Abstract
Background
The well-documented shortages of health care workers (HCWs) in sub-Saharan Africa are further intensified by the increased human resource needs of expanding HIV treatment programs. Burnout is a syndrome of emotional exhaustion (EE), depersonalization (DP), and a sense of low personal accomplishment (PA). HCWs’ burnout can negatively impact the delivery of health services. Our main objective was to examine the prevalence of burnout amongst HCWs in Malawi and explore its relationship to self-reported suboptimal patient care.
Methods
A cross-sectional study among HCWs providing HIV care in 89 facilities, across eight districts in Malawi was conducted. Burnout was measured using the Maslach Burnout Inventory defined as scores in the mid-high range on the EE or DP subscales. Nine questions adapted for this study assessed self-reported suboptimal patient care. Surveys were administered anonymously and included socio-demographic and work-related questions. Validated questionnaires assessed depression and at-risk alcohol use. Chi-square test or two-sample t-test was used to explore associations between variables and self-reported suboptimal patient care. Bivariate analyses identified candidate variables (p < 0.2). Final regression models included variables with significant main effects.
Results
Of 520 HCWs, 62% met criteria for burnout. In the three dimensions of burnout, 55% reported moderate-high EE, 31% moderate-high DP, and 46% low-moderate PA. The majority (89%) reported engaging in suboptimal patient care/attitudes including making mistakes in treatment not due to lack of knowledge/experience (52%), shouting at patients (45%), and not performing diagnostic tests due to a desire to finish quickly (35%). In multivariate analysis, only burnout remained associated with self-reported suboptimal patient care (OR 3.22, [CI 2.11 to 4.90]; p<0.0001).
Conclusion
Burnout was common among HCWs providing HIV care and was associated with self-reported suboptimal patient care practices/attitudes. Research is needed to understand factors that contribute to and protect against burnout and that inform the development of strategies to reduce burnout.
Introduction
The successful scale-up of antiretroviral treatment (ART) has resulted in an impressive increase in the number of individuals initiating treatment since 2000 [1, 2]. Currently, more than 18 million persons, the majority of whom reside in sub-Saharan Africa (SSA), are receiving ART [1, 2]. Unfortunately, the well-documented shortages of health care workers (HCWs) in SSA are further intensified by the increased human resource needs of rapidly expanding HIV-treatment programs [3–8]. Countries in SSA have 68% of the world's burden of illness from AIDS, yet have only 3% of HCWs worldwide [5]. The combination of staffing shortages and increasing numbers of patients can lead to heavy workloads and workforce burnout, which may result in compromised healthcare outcomes [9–11].
Burnout is a syndrome of emotional exhaustion (EE), depersonalization (DP), and a sense of low personal accomplishment (PA) resulting from chronic job-related stress that can lead to decreased quality of care rendered [12]. The prevalence of burnout among HCWs globally ranges from 15–85%, depending on the medical specialty and working conditions [11, 13–16]. Burnout among HCWs has been shown to be associated with physical and mental illness as well as increased absenteeism, decreased job performance, poor patient practices, and medical errors [10, 17, 18].
Malawi is one of the most resource-limited countries in the world, with one of the lowest per capita GNP in the world at $340 USD [19, 20]. It is a land-locked country of 17.2 million, in Southern Africa. The adult HIV prevalence is high at 10.6%, with 900,000 persons living with HIV/AIDS and an average life expectancy of 64 years [21]. The physician-patient ratio is exceptionally low, with one physician per 62,000 patients, compared to the World Health Organization’s (WHO) recommended ratio of one per 5000 persons [11, 22].
In spite of these limitations in economic and human resources for health, Malawi has implemented an impressive scale-up of HIV treatment. Currently, 679,000 persons are receiving ART, a 2.5-fold increase from 2010 [23, 24]. Moreover, Malawi along with much of Southern Africa has recently launched test-and-treat, an ambitious initiative to offer lifelong ART for all HIV-positive persons upon diagnosis [25, 26]. Although it is a welcome initiative, it threatens to place further strain on an already fragile healthcare system [27]. As resource-constrained countries such as Malawi mount this ambitious ART scale-up, they risk launching an impending crisis of burnout among HCWs that will negatively impact the quality of patient care provided and compromise the tremendous gains in ART expansion. There is a dearth of information from sub-Saharan Africa on burnout among HCWs providing HIV care, especially evidence specifically examining the potential relationship between burnout and quality of patient care. We examined the prevalence and degree of burnout among HCWs providing HIV care in Malawi and explored the relationship of burnout to self-reported patient care practices.
Methods
Design
This was a cross-sectional study conducted at 89 public health facilities within 8 districts in the southeastern (districts: Balaka, Machinga, Mangochi, Mulanje, Phalombe, Zomba) and central regions (districts: Lilongwe, Salima) of Malawi from August 2015—January 2016.
Ethical approval
The National Health Sciences Research Committee in Malawi, as well as the Baylor College of Medicine (BCM) IRB in USA, granted ethical approval.
Participants and data collection
We approached a convenience sample of HCWs providing clinical care for HIV-positive patients at 89 health facilities in central and southern Malawi to participate in the study. In Malawi, due to the lack of medical doctors, primarily clinical officers, nurses, and medical assistants, all of whom were eligible to participate in the study, provide medical care. Clinicians from Baylor College of Medicine Children’s Foundation Malawi routinely provide bi-monthly clinical mentorship to HCWs with the Ministry of Health. During these routine teaching visits, BCM clinicians approached HCWs providing HIV care and available on the day of the visit to invite them to participate in the study. Of the 539 HCWs available and approached to participate, 535 (99%) consented and enrolled in the study. The BCM clinicians obtained written consent and gave participants the self-administered written surveys. The paper-based surveys were completed anonymously, and all participants were assured that their names would not be written anywhere on the surveys. The survey included the following measures.
