Abstract
Background
Burnout rates for internal medicine residents are among the highest of all specialties, yet little is known about how residents recover from burnout.
Objective
We identified factors promoting recovery from burnout and factors that assist with the subsequent avoidance of burnout among internal medicine residents.
Methods
A purposive sample of postgraduate year 2 (PGY-2), PGY-3, and recent graduates who experienced and recovered from burnout during residency participated in semistructured, 60-minute interviews from June to August 2016. Using qualitative methods derived from grounded theory, saturation of themes occurred after 25 interviews. Coding was performed in an iterative fashion and consensus was reached on major themes.
Results
Coding revealed 2 different categories of resident burnout—circumstantial and existential—with differing recovery and avoidance methods. Circumstantial burnout stemmed from self-limited circumstances and environmental triggers. Recovery from, and subsequent avoidance of, circumstantial burnout arose from (1) resolving workplace challenges; (2) nurturing personal lives; and (3) taking time off. In contrast, existential burnout stemmed from a loss of meaning in medicine and an uncertain professional role. These themes were identified around recovery: (1) recognizing burnout and feeling validated; (2) connecting with patients and colleagues; (3) finding meaning in medicine; and (4) redefining a professional identity and role.
Conclusions
Our study suggests that residents experience different types of burnout and have variable methods by which they recover from and avoid further burnout. Categorizing residents' burnout into circumstantial versus existential experiences may serve as a helpful framework for formulating interventions.
Introduction
Burnout is a syndrome resulting from work-related stress and is characterized by emotional exhaustion, depersonalization, and a low sense of personal accomplishment.1 Its prevalence is particularly high during residency training.2,3 Burnout in internal medicine ranks among the highest of all specialties,4 with rates as high as 76%.5 Burnout is associated with lapses in professionalism,6 absenteeism, self-reported delivery of suboptimal patient care,5 and medical errors.7 Medical educators should consider how to help residents mitigate burnout and, subsequently, how to facilitate growth toward fulfilling and productive careers.
Interventions to reduce burnout have largely centered on prevention with modest success. At the individual level, mindfulness training, stress management, and small group discussions have shown small decreases in overall burnout prevalence.8,9 Interventions targeting the learning environment have centered on duty hour limitations and showed modest reductions in burnout.8,10 For example, the 6 studies on duty hour restrictions identified in a meta-analysis8 of burnout interventions found, among residents, a pooled burnout reduction from 62% to 50%. While these are promising steps toward decreasing burnout prevalence, those rates still leave a large group of residents who struggle with burnout. It is unclear how to help those individuals recover and avoid future burnout.
Given that limited information, we designed a qualitative study to identify factors promoting recovery from and subsequent avoidance of future burnout among resident physicians.
Methods
Study Design
We used a grounded theory qualitative approach with semistructured interviews to deepen our conceptual understanding of the factors contributing to resident burnout recovery. The lead investigator (N.C.A.) had conducted several previous qualitative studies and oversaw all critical components of the research and analysis to ensure methodological rigor. Two investigators (S.W.S. and K.P.S.) are medical educators with broad knowledge of factors surrounding resident education and well-being, ensuring content expertise in the design and implementation of the study. Faculty (S.W.S. and K.P.S.) were blinded to participants' identities to ensure anonymity and avoid coercion of participants.
Study Population
We used a purposive sampling of early postgraduate year (PGY)-2, early PGY-3, and recent graduates of the University of Washington Internal Medicine Residency Program who self-identified as having experienced and recovered from burnout during residency. We excluded interns as it was unlikely that they had both experienced and recovered from burnout in their first few months of training.
We sent 3 separate recruitment e-mails; amenable participants underwent informed consent and completed a single-item burnout measure with some evidence of validity11,12 prior to their interview. We excluded individuals whose responses indicated current burnout, as well as those who described depressive symptoms during their interview. Participants received a $10 gift card as compensation.
