus BE, Six AJ, Kelder JC, et al. Chest pain in the emergency room: a multicenter validation of the HEART Score. Crit Pathw Cardiol. 2010; 9 3: 164– 169. [DOI] [PubMed] [Google Scholar]
- 30. . Barab SA, Barnett M, Squire A. . Developing an empirical account of a community of practice: characterizing the essential tensions. J Learn Sci. 2002; 11 4: 489– 542. [Google Scholar]
- 31. . Cruess RL, Cruess SR, Steinert Y. . Medicine as a community of practice: implications for medical education [published correction appears in Acad Med . July 25, 2017.]. Acad Med . doi: 10.1097/ACM.0000000000001826. [DOI] [PubMed]
- 32. . Kolb D. . Experiential Learning. Englewood Cliffs, NJ: Prentice-Hall; 1984. [Google Scholar]
- 33. . Dehmer JJ, Amos KD, Farrell TM, et al. Competence and confidence with basic procedural skills: the experience and opinions of fourth-year medical students at a single institution. Acad Med. 2013; 88 5: 682– 687. [DOI] [PubMed] [Google Scholar]
- 34. . Hutul OA, Carpenter RO, Tarpley JL, et al. Missed opportunities: a descriptive assessment of teaching and attitudes regarding communication skills in a surgical residency. Curr Surg. 2006; 63 6: 401– 409. [DOI] [PubMed] [Google Scholar]
- 35. . Pugno PA, Gillanders WR, Kozakowski SM. . The direct, indirect, and intangible benefits of graduate medical education programs to their sponsoring institutions and communities. J Grad Med Educ. 2010; 2 2: 154– 159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. . Iwashyna TJ, Curlin FA, Christakis NA. . Racial, ethnic, and affluence differences in elderly patients' use of teaching hospitals. J Gen Intern Med. 2002; 17 9: 696– 703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. . Papanikolaou PN, Christidi GD, Ioannidis JP. . Patient outcomes with teaching versus nonteaching healthcare: a systematic review. PLoS Med. 2006; 3 9: e341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. . Durand MA, Carpenter L, Dolan H, et al. Do interventions designed to support shared decision-making reduce health inequalities? A systematic review and meta-analysis. PLoS One. 2014; 9 4: e94670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. . van der Horst K, Giger M, Siegrist M. . Attitudes toward shared decision-making and risk communication practices in residents and their teachers. Med Teach. 2011; 33 7: e358– e363. [DOI] [PubMed] [Google Scholar]
- 40. . Pellerin MA, Elwyn G, Rousseau M, et al. Toward shared decision making: using the OPTION scale to analyze resident-patient consultations in family medicine. Acad Med. 2011; 86 8: 1010– 1018. [DOI] [PubMed] [Google Scholar]
- 41. . Gaw CE. . Trainee involvement in advancing pediatric shared decision-making. Pediatrics. 2017; 140 3: e20171772. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.