Abstract
Background
Continuity between patients and physicians is a core principle of primary care and an accreditation requirement. Resident continuity clinics face challenges in nurturing continuity for their patients and trainees.
Objective
We undertook a scoping review of the literature to better understand published benchmarks for resident continuity; the effectiveness of interventions to improve continuity; and the impact of continuity on resident and patient satisfaction, patient outcomes, and resident career choice.
Methods
We developed a MEDLINE search strategy to identify articles that defined continuity in residency programs in internal medicine, family medicine, and pediatrics published prior to December 31, 2015, and used a quality evaluation tool to assess included studies.
Results
The review includes 34 articles describing 12 different measures of continuity. The usual provider of care and continuity for physician formulas were most commonly utilized, and mean baseline continuity was 56 and 55, respectively (out of a total possible score of 100). Clinic and residency program redesign innovations (eg, advanced access scheduling, team-based care, and block scheduling) were studied and had mixed impact on continuity. Continuity in resident clinics is lower than published continuity rates for independently practicing physicians.
Conclusions
Interventions to enhance continuity in resident clinics have mixed effects. More research is needed to understand how changes in continuity affect resident and patient satisfaction, patient outcomes, and resident career choice. A major challenge to research in this area is the lack of empanelment of residents' patients, creating difficulties in scheduling and measuring continuity visits.
Introduction
For many, the picture of an ideal primary care relationship suggests a health care team, often with a physician lead, with a deep and broad knowledge of a patient's medical and social history, and the ability to place new complaints and preventive health care in the context of that relationship. This continuous relationship is a core principle1,2 of primary care but has proved challenging to define. Continuity has been used in reference to location of service, medical record, medical group, and relationship between physician and patient.3 Longitudinal care has been used to separate the relationship between physician and patient across episodes of illness from other definitions of continuity.3,4 Improved continuity has been associated with fewer missed appointments, decreased redundancy in testing, and increased appropriate follow-up care.5 A body of literature evaluating the benefits of longitudinal continuity in the outpatient setting has shown improvements in mortality,6–8 health outcomes,9–12 and patient satisfaction13,14 as well as reduced health care costs.6,15
The Accreditation Council for Graduate Medical Education (ACGME) recognizes the value of continuity by requiring residency programs in family medicine (FM), internal medicine (IM), and pediatrics to create a continuous, long-term relationship for residents with a panel of patients.16–18 This continuity has been found to be a predictor for resident satisfaction in clinic19,20 and a core motivator for future practice in general IM.21,22 However, continuity remains a challenge in graduate medical education (GME) due to residents' limited time to establish therapeutic relationships and the complexities of simultaneously scheduling a wide variety of training experiences. Recent work hour limits have further complicated the ability to achieve this balance, leaving residency programs seeking innovative models to optimize their ambulatory experience.23,24
There are no benchmarks for optimal levels of continuity. In this environment, some have called for a transition to a more immersive ambulatory experience,25–27 while others have suggested a retreat from the focus on continuity in GME.28
We conducted a scoping review to map the current literature on the topic to better understand how continuity has been defined in the resident clinic setting. We focused our review on establishing benchmarks for resident continuity and exploring how clinic and programmatic innovations on continuity affect outcomes that include resident and patient satisfaction, patient outcomes, and resident career choice.
Methods
Data Sources
We conducted a MEDLINE search using “continuity of patient care” as a MeSH term or any of these keywords in the title/abstract: “coc,” “continuity,” “continuity of care,” and “continuity clinic(s).” These results were then narrowed to “internship and residency” as a MeSH term or 1 of these keywords in the title/abstract: “residency clinic(s)” or “residen*.” We evaluated all studies published prior to December 31, 2015. We further limited the search to English-language articles and US residency programs.
Study Selection
We included articles that provided a definition and quantitative value for continuity in resident ambulatory clinics in FM, IM, pediatrics, or medicine-pediatrics. We excluded articles that did not involve a long-term ambulatory continuity clinic and that were not original research. Two investigators (J.W. and E.D.S.) conducted abstract and title reviews, followed by full-text reviews of articles that either reviewer deemed eligible. Both investigators reviewed these texts and determined eligibility; all discrepancies were discussed and consensus was obtained.
Data Abstraction and Quality Assessment
We reviewed articles for study design, setting, number of patients and residents included, and definition of continuity, and evaluated the definition of primary physician used in the continuity calculation. In the studies with an intervention, we evaluated the overall impact of the intervention and its effect on continuity. We categorized interventions by educational and patient outcomes.
Study quality was evaluated using the Medical Education Research Study Quality Instrument.29,30 This measure evaluates several domains, including study design, sampling, data type, instrument validity, data analysis, and outcomes, and it has been examined with evidence of validity, which has a maximum score of 18.29 Response rate was not applicable in most studies, leaving 16.5 possible points. Two investigators (J.W. and E.D.S.) independently applied the instrument, discrepancies were discussed, and final scores were reached by consensus.