Data Collection
From June to August 2016, we conducted individual, semistructured, 60-minute interviews using a 9-question interview guide (Box). To ensure our questions would elicit the intended responses, this guide was developed specifically for this study based on our literature review of trainee and physician burnout6,8,13–15 and discussions with current residents and resident educators to understand the breadth of etiologies of burnout and possible recovery methods. We provided a standard definition of burnout to guide participants' reflections (Box, question 1).1 With the exception of 3 pilot interviews and 4 opt-out cases in which participants requested to be interviewed by the lead investigator (N.C.A.), a nonfaculty, nonresident investigator (J.L.G.) performed all interviews. Interviews were audio-recorded and transcribed verbatim; all identifiers were removed prior to analysis.
Box Semistructured Interview Guide.
1. Burnout is a syndrome resulting from work-related stress and characterized by emotional exhaustion, feelings of cynicism and detachment toward patients (depersonalization), and a low sense of personal accomplishment. Can you describe a time during your residency training when you experienced any of these symptoms?
2. What contributed to your recovery from burnout?
3. What were circumstances like at work/home?
4. What was different about your attitude or your personal circumstances, if anything?
5. Since that time, have you experienced burnout again? If so, what were the circumstances that caused you to experience burnout again?
6. How did you recover? How was it different/similar to your prior experience of burnout?
7. What has helped you avoid recurrence of burnout?
8. If you had to pick 1 thing that was most helpful for you to overcome and prevent burnout, what would it be?
9. Where do you derive meaning in medicine?
This study was approved by the University of Washington Institutional Review Board.
Data Analysis
Using inductive methods derived from grounded theory, 3 investigators (N.C.A., S.W.S., J.L.G.) independently coded transcripts. We assigned open codes (labels describing patterns in the data) on the first transcript review. Subsequent iterative review of transcripts led to axial coding (labels drawing connections among open codes) and selective coding (broader subthemes and themes that describe how residents recover from and avoid burnout).16,17
Examples of how open, axial, and selective coding were used to identify themes are provided as online supplemental material. Coding was performed concomitantly with data collection. We revised interview questions to elaborate emerging themes. Investigator triangulation occurred through regular meetings among N.C.A., S.W.S., and J.L.G., resulting in a consensus-based codebook. Interviews continued until saturation of themes was achieved. The lead investigator then recoded all transcripts with NVivo 10.0 software (QSR International, Melbourne, Victoria, Australia), using focused, line-by-line analysis based on the final codebook. Member checking (a validation process by which participants are provided an opportunity to review and amend study results) occurred by presenting results of the study at several resident group meetings that included study participants and nonparticipants. Residents did not suggest amendments to the study findings, and no changes were made to the analysis based on member checking.
Results
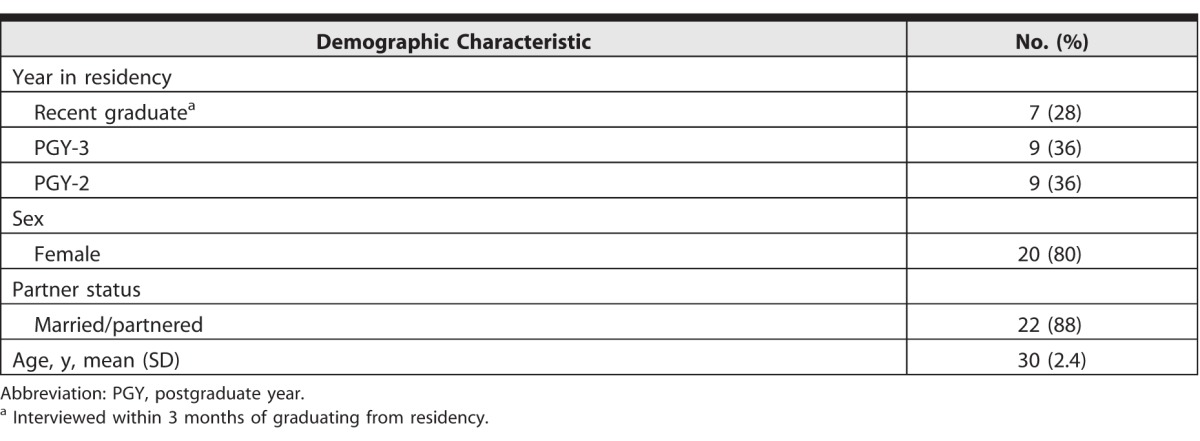
Of 126 residents, 37 (29%) self-identified as having recovered from burnout and were willing to participate in the study, and 28 interviews were ultimately conducted. Of those, 1 resident was excluded for displaying depressive symptoms during the interview, and 2 residents were excluded for evidence of burnout on the single-item burnout measure. The remaining 25 interviews included 9 PGY-2s, 9 PGY-3s, and 7 recent graduates (Table).