Survey measures
Burnout
Burnout was measured using the 22- question Maslach Burnout Inventory (MBI), which has been widely validated and is considered the gold standard measure for burnout [12]. The inventory has been used throughout the world including among HCWs in several countries in Africa and other types of workers in South Africa [6, 11, 28–33]. Each inventory item is rated on a seven-point Likert scale that measures how frequently the respondent experiences a particular feeling (from 0 for never to 6 for everyday). The MBI measures three constructs of burn out: Emotional Exhaustion (EE), using 9 items to measure physical and emotional depletion; Depersonalization (DP), using 5 items to measure negative or cynical feelings about patients; and Reduced Personal Accomplishment (PA), using 8 items to measure how one perceives one’s own competence. A recent study in Malawi among nurses used the MBI and suggested that it might need modifications to make it more appropriate for use in Malawi (Cronbach alpha scores: 0.67 for EE, 0.42 for DP, and 0.60 for PA) [11]. Informed by this study, we made several modifications to improve clarity and relevance in the Malawi context. The modifications were made with the assistance of Malawian HCWs. The HCWs reviewed the tool and identified questions they found difficult to understand. With study investigators, specific words/statements that were unclear were replaced with clarifying language. For example, for item 1, the term “drained” was replaced with exhausted; item 11 was modified from “I worry that this job is hardening me emotionally" to "I worry that this job is making me emotionally tough"; and item 20 was modified from "I feel like I am at the end of my rope" to "I feel like I can't manage at all anymore." Once changes were made, pretesting was performed among potential participants.
The standardized Cronbach alpha coefficients for the modified MBI were better EE (0.75), DP (0.55), and PA (0.74), as compared to EE (0.67), DP (0.42), and PA (0.60) found in a burnout study previously performed in Malawi [11]. High mean scores on EE and DP scales corresponded to higher degrees of burnout, whereas low scores on the PA subscale corresponded to a high degree of burnout. In line with recent developments in burnout research [9, 17, 34], we chose not to include PA subscales in our overall assessment of burnout, as prior research has suggested this subscale may not belong to burnout syndrome [35, 36].
We defined burnout as scores in the mid-high range on the EE (17–54) or DP (7–30) subscales based on cut-off scores used recently among maternal health staff in Malawi [11]. We also calculated a global burnout score to examine the relationship between burnout as a unified entity and its potential for dose-response relationship with suboptimal patient care. To calculate the global burnout score we used the weighting system developed by Bianchi et al (0.6 emotional exhaustion + 0.4 depersonalization) for their study on burnout [34, 37]. This weighting scheme recognizes the primacy of emotional exhaustion in burnout [38, 39].
Self-reported patient care practices and attitudes
We measured suboptimal patient care practices and attitudes with nine statements adapted from prior research that investigated self-reported patient care amongst health care workers [17, 40]. A group of health care workers providing HIV care in Malawi modified the statements to present HIV-focused patient care practices that are common, relevant and important to provide HIV care. These statements were: (1) I did not welcome the patient politely; (2) I did not fully discuss the treatment plan or answer a patient’s questions; (3) I made mistakes in treatment or medication that were not due to a lack of knowledge/inexperience; (4) I did not perform a diagnostic test because of desire to finish up with the patient quickly; (5) I have sometimes been absent from work when I was not supposed to be; (6) I shouted at a patient; (7) I paid little attention to how much HIV might affect a patient personally or socially; (8) I had little emotional reaction to the death of one of my patients; (9) I felt guilty about how I treated a patient from a humanitarian standpoint.
The questionnaire did not explicitly use the word suboptimal or suggest that these practices/attitudes were undesirable. Participants were asked to rate how frequently (never, few times a year or less, once a month or less, few times a month, weekly, few times a week or every day) they participated in certain behaviors using the prior year as reference. We created a summary measure for self-reported suboptimal patient-care practices defined as one or more suboptimal patient-care practices reported more frequently than monthly to a few times a month, hereafter called suboptimal patient care monthly. This summary outcome measure was used for the univariate and multivariate regression analyses. Because of the similarity of questions related to the DP component of the MBI and suboptimal patient-care attitudes, as in prior studies [17, 40], we excluded suboptimal patient-care attitudes from the summary outcome measure.
Depression and substance abuse
The World Health Organization’s (WHO) self-reporting questionnaire (SRQ) is a widely validated screening tool for depression [41]. It has been validated in Malawi and was used in this study [42]. Based on cut-off scores used in other studies, including those done in Malawi, a cut-off score of 8 was defined as a positive screen for depression. Depression was also evaluated as a continuous variable. We also asked about prior history of depression. The standardized Cronbach’s alpha for the SRQ in our study was an acceptable 0.79, similar to prior work done in Malawi using the SRQ [42] (Cronbach's alpha, 0.85).
The widely validated WHO Alcohol Use Disorders Identification Test (AUDIT) [43] was used to screen for at-risk use of alcohol. A total score is calculated by summing individual item responses across all 10 items. A higher score indicates more problematic use of alcohol. As per AUDIT instructions [43], items 9 and 10 were scored such that “No” = 0; “Yes, but not in the past year” = 2; and “Yes, during the past year” = 4. Based on cut-off scores recommended by WHO and research from studies in Malawi and South Africa, a total score of 8 was considered a positive screen for potentially hazardous or harmful use of alcohol [43–45]. To measure use of other recreational drugs, we asked “How often do you use other drugs (marijuana, etc.),” and the score was adapted from the DUDIT [46].
Demographic, patient and work characteristics
Participants’ self-reported demographics and work characteristics included continuous variables: age, number of children, years since completing training and number of years worked as a HCW; binary variables: gender, HCW cadre and provision of HIV care; and other categorical variables: type of health facility, time spent providing direct clinical care and number of hours worked in a typical week.
Data analysis
Data were summarized by descriptive statistics (mean, SD, median, IQR, frequency). Chi-square test, two-sample t-test, and Fisher’s exact test were used to explore the associations between potential factors and sub-optimal patient care practiced monthly.
Logistic regression models were used to examine the association between burnout and self-reported suboptimal patient care, while controlling for other variables. We performed univariate screening by bivariate analysis. Variables were selected for inclusion in the model selection if their p-value was < 0.20. A backwards selection procedure was applied with a significance level of 0.05. Only variables with a p-value < 0.05 were retained in the final model. The scale for continuous variables was examined using quartiles to ensure a linear assumption was met prior to entry into the logistic model. We used 95% confidence intervals for the estimates.
