Abstract
The elbow comprises a complex of bony and ligamentous stabilizers that provide both primary and secondary constraints to elbow instability. Through trauma and overuse, classic instability patterns arise by loss of these important stabilizers. The diagnosis of elbow instability can made using specific examination maneuvers and testing to diagnose the clinical pattern. This article reviews the elbow’s unique anatomy and biomechanical characteristics and these are applied when reviewing the maneuvers and testing used to diagnose elbow instability.
Keywords: Valgus instability, posterolateral rotatory instability, varus posteromedial rotatory instability, elbow biomechanics
Elbow instability may arise through chronic overuse syndromes or as posttraumatic sequelae. Patients with chronic instability classically present with pain, apprehension, or mechanical symptoms after movements that bring about joint subluxation. A careful history should include exacerbating activities, pain location, mechanical symptoms, associated neurological symptoms, athletic participation, decrease in athletic performance, prior elbow trauma, and elbow surgery. A focused physical examination with specific diagnostic maneuvers can help guide the differential diagnosis.1 Judicious use of additional imaging may confirm the suspected diagnosis and assist in preoperative planning.
The purpose of this current concepts article is to discuss the osseous and ligamentous stabilizers of the elbow and to review the diagnostic maneuvers and imaging studies used to evaluate classic elbow instability patterns.
ANATOMY
Osteology
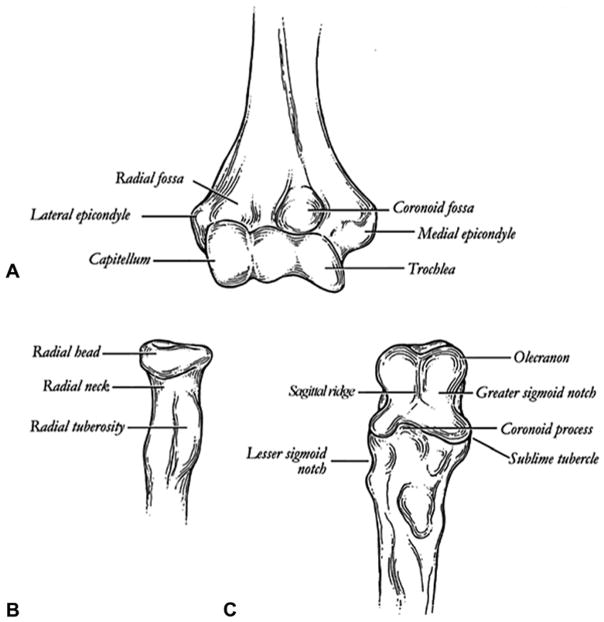
The elbow is a trochleogingylomoid joint composed of 2 primary motions: the ulnohumeral articulation is hinged, ginglymoid, and the radiocapitellar articulation is radial, trochoid. The distal humerus is composed of 2 articulations: the trochlea, a spool-shaped articulation along the long axis of the distal humerus, and the capitellum, a hemispheric structure lateral to the trochlea. The trochlea has a slight posterior tilt that prevents posterior translation by relying on the coronoid buttress.2,3 The proximal ulna contains 2 articulations, the greater and lesser sigmoid notches. The trochlea and greater sigmoid notch have highly congruent anatomy with nearly 180° of articular contact during elbow range of motion. The lesser sigmoid notch articulates with the margin of the radial head at the proximal radioulnar joint. The radial head is a concave elliptical structure, covered with articular cartilage along the radiocapitellar joint and approximately 270° of the articular margin; this articulates with both the capitellum and the lesser sigmoid notch. The radial head functions in pronation and supination and as an anterior and valgus buttress of the elbow.1–3
The coronoid process of the proximal ulna is an anterior and varus buttress of the elbow composed of tip, body, anterolateral facet, and anteromedial facet. The sublime tubercle, on the anteromedial facet, is the insertion for the anterior bundle of the medial collateral ligament (MCL).4 The osseous stability of the elbow is maximized in flexion owing to symmetrical positioning of the coronoid and radial head within their respective fossae (Fig. 1).
FIGURE 1.
Osseous anatomy of the elbow. A Distal humerus. B Proximal radius. C Proximal ulna. (From Total elbow arthroplasty design. In: Williams GR, Yamaguchi K, Ramsey ML, et al, eds. Shoulder and Elbow Arthroplasty. Philadelphia: Lippincott Williams & Wilkins; 2005:301. Reprinted with permission.)