Table.
Demographic Characteristics for 25 Interview Participants
Coding revealed multiple themes and subthemes presented in a nonordinal manner (Figure). Among those themes, 2 categories of resident burnout emerged—circumstantial and existential burnout—which are further elaborated below. Notably, there were also individuals who appeared to have a mix of circumstantial and existential burnout.
Figure.
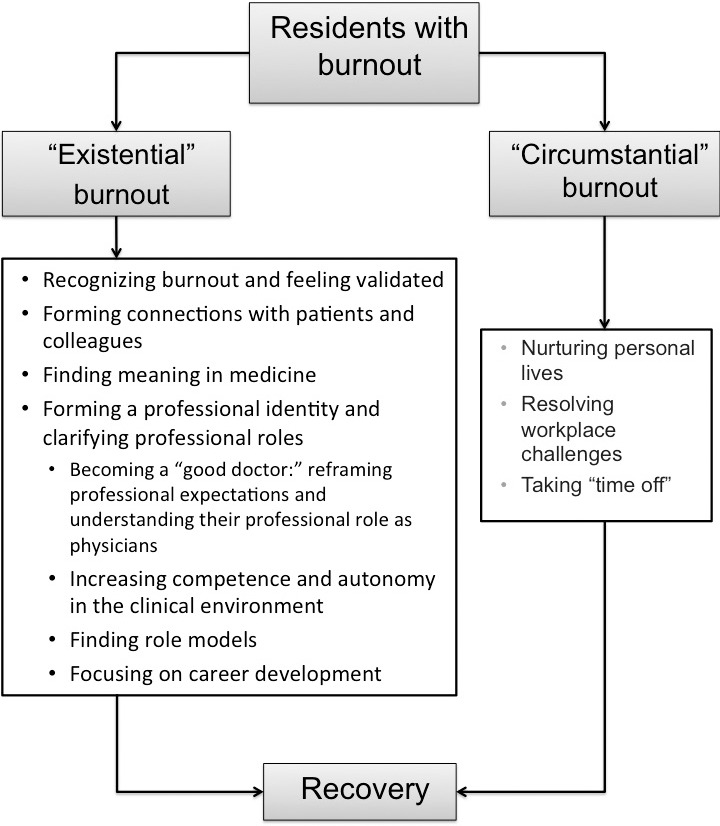
Schema Demonstrating Variable Methods of Recovery Among Residents Experiencing Circumstantial Versus Existential Burnout
Recovering From Circumstantial Burnout
Residents referred to situations associated with the work environment or personal challenges that precipitated circumstantial burnout. Their recovery was tied to 3 themes that led to resolution of those circumstances:
1. Resolving Workplace Challenges:
Residents identified workplace challenges contributing to burnout, including difficult interpersonal relationships with members of the medical team, high caseloads, long hours, patient acuity and deaths, taxing patient interactions, interfacing with the electronic health record, and inefficient or unclear workflow patterns. Resolution of those challenges, usually by leaving the rotation or making changes in the rotation conditions, often led to recovery from burnout. One resident reflected on her prior burnout after a prolonged period of heavy caseloads: “. . . [T]here was certainly a concern and fear that I was going to feel that way again . . . but [my caseload] never got anywhere near that point again” (Interview 21, PGY-2).