Data Synthesis and Analysis
Descriptive statistics, including mean, median, and standard deviation, were used to compare measures of continuity. For those studies that included a control and an experimental group, the control group was considered representative of the baseline continuity.
Results
The MEDLINE search yielded 1398 articles. A total of 95 articles underwent full-text review, and 34 articles met criteria for inclusion in this review. A flow diagram illustrating the process and a summary of studies and significant results are provided as online supplemental material.
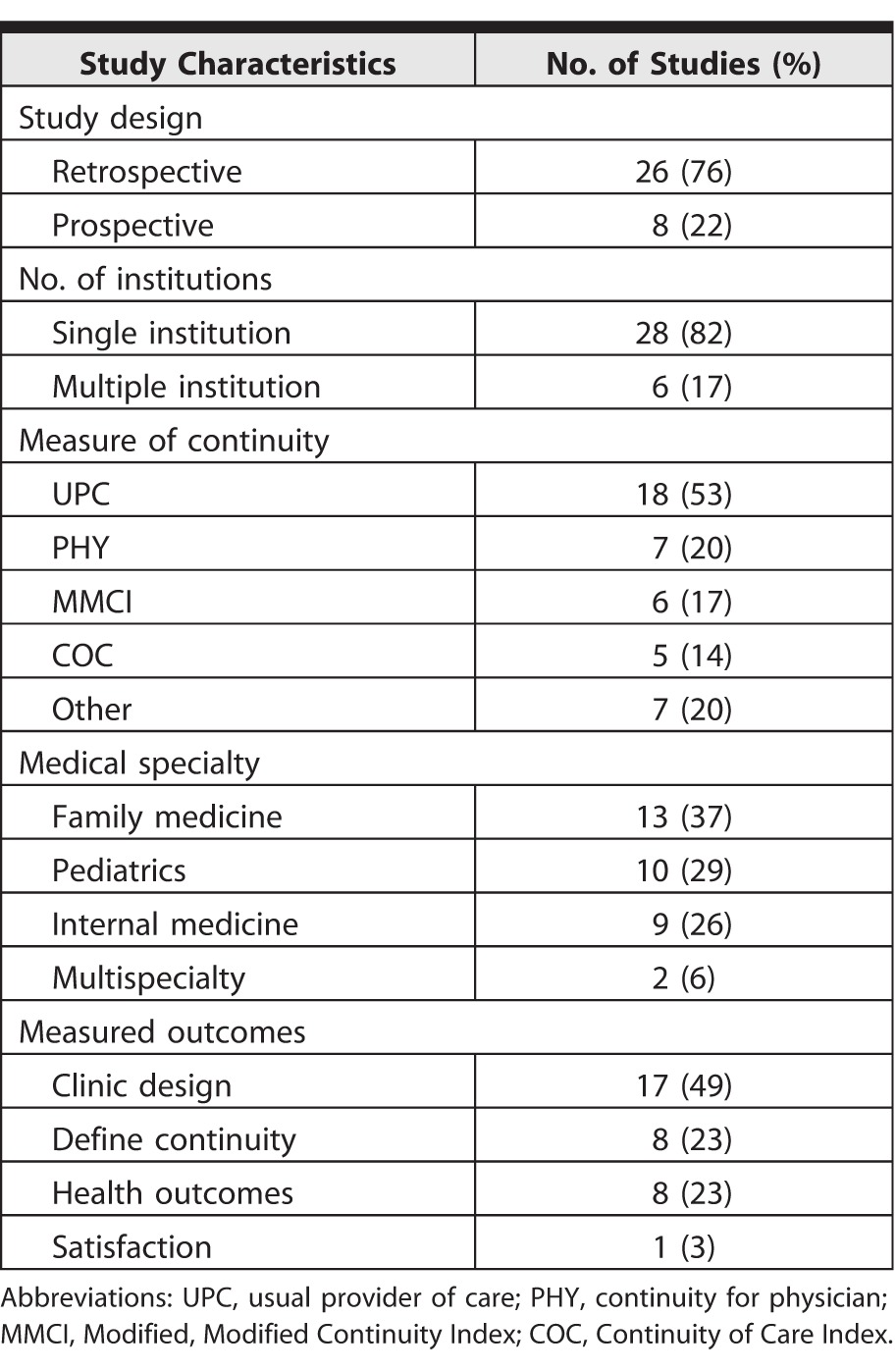
Characteristics of included studies are shown in Table 1. The majority selected were retrospective and single institution studies. Twelve studies25,26,31–40 describe an intervention; others provide a cross-sectional overview of continuity in a particular group. Median quality score using the Medical Education Research Study Quality Instrument was 12 (range, 9.5–14). A frequent concern was lack of a clear method to determine the primary resident used in continuity calculations.
Table 1.