Missing items on the MBI were imputed using mean substitution for the same subscale and the same participant [37, 47, 48]. We also conducted sensitivity analysis, by analyzing data using subjects with all completed items. All results were very similar. All analyses were performed using SAS software version 9.4 (SAS Institute, Inc., North Carolina, USA).
Results
A total of 535 HCWs enrolled in the study (Table 1). Of these, 15 completed surveys were excluded due to significant missing data. The mean age (SD) was 34 (10.2) years, 59% were female, 58% were married, and 37% were medical officers, clinical officers, or medical assistants. The majority (88%) provided clinical care more than 75% of the time, 36% worked more than 60 hours a week, 7% had a positive depression screen, 5% reported a history of depression, 6% had at risk use of alcohol, and only 4 participants reported using drugs.
Table 1. Characteristics of participants.
N = 520.
| Age, years, mean (SD) | 34 (10.2) |
| Gender, female, n (%) | 305 (59) |
| Marital Status, n (%) | |
| Married | 301 (58) |
| Widowed/divorced | 40 (8) |
| Single | 178 (34) |
| Missing | 1 |
| No of children, median (IQR) | 1 (0–2.0) |
| Missing | 6 |
| Children less than 5 years old | |
| No | 327 (64) |
| Yes | 187 (36) |
| Missing | 6 |
| Type of HCW, n (%) | |
| Medical Officer/Clinical officer/Medical assistant | 190 (37) |
| Nurse midwife technician/state registered nurse | 330 (63) |
| Length of time from completing health care worker training, years, median (IQR) | 6.0 (3.0–10.0) |
| Missing | 2 |
| Years worked as a health care worker, median (IQR) | 5.0 (3.0–10.0) |
| Missing | 1 |
| Provided clinical care to persons living with HIV in the past month, n (%) | 420 (81) |
| Health facility type, n (%) | |
| District Hospital | 134 (26) |
| Rural Hospital | 90 (17) |
| Health center or other | 296 (57) |
| Number of hours worked in a week, n (%) | |
| Less than 40 hours | 35 (7) |
| 40–50 hours | 230 (44) |
| 51–60 hours | 68 (13) |
| More than 60 hours | 184 (36) |
| Missing | 3 |
| Time spent providing direct clinical care, n (%) | |
| All of my time | 249 (48) |
| >75% | 205 (40) |
| 50% | 41 (8) |
| <50% or don’t provide clinical care | 21 (4) |
| Missing | 4 |
| At-risk alcohol use* n (%) | 33 (6) |
| Depression- positive screen#, n (%) | 36 (7) |
| Missing | 1 |
| Suicidal Ideation, n (%) | 20 (4) |
| Missing | 1 |
*As measured by AUDIT (Alcohol Use Disorders Identification Test) score >8
#World Health Organization, Self-Reporting Questionnaire (SRQ), cut off 8
Table 2 summarizes burnout, MBI subscale scores, and self-reported patient care practices and attitudes. For the MBI, 98.3% of participants responded to all items; 9 participants had 1 item missing, 1 participant had 2 items missing, and 1 participant had three items missing. No participants were missing more than 1 item in one subscale. The majority (62%) of HCWs met criteria for burnout. In the three dimensions of burnout, 55% reported moderate-high EE, 31% moderate-high DP, and 46% low-moderate PA. The vast majority of HCWs (89%) reported having at least one suboptimal patient care practice or attitude more than a few times a year or less, 66% reported more than once a month or less, and 41% reported at least weekly. Suboptimal patient care practices were reported by 50% of participants. Self-reported suboptimal care included making mistakes in treatment not due to lack of knowledge/experience (52%), not fully discussing the treatment plan or answering patient questions (52%), shouting at patients (45%), not welcoming the patient politely (43%), not performing diagnostic tests due to a desire to finish up quickly (35%), and absenteeism (24%).
Table 2. Burnout out and self-reported suboptimal patient care practices and attitudes, n = 520.
| Burnout | |
| Mod-high emotional exhaustion (EE) or mod-high depersonalization (DP), n (%) | 321 (62) |
| Mod-high EE or mod-high DP or low-mod PA, n (%) | 405 (78) |
| Global burnout score#, mean (SD) | 13.0 (7.3) |
| Maslach Burnout Index subscales | |
| Moderate to High score for EE, n (%) | 284 (55) |
| Mean (SD), and Median (IQR) | 18.3 (10.3), 18 (10–25) |
| Moderate to High score for DP, n (%) | 161 (31) |
| Mean (SD), and Median (IQR) | 5.0 (5.0), 4 (1–7) |
| Low to Moderate score for PA, n (%) | 237 (46) |
| Mean (SD), and Median (IQR) | 37.6 (9.2), 40 (33–44.5) |
| Self-reported suboptimal patient care/attitudes practiced, n (%) | |
| more than a few times a year or less | 463 (89) |
| more than once a month or less | 342 (66) |
| a few times a month or less | 271 (52) |
| at least weekly | 214 (41) |
| Self-reported suboptimal patient care practiced, n (%) | |
| more than a few times a year or less | 416 (80) |
| more than once a month or less | 259 (50) |
| a few times a month or less | 173 (33) |
| at least weekly | 108 (21) |
| Self-reported suboptimal patient care practiced a few times a year or less n (%) | |
| I did not welcome the patient politely | 222 (43) |
| I did not fully discuss the treatment plan or answer a patient’s questions | 271 (52) |
| I made mistakes in treatment or medication that were not due to a lack of knowledge/inexperience | 268 (52) |
| I did not perform a diagnostic test because of desire to finish up with the patient quickly | 181 (35) |
| I have sometimes been absent from work when I was not supposed to be | 127 (24) |
| I shouted at a patient | 232 (45) |
| Self-reported suboptimal patient care attitudes a few times a year or less n(%) | |
| I paid little attention to how much HIV might affect a patient personally or socially | 158 (30) |
| I had little emotional reaction to the death of one of my patients | 226 (43) |
| I felt guilty about how I treated a patient from a humanitarian standpoint | 363 (70) |
# Global burn out score = [0.6*EE + 0.4*DP]
EE (emotional exhaustion) subscale cut offs: High ≥27, Moderate 17–26. DP (depersonalization) subscale cut offs: High ≥13, Moderate 7–12. PA (personal accomplishment) subscale cut offs: Low ≤31, Moderate 32–38. Moderate to high score for EE was 17–54, moderate to high score for DP was 7 to 30, low to moderate score for PA was 0 to 38.