2. Nurturing Personal Lives:
Residents often noted that concurrent personal stressors, such as financial struggles or relationship conflicts, often instigated their burnout. Nurturing aspects of their personal lives helped them overcome and often avoid recurrent burnout: “[If] you have other elements of your life that are solid and that . . . you've nurtured, and . . . you can . . . derive a sense of security, safety, and feel that you're valued and useful to other people, that helps you weather the storm in other parts [of your life]” (Interview 3, PGY-3).
3. Taking Time Off:
Many residents noted that time off aided their recovery. They described many helpful activities outside of work, such as prioritizing restorative sleep, spending time with family and friends, exercising, and traveling. Some residents planned time off intentionally within the workday. The key was “doing something that doesn't make you feel like your entire life is medicine” (Interview 14, PGY-3).
Recovering From Existential Burnout
Many residents experienced existential burnout, which was tied to internal dilemmas of how they viewed themselves within the context of their developing role as physicians. These individuals utilized a different set of recovery methods outlined below:
1. Recognizing Burnout and Feeling Validated:
Participants reported that recognizing burnout as a cause of their symptoms was an important step in recovery. Additionally, reaching out to peers and faculty made them feel validated and comforted. One resident recalled reaching a breaking point after several difficult weeks on service in which she realized she was experiencing symptoms of burnout: “. . . [T]here was this 1 day where I was just so burnt out. These patients were so challenging . . . and [my attending] just gave me a hug and was like, ‘You are doing such a good job. You are doing everything you can for these patients and this is really hard.' Her recognizing that it was really hard was really helpful for me” (Interview 25, PGY-2).
Several residents reported self-imposed stigma after recognizing their burnout, and a need to overcome this stigma to begin recovery. As 1 resident noted, “[Burnout] is largely a reflection of your own perception of yourself—of being incompetent and inferior and weak. Until I really started talking about it, I don't feel that the progress really headed in the right direction” (Interview 5, PGY-3).
2. Forming Connections With Patients and Colleagues:
Focusing on developing connections with colleagues or patients was important for recovery by reinforcing humanistic qualities that residents found important in the practice of medicine. One resident discussed the challenge of connecting to patients while experiencing burnout, feeling inclined to “distance yourself from the people who are in pain to protect yourself.” However, she later found that connecting with patients was key to recovery: “If you bring yourself close to [your patients], you will find [your work] more fulfilling” (Interview 26, Grad).
Connection with coresidents through facilitated discussion helped residents process emotionally difficult circumstances at work and celebrate positive achievements. Several residents cited death rounds,18 a formal opportunity during the workday to discuss difficult or fulfilling experiences: “It's just nice to have a space to talk about specific examples of things that affected you and also hear how other people were also affected by them” (Interview 9, PGY-3).
3. Finding Meaning in Medicine:
Many residents attributed recovery from burnout to refocusing on areas where they derived meaning in medicine. To explore this theme further, question 6 was added to the interview guide (Box). While many derived meaning from relationships with patients and colleagues, or from helping patients through personal and physical hardships, others found meaning in acquiring unique skills and knowledge and engaging in scientific inquiry. One resident described a mental “restructuring and putting things in perspective” that was essential for his avoidance of burnout, by deliberately focusing on what brought him meaning in medicine (Interview 22, PGY-2).
4. Forming a Professional Identity and Clarifying Professional Roles:
Many residents attributed burnout to uncertainty in their professional identity and role. The longitudinal process of resolving that uncertainty played an important part in recovery from existential burnout, occurring in several different ways:
a. Becoming a “good doctor”: Reframing professional expectations and understanding their role as physicians. The majority of residents described self-imposed professional expectations that were difficult to fulfill within the workday; these contributed to feelings of inadequacy and exacerbated their burnout. With time, experience, and reflection, those residents came to understand their professional role, which helped them set realistic expectations and be more efficient in navigating the health care system.