Characteristics of Included Studies
Measures of Continuity
Studies included 12 different measures of continuity and 6 unique formulas. Four common measures used a 100-point scale, with 0 representing no continuity and 100 representing perfect continuity. For more information, a sample data set and calculation of continuity using these 4 measures are provided as online supplemental material. Table 2 shows baseline levels on these calculations reported in included studies by setting.
Table 2.
Studies by Program Type
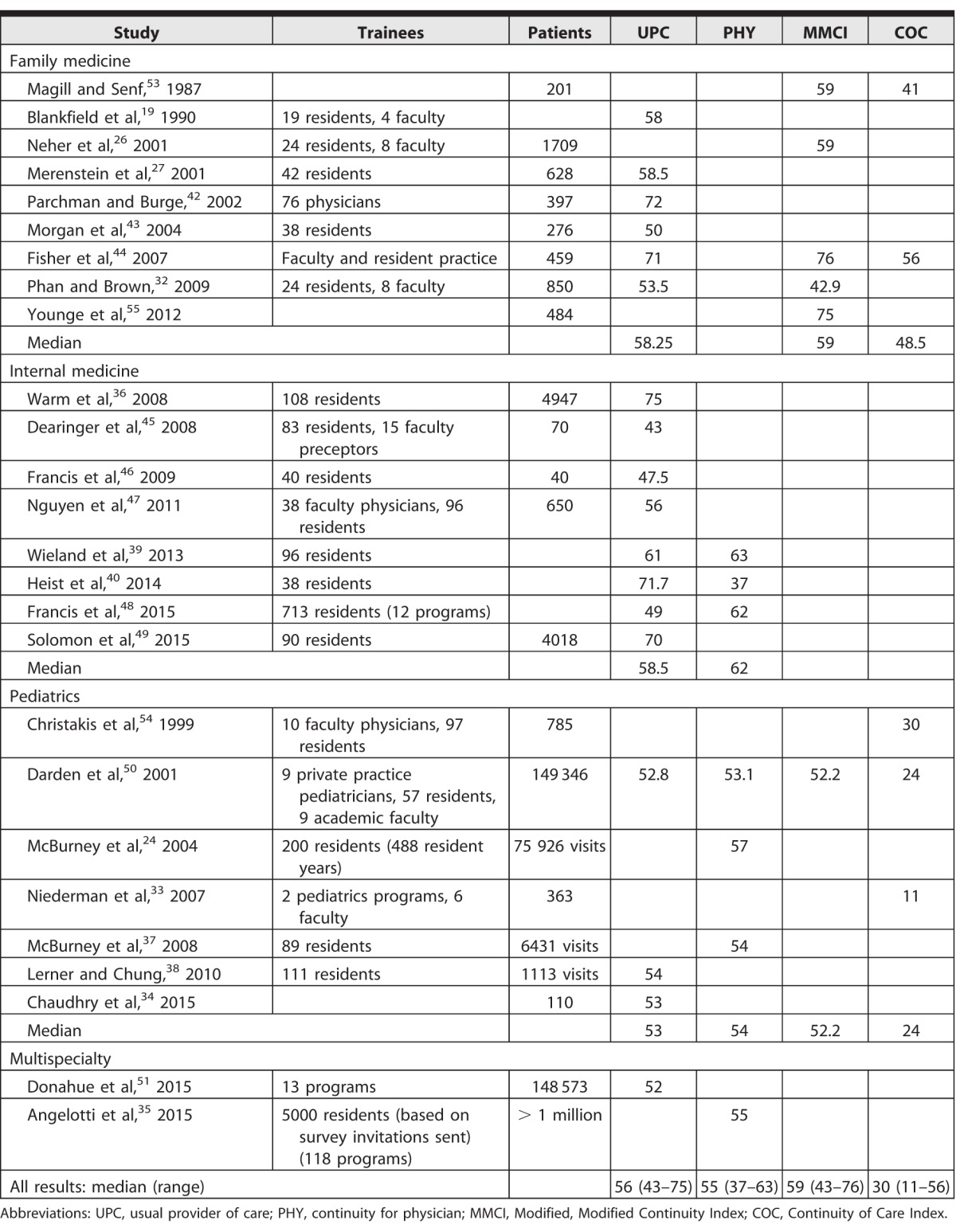
The most commonly utilized calculation was the usual provider of care (UPC) formula, which is the proportion of visits with their primary physician over the patient's total number of visits.41 This requires an assigned relationship between patient and provider. Many studies retrospectively assigned this relationship based on the provider the patient saw most frequently. The UPC was reported in 18 of the studies reviewed, representing more than 300 000 patients. Median baseline continuity using UPC was 56 (SD = 9.5, range, 43–75).19,27,32,34,36,38–40,42–51
The continuity for physician (PHY) formula50 is the number of appointments a physician has with his or her assigned patients over the physician's total number of appointments. As with UPC, an assigned provider-patient relationship is required for this calculation. The PHY was reported in 7 studies, representing nearly 1200 residents.24,35,37,39,40,48,50 Median baseline continuity by PHY was 55 (SD = 8.6, range, 37–63).