Soft tissue anatomy
The collateral ligaments of the elbow are medial and lateral capsular thickenings that provide enhanced stability. The MCL, also known as the ulnar collateral ligament, comprises 3 ligamentous portions: anterior bundle (AMCL), posterior bundle, and transverse ligament (Cooper ligament). The AMCL and the posterior bundle originate at the anteroinferior medial epicondyle of the elbow. This origin lies posterior to the axis of the elbow, and therefore, elbow flexion increases ligament tension. The AMCL inserts at the sublime tubercle on the coronoid and the posterior bundle inserts on the medial olecranon.2,5
The lateral collateral ligament (LCL) is a complex with 4 primary ligamentous portions: lateral ulnar collateral ligament (LUCL), radial collateral ligament (RCL), annular ligament, and accessory collateral ligament. The LUCL and RCL originate from an isometric point on the inferior surface of the lateral epicondyle, providing consistent tension through elbow motion. The LUCL attaches to the supinator crest of the proximal ulna and is a restraint to varus and posterolateral rotatory instability (PRLI). The annular ligament encircles the radial head and attaches to the anterior and posterior margins of the lesser sigmoid notch. The RCL attaches to the annular ligament to stabilize the radial head2,4,5 (Fig. 2).
FIGURE 2.
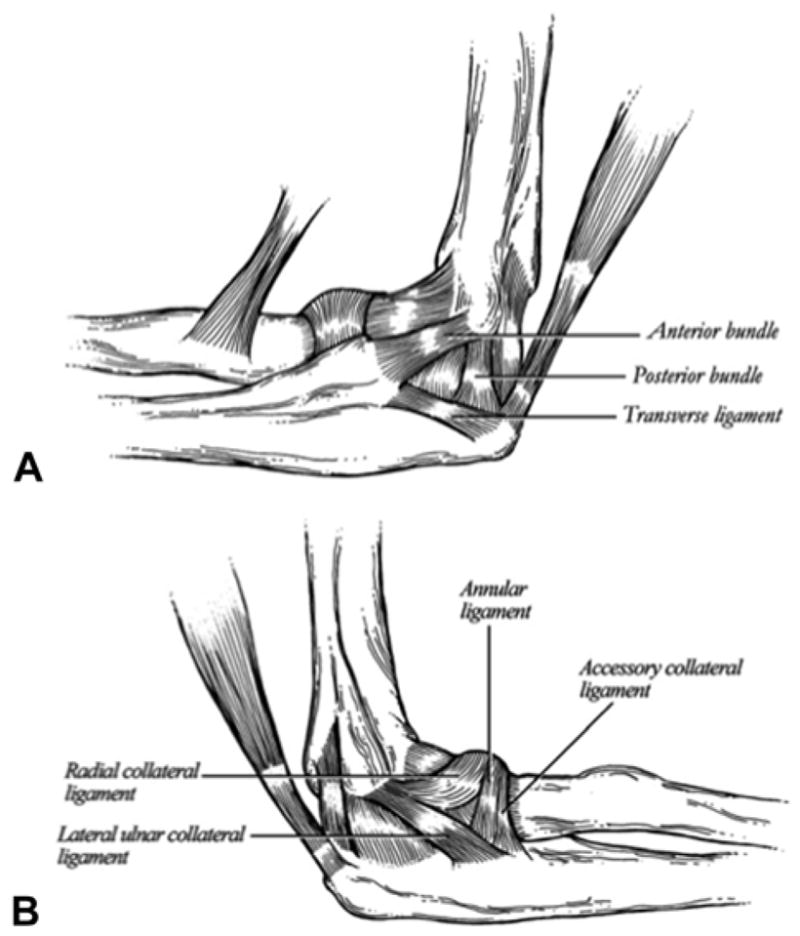
Medial and lateral ligamentous stabilizers of the elbow. A MCL complex. B LCL complex. (From Total elbow arthroplasty design. In: Williams GR, Yamaguchi K, Ramsey ML, et al, eds. Shoulder and Elbow Arthroplasty. Philadelphia: Lippincott Williams & Wilkins; 2005:303. Reprinted with permission.)