Table 3 displays results of univariate analyses examining the associations between self-reported suboptimal patient care and other variables. The only variable found to be significantly associated with self-reported suboptimal patient care (p<0.05) was burnout. HCWs who met criteria for burnout were more likely to report suboptimal patient care (42.4% vs. 18.6%, p<0.0001). The EE and DP subscales (p <0.001), but not the PA subscale (p = 0.18), were found to be associated with providing suboptimal patient care.
Table 3. Factors associated with self-reported suboptimal patient care practices- more than once a month–univariate analysis.
| Variable | Suboptimal care No | Suboptimal care Yes | p-value |
|---|---|---|---|
| Age, years, mean (SD) | 33.5 (9.8) | 34.34 (11.0) | 0.38* |
| Gender, n (%) | 0.40 | ||
| Male | 139 (64.7) | 76 (35.3) | |
| Female | 208 (68.2) | 97 (31.8) | |
| Marital Status, n (%) | 0.72 | ||
| Married | 205 (68.1) | 96 (31.9) | |
| Widowed/divorced | 25 (62.5) | 15 (37.5) | |
| Single | 117 (65.7) | 61 (34.3) | |
| No of children, median (IQR) | 1 (0–2) | 1 (0–3) | 0.94* |
| Children less than 5 years old | 0.374 | ||
| No | 213 (65.1) | 114 (34.9) | |
| Yes | 129 (69) | 58 (31) | |
| Type of HCW, n (%) | 0.09 | ||
| Medical Officer/Clinical officer/Medical assistant | 118 (62.1) | 72 (37.9) | |
| Nurse midwife technician/state registered nurse | 229 (69.4) | 101 (30.6) | |
| Length of time from completing health care worker training, years, median (IQR) | 8.5 (9.0) | 9.1 (9.9) | 0.50* |
| Years worked as a health care worker, median (IQR) | 8.7 (8.9) | 9.2 (9.8) | 0.55* |
| Provided clinical care to persons living with HIV in the past month, n (%) | 0.48 | ||
| No | 69 (69.7) | 30 (30.3) | |
| Yes | 277 (66) | 143 (34) | |
| Health facility type, n (%) | 0.07 | ||
| District Hospital | 99 (73.9) | 35 (26.1) | |
| Rural Hospital | 62 (68.9) | 28 (31.1) | |
| Health center or other | 186 (62.8) | 110 (37.2) | |
| Number of hours worked in a week, n (%) | 0.67 | ||
| Less than 40 hours | 24 (68.6) | 11 (31.4) | |
| 40–50 hours | 159 (69.1) | 71 (30.9) | |
| 51–60 hours | 43 (63.2) | 25 (36.8) | |
| More than 60 hours | 18 (64.1) | 66 (35.9) | |
| Time spent providing direct clinical care, n (%) | 0.42 | ||
| All of my time | 172 (69.1) | 77 (30.9) | |
| >75% | 134 (65.4) | 71 (34.6) | |
| 50% | 23 (56.1) | 18 (43.9) | |
| <50% or don’t provide clinical care | 14 (66.7) | 7 (33.3) | |
| At-risk alcohol use* n (%) | 0.06 | ||
| No | 330 (67.8) | 157 (32.2) | |
| Yes | 17 (51.5) | 16 (48.5) | |
| Depression- positive screen#, n (%) | 0.07 | ||
| No | 327 (67.7) | 156 (32.3) | |
| Yes | 19 (52.8) | 17 (47.2) | |
| Suicidal Ideation, n (%) | 0.11 | ||
| No | 337 (67.5) | 162 (32.5) | |
| Yes | 10 (50) | 10 (50) | |
| History of Depression, n (%) | 0.37 | ||
| No | 333 (67.1) | 163 (32.9) | |
| Yes | 14 (58.3) | 10 (41.7) | |
| Burnout: MBI, mod-high EE or mod-high DP | <0.0001 | ||
| No | 162 (81.4) | 37 (18.6) | |
| Yes | 185 (57.6) | 136 (42.4) | |
| Burnout: global score, mean (SD) | 11.47 (6.86) | 16.15 (7.27) | <0.0001* |
Analyses by chi-square test unless otherwise noted.
* Two-sample t-test
Five variables (cadre of HCW, health facility type, burnout, depression- positive screen and at-risk alcohol use) were included in the multivariate logistic regression model. Burnout was the only variable that remained associated with suboptimal patient care (EE+DP, odds ratio [OR] 3.22, [CI 2.11 to 4.90]; p<0.0001). When the EE and DP dimensions were examined separately, they both remained independently associated with suboptimal patient care: (EE, OR 2.03, [CI 1.34 to 3.06]; p = 0.0008) and (DP, OR 3.20, [CI 2.12 to 4.82]; p<0.0001).
To determine if a dose-response relationship existed between burnout and suboptimal patient care practices monthly, we used the global burnout score. With each unit increase in the global burnout score, there was a 1.10-fold change in the odds of providing suboptimal patient care monthly (OR 1.10, [CI 1.07 to 1.13]; p<0.0001).
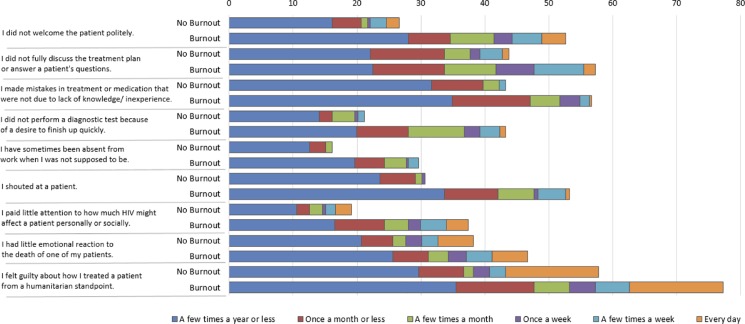
Fig 1 illustrates a comparison of self-reported rates of various suboptimal patient care practices and attitudes between HCWs who met criteria for burnout versus those who did not. The top bar represents HCWs who did not meet criteria for burnout. The bottom bar represents HCWs who met criteria for burnout. More HCWs who met criteria for burnout self-reported each of the nine suboptimal patient care practices/attitudes.