The Continuity of Care Index (COC)52 incorporates the number of different providers seen and the frequency of visits with each provider; it does not require an a priori designation of a primary physician. The results drop with increased numbers of providers and tend to be lower than other measures of continuity given the same data set. The COC was reported in 5 studies representing approximately 5200 patients.33,44,50,53,54 Median baseline continuity using the COC index was 30 (SD = 17, range, 11–56).
The Modified, Modified Continuity Index (MMCI)53 also evaluates the total number of physicians over the total number of visits, but it is simpler than the COC. The MMCI was reported in 6 studies, representing over 6700 patients.26,32,44,50,53,55 Median baseline MMCI was 59 (SD = 12.9, range, 43–76).
The UPC and PHY are the prominent calculations in more contemporary studies. The difference between these measures is highlighted in a study by the Educational Innovations Project Ambulatory Collaborative involving 12 IM residencies surveyed during 2010 through 2011.48 This study showed that as the number of clinic sessions increased, UPC rose and PHY declined. Conversely, as panel size increased, UPC declined and PHY rose. Another study confirmed the effect on UPC, estimating a 0.4% increase for each additional clinic per year and a 0.7% decrease for each added 10 patients in a resident panel.46 In contrast, a study that examined 488 resident years in a single pediatrics residency found a positive correlation between percentage of time in clinic (correlating with clinic sessions) and PHY (r = 0.22, P < .10).24
Clinic Redesign and Continuity
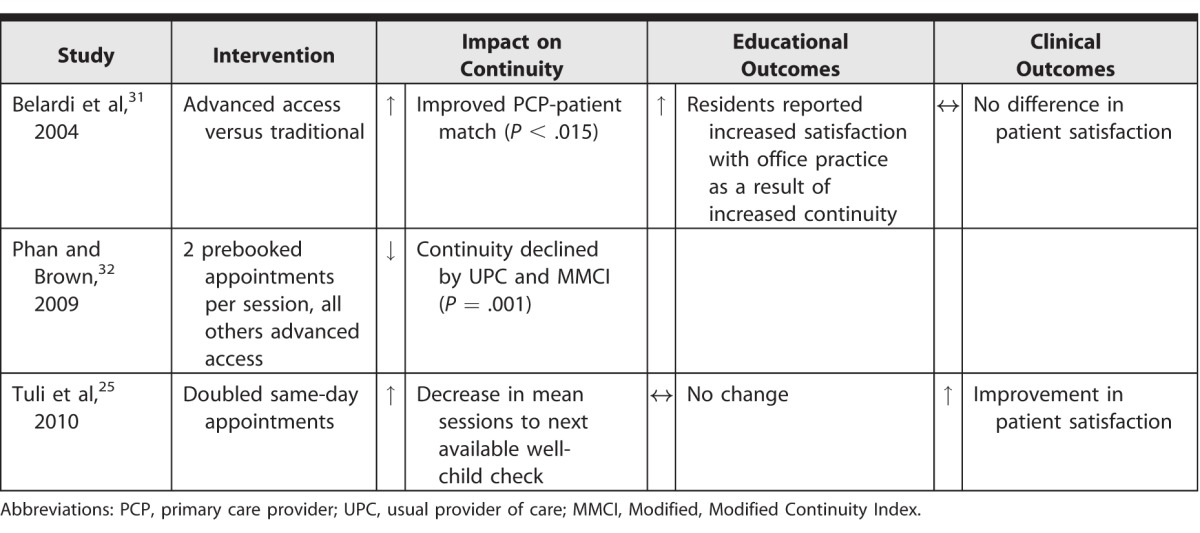
The 15 studies that focused on a redesign of aspects of the continuity clinic assessed the effect of advanced access scheduling,25,31,32 changes in clinic structure,33–35 and a change at the residency program level.23,26,27,36–40,48
Advanced access scheduling makes a portion of clinic appointments available for same-day scheduling. Three studies assessed the impact of advanced access scheduling (Table 3).25,31,32 An intervention that increased same-day appointments in an FM clinic from 40% to 75% for the combined resident and faculty practice increased the primary physician-patient match 3-fold (P = .01).31 In contrast, transitioning from less than 10% to more than 65% same-day appointments reduced continuity measured by UPC from 56 to 54 (P = .01).32 A third study showed that transitioning to 83% same-day appointments in a pediatrics clinic reduced the number of well-child checks seen in the acute clinic from 4% to 1.5% (P < .001), which was perceived as an improvement in continuity.25
Table 3.