Muscles crossing the elbow compress the elbow joint, enhancing the osseous stability of the elbow and functioning as dynamic constraints.4,5 The anconeus deserves specific attention because it is a major dynamic constraint to varus and PRLI.2 The medial flexor musculature of the elbow—the flexor carpi ulnaris, flexor carpi radialis, flexor digitorum superficialis, and pronator teres—resists valgus forces; and the lateral extensor musculature— extensor carpi ulnaris, extensor digitorum communis, extensor carpi radialis brevis, extensor carpi radialis longus, and anconeus—resist varus forces.2,5
BIOMECHANICS
Elbow stability is provided by static and dynamic stabilizers. There are 3 primary static constraints: the ulnohumeral articulation, the AMCL, and the LCL complex. Secondary static constraints include the radiocapitellar articulation, the common flexor tendons, the common extensor tendons, and the joint capsule. Muscles crossing the elbow compose the dynamic stabilizers.6
Normal elbow range of motion is from 0° at full extension to 140° of flexion, with a range of 30° to 130° required for activities of daily living. The radiocapitellar joint allows approximately 180° of pronation-supination along an axis from the center of the radial head to the distal ulna; 50° of pronation and 50° of supination are required for activities of daily living.2
Within the ulnohumeral articulation, the coronoid process is the most important articular stabilizer of the elbow. The radial head and coronoid buttress against the intrinsic posteriorly directed muscular pull of the flexors and extensors to prevent posterior translation of the forearm. Through serial resection of the coronoid, Closkey et al7 demonstrated that 50% of the coronoid height is necessary for elbow stability, with increased elbow instability in extension. Morrey and An3 demonstrated that the radial head is a secondary stabilizer relative to the coronoid.
The MCL functions as a restraint to valgus and posteromedial rotatory instability. It functions as the primary restraint to valgus stress, and the radial head provides a secondary restraint. The MCL provides approximately one-third of the valgus stability in extension, versus half of the stability in 90° of flexion. The AMCL of the MCL provides the majority of the restraint to valgus and posteromedial rotatory instability; it is composed of 2 bands with the anterior band functioning as the primary restraint from 0° to 90° flexion and the anterior and posterior bands functioning as coprimary restraints at greater than 90° flexion.2,5 With an intact MCL, radial head resection does not cause significant valgus instability; however, upon resection of the MCL, the joint sub-luxates, thus demonstrating that the radiocapitellar joint is a secondary restraint to valgus stress.2,8 Isolated injury to the posterior bundle of the MCL may contribute to posteromedial rotatory instability. The forearm flexors provide dynamic stabilization to valgus force. With MCL transection, maximal valgus instability is seen at 70°, and maximal posteromedial rotational instability is at 60°. Laboratory studies demonstrate that MCL-deficient elbows are most unstable in neutral rotation.2,5
The LCL complex is the primary restraint to PRLI and has a lesser role in varus instability. With varus stress, the osseous stability of the ulnohumeral anatomy provides the majority of joint stability; the LCL complex resists approximately 10% varus stress. Initial studies suggested the LUCL to be the primary stabilizer within the LCL complex; however, recent work demonstrates that the LCL complex functions as a unit to prevent posterolateral instability and stabilize the radiohumeral, radioulnar, and ulnohumeral joints. The extensor musculature at the elbow is an important dynamic stabilizer. Lateral collateral ligament–deficient elbows are most unstable in supination.2,5
The joint capsule plays a critical role in elbow joint stability. Multiple studies have demonstrated that the anterior joint capsule provides significant resistance to joint distraction, joint hyperextension, and valgus stress. Although no studies have evaluated the posterior capsule function, it has been suggested that the posterior capsule resists joint hyperflexion and posterior directed forces.5
DIAGNOSTIC MANEUVERS
Valgus instability
Valgus instability arises through injuries to the MCL, specifically the AMCL. Medial collateral ligament injuries may occur after trauma, such as an elbow dislocation, or as a repetitive overuse injury, commonly seen in overhead-throwing athletes. The typical history includes a “pop” and medial elbow pain following throwing activities, or patients may present with recurrent medial elbow pain, classically during the late cocking to early acceleration phase of throwing. Athletes typically complain of a progressive loss of velocity, accuracy, and endurance, which may be exacerbated by glenohumeral internal rotation deficits common to throwing athletes. The physical examination typically elicits tenderness over the MCL (81%–94% sensitivity, 22% specificity for an MCL tear).9
Multiple examination maneuvers have been described and these are demonstrated in Video 1 (available on the Journals Web site at www.jhandsurg.org). A list of the included examination maneuvers is in Table 1. In the valgus stress test, the elbow is placed in 20° to 30° of flexion with the forearm supinated and a valgus stress is applied. The test is positive when no firm end point is palpated, greater than 1 mm of medial joint opening is noted (fluoroscopically), or there is reproduction of the patient’s pain. The valgus stress test is 66% sensitive and 60% specific. Although commonly used, this test does not exploit the position of maximum elbow instability (70° flexion and neutral rotation).9,10
TABLE 1.