Fig 1. Relationship of burnout (moderate/high EE or moderate/high DP) to self-reported suboptimal patient care practices and attitudes.
Discussion
To our knowledge, this is one of the largest published studies of HCW burnout in SSA and among the first to report a relationship between HCW burnout and patient care. Burnout was commonly experienced among the HCWs in our study: more than 60% met criteria for burnout. A disconcertingly high proportion of HCWs, almost 90%, self-reported engaging in suboptimal patient care practices or attitudes, 66% reported doing it monthly and 41% weekly. HCWs who were burned out were more likely to report providing suboptimal patient care monthly. Although we are unable to determine causality due to time-varying confounding, we observed that burnout was associated with a 3.2 times increased odds of reporting a suboptimal patient care practice. Each one-point increase in global burnout score was associated with a 10% higher likelihood of reporting suboptimal patient care.
Burnout is defined as when HCWs feel emotionally exhausted, cynical and detached, and ineffective and when they feel “an erosion in values, dignity, spirit, and will” [49, 50]. HCWs are the backbone of an optimally functioning health system, so when HCWs are not well, the performance of the health care system suffers [49, 50].
Unfortunately, HCWs in SSA often work under burnout-inducing conditions: long hours, high and increasing burden of responsibility, low perceived control, unsupportive environments, staffing shortages, and the crushing weight of high rates of patient morbidity and mortality [51–53]. Nonetheless, there has been a dearth of research on and attention given to HCW burnout in sub Saharan Africa (SSA).
In comparison, research on burnout in developed countries is well established, and the field has now largely moved towards examining potential interventions. In a recent comprehensive meta-analysis on burnout prevention and treatment interventions [54] only three of 52 studies included were done in low-income countries.
Why has burnout in SSA received comparatively little attention? In the West, when burnout was seen as a crisis of well being among privileged physicians, it elicited little public sympathy. However, as mounting evidence began to suggest that burnout negatively affects physicians’ effectiveness and patient safety, health planners and the public became justifiably worried about the impact of burnout on the quality of patient care [50]. Perhaps similarly in SSA, set against the backdrop of pressing and unmet patient needs, HCW burnout, when viewed as affecting only the HCWs themselves, has not been deemed a priority. More evidence regarding how significant the problem of burnout might be, as well as how burnout might negatively affect health services output in SSA, may help health planners acknowledge human limitations when layering increasing demands on HCWs [50].
More than half of the participating HCWs met criteria for burnout, with 55% reporting moderate-high EE, 31% moderate-high DP, and 46% low-moderate PA. These findings were similar to those found in other studies among HCWs in Malawi (66% moderate-high EE, DP moderate-high 69%) [55], two studies in Zambia (in one study, 51% were defined as burned out [3], and in the other study 62% felt moderate-to-high EE) [6], a study amongst nurses in Nigeria [28] (39% reported moderate-to-high EE), voluntary medical male circumcision providers (Kenya (66%), South Africa (33%), Zimbabwe (17%), and Tanzania (15%) reported starting to experience work fatigue/burnout) [56]. MBI cut-off points can vary by country based on socio-cultural reasons [57], and, therefore, comparisons should be interpreted with this limitation in mind. However, the rates of burnout are similar to those found in other studies among HCWs in the region, and the high proportion of HCWs meeting burnout criteria is concerning.
An alarming majority of HCWs, almost 90%, self-reported suboptimal patient care practices and attitudes; 80% reported suboptimal patient care practices, with 50% reporting it monthly. Suboptimal patient care practices included admitting mistakes in treatment not due to lack of knowledge/experience (52%), shouting at patients (45%), not performing diagnostic tests due to a desire to finish quickly (35%), and absenteeism (24%). Provider-patient relationships have been shown repeatedly to impact patient outcomes. Disrespectful treatment can lead to patients not engaging in or abandoning treatment, whereas healthy relationships can enhance HIV care [58–65]. Despite this evidence, as well as the significant investment in the improvement of health systems in SSA, there is a surprising dearth of evidence regarding the quality of HCW patient care practices in SSA, and these results highlight the urgent need for additional examination.
We found that burnout was the only variable that remained associated with suboptimal patient care. HCWs who met criteria for burnout had a 3.2 times increased odds of reporting a suboptimal patient care event. Each one-point increase in a global burnout score was associated with a 10% higher likelihood of reporting a suboptimal patient-care event. Our findings are consistent with preliminary research on burnout from resource-limited settings that have shown that HCW burnout is associated with negative effects on health care delivery [10, 17, 40]. Further, it is possible that the reports from SSA on the increasing challenges with HCWs’ absenteeism [66], negative treatment of patients, and high turnover [67], may result in part from HCWs’ burnout. We hope that our observation regarding the relationship between burnout and self-reported suboptimal boosts enthusiasm for additional research and action.
This study has several limitations. We used a convenience sample of HCWs who were available during routine program visits. The definition and reporting of suboptimal patient care were based on self-report. However, other studies have also used self-report as a measure of suboptimal patient care [17, 40, 68]. Due to time-varying confounding we cannot determine the causal direction of the association found between burnout and suboptimal patient care. In addition, there are likely unmeasured confounders. For example, certain personality disorders (cynicism, narcissism, high negativity-personality) may have influenced individuals’ perceptions of patient-care practices and could be examined in future work. We did measure and adjust for several important potential confounders such as depression, alcohol use, and work hours. However, the current study cannot account for more complex mechanisms such as time-varying confounding. Despite these limitations, to our knowledge, there are no published studies from SSA that examine the relationship between burnout and patient care, and, therefore, our findings help address a clear gap.