Several residents initially defined “good doctoring” as directly spending time with patients, viewing administrative work, such as note writing, answering pages, and coordinating care, as being counter to good doctoring. However, in recognizing that their role was multifaceted and accepting that those administrative tasks also contributed to good doctoring, they were able to overcome their burnout. “[I realized that] getting frustrated at this stuff is kind of pointless. This is what I chose to do, and if somebody pages me for something silly, the reality is that it's my job. [It] was just sort of a reset in my mind that helped me to sort of deal with things better” (Interview 22, PGY-2).
Residents reported that a lack of knowledge on how to set boundaries with patients and patient care often led to burnout when the residents overextended themselves. As such, learning to set boundaries helped them avoid recurrent burnout. “I don't think [prior to residency] I thought about how much the patients would kind of overwhelm [me]. Their needs and their desires, their interest in my time, would kind of be never-ending, and that there would need to be barriers set up. [It's] a hard thing and not something that we talk about or get trained on how to do well” (Interview 4, PGY-3).
b. Increasing competence and autonomy in the clinical environment. Clinical advancement, improved knowledge and understanding of the health care system, and increasing levels of autonomy also helped residents recover from burnout and avoid recurrence. “[When] you're an intern, you can't be a doctor because you don't know how to get anything done. Even if you could make the decisions and have great relationships with your patients, you don't know how to get their care done effectively, which is really frustrating” (Interview 21, PGY-2). Another commented that as a senior resident, “[Feeling] like I'm the one in the driver's seat is . . . incredibly validating,” in terms of affirming his competence and reducing feelings of inadequacy that contributed to his burnout (Interview 14, PGY-3).
c. Finding role models. Witnessing attending physicians practice compassionate patient care was restorative for many participants. One resident stated that she felt uninspired while experiencing burnout, but then found “good role models who showed me again why I went into medicine and how to listen to patients and how to think about vulnerable patients, which . . . was a reminder of what [medicine] should be” (Interview 1, Grad).
d. Focusing on career development. Approaching work obligations with a sense of purpose toward learning and professional development was helpful for many residents: “Trying to take something away from every patient interaction . . . is really important. When I do those things, I feel like I enjoy work a lot more, because I'm learning, and I think so much of residency [is focusing] on getting things done . . . that I think it's hard to just take time to really get something out of it” (Interview 12, PGY-2). Others found that taking on additional career-related opportunities outside of work was restorative, such as research, coursework in bioethics, attending conferences, participating on committees, or taking part in resident and medical student education.
Discussion
Among internal medicine residents who had endured a history of burnout, we identified a number of methods by which they recovered from and subsequently avoided burnout. Those methods appeared to be predicated on the type of burnout the resident experienced: circumstantial or existential. Circumstantial burnout was tied largely to external environmental factors, and recovery depended on resolution of those factors. Conversely, residents with existential burnout faced a variety of internal dilemmas. Some residents needed to recognize burnout within themselves, overcome self-imposed stigma, and/or find validation before they could recover. Others required new social relationships, such as developing connections with patients or sharing and normalizing experiences with colleagues. Some residents experienced burnout due to a loss of meaning and needed to rediscover or redefine what brought them meaning in medicine. Perhaps most profoundly, several residents described contending with uncertainty in their professional role in the context of nascent skills and knowledge or struggling with the formation of their professional identity as they were forced to reconsider what being a “good doctor” meant. These residents required meaningful, and often longitudinal, reflection to reframe their experiences and expectations before they could recover.
Many participants who have experienced circumstantial burnout have been described13,19 and, similar to the findings in our study, are often self-limited. Campbell et al20 found that 28% of residents recover from burnout without any specific programmatic intervention, which they attributed to a natural improvement in work hours as residents progressed in their training. Notably, most circumstantial interventions to date have had only modest effects.8,10 Our results suggest that this may be due, in part, to the presence of existential burnout, either concomitantly with circumstantial burnout or independently, which likely requires a different set of recovery strategies. Moreover, our results suggest that existential burnout may be a potential cause of the prolonged or recurrent burnout described by Campbell et al.20 Future work should be directed at further delineating the prevalence of circumstantial and existential burnout among residents.
