Abstract
Three-dimensional (3D) printings are gaining a place in a variety of the medical sectors. With applications in urogenital diseases, 3D printing is a new tool that present difficulties at stages of imaging, planning, and carry out therapeutic interventions. In this review we tried to find answers to the questions that come to mind on this new topic by empasizing the suitable 3D printing models in urology, their clinical usage, and the limitations.
Keywords: Future prospects, three dimensional printing, urology
Introduction
Three dimensional (3D) printing which is also known as a prototyping process has emerged within the last two decades.[1,2] Most commonly plastics but many different materials like gold, titanium, polymers, nylon etc can be also used in 3D printing (Table 1). 3D printing has found an increasing application in all fields of medicine but especially in plastic surgery, orthopedics and dentistry. In urology there is less, but increasing number of articles about this technology have been published within the last few years. In this article, we wish to review the practical medical applications especially in urology hoping that our article will help the readers to understand its contributions into clinical practice.
Table 1.
Materials used in 3D printing
| Type of the material | Advantages | Disadvantages |
|---|---|---|
| Metals (platinum, gold, silver, brass, bronze, steel, aliminum) | Very good solidity and temperature resistance | Poor flexibility |
| Acrylate (plexiglass) | Low shrinkage, successful in detailed figures | Expensive, heat can cause depolymerisation |
| Plastics | Low cost, both solid and flexible, high versality | Amount of waste material carries risk for nature |
| Nylon | Strong, durable | Less printing resolution, harmful emmisions |
| Ceramics | Practical, decorative,food safe | Not ideal for glazing, kilning |
| Sandstone | Cheap | Color shade anavoidable |
First of all, we wish to give an insight to medical 3D tecniques. In order to create 3D models from medical imaging, data must be derived from images. Then for its application concerning the region of interest the data must be evaluated with software version. Finally, data sent can be recognized by the 3D printer software. The schema on how 3D printers work summarizes the basic principles (Figure 1). There are many different techniques of printing. The liquid based 3D technologies (vat photopolymerisation) are the most widely used ones for surgery and were first applied for grafting of a skull more than twenty years ago. These systems consist of a photosensitive mirror, a model-building platform, and a light (laser or traditional light) for coloring. Jetting is a newer 3D printing technology that jets layers of liquid photopolymer as thin as microns to build models and prototypes with extremely complex geometries, ultra thin details, and smooth surfaces. Each photopolymer layer is contacted by ultraviolet light after it is jetted thus rendering the material it rigidity. In material extrusion or powder bed fusion models tiny particles are turned into mass models. The printing types (or some may call them types of 3D printers) are summarized in Table 2. In all fields of medicine a developing software model can only take place by a cheap design progress. Today these computer programmes are cheaper than they were a few few decades ago but it is still difficult to find these programs in many countries. Beside medical imaging printers are used for instrumentation and forming cell cultures. Available 3D printed devices are being used in different fields (eg. as templates of surgical devices prosthesis and implants). There are many ongoing studies aiming to manufacture living organs like kidney, liver, and heart. These printings can be patient- matched so that the individual features such as anatomy of every patients can be gained with maximum specifications.
Figure 1.
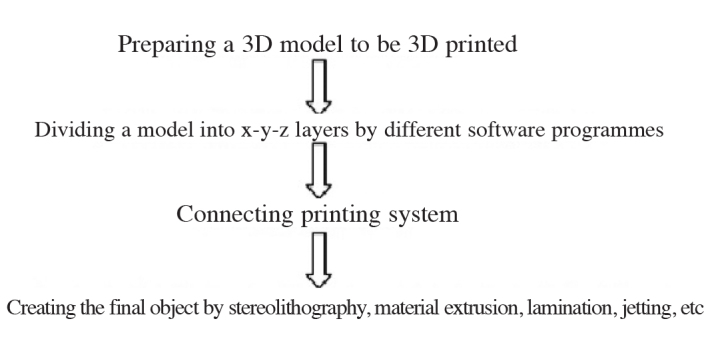
The basic working principles of 3D printers
Table 2.