Strengths of the study include a large sample size both in terms of the number of HCWs who participated and the number of representative healthcare facilities (>89 facilities). The response rate was very good, and the surveys were conducted anonymously to reduce social-desirability bias. Another strength is that in line with recent developments describing that PA likely does not fall under burnout syndrome, we excluded PA in our burnout criteria. Finally, this study was conducted in Malawi, where the HCW workforce is already strained and expectations are increasing with the test and treat all approach and integration of outpatient treatment for non-communicable diseases [27, 69].
The HCWs who participated in this study, like many HCWs throughout SSA, not only provide HIV care but are the critical backbone of health care systems, functioning as the frontline providers for most outpatient health services. They are very likely the same HCWs who are tasked to attend to the increasing patient load from the test-and-treat approach and will be called upon to address the rising need to address care of non-communicable diseases in developing countries. Even before the inauguration of the ambitious test-and-treat approach, research on ART scale-up highlighted the importance of limiting burnout and attrition to achieve a program’s maximum efficiency [70]. Now, through the great success of ART scale-up, we are faced with clear concerns around long-term retention of patients on ART, which is where HCWs’ attitudes may have the greatest influence. The additional strain on an under-resourced healthcare system may exacerbate the already significant levels of burnout.
Burnout among HCWs providing HIV care is a critical and impending challenge that requires urgent attention to prevent compromising treatment gains. Additional research is needed to better characterize burnout in SSA, understand its relationship to patient outcomes, and inform the development of strategies to reduce burnout.
Supporting information
(PDF)
Acknowledgments
We thank the Malawi Ministry of Health for their partnership in this endeavor. We thank the Baylor College of Medicine Children’s Foundation Malawi research team who participated in data collection. We are grateful to all the health care workers who participated in this study.
Disclaimer
The contents are the responsibility of the authors and do not necessarily reflect the views of the funders, including the National Institutes of Health, USAID and the United States Government.
Data Availability
The consent forms associated with this study did not include explicit language allowing for data collected to be made publically available. The National Health Sciences Research Committee in Malawi and The Baylor College of Medicine IRB Data granted approvals. Data requests may be sent to the data manager at Baylor Children’s Foundation Malawi, Joseph Mhango, at jmhango@baylor-malawi.org.
Funding Statement
This study was made possible by support from the USAID cooperative agreement number 674-A-00-10-00093-00. MHK was supported by the Fogarty International Center of the National Institutes of Health under award number K01 TW009644. Data analysis was provided by the Design and Analysis Core of the Baylor-UT Houston Center for AIDS Research, a NIH funded program numbered P30-AI36211. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.HIV/AIDS Data and Statistics [http://www.who.int/hiv/data/en/]
- 2.UNAIDS: Global AIDS Update 2016. In. Geneva, Switzerland: Joint United Nations Programme on HIV/AIDS; 2016. [Google Scholar]
- 3.Kruse GR, Chapula BT, Ikeda S, Nkhoma M, Quiterio N, Pankratz D, et al. Burnout and use of HIV services among health care workers in Lusaka District, Zambia: a cross-sectional study. Hum Resour Health 2009, 7(1):2303–2310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen L, Evans T, Anand S, Boufford JI, Brown H, Chowdhury M, et al. Human resources for health: overcoming the crisis. The Lancet 2004, 364(9449):1984–1990. [DOI] [PubMed] [Google Scholar]
- 5.Maddison AR, Schlech WF. Will universal access to antiretroviral therapy ever be possible? The health care worker challenge. Can J Infect Dis Med Microbiol 2010, 21(1):e64–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dieleman M, Biemba G, Mphuka S, Sichinga-Sichali K, Sissolak D, van der Kwaak A, et al. ‘We are also dying like any other people, we are also people’: perceptions of the impact of HIV/AIDS on health workers in two districts in Zambia. Health Policy Plan 2007, 22(3):139–148. doi: 10.1093/heapol/czm006 [DOI] [PubMed] [Google Scholar]
- 7.Katende D, Mutungi G, Baisley K, Biraro S, Ikoona E, Peck R,et al. Readiness of Ugandan health services for the management of outpatients with chronic diseases. Trop Med Int Health 2015, 20(10):1385–1395. doi: 10.1111/tmi.12560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dutta A, Barker C, Kallarakal A. The HIV treatment gap: estimates of the financial resources needed versus available for scale-up of antiretroviral therapy in 97 countries from 2015 to 2020. PLoS Med 2015, 12(11):e1001907 doi: 10.1371/journal.pmed.1001907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schaufeli WB, Leiter MP, Maslach C. Burnout: 35 years of research and practice. Career Dev Int 2009, 14(3):204–220. [Google Scholar]
- 10.Shanafelt TD, Balch CM, Bechamps G, Russell T, Dyrbye L, Satele D, et al. Burnout and medical errors among American surgeons. Ann Surg 2010, 251(6):995–1000. doi: 10.1097/SLA.0b013e3181bfdab3 [DOI] [PubMed] [Google Scholar]
- 11.Thorsen VC, Tharp ALT, Meguid T. High rates of burnout among maternal health staff at a referral hospital in Malawi: A cross-sectional study. BMC Nursing 2011, 10(1):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maslach C, Jackson SE, Leiter MP. Maslach burnout inventory. Evaluating stress: A book of resources 1997, 3:191–218. [Google Scholar]
- 13.Carod-Artal FJ, Vázquez-Cabrera C. Burnout syndrome in an international setting In: Burnout for experts. edn.: Springer; 2013: 15–35. [Google Scholar]
- 14.Felton J. Burnout as a clinical entity—its importance in health care workers. Occup Med 1998, 48(4):237–250. [DOI] [PubMed] [Google Scholar]
- 15.Embriaco N, Papazian L, Kentish-Barnes N, Pochard F, Azoulay E. Burnout syndrome among critical care healthcare workers. Curr Opin Crit Care 2007, 13(5):482–488. doi: 10.1097/MCC.0b013e3282efd28a [DOI] [PubMed] [Google Scholar]
- 16.Poncet MC, Toullic P, Papazian L, Kentish-Barnes N, Timsit J-F, Pochard F, et al. Burnout syndrome in critical care nursing staff. Am J Respir Crit Care Med 2007, 175(7):698–704. doi: 10.1164/rccm.200606-806OC [DOI] [PubMed] [Google Scholar]
- 17.Shanafelt TD, Bradley KA, Wipf JE, Back AL. Burnout and self-reported patient care in an internal medicine residency program. Ann Internal Med 2002, 136(5):358–367. [DOI] [PubMed] [Google Scholar]
- 18.West MA, Guthrie JP, Dawson JF, Borrill CS, Carter M. Reducing patient mortality in hospitals: the role of human resource management. J Organ Behav 2006, 27(7):983–1002. [Google Scholar]
- 19.UNDP: Human Development Report 2016. Human Development for Everyone. In. New York: United Nations Development Programme; 2016. [Google Scholar]
- 20.The World Bank. World Bank online data. http://data.worldbank.org/indicator.