Advanced Access Innovations
Changes at the clinic level were discussed in 3 studies33–35 shown in Table 4. Designing the electronic health record (EHR) to include a designated primary care resident and training clinic schedulers to preferentially schedule to this resident improved UPC from 53 to 77 in 1 pediatrics residency.34 A second study described the use of the Hospital Medical Home program in New York State, which provided coaching and funding to transform hospital clinics to patient-centered medical homes utilizing interprofessional team models. This program was implemented in 118 residency programs in multiple specialties, which encompassed more than 5000 residents.35 While many programs had not measured baseline continuity, postintervention continuity was 55 by PHY, which residents and administrators perceived to be an improvement. A third study also used interprofessional team-based redesign, which embedded an early childhood specialist in a pediatrics residency practice; this increased continuity by COC from 11 to 24.33
Table 4.
Clinic Structure Innovations

Interventions to improve continuity with a change in overall program structure are shown in Table 5.26,37,38 The 2003 ACGME duty hour standards led many residency programs to adjust their clinic schedules. One study that evaluated the impact of a schedule change in 1 pediatrics residency found no change in PHY.37 A second, which described a change to a fixed half-day clinic in a pediatrics program, found that 75% of the patient sessions actually occurred on the assigned clinic day, with an increase in UPC from 54 to 64 (P < .01).37 A third study increased clinic sessions in an FM program, with sessions of varying length, which increased MMCI from 59 to 64 (P = .001).26
Table 5.
Residency Structure Innovations
Several studies investigated new scheduling schemes to address the competing demands of inpatient and outpatient responsibilities. One study assessed 6 FM residencies, 3 of which had transitioned to a longitudinal model, defined as residents learning primarily through care of their own patients in a family practice center. The primary outcome was continuity, and the authors found no difference in UPC between the 2 models.27 The second studied 713 residents from 12 IM programs using 3 models: weekly continuity clinic, block scheduling with discrete inpatient and outpatient rotations, and a combination model with weekly clinic and 2 to 6 months of additional ambulatory rotations over 3 years.23,48 The UPC was highest for the block scheduling model and lowest for the weekly clinic, while PHY was lowest for the block model. Resident-perceived continuity was highest in the combination model.
Three studies in IM reflected unique clinic scheduling models. One assessed an ambulatory long block consisting of 3 clinic sessions per week for months 17 to 28 of the residency.36 The UPC increased from 75 to 89 with this model (P = .003). In the second model, in which residents had 2 half-day sessions per week during outpatient months alternating with no clinic during inpatient months, decreased both PHY and UPC.41 However, the proportion of missed appointments decreased, and there were no differences in satisfaction or clinical outcomes. The third study of a 4+1 model (4-week block with no clinic, followed by 1 week of a more intense ambulatory experience with 7 to 8 clinic sessions) found a reduction in UPC from 71 to 63 (P = .008), while PHY increased from 37 to 52 (P = .0001).40 No studies in our sample were able to comment on an intervention's impact on resident career choice.
Discussion
While previous systematic reviews have investigated continuity in the general outpatient setting,9,13 we present the first review of continuity in resident clinic. The continuously evolving environment of GME and the transient nature of residency offer a unique context to study this important measure of patient care.
Regardless of the measure used, the literature suggested that there is considerable room for improvement in continuity for resident clinics. The median continuity was 56 and 55 for UPC and PHY, respectively. In continuity studies that do not focus on trainees, UPC ranges from 63 to 78 in recent publications.56–58 Despite significant variability in studies across clinic settings, geographic location, and patient populations, resident continuity is consistently lower compared with that of physicians in practice.47,50,54 When parsed specifically, time in clinic and panel size seem to have the most impact on resident-patient continuity.24,26,37,46 These 2 factors appear to have an opposing impact on PHY and UPC. Providing more appointment availability per resident, while holding panel size stable, may offer more opportunities for patients to schedule with their primary resident, increasing UPC. A larger panel size, while holding number of appointments stable, will increase PHY, as there will be more assigned patients to schedule with a primary resident. Clinic redesign efforts should work to balance both issues to maximize both measures.
Primary care delivery systems are changing across the United States,59–62 and residency programs are no exception. The ACGME common program requirements for pediatrics includes the integration of a medical home for all residents, emphasizing the importance of this holistic approach.18 The 2 studies that evaluated the impact of a transition to team-based, patient-centered care had largely positive results.33,35 As the definition of continuity evolves to include continuity to an interprofessional team, the result may be new approaches to study continuity, as patients ultimately may feel a tighter connection to a nonphysician on the team compared with a trainee, who by nature may only have a few years working in the clinic setting.
Either in response to external changes or with a goal to improve the ambulatory experience, residency programs across the country have undertaken scheduling changes that dramatically impact their ambulatory care segments. While some report success with improved clinical and educational outcomes, it is not clear whether improved continuity is the driver of that success. Other, simpler scheduling changes, including advanced access and fixed clinic days, have shown inconsistent impact on continuity.