The recovery methods pertaining to existential burnout from our study share commonalities with prior studies that demonstrated the importance of protected time for reflection and discussion to decrease burnout prevalence. A number of our residents cited death rounds, a monthly formalized, protected time for reflection and discussion of challenging emotional patient interactions during select difficult rotations,18 as an important space to bring awareness to the trying circumstances leading to burnout, to create community and validate their feelings, and to help them reframe their experiences in a meaningful light. Similarly, facilitated, protected time for reflection and discussion among career physicians and residents has shown success in reducing the prevalence of burnout.21–24 These forums could also be important venues for residents to reconcile ambiguity in their professional role and around “good doctoring,” which our study suggests are important contributors to existential burnout and are worthy of further study. Those forums can be considered in the context of professional identity formation,25 a process which Cruess et al26 described as being guided through social connection and facilitated discussion. Our study suggests that integrating avenues to support residents' professional development and identity formation through facilitated discussion and reflection may be important components in addressing existential burnout.
Our study has limitations. First, women made up the majority of our cohort, although studies have demonstrated sex is not independently associated with a propensity for burnout. We used the single item burnout screening tool, which does not capture depersonalization or low sense of personal accomplishment. Because our data are from a single center, generalizability may be limited. Finally, our study excluded individuals who had persistent burnout.
Future work could determine what factors lead to prolonged or persistent burnout, which may not be resolved by the methods described here.
Conclusion
This study reveals the dual nature of how residents recover from and avoid burnout. Our findings suggest that making that distinction can guide future interventions by relieving the circumstantial contributors to burnout and addressing the existential contributors of burnout by promoting longitudinal reflection and discussion on professional and personal growth.
Supplementary Material
Footnotes
Editor's Note: The online version of this article contains examples of open, axial, and selective coding that informed the development of the qualitative themes and subthemes.
Funding: The authors report no external funding source for this study.
Conflict of interest: The authors declare they have no competing interests.
This work was presented at the Washington Chapter American College of Physicians Annual Meeting, Seattle, Washington, November 11–12, 2016; at the Northwest Regional Meeting of the Society of General Internal Medicine, Portland, Oregon, February 3, 2017; and at the Society of General Internal Medicine Annual National Meeting, Washington, DC, April 19–22, 2017.
The authors would like to thank Lynne Robins, PhD, for her thoughtful review of this manuscript.
What was known and gap
Attention has increasingly focused on resident burnout, yet little is known about how residents recover from burnout.
What is new
A qualitative study identified 2 types of burnout: circumstantial burnout during challenging assignments, with recovery; and existential burnout, with a likely need for intervention.
Limitations
Single site visit may limit generalizability; use of a single item screening tool.
Bottom line
Categorizing resident burnout into circumstantial and existential may help in identifying appropriate interventions.
References
- 1. . Maslach C, Jackson SE. . The measurement of experienced burnout. J Occup Behav. 1981; 2 2: 99– 113. [Google Scholar]
- 2. . Dyrbye LN, West CP, Satele D, et al. . Burnout among US medical students, residents, and early career physicians relative to the general US population. Acad Med. 2014; 89 3: 443– 451. [DOI] [PubMed] [Google Scholar]
- 3. . Schwenk TL. . Resident depression: the tip of a graduate medical education iceberg. JAMA. 2015; 314 22: 2357– 2358. [DOI] [PubMed] [Google Scholar]
- 4. . Lefebvre DC. . Perspective: resident physician wellness: a new hope. Acad Med. 2012; 87 5: 598– 602. [DOI] [PubMed] [Google Scholar]