Diagnostic Maneuvers Used in Evaluating Elbow Instability
| Valgus Instability | Valgus stress test |
| Milking maneuver | |
| Modified milking maneuver | |
| Moving valgus stress test | |
| PLRI | Lateral pivot-shift test |
| Posterolateral rotatory drawer test | |
| Chair push-up test | |
| Prone push-up test | |
| Table-top relocation test | |
| VPMI | Gravity-assisted varus stress test |
The milking maneuver tests the AMCL; it is performed with the shoulder externally rotated and the elbow flexed beyond 90°. A valgus force is applied by pulling the patient’s thumb while the examiner’s other hand stabilizes the elbow and palpates the medial joint line. A modification of the milking maneuver is performed with the shoulder adducted, maximally externally rotated, and the elbow flexed to 70° as a valgus stress is applied by pulling the thumb.9
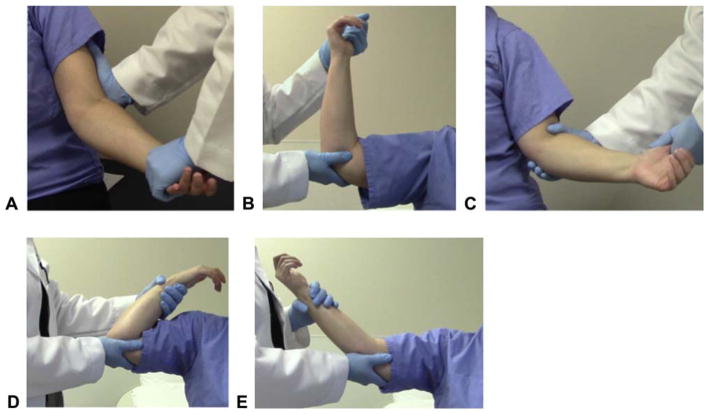
The moving valgus stress test, described by O’Driscoll et al,11 was found to be 100% sensitive and 75% specific for MCL injuries. The test is performed with the patient upright; the shoulder is placed in 90° of abduction and maximal external rotation with the elbow in maximal flexion. A constant valgus force is applied as the elbow is extended to 30° of flexion. A positive test must reproduce pain over the MCL between 70° and 120° of flexion, which is reminiscent of throwing between the late cocking and the early acceleration phases. To confirm the examination findings, the examiner may reverse the movements and flex the elbow while applying valgus force, demonstrating elbow pain in the same range of flexion11 (Fig. 3).
FIGURE 3.
Diagnostic maneuvers for valgus elbow instability. A Valgus stress test. The elbow is flexed to 20°, the forearm is supinated, and a valgus stress is applied across the elbow. A positive test elicits pain over the medial ligaments or widening of the medial joint line. B Milking maneuver. The elbow is flexed to greater than 90° and a valgus stress is applied through the elbow by pulling on the patient’s thumb. C Modified milking maneuver. The arm is adducted and externally rotated, the patient’s elbow is flexed to 70°, and a valgus stress is applied through the thumb. D, E Moving valgus stress test. The patient’s shoulder is abducted and externally rotated while the elbow is ranged from maximal flexion to 30° flexion as a valgus force is applied. A patient with valgus instability will experience medial elbow pain or apprehension in the 70° to 120° flexion range.
Posterolateral rotatory instability
Posterolateral rotatory instability is the most common recurrent instability of the elbow; it occurs secondary to a traumatic or iatrogenic injury to the LCL. Symptoms are due to recurrent posterior radial head subluxation, manifesting as lateral elbow pain or mechanical symptoms when a load is applied while the elbow is in flexion and supination.12
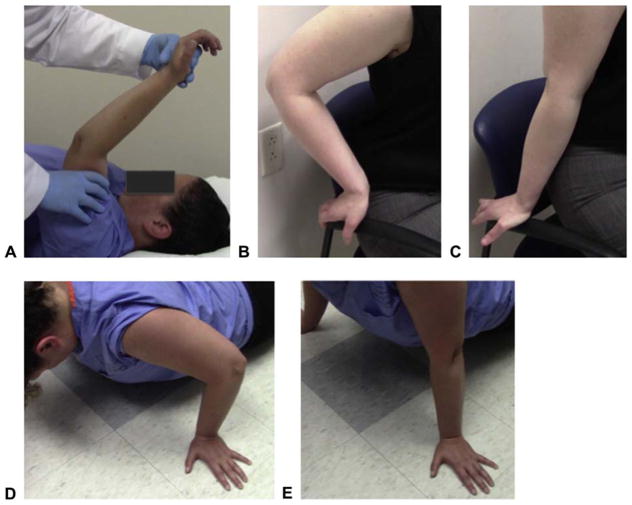
The lateral pivot-shift test, initially described by O’Driscoll in 1991,13 is performed with the patient supine; the arm is elevated over the patient’s head with the shoulder placed in full external rotation and the forearm is supinated. A valgus, supinating, and axial force is applied as the elbow is slowly flexed. At 40° of flexion, the rotatory displacement is maximized and a skin dimple proximal to the radial head can be seen owing to radial head dislocation. With increased flexion, the dimple disappears as the radial head reduces. In an awake patient, the only symptom may be apprehension13 (Fig. 4). In anesthetized patients, the lateral pivot-shift test is 100% sensitive; however, in awake patients, it is 38% sensitive.14
FIGURE 4.