Patient empanelment with residents is a major challenge in measuring continuity, and this issue may have become both more important and more visible with the advent of the EHR. Empanelment means that a given patient has a clearly defined primary resident physician (ie, a patient is included in a resident panel). Many studies did not start with such a relationship defined and assessed the impact post hoc. This was a quality concern, as retrospective identification of the primary care resident may bias results toward higher continuity. In contrast, simply identifying the primary resident in the EHR led to a 25% increase in continuity, in addition to improving the accuracy of continuity calculations.50 We propose that an effective approach to enhancing continuity will be empanelment of resident patients, which will make continuity easier to measure and to achieve in the practical sense. Flexibility of EHR design and institutional support may go a considerable way in solving the issue of low patient continuity in training settings.
Our systematic approach, large sample size (n = 34), and use of recent studies (two-thirds published after 2003) in an evolving field are strengths of our study. Our review highlights the rising importance of continuity over time. Limitations of our review include reliance on a single database as well as a heavily retrospective and observational study set, often with short study durations to evaluate change in a transient group. As new models are developed, studies should assess continuity but should also expand the focus to a broader range of outcomes. Specifically, multi-study studies, larger samples, and longer follow-up are needed to understand whether these changes will affect resident perceptions of readiness for outpatient medicine and, ultimately, career choice. The heterogeneous populations included in our study add strength in the narrative sense, allowing a thorough description of the continuity within the residency setting. However, the heterogeneity does make it difficult to synthesize the data or make conclusions that are generalizable.
Conclusion
Longitudinal continuity of care in the outpatient setting, long a core pillar of primary care practice, has been challenging to achieve in the GME setting. While we found both simple and complex interventions that improved continuity, there were no consistent keys to achieving higher levels of continuity. The definition of continuity may also be changing with an evolving primary care system. New research in this field may consider evaluating multiple measures of continuity, including team continuity, to better understand the importance of continuity within a resident clinic.
Supplementary Material
Footnotes
Editor's Note: The online version of this article contains a PRISMA diagram for study selection, sample patient data set and continuity calculations, and a summary of the articles.
Funding: The authors report no external funding source for this study.
Conflict of interest: The authors declare they have no competing interests.
References
- 1. . Saultz JW. . Continuity of care. : Saultz JW, . Textbook of Family Medicine. New York, NY: McGraw-Hill; 2000: 52– 77. [Google Scholar]
- 2. . Donaldson M, Yordy K, Lohr K, et al. Primary Care: America's Health in a New Era. Washington, DC: National Academy of Sciences; 1996. [PubMed] [Google Scholar]
- 3. . Rogers J, Curtis P. . The concept and measurement of continuity in primary care. Am J Public Health. 1980; 70 2: 122– 127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. . Starfield B. . Continuous confusion? Am J Public Health. 1980; 70 2: 117– 119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. . Shortell SM, Care SM, May N. . Continuity of medical care: conceptualization and measurement. Med Care. 1976; 14 5: 377– 391. [DOI] [PubMed] [Google Scholar]
- 6. . Cho J, Park JH, Kim H. . Impact of continuity of care on mortality and health care costs: a nationwide cohort study in Korea. Ann Fam Med. 2014; 12 6: 534– 542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. . Leleu H, Minvielle E. . Relationship between longitudinal continuity of primary care and likelihood of death: analysis of national insurance data. PLoS One. 2013; 8 8: 2– 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. . Wolinsky FD, Bentler SE, Liu L, et al. Continuity of care with a primary care physician and mortality in older adults. J Gerontol A Biol Sci Med Sci. 2010; 65 4: 421– 428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. . Saultz JW, Lochner J. . Interpersonal continuity of care and care outcomes: a critical review. Ann Fam Med. 2005; 3 2: 159– 166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. . Nelson K, Sun H, Dolan E, et al. Elements of the patient-centered medical home associated with health outcomes among veterans: the role of primary care continuity, expanded access, and care coordination. J Ambul Care Mange. 2014; 37 4: 331– 338. [DOI] [PubMed] [Google Scholar]
- 11. . Guthrie B, Wyke S, Guthrie B. . Does continuity in general practice really matter? BMJ. 2000; 321 7263: 734– 736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. . Mainous AG, Koopman RJ, Gill JM, et al. Relationship between continuity of care and diabetes control: evidence from the third National Health and Nutrition Examination Survey. Am J Public Health. 2004; 94 1: 66– 70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. . Saultz JW. . Interpersonal continuity of care and patient satisfaction: a critical review. Ann Fam Med. 2004; 2 5: 445– 451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. . Hjortdahl P, Laerum E. . Continuity of care in general practice: effect on patient satisfaction. BMJ. 1992; 304 6837: 1287– 1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. . Weiss LJ, Blustein J. . Faithful patients: the effect of long-term physician-patient relationships on the costs and use of health care by older Americans. Am J Public Health. 1996; 86 12: 1742– 1747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. . Accreditation Council for Graduate Medical Education. ACGME program requirements for graduate medical education in internal medicine. https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/140_internal_medicine_2017-07-01.pdf. Accessed December 14, 2017.