Some well known types of 3D printing techniques and possible comparable costs
| Fused deposition modeling | Thermoplastic filament is heated and extruded (200–1500$) |
| Stereolithography | Converts liquid plastic into solid 3D objects (3000–6000$) |
| Digital light processing | Only light source is different than SLA (2000–4000$) |
| Selective laser sintering | Uses powdered material instead of liquid resin as SLA does (NA) |
| Selective laser melting | Uses a high-power laser beam that fuses and melts metallic powders (3000–6000$) |
| Electron beam melting | Uses an electron beam instead of laser (NA) |
| Laminated object manufacturing | Adhesive-materials are fused together using heat and pressure and then cut (NA) |
| Binder jetting | The binder is extruded in liquid form from a printhead (300000$) |
| Material jetting | Molten wax is deposited onto an aluminum platform in layers (NA) |
NA: exact price changes between different areas
Clinical and research consequences
In urology 3D printing technique can be used in different sections. One of these is resection planning of genitourinary organs. Today we plan our surgeries depending on two dimentional images. There are many encouraging studies especially in orthopedics, plastic surgery etc. while there are only a few reports in urology yet. With this technology, it is possible for surgeons to produce body parts that need to be removed. For an example, in partial nephrectomy patient’s previous perception of assessment was found to be altered after presentation of the personalized 3D printed model.[2,3] Before a partial nephrectomy, understanding of the treatment strategies like ablation, excision with their specific risks of complications will be very easy with 3D model in front of both the patient and the surgeon. Also just before an organ removing surgeries like penectomy, orchiectomy etc. 3D models will be very useful.
Use of 3D technology in prostate biopsies has been also contemplated. The geometric distribution of the cores on the detection of prostate cancer is important. Today in order to increase the diagnostic accuracy Magnetic Resonance Imaging (MRI) guided biopsies are being used. As an alternative to these biopsies Chang et al.[4] demonstrated the geometric 3D biopsy schema. This technique is another type of prostate screening in three dimensions. In a recent article the low-cost desktop 3D printer manufactured molds using very cheap material with minimal human supervision and prostate geometry was materialized in a few second to produce a very high-resolution model.[5] MR-TRUS fusion biopsies were found to be superior over standard transrectal biopsies.[6] If the softwares will get cheaper, 3D printed prostatic biopsies can take place of MR-guided ones.
Determining detailed and accurate imaging, and planning a surgery with exact knowledge of anatomy is precisely important to gain success in urological surgeries (both open and endourological).[7] Despite many improvements concerning intrarenal access applied in the percutaneus nephrolithotomy (PNL), the rapid and precise establishment of the nephrostomy tract is still difficult. The ultimate goal is complete stone clearance with lower complication rates, and with the growing market of low-cost 3D printers, PNL procedure can be shortened and the complication associated with needle puncture can be decreased in a cost-efficient manner.[8,9] The prompt evaluation of urological organs is mandatory in traumas. As Peng et al. suggested, the enhanced multi -scan CT permits reliable detection of renal trauma and the associated organ or tissue injuries and provide important clinical value for the diagnosis and classification of trauma or internal organ injures, however 3D technology precisely will give guide the surgical decision making process concerning both blunt and penetrating traumas.[10]
Three-dimensional organ-mimicking phantoms provide realistic imaging environments for testing various aspects of optical systems and assessing novel image processing algorithms.[11] Murphy summarized the technological innovations in the field of ureterorenoscopy and concluded that the ongoing developments in virtual 3D imaging, and wireless endoscopy continue to create opportunities to improve the endoscopic urologic procedures.[12]
An interesting study, although with limited number of patients, demonstrated that 3D reconstruction cloacagrams yielded similar results to endoscopic findings. Since these anomalies are complex, their anatomy is hardly revealed under general anestesia, and 3D reconstruction cloacagrams will provide a great advantage before surgical procedures.[13]
The quantitative metrics that are currently used to describe the deformities in Peyronie’s Disease are inadequate and non-standardized. In order to solve this problem penis models simulating deformities were constructed and excellent methodologic reliability was obtained.[14]
3D printing also has a role in moving from 2D cell culture methods into 3D models which enable more accurate investigation of interactions between cells.[15] Thanks to the process of this fabrication the deposits of biological materials will be evolved into new human organs. Beside the need for renal transplantation, increase in aging populations has accelerated the need for replacement different organs of urogenital system. Although it is a fantasy today, in near future different scaffolds will be covered with the patient’s own cells, cultured and the engineered organ can be implanted into the patient.
An issue that has been discussed about the benefits of 3D technology is reduction in the operating time. This technology reduced operation room time in many studies.[16–18] In general, most 3D-printing applications seem to reduce the operation time, but wide variances can be seen between the different usages. Some reductions in operation times are too small to become beneficial. Although operation room time reduction is a major advantage that could contribute to significant financial gain, the increased time needed for surgical planning is rarely considered. But, the increased time needed for surgical planning is rarely considered in those studies so the debate about both the financial gain and shortened management seems to go on.[19] The use of 3-D printing in different areas of urology along with their potential use is summarized in Table 3.