- 5. . Shanafelt TD, Bradley KA, Wipf JE, et al. . Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002; 136 5: 358– 367. [DOI] [PubMed] [Google Scholar]
- 6. . Dyrbye L, Shanafelt T. . A narrative review on burnout experienced by medical students and residents. Med Educ. 2016; 50 1: 132– 149. [DOI] [PubMed] [Google Scholar]
- 7. . West CP, Huschka MM, Novotny PJ, et al. . Association of perceived medical errors with resident distress and empathy: a prospective longitudinal study. JAMA. 2006; 296 9: 1071– 1078. [DOI] [PubMed] [Google Scholar]
- 8. . West CP, Dyrbye LN, Erwin PJ, et al. . Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016; 388 10057: 2272– 2281. [DOI] [PubMed] [Google Scholar]
- 9. . Krasner MS, Epstein RM, Beckman H, et al. . Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA. 2009; 302 12: 1284– 1293. [DOI] [PubMed] [Google Scholar]
- 10. . Krug MF, Golob AL, Wander PL, et al. . Changes in resident well-being at one institution across a decade of progressive work hours limitations. Acad Med. 2017; 92 10: 1480– 1484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. . Dolan ED, Mohr D, Lempa M, et al. . Using a single item to measure burnout in primary care staff: a psychometric evaluation. J Gen Intern Med. 2015; 30 5: 582– 587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. . West CP, Dyrbye LN, Sloan JA, et al. . Single item measures of emotional exhaustion and depersonalization are useful for assessing burnout in medical professionals. J Gen Intern Med. 2009; 24 12: 1318– 1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. . Thomas NK. . Resident burnout. JAMA. 2004; 292 23: 2880– 2889. [DOI] [PubMed] [Google Scholar]
- 14. . Chou CM, Kellom K, Shea JA. . Attitudes and habits of highly humanistic physicians. Acad Med. 2014; 89 9: 1252– 1258. [DOI] [PubMed] [Google Scholar]
- 15. . Howe A, Smajdor A, Stöckl A. . Towards an understanding of resilience and its relevance to medical training. Med Educ. 2012; 46 4: 349– 356. [DOI] [PubMed] [Google Scholar]
- 16. . Corbin J, Strauss A. . Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. 4th ed. Thousand Oaks, CA: SAGE Publications Inc; 2015. [Google Scholar]
- 17. . Creswell JW. . Qualitative Inquiry and Research Design: Choosing Among Five Approaches. 2nd ed. Thousand Oaks, CA: SAGE Publications Inc; 2007. [Google Scholar]
- 18. . Hough CL, Hudson LD, Salud A, et al. . Death rounds: end-of-life discussions among medical residents in the intensive care unit. J Crit Care. 2005; 20 1: 20– 25. [DOI] [PubMed] [Google Scholar]
- 19. . Goitein L, Shanafelt TD, Wipf JE, et al. . The effects of work-hour limitations on resident well-being, patient care, and education in an internal medicine residency program. Arch Intern Med. 2005; 165 22: 2601– 2606. [DOI] [PubMed] [Google Scholar]
- 20. . Campbell J, Prochazka AV, Yamashita T, et al. . Predictors of persistent burnout in internal medicine residents: a prospective cohort study. Acad Med. 2010; 85 10: 1630– 1634. [DOI] [PubMed] [Google Scholar]
- 21. . West CP, Dyrbye LN, Rabatin JT, et al. . Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med. 2014; 174 4: 527– 533. [DOI] [PubMed] [Google Scholar]
- 22. . Bar-Sela G, Lulav-Grinwald D, Mitnik I. . “Balint group” meetings for oncology residents as a tool to improve therapeutic communication skills and reduce burnout level. J Cancer Educ. 2012; 27 4: 786– 789. [DOI] [PubMed] [Google Scholar]
- 23. . Ghetti C, Chang J, Gosman G. . Burnout, psychological skills, and empathy: Balint training in obstetrics and gynecology residents. J Grad Med Educ. 2009; 1 2: 231– 235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. . Kjeldmand D, Holmström I. . Balint groups as a means to increase job satisfaction and prevent burnout among general practitioners. Ann Fam Med. 2008; 6 2: 138– 145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. . Holden M, Buck E, Clark M, et al. . Professional identity formation in medical education: the convergence of multiple domains. HEC Forum. 2012; 24 4: 245– 255. [DOI] [PubMed] [Google Scholar]
- 26. . Cruess RL, Cruess SR, Boudreau JD, et al. . A schematic representation of the professional identity formation and socialization of medical students and residents: a guide for medical educators. Acad Med. 2015; 90 6: 718– 725. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