- 17. . Accreditation Council for Graduate Medical Education. ACGME program requirements for graduate medical education in family medicine. http://www.acgme.org/portals/0/pfassets/programrequirements/120_family_medicine_2017-07-01.pdf. Accessed December 14, 2017.
- 18. . Accreditation Council for Graduate Medical Education. ACGME program requirements for graduate medical education in pediatrics. https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/320_pediatrics_2017-07-01.pdf. Accessed December 14, 2017.
- 19. . Blankfield RP, Kelly RB, Alemagno SA, et al. Continuity of care in a family practice residency program. J Fam Pract. 1990; 31 1: 69– 73. [PubMed] [Google Scholar]
- 20. . Barnett DR, Bass PF, Griffith CH, et al. Determinants of resident satisfaction with patients in their continuity clinic. J Gen Intern Med. 2004; 19(5, pt 1):456–459. [DOI] [PMC free article] [PubMed]
- 21. . Peccoralo LA, Tackett S, Ward L, et al. Resident satisfaction with continuity clinic and career choice in general internal medicine. J Gen Intern Med. 2013; 28 8: 1020– 1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. . Laponis R, O'Sullivan PS, Hollander H, et al. Educating generalists: factors of resident continuity clinic associated with perceived impact on choosing a generalist career. J Grad Med Educ. 2011; 3 4: 469– 474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. . Francis MD, Thomas K, Langan M, et al. Clinic design, key practice metrics, and resident satisfaction in internal medicine continuity clinics: findings of the educational innovations project ambulatory collaborative. J Grad Med Educ. 2014; 6 2: 249– 255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. . McBurney PG, Moran CM, Ector WL, et al. Time in continuity clinic as a predictor of continuity of care for pediatric residents. Pediatrics. 2004; 114 4: 1023– 1027. [DOI] [PubMed] [Google Scholar]
- 25. . Tuli SY, Thompson LA, Ryan KA, et al. Improving quality and patient satisfaction in a pediatric resident continuity clinic through advanced access scheduling. J Grad Med Educ. 2010; 2 2: 215– 221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. . Neher JO, Kelsberg G, Oliveira D. . Improving continuity by increasing clinic frequency in a residency setting. Fam Med. 2001; 33 10: 751– 755. [PubMed] [Google Scholar]
- 27. . Merenstein D, D'Amico F, Devine B, et al. Longitudinal versus traditional residencies: a study of continuity of care. Fam Med. 2001; 33 10: 746– 750. [PubMed] [Google Scholar]
- 28. . Huddle TS, Heudebert GR. . Internal medicine training in the 21st century. Acad Med. 2008; 83 10: 910– 915. [DOI] [PubMed] [Google Scholar]
- 29. . Reed DA, Beckman TJ, Wright SM, et al. Predictive validity evidence for medical education research study quality instrument scores: quality of submissions to JGIM's Medical Education Special Issue. J Gen Intern Med. 2008; 23 7: 903– 907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. . Reed DA, Cook DA, Beckman TJ, et al. Association between funding of published medical education research. JAMA. 2007; 298 9: 1002– 1009. [DOI] [PubMed] [Google Scholar]
- 31. . Belardi FG, Weir S, Craig FW. . A controlled trial of an advanced access appointment system in a residency family medicine center. Fam Med. 2004; 36 5: 341– 345. [PubMed] [Google Scholar]
- 32. . Phan K, Brown SR. . Decreased continuity in a residency clinic: a consequence of open access scheduling. Fam Med. 2009; 41 1: 46– 50. [PubMed] [Google Scholar]
- 33. . Niederman LG, Schwartz A, Connell KJ, et al. Healthy Steps for Young Children program in pediatric residency training: impact on primary care outcomes. Pediatrics. 2007; 120 3: e596– e603. [DOI] [PubMed] [Google Scholar]
- 34. . Chaudhry SR, Hanna-Attisha M, LaChance J, et al. Primary resident physician: improving continuity of care. J Grad Med Educ. 2015; 7 2: 291– 292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. . Angelotti M, Bliss K, Schiffman D, et al. Transforming the primary care training clinic: New York State's hospital medical home demonstration pilot. J Grad Med Educ. 2015; 7 2: 247– 252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. . Warm EJ, Schauer DP, Diers T, et al. The ambulatory long-block: an Accreditation Council for Graduate Medical Education (ACGME) Educational Innovations Project (EIP). J Gen Intern Med. 2008; 23 7: 921– 926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. . McBurney PG, Gustafson KK, Darden PM. . Effect of 80-hour workweek on continuity of care. Clin Pediatr (Phila). 2008; 47 8: 803– 808. [DOI] [PubMed] [Google Scholar]
- 38. . Lerner CF, Chung PJ. . Continuity of care in fixed-day versus variable-day resident continuity clinics. Acad Pediatr. 2010; 10 2: 119– 123. [DOI] [PubMed] [Google Scholar]