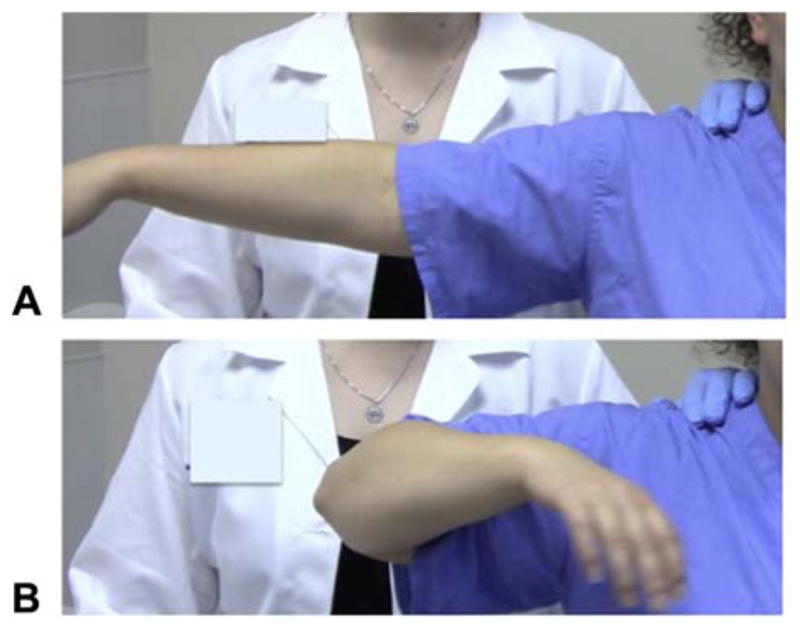
PRLI tests. A Lateral pivot-shift test. The arm is raised above the head of the supine patient, the forearm is supinated, and a valgus and axial force is applied as the elbow is flexed. A “dimple” proximal to the radial head will be seen at 40° of flexion that produces a clunk with increased flexion. B, C. Chair push-up test. In a seated patient, the elbows are flexed to 90° and the forearms supinated. The patient then pushes up on the arms of the chair and extends the elbows. D, E Prone push-up test. The patient assumes a push-up position and supinates the forearm, then pushes up from 90° elbow flexion. A positive test will cause radial head subluxation or pain in a patient with PLRI.
The posterolateral rotatory drawer test is performed in a supine patient with the arm overhead and the forearm in full supination, much like the lateral pivot-shift test. The elbow is placed in 40° flexion and an anteroposterior force is applied to the radius and ulna. The test elicits radial head subluxation in a sedated patient or apprehension in an awake patient.6,12
The lateral pivot-shift test and posterolateral rotatory drawer test provide reliable results in sedated patients. However, several maneuvers are better tolerated in awake patients. The chair push-up test is performed with the patient seated and the elbows abducted away from the body and flexed to 90° with the forearms in supination. The patient places hands on the arms of a chair and pushes up as if to get out of the chair. Elbow extension applies an axial and valgus load to the supinated elbow while the patient rises.14 The prone push-up test is performed by having the patient start in the push-up position, with the elbows flexed to 90° and the forearm in supination. The patient then extends the elbows, in a push-up. These tests cause apprehension or radial head dislocation in patients with PLRI. Regan and Lapner14 reviewed the prone push-up and chair push-up test and demonstrated 87.5% sensitivity in individual test use and 100% sensitivity when both tests are used together (Fig. 4).