Table 3.
The use of 3-D printing in different areas of urology along with their potential use
| Resection planning of genitourinary organs |
| Prostate biopsies |
| Determining detailed and accurate imaging before surgeries like PNL |
| Operation decision on both blunt and sharp traumas |
| Culture models in order to create organs |
| Tactile anatomical models to medical students, surgical assistants |
Preclinical and research consequences
Anatomical models constructed using 3D technology can be an advantage for medical students. Today medical education depends on anatomy books. Tactile anatomical models can also assist medical and surgical students to improve their knowledge. In Canada in order to improve resident education 3D printed bladder bench models were used and the results have been recently published. The authors concluded these models confer many advantages to anatomy education, surgical manipulations for students from different grades.[20]
Conclusion
Although we screened articles which can be found in the references section, we are aware that some important articles might have been missed. We believe that 3D printing will become an indispensable part of medicine and urology in the future. Today the most important problem seems to be the cost but that depends heavily on the manufacturing facility. However, the reported costs of self-printed parts differ from author to author, and only few authors have indicated direct preparation prices (CT, MRI, number of prints, software, and computer) or the time consumed in designing the model so the exact amount of expenses is very hard to estimate. Medical 3D-printing applications used only for demonstrations and training were not incorporated in this review. Although prototyping individual models and implants are already applied very successfully, most of the materials used for 3D are not yet suitable for implantation in the body.[21] There is likely to be some degree of resistance as with any new technology but this will not impede the adoption of 3D-technology into daily urological practice.
Footnotes
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - A.A.; Design - B.C.Ö.; Supervision - B.C.Ö.; Resources - B.C.Ö., A.A.; Materials - B.C.Ö., A.A.; Data Collection and/or Processing - B.C.Ö., A.A.; Analysis and/or Interpretation - B.C.Ö., A.A.; Literature Search - B.C.Ö.; Writing Manuscript - B.C.Ö.; Critical Review - B.C.Ö., A.A.; Other - B.C.Ö., A.A.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Rohner D, Guijarro-Martinez R, Bucher P, Hammer B. Importance of patient-specific intraoperative guides in complex maxillofacial reconstruction. J Craniomaxillofac Surg. 2013;41:382–90. doi: 10.1016/j.jcms.2012.10.021. https://doi.org/10.1016/j.jcms.2012.10.021. [DOI] [PubMed] [Google Scholar]
- 2.Silberstein JL, Maddox MM, Dorsey P, Feibus A, Thomas R, Lee BR. Physical models of renal malignancies using standard cross-sectional imaging and 3-dimensional printers: a pilot study. Urology. 2014;84:268–72. doi: 10.1016/j.urology.2014.03.042. https://doi.org/10.1016/j.urology.2014.03.042. [DOI] [PubMed] [Google Scholar]
- 3.Bernhard JC, Isotani S, Matsugasumi T, Duddalwar V, Hung AJ, Suer E, et al. Personalized 3D printed model of kidney and tumor anatomy:a useful tool for patient education. World J Urol. 2016;34:337–45. doi: 10.1007/s00345-015-1632-2. https://doi.org/10.1007/s00345-015-1632-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chang D, Chong X, Kim C, Jun C, Petrisor D, Han M, et al. Geometric systematic prostate biopsy. Minim Invasive Ther Allied Technol. 2016;19:1–20. doi: 10.1080/13645706.2016.1249890. [DOI] [PubMed] [Google Scholar]
- 5.Priester A, Natarajan S, Le JD, Garritano J, Radosavcev B, Grundfest W, et al. A system for evaluating magnetic resonance imaging of prostate cancer using patient-specific 3D printed molds. Am J Clin Exp Urol. 2014;2:127–35. [PMC free article] [PubMed] [Google Scholar]