- 39. . Wieland ML, Halvorsen AJ, Chaudhry R, et al. An evaluation of internal medicine residency continuity clinic redesign to a 50/50 outpatient-inpatient model. J Gen Intern Med. 2013; 28 8: 1014– 1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. . Heist K, Guese M, Nikels M, et al. Impact of 4+1 block scheduling on patient care continuity in resident clinic. J Gen Intern Med. 2014; 29 8: 1195– 1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. . Breslau N, Reeb K. . Continuity of care in a university based practice. J Med Educ. 1975; 50 10: 965– 969. [DOI] [PubMed] [Google Scholar]
- 42. . Parchman ML, Burge SK. . Continuity and quality of care in type 2 diabetes. J Fam Pract. 2002; 51 7: 619– 624. [PubMed] [Google Scholar]
- 43. . Morgan ED, Pasquarella M, Holman JR. . Continuity of care and patient satisfaction in a family practice clinic. J Am Board Fam Med. 2004; 17 5: 341– 346. [DOI] [PubMed] [Google Scholar]
- 44. . Fisher M, Sloane P, Edwards L, et al. Continuity of care and hypertension in a university-based practice. Ethn Dis. 2007; 17: 693– 698. [PubMed] [Google Scholar]
- 45. . Dearinger AT, Wilson JF, Griffith CH, et al. The effect of physician continuity on diabetic outcomes in a resident continuity clinic. J Gen Intern Med. 2008; 23 7: 937– 941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. . Francis MD, Zahnd WE, Varney A, et al. Effect of number of clinics and panel size on patient continuity for medical residents. J Grad Med Educ. 2009; 1 2: 310– 315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. . Nguyen DL, Dejesus RS, Wieland ML. . Missed appointments in resident continuity clinic: patient characteristics and health care outcomes. J Grad Med Educ. 2011; 3 3: 350– 355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. . Francis MD, Wieland ML, Drake S, et al. Clinic design and continuity in internal medicine resident clinics: findings of the educational innovations project ambulatory collaborative. J Grad Med Educ. 2015; 7 1: 36– 41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. . Solomon SR, Gooding HC, Reyes Nieva H, et al. Acute care utilization by patients after graduation of their resident primary care physicians. J Gen Intern Med. 2015; 30 11: 1611– 1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. . Darden PM, Ector W, Moran C, et al. Comparison of continuity in a resident versus private practice. Pediatrics. 2001; 108 6: 1263– 1268. [DOI] [PubMed] [Google Scholar]
- 51. . Donahue KE, Reid A, Lefebvre A, et al. Tackling the triple aim in primary care residencies: the I3 POP Collaborative. Fam Med. 2015; 47 2: 91– 97. [PubMed] [Google Scholar]
- 52. . Bice T, Boxerman S. . A quantitative measure of continuity of care. Med Care. 1977; 15 4: 347– 349. [DOI] [PubMed] [Google Scholar]
- 53. . Magill M, Senf J. . A new method for measuring continuity of care in family practice residencies. J Fam Pract. 1987; 24 2: 165– 168. [PubMed] [Google Scholar]
- 54. . Christakis DA, Wright JA, Koepsell TD, et al. Is greater continuity of care associated with less emergency department utilization? Pediatrics. 1999; 103(4, pt 1):738–742. [DOI] [PubMed]
- 55. . Younge R, Jani B, Rosenthal D, et al. Does continuity of care have an effect on diabetes quality measures in a teaching practice in an urban underserved community? J Health Care Poor Underserved. 2012; 23 4: 1558– 1565. [DOI] [PubMed] [Google Scholar]
- 56. . Mittelstaedt TS, Mori M, Lambert WE, et al. Provider practice characteristics that promote interpersonal continuity. J Am Board Fam Med. 2013; 26 4: 356– 365. [DOI] [PubMed] [Google Scholar]
- 57. . Gill J, Mainous A, Diamond J, et al. Impact of provider continuity on quality of care for persons with diabetes mellitus. Ann Fam Med. 2003; 1 3: 162– 170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. . Hetlevik Ø, Gjesdal S. . Personal continuity of care in Norwegian general practice: a national cross-sectional study. Scand J Prim Health Care. 2012; 30 4: 214– 221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. . Sinsky CA, Willard-Grace R, Schutzbank AM, et al. In search of joy in practice: a report of 23 high-functioning primary care practices. Ann Fam Med. 2013; 11 3: 272– 278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. . Linzer M, Bitton A, Tu SP, et al. The end of the 15–20 minute primary care visit. J Gen Intern Med. 2015; 30 11: 1584– 1586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. . Kernan W, Elnicki DM, Hauer K. . The selling of primary care 2015. J Gen Intern Med. 2015; 30 9: 1376– 1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. . Whitcomb ME, Cohen JJ. . The future of primary care medicine. N Engl J Med. 2004; 351 7: 710– 712. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.