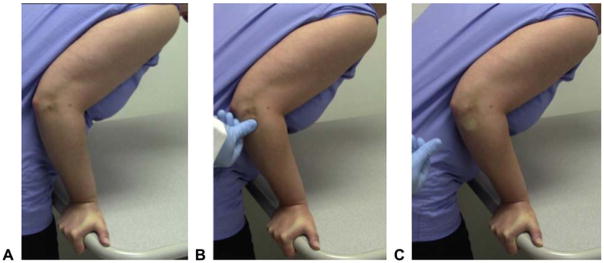
The table-top relocation test has 3 components. The maneuver is started with the forearm in supination and the hand is placed around the edge of a table. Initially, (1) the patient applies an axial load through the elbow while the elbow flexes, causing apprehension at 40° of flexion. (2) The patient repeats the first maneuver while the examiner applies pressure on the radial head, thus preventing subluxation and symptoms. (3) The examiner then removes his or her thumb from the partially flexed elbow, and radial head subluxation reproduces pain. This test is theoretically more specific than the chair push-up and prone push-up test because the relief from apprehension makes intra-articular pathology less likely to be causing symptoms15 (Fig. 5).
FIGURE 5.
Table-top relocation test for PLRI. A First component. The patient’s hand is supinated and grasps the edge of a table, then applies an axial force and flexes the elbow. The patient will have pain or radial head subluxation at approximately 40° of flexion. B Second component. From the starting position, the examiner applies force upon the radial head as the patient flexes the elbow. This prevents radial head subluxation and prevents pain. C Third component. The examiner then removes his or her thumb, which causes recurrence of the patient’s pain.
Varus posteromedial rotatory instability
This instability pattern occurs after an axial and valgus load with the forearm in pronation causes a fracture to the anteromedial facet of the coronoid and a rupture of the LCL.16,17 Immediately after trauma, physical examination maneuvers may not be possible. However, in the subacute setting, the gravity-assisted varus stress test can be used to elicit instability or mechanical symptoms. This test is performed with the arm abducted to 90°; the shoulder is in neutral rotation as the patient flexes and extends the elbow. Owing to the absence of the medial buttress of the LCL and coronoid, the varus stress causes mechanical symptoms by loading the medial ulnohumeral joint.18 Pollock et al19 evaluated multiple simulated examination maneuvers in LCL and anteromedial facet deficient–elbows; and the gravity-assisted varus stress test proved the most sensitive and specific maneuver (Fig. 6).
FIGURE 6.
Gravity-assisted varus stress test for VPMI. A, B The patient’s arm is abducted to 90° in neutral rotation as the elbow is flexed and extended, allowing gravity to apply a varus stress.
TESTING
Radiographs
Routine anteroposterior, lateral, and 2 oblique elbow radiographs should be obtained for all patients to evaluate for underlying osseous abnormalities and associated fractures. Radiographs in valgus instability may demonstrate avulsion fractures of the MCL, or in chronic injuries, ossification of the MCL, loose bodies, or periarticular osteophytes. Elbow axial and oblique axial views, with the elbow in 110° flexion, may demonstrate posteromedial olecranon osteophytes. Valgus stress radiographs may demonstrate increased ulnohumeral gapping compared with the contralateral elbow. Widening greater than 0.5 mm compared with the contralateral elbow may represent a significant MCL injury; however, the findings are inconsistent.9 An arthrogram may demonstrate contrast leakage from the joint or a “T sign” from partial undersurface tearing of the MCL insertion.10
Unstressed radiographs in PLRI may show an avulsion from the lateral epicondyle or widening of the radiocapitellar joint. Radial head subluxation may create impaction fractures to the posterior capitellum. The drop sign, described as an ulnohumeral distance greater than 4 mm on the lateral radiograph, documents sagging of the ulna in the grossly unstable elbow. Stress radiographs obtained while performing the lateral pivot-shift test demonstrate ulnohumeral widening and radial head subluxation.4,20
In varus posteromedial instability (VPMI), imaging studies may demonstrate small lateral epicondyle avulsion fractures and disruptions of the anteromedial coronoid. Varus stress radiographs under anesthesia are the gold standard with widening seen at the ulnohumeral joint.18
Computed tomography