- 21.MPHIA. Malawi Population-Based HIV Impact Assessment: MPHIA 2015–2016. In. New York: Malawi Population-Based HIV Impact Assessment; 2016. [Google Scholar]
- 22.Palmer D. Tackling Malawi's human resources crisis. Reprod Health Matters 2006, 14(27):27–39. doi: 10.1016/S0968-8080(06)27244-6 [DOI] [PubMed] [Google Scholar]
- 23.MOH: Malawi HIV Program Data 2017 Q1. In. Lilongwe, Malawi; 2017.
- 24.Data Sheet—Coverage of people receiving ART [http://aidsinfo.unaids.org/#]
- 25.MOH. Clinical Management of HIV in Children and Adults, 3rd edn. Lilongwe, Malawi: Malawi Ministry of Health; 2016. [Google Scholar]
- 26.WHO. Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV In. Geneva, Switzerland: World Health Organization; 2015: 78. [PubMed] [Google Scholar]
- 27.Kalua T, Barr BAT, van Oosterhout JJ, Mbori-Ngacha D, Schouten EJ, Gupta S, et al. Lessons learned from option B+ in the evolution toward “test and start” from Malawi, Cameroon, and the United Republic of Tanzania. J Acquir Immune Defic Syndr 2017, 75:S43–S50. doi: 10.1097/QAI.0000000000001326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lasebikan VO, Oyetunde MO. Burnout among Nurses in a Nigerian General Hospital: Prevalence and Associated Factors. ISRN Nurs 2012, 2012(1):402157–402156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Olley BO. A comparative study of burnout syndrome among health professionals in a Nigerian teaching hospital. Afr J Med Med Sci 2003, 32(3):297–302. [PubMed] [Google Scholar]
- 30.Essenko N, Rothmann S. Job characteristics, optimism, burnout, and ill health of support staff in a higher education institution in South Africa. S Afr J Psychol 2007, 37(1):135–152. [Google Scholar]
- 31.Pienaar J, Van Wyk D. Teacher burnout: construct equivalence and the role of union membership. S Afr J Educ 2006, 26(4):541–551. [Google Scholar]
- 32.Jordaan I, Spangenberg J, Watson M, Fouché P. Burnout and its correlates in South African clinical and counselling psychologists. Acta Academica 2007, 39(1):176–201. [Google Scholar]
- 33.Khamisa N, Oldenburg B, Peltzer K, Ilic D. Work related stress, burnout, job satisfaction and general health of nurses. Int J Environ Res Public Health 2015, 12(1):652–666. doi: 10.3390/ijerph120100652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bianchi R, Schonfeld IS, Laurent E. Is burnout a depressive disorder? A reexamination with special focus on atypical depression. Int J Stress Manag 2014, 21(4):307–324. [Google Scholar]
- 35.Hakanen JJ, Schaufeli WB. Do burnout and work engagement predict depressive symptoms and life satisfaction? A three-wave seven-year prospective study. J Affect Disord 2012, 141(2):415–424. [DOI] [PubMed] [Google Scholar]
- 36.Schaufeli WB, Taris TW. The conceptualization and measurement of burnout: Common ground and worlds apart. Work Stress 2005, 19(3):256–262. [Google Scholar]
- 37.Ahola K, Honkonen T, Isometsä E, Kalimo R, Nykyri E, Aromaa A, et al. The relationship between job-related burnout and depressive disorders—results from the Finnish Health 2000 Study. J Affect Disord 2005, 88(1):55–62. doi: 10.1016/j.jad.2005.06.004 [DOI] [PubMed] [Google Scholar]
- 38.Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol 2001, 52(1):397–422. [DOI] [PubMed] [Google Scholar]
- 39.Enzmann D, Schaufeli WB, Janssen P, Rozeman A: Dimensionality and validity of the Burnout Measure. J Occup Organ Psychol 1998, 71(4):331–351. [Google Scholar]
- 40.Lu DW, Dresden S, McCloskey C, Branzetti J, Gisondi MA. Impact of Burnout on self-reported patient care among emergency physicians. West J Emerg Med 2015, 16(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Beusenberg M, Orley JH: A User's guide to the self reporting questionnaire (SRQ). Geneva: World Health Organization; 1994. [Google Scholar]
- 42.Stewart RC, Kauye F, Umar E, Vokhiwa M, Bunn J, Fitzgerald M, et al. Validation of a Chichewa version of the self-reporting questionnaire (SRQ) as a brief screening measure for maternal depressive disorder in Malawi, Africa. J Affect Disord 2009, 112(1):126–134. [DOI] [PubMed] [Google Scholar]
- 43.Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The alcohol use disorders identification test: guidelines for use in primary health care; 2001. [Google Scholar]
- 44.Peltzer K, Davids A, Njuho P. Alcohol use and problem drinking in South Africa: findings from a national population-based survey. Afr J Psychiatry 2011, 14(1). [DOI] [PubMed] [Google Scholar]
- 45.Zverev Y. Problem drinking among university students in Malawi. Coll Antropol 2008, 32(1):27–31. [PubMed] [Google Scholar]
- 46.Berman A, Bergman H, Palmstierna T, Schlyter F. The Drug Use Disorders Identification Test (DUDIT) Manual. Stockholm, Sweden: Karolinska Institutet; 2003. [Google Scholar]
- 47.Marcelino G, Cerveira JM, Carvalho I, Costa JA, Lopes M, Calado NE, et al. Burnout levels among Portuguese family doctors: a nationwide survey. BMJ Open 2012, 2(3):e001050 doi: 10.1136/bmjopen-2012-001050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Smith HK. Testing work characteristics as mediating factors in the relationships among nurse leadership, burnout, and engagement. 2012. [Google Scholar]
- 49.Maslach C, Leiter MP. The truth about burnout: How organizations cause stress and what to do about it. San Francisco: Jossey-Bass; 1997. [Google Scholar]
- 50.Epstein RM, Privitera MR. Doing something about physician burnout. The Lancet 2016, 388(10057):2216. [DOI] [PubMed] [Google Scholar]