- 6.Cool DW, Romagnoli C, Izawa JI, Chin J, Gardi L, Tessier D, et al. Comparison of prostate MRI-3D transrectal ultrasound fusion biopsy for first-time and repeat biopsy patients with previous atypical small acinar proliferation. Can Urol Assoc J. 2016;10:342–8. doi: 10.5489/cuaj.3831. https://doi.org/10.5489/cuaj.3831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Theisen KM, Kadow BT, Rusilko PJ. Three-Dimensional Imaging of Urethral Stricture Disease and Urethral Pathology for Operative Planning. Curr Urol Rep. 2016;17:54. doi: 10.1007/s11934-016-0616-0. https://doi.org/10.1007/s11934-016-0616-0. [DOI] [PubMed] [Google Scholar]
- 8.Golab A, Smektala T, Krolikowski M, Slojewski M. Percutaneous Nephrolithotomy Using an Individual 3-Dimensionally Printed Surgical Guide. Urol Int. 2016 doi: 10.1159/000446291. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 9.Brehmer M, Beckman MO, Magnusson A. Three-dimensional computed tomography planning improves percutaneous stone surgery. Scand J Urol. 2014;48:316–23. doi: 10.3109/21681805.2013.876552. https://doi.org/10.3109/21681805.2013.876552. [DOI] [PubMed] [Google Scholar]
- 10.Peng N, Wang X, Zhang Z, Fu S, Fan J, Zhang Y. Diagnosis value of multi-slice spiral CT in renal trauma. Xray Sci Technol. 2016;24:649–55. doi: 10.3233/XST-160585. https://doi.org/10.3233/XST-160585. [DOI] [PubMed] [Google Scholar]
- 11.Smith GT, Lurie KL, Zlatev DV, Liao JC, Ellerbee Bowden AK. Multimodal 3D cancer-mimicking optical phantom. Biomed Opt Express. 2016;7:648–62. doi: 10.1364/BOE.7.000648. https://doi.org/10.1364/BOE.7.000648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Murphy SV, Atala A. 3D bioprinting of tissues and organs. Nat Biotechnol. 2014;32:773–85. doi: 10.1038/nbt.2958. https://doi.org/10.1038/nbt.2958. [DOI] [PubMed] [Google Scholar]
- 13.Patel MN. Use of rotational fluoroscopy and 3-D reconstruction for pre-operative imaging of complex cloacal malformations. Semin Pediatr Surg. 2016;25:96–101. doi: 10.1053/j.sempedsurg.2015.11.008. https://doi.org/10.1053/j.sempedsurg.2015.11.008. [DOI] [PubMed] [Google Scholar]
- 14.Margolin EJ, Mlynarczyk CM, Mulhall JP, Stember DS, Stahl PJ. Three-Dimensional Photography for Quantitative Assessment of Penile Volume-Loss Deformities in Peyronie’s Disease. J Sex Med. 2017;14:829–33. doi: 10.1016/j.jsxm.2017.03.257. https://doi.org/10.1016/j.jsxm.2017.03.257. [DOI] [PubMed] [Google Scholar]
- 15.Nyga A, Neves J, Stamati K, Loizidou M, Emberton M, Cheema U. The next level of 3D tumour models: immunocompetence. Drug Discov Today. 2016;21:1421–8. doi: 10.1016/j.drudis.2016.04.010. https://doi.org/10.1016/j.drudis.2016.04.010. [DOI] [PubMed] [Google Scholar]
- 16.Pornrattanamaneewong C, Chareancholvanich K, Narkbunnam R. A prospective randomised controlled study of patient-specific cutting guides compared with conventional instrumentation in total knee replacement. J Bone Joint Surg-Series. 2013;95:354–9. doi: 10.1302/0301-620X.95B3.29903. [DOI] [PubMed] [Google Scholar]
- 17.Kassab S, Pietrzak WS. Patient-specific positioning guides versus manual instrumentation for total knee arthroplasty: an intraoperative comparison. J Surg Orthop Adv. 2014;23:140–6. doi: 10.3113/jsoa.2014.0140. https://doi.org/10.3113/JSOA.2014.0140. [DOI] [PubMed] [Google Scholar]
- 18.Di Giacomo GA, Cury PR, de Araujo NS, Sendyk WR, Sendyk CL. Clinical application of stereolithographic surgical guides for implant placement: preliminary results. J Periodontol. 2005;76:503–7. doi: 10.1902/jop.2005.76.4.503. https://doi.org/10.1902/jop.2005.76.4.503. [DOI] [PubMed] [Google Scholar]
- 19.Tack P, Victor J, Gemmel P, Annemans P. 3D-printing techniques in a medical setting: a systematic literature review. Biomed Eng Online. 2016;15:115. doi: 10.1186/s12938-016-0236-4. https://doi.org/10.1186/s12938-016-0236-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wong NC, Hoogenes J, Guo Y, Quantz MA, Matsumoto ED. Techniques: Utility of a 3D printed bladder model for teaching minimally invasive urethrovesical anastomosis. Can Urol Assoc J. 2017;11:321–2. doi: 10.5489/cuaj.4262. https://doi.org/10.5489/cuaj.4262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Heller M, Bauer HK, Goetze E, Gielisch M, Roth KE, Drees P, et al. Applications of patient-specific 3D printing in medicine. Int J Comput Dent. 2016;19:323–39. [PubMed] [Google Scholar]