Computed tomography (CT) is used to evaluate bony anatomy and characterize fractures seen after complex elbow fracture-dislocations. The coronoid fracture seen in VPMI is best evaluated with CT, and this assists in preoperative planning.18 In valgus instability, CT arthrograms improve detection of partial thickness MCL tears and are between 71% and 86% sensitive and 91% specific.10 With regard to PLRI, studies have not confirmed the effectiveness of CT imaging, despite the potential ability to characterize joint incongruity in PLRI.21
Magnetic resonance imaging
Magnetic resonance imaging (MRI) is able to characterize the soft tissue structures, including collateral ligaments, and possible osteochondral fragments.22 Magnetic resonance imaging is the test of choice for valgus instability. Nonenhanced MRI is 57% to 79% sensitive and 100% specific for MCL tears, whereas magnetic resonance arthrogram with saline or gadolinium is 97% sensitive and 100% specific.9,23 The AMCL is visualized on coronal T1 images as a thin band of low signal intensity along the medial joint line. Sprains appear as increased signal on T1 and T2 images, whereas complete ruptures demonstrate poor definition, redundancy, or an irregular pattern. Chronic injuries may demonstrate heterotopic calcification or ligamentous ossification.9,22 Associated injuries to the articular cartilage, tearing of the common flexor origin, and inflammation of the ulnar nerve can additionally be evaluated on MRI.9
In PLRI, MRI can be used to characterize ligamentous injury and evaluate the articular damage related to recurrent radial head subluxation. Hackl et al21 demonstrated that posterior translation of the radial head greater than 2 mm and axial ulnohumeral incongruity greater than 1 mm was highly suspicious for PLRI. The LCL complex cannot be easily seen on a single MRI view. The LUCL may visualized by tracing the path from anterior to posterior. Multiple studies have failed to reach a consensus on the effectiveness of MRI in diagnosing LUCL injuries.12,22 Ligamentous edema, tendon thickening, and articular injury or bone bruising to the medial ulnohumeral joint, posterior capitellum, or volar radial head help to support the diagnosis of PLRI.23
Ultrasonography
Ultrasonography (US) can be performed rapidly to evaluate for ligamentous sprains and ruptures. Ligament ruptures demonstrate discontinuity of the hyperechoic ligament with anechoic fluid in the gap. The MCL can be evaluated on a supine patient with the shoulder in abduction and external rotation and the elbow at 90°.24 Dynamic US can demonstrate the medial joint instability when a valgus stress is applied; however, this examination may not be diagnostic owing to expected joint widening in the dominant arm of throwing athletes.9 The LCL complex can be evaluated with the hand in supination as a varus stress is applied; however, there is no consensus about the role of US in evaluation of the LCL.24
The elbow consists of static and dynamic stabilizers that function in synchrony to prevent elbow instability. After injury to any of the primary static stabilizers, the ulnohumeral joint, AMCL, and LCL, joint instability commonly follows. Valgus instability, PRLI, and VPMI have been discussed with reference to the diagnostic maneuvers and imaging studies used to detect these instability patterns.
Supplementary Material
Footnotes
No benefits in any form have been received or will be received related directly or indirectly to the subject of this article.
References
- 1.Hausman MR, Lang P. Examination of the elbow: current concepts. J Hand Surg Am. 2014;39(12):2534–2541. doi: 10.1016/j.jhsa.2014.04.028. [DOI] [PubMed] [Google Scholar]
- 2.Bryce CD, Armstrong AD. Anatomy and biomechanics of the elbow. Orthop Clin North Am. 2008;39(2):141–154. v. doi: 10.1016/j.ocl.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 3.Morrey BF, An KN. Stability of the elbow: osseous constraints. J Shoulder Elbow Surg. 2005;14(1 Suppl S):174S–178S. doi: 10.1016/j.jse.2004.09.031. [DOI] [PubMed] [Google Scholar]
- 4.Ahmed I, Mistry J. The management of acute and chronic elbow instability. Orthop Clin North Am. 2015;46(2):271–280. doi: 10.1016/j.ocl.2014.11.008. [DOI] [PubMed] [Google Scholar]
- 5.Safran MR, Baillargeon D. Soft-tissue stabilizers of the elbow. J Shoulder Elbow Surg. 2005;14(1 Suppl S):179S–185S. doi: 10.1016/j.jse.2004.09.032. [DOI] [PubMed] [Google Scholar]