- 51.Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med 2014, 12(6):573–576. doi: 10.1370/afm.1713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sikka R, Morath JM, Leape L. The Quadruple Aim: care, health, cost and meaning in work. BMJ Qual Saf 2015. [DOI] [PubMed] [Google Scholar]
- 53.Anyangwe SC, Mtonga C. Inequities in the global health workforce: the greatest impediment to health in sub-Saharan Africa. Int J Environ Res Public Health 2007, 4(2):93–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. The Lancet 2016, 388(10057):2272–2281. [DOI] [PubMed] [Google Scholar]
- 55.McAuliffe E, Bowie C, Manafa O, Maseko F, MacLachlan M, Hevey D, et al. Measuring and managing the work environment of the mid-level provider–the neglected human resource. Hum Resour Health 2009, 7(1):13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Perry L, Rech D, Mavhu W, Frade S, Machaku MD, Onyango M, et al. Work experience, job-fulfillment and burnout among VMMC providers in Kenya, South Africa, Tanzania and Zimbabwe. PLoS One 2014, 9(5):e84215 doi: 10.1371/journal.pone.0084215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Schaufeli WB, Van Dierendonck D. A cautionary note about the cross-national and clinical validity of cut-off points for the Maslach Burnout Inventory. Psychol Rep 1995, 76(3 suppl):1083–1090. [DOI] [PubMed] [Google Scholar]
- 58.Kebaabetswe P. Barriers to participation in the prevention of mother-to-child HIV transmission program in Gaborone, Botswana a qualitative approach. AIDS Care 2007, 19(3):355–360. doi: 10.1080/09540120600942407 [DOI] [PubMed] [Google Scholar]
- 59.Aspeling HE, Van Wyk NC. Factors associated with adherence to antiretroviral therapy for the treatment of HIV‐infected women attending an urban care facility. Int J Nurs Pract 2008, 14(1):3–10. doi: 10.1111/j.1440-172X.2007.00659.x [DOI] [PubMed] [Google Scholar]
- 60.Painter TM, Diaby KL, Matia DM, Lin LS, Sibailly TS, Kouassi MK, et al. Women's reasons for not participating in follow up visits before starting short course antiretroviral prophylaxis for prevention of mother to child transmission of HIV: qualitative interview study. BMJ 2004, 329(7465):543 doi: 10.1136/bmj.329.7465.543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bakken S, Holzemer WL, Brown M-A, Powell-Cope GM, Turner JG, Inouye J, et al. Relationships between perception of engagement with health care provider and demographic characteristics, health status, and adherence to therapeutic regimen in persons with HIV/AIDS. AIDS Patient Care STDS 2000, 14(4):189–197. doi: 10.1089/108729100317795 [DOI] [PubMed] [Google Scholar]
- 62.Ingersoll KS, Heckman CJ. Patient–clinician relationships and treatment system effects on HIV medication adherence. AIDS Behav 2005, 9(1):89–101. doi: 10.1007/s10461-005-1684-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Molassiotis A, Morris K, Trueman I. The importance of the patient–clinician relationship in adherence to antiretroviral medication. Int J Nurs Pract 2007, 13(6):370–376. doi: 10.1111/j.1440-172X.2007.00652.x [DOI] [PubMed] [Google Scholar]
- 64.Schneider J, Kaplan SH, Greenfield S, Li W, Wilson IB. Better physician‐patient relationships are associated with higher reported adherence to antiretroviral therapy in patients with HIV infection. J Gen Intern Med 2004, 19(11):1096–1103. doi: 10.1111/j.1525-1497.2004.30418.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Beach MC, Keruly J, Moore RD. Is the Quality of the Patient‐Provider Relationship Associated with Better Adherence and Health Outcomes for Patients with HIV? J Gen Intern Med 2006, 21(6):661–665. doi: 10.1111/j.1525-1497.2006.00399.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mudaly P, Nkosi Z. Factors influencing nurse absenteeism in a general hospital in Durban, South Africa. J Nurs Manag 2015, 23(5):623–631. doi: 10.1111/jonm.12189 [DOI] [PubMed] [Google Scholar]
- 67.Bonenberger M, Aikins M, Akweongo P, Wyss K. The effects of health worker motivation and job satisfaction on turnover intention in Ghana: a cross-sectional study. Hum Resour Health 2014, 12(1):43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Salyers MP, Fukui S, Rollins AL, Firmin R, Gearhart T, Noll JP, et al. Burnout and self-reported quality of care in community mental health. Admin Policy Ment Health and Ment Health Serv Res 2015, 42(1):61–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lupafya PC, Mwagomba BLM, Hosig K, Maseko LM, Chimbali H. Implementation of Policies and Strategies for Control of Noncommunicable Diseases in Malawi Challenges and Opportunities. Health Educ Behav 2016, 43(1 suppl):64S–69S. [DOI] [PubMed] [Google Scholar]
- 70.Wagner G, Ryan G, Taylor S. Formative evaluation of antiretroviral therapy scale-up efficiency in sub-Saharan Africa. AIDS Patient Care STDS 2007, 21(11):871–888. doi: 10.1089/apc.2007.0008 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
Data Availability Statement
The consent forms associated with this study did not include explicit language allowing for data collected to be made publically available. The National Health Sciences Research Committee in Malawi and The Baylor College of Medicine IRB Data granted approvals. Data requests may be sent to the data manager at Baylor Children’s Foundation Malawi, Joseph Mhango, at jmhango@baylor-malawi.org.