- 6.O’Driscoll SW, Jupiter JB, King GJ, Hotchkiss RN, Morrey BF. The unstable elbow. Instr Course Lect. 2001;50:89–102. [PubMed] [Google Scholar]
- 7.Closkey RF, Goode JR, Kirschenbaum D, Cody RP. The role of the coronoid process in elbow stability. A biomechanical analysis of axial loading. J Bone Joint Surg Am. 2000;82-A(12):1749–1753. doi: 10.2106/00004623-200012000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Morrey BF, Tanaka S, An KN. Valgus stability of the elbow. A definition of primary and secondary constraints. Clin Orthop Relat Res. 1991;265:187–195. [PubMed] [Google Scholar]
- 9.Hariri S, Safran MR. Ulnar collateral ligament injury in the overhead athlete. Clin Sports Med. 2010;29(4):619–644. doi: 10.1016/j.csm.2010.06.007. [DOI] [PubMed] [Google Scholar]
- 10.Timmerman LA, Schwartz ML, Andrews JR. Preoperative evaluation of the ulnar collateral ligament by magnetic resonance imaging and computed tomography arthrography. Evaluation in 25 baseball players with surgical confirmation. Am J Sports Med. 1994;22(1):26–31. doi: 10.1177/036354659402200105. discussion 32. [DOI] [PubMed] [Google Scholar]
- 11.O’Driscoll SW, Lawton RL, Smith AM. The “moving valgus stress test” for medial collateral ligament tears of the elbow. Am J Sports Med. 2005;33(2):231–239. doi: 10.1177/0363546504267804. [DOI] [PubMed] [Google Scholar]
- 12.Anakwenze OA, Kancherla VK, Iyengar J, Ahmad CS, Levine WN. Posterolateral rotatory instability of the elbow. Am J Sports Med. 2014;42(2):485–491. doi: 10.1177/0363546513494579. [DOI] [PubMed] [Google Scholar]
- 13.O’Driscoll SW, Bell DF, Morrey BF. Posterolateral rotatory instability of the elbow. J Bone Joint Surg Am. 1991;73(3):440–446. [PubMed] [Google Scholar]
- 14.Regan W, Lapner PC. Prospective evaluation of two diagnostic apprehension signs for posterolateral instability of the elbow. J Shoulder Elbow Surg. 2006;15(3):344–346. doi: 10.1016/j.jse.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 15.Arvind CH, Hargreaves DG. Table top relocation test—new clinical test for posterolateral rotatory instability of the elbow. J Shoulder Elbow Surg. 2006;15(4):500–501. doi: 10.1016/j.jse.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 16.Wyrick JD, Dailey SK, Gunzenhaeuser JM, Casstevens EC. Management of complex elbow dislocations: a mechanistic approach. J Am Acad Orthop Surg. 2015;23(5):297–306. doi: 10.5435/JAAOS-D-14-00023. [DOI] [PubMed] [Google Scholar]
- 17.Ebrahimzadeh MH, Amadzadeh-Chabock H, Ring D. Traumatic elbow instability. J Hand Surg Am. 2010;35(7):1220–1225. doi: 10.1016/j.jhsa.2010.05.002. [DOI] [PubMed] [Google Scholar]
- 18.Ramirez MA, Stein JA, Murthi AM. Varus posteromedial instability. Hand Clin. 2015;31(4):557–563. doi: 10.1016/j.hcl.2015.06.005. [DOI] [PubMed] [Google Scholar]
- 19.Pollock JW, Brownhill J, Ferreira L, McDonald CP, Johnson J, King G. The effect of anteromedial facet fractures of the coronoid and lateral collateral ligament injury on elbow stability and kinematics. J Bone Joint Surg Am. 2009;91(6):1448–1458. doi: 10.2106/JBJS.H.00222. [DOI] [PubMed] [Google Scholar]
- 20.Charalambous CP, Stanley JK. Posterolateral rotatory instability of the elbow. J Bone Joint Surg Br. 2008;90(3):272–279. doi: 10.1302/0301-620X.90B3.19868. [DOI] [PubMed] [Google Scholar]
- 21.Hackl M, Wegmann K, Ries C, Leschinger T, Burkhart KJ, Muller LP. Reliability of Magnetic resonance imaging signs of posterolateral rotatory instability of the elbow. J Hand Surg Am. 2015;40(7):1428–1433. doi: 10.1016/j.jhsa.2015.04.029. [DOI] [PubMed] [Google Scholar]
- 22.Binaghi D. MR Imaging of the elbow. Magn Reson Imaging Clin N Am. 2015;23(3):427–440. doi: 10.1016/j.mric.2015.04.005. [DOI] [PubMed] [Google Scholar]
- 23.Saliman JD, Beaulieu CF, McAdams TR. Ligament and tendon injury to the elbow: clinical, surgical, and imaging features. Top Magn Reson Imaging. 2006;17(5):327–336. doi: 10.1097/RMR.0b013e3180421c9e. [DOI] [PubMed] [Google Scholar]
- 24.Tagliafico AS, Bignotti B, Martinoli C. Elbow US: anatomy, variants, and scanning technique. Radiology. 2015;275(3):636–650. doi: 10.1148/radiol.2015141950. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.