Abstract
INTRODUCTION
Few studies to date have explored patient and caregiver views on the clinical use of amyloid PET.
METHODS
A 7-item questionnaire assessing patient and caregiver views (510 total respondents) toward amyloid PET imaging was advertised broadly through alz.org/trialmatch.
RESULTS
We received 510 unique responses from 48 US states, two Canadian provinces, the Dominican Republic, and Greece. Both patients and caregivers indicated that they would want to receive amyloid imaging if offered the opportunity. Over 88% of respondents had a positive response (approximately 10% with neutral and 2% with negative responses) to whether amyloid PET should be offered routinely and be reimbursed. Such information was felt to be useful for long-term legal, financial and healthcare planning. Respondents identifying with early age cognitive decline (<65 years) were more likely to explore options for disability insurance (p = 0.03). Responders from the Midwest were more likely to utilize information from amyloid imaging for legal planning (p = 0.02), disability insurance (p = 0.02), and life insurance (p = 0.04) than other US regions.
DISCUSSION
Patients and caregivers supported the use of amyloid PET imaging in clinical practice and felt that the information would provide significant benefits particularly in terms of future planning.
Keywords: Amyloid, positron emission tomography (PET), clinical use, Alzheimer’s disease (AD), patient, caregiver
1. Introduction
Alzheimer’s disease (AD) is the most common age-related neurodegenerative disease in the world. In the United States, approximately 5.5 million individuals have the disease and it is the sixth leading cause of death in the country. AD places a significant burden not only on persons affected by the disease, but also their families, with more than 15 million caregivers providing an estimated 18.2 billion hours of care in the year 2016.1 The burden faced by caregivers is not only due to time sacrificed and the challenges of a progressive disease, but also financial in nature and due to personal suffering.
Clinical diagnosis of AD is achieved by establishing the presence of progressive cognitive decline, while ruling out other causes of cognitive and functional impairment.2,3 The “gold standard” for definitive diagnosis of AD, however, is through discovering AD pathology during postmortem neuropathological examination using widely accepted criteria.4,5 Recent studies have assessed the accuracy of clinical diagnosis in comparison with neuropathology at autopsy, demonstrating sensitivity of 70.9%–87.3% and specificity of 44.3% –70.8%.6 Thus, while clinical data is often used to deduce underlying AD pathology, clinical diagnosis is not robustly accurate.
Current studies suggest that AD initially begins in a presympomatic phase with abnormal processing of β-amyloid (Aβ) peptide, leading to accumulation of amyloid plaques in the brain. This is followed by neuronal injury and degeneration, a tau-mediated process, accompanied by synaptic dysfunction, leading to eventual cognitive symptoms and the syndrome of dementia.7 This model for AD pathophysiology has led to the consensus that biomarker evidence for brain amyloid deposition would enhance specificity in the diagnosis of AD.2
In recent years, there have been many biomarker developments to assist in the diagnosis of AD. Of these, some of the most significant are positron emission tomography (PET) imaging ligands with strong affinity for Aβ plaques, allowing for in vivo visualization of AD pathology. Three amyloid PET ligands, F18-Florbetapir, F18-Florbetaben, and F18-Flutemetamol, have recently achieved U.S. Food and Drug Administration (FDA) approval in the United States.8–14 Diagnostic performance for these compounds was presented in the results of phase 3 trials demonstrating a median sensitivity of 92% and specificity of 95% for F18-Florbetapir 10, a median sensitivity of 88% and specificity of 92% for F18-Florbetaben 9, and a median sensitivity of 98% and specificity of 85% for F18-Flutemetamol.14 A recent meta-analysis of F18-Florbetapir and F18-Florbetaben showed similar sensitivities and slightly lower specificities compared to those published in the phase 3 trials.15 It is important to reiterate that the sensitivity and specificity values from the phase 3 trials are for the detection of amyloid plaques compared to autopsy tissues – not for the diagnosis of AD. Two other meta-analyses recently determined that amyloid imaging has 95% sensitivity and 57% specificity for predicting conversion from mild cognitive impairment to AD16 and suggested that amyloid PET might be particularly useful in the diagnostic work-up of early-onset dementia.17 While these results suggest benefit in specific clinical circumstances, amyloid PET is not currently part of routine clinical care in the United States and recommendations for which patient populations would benefit the most from amyloid PET are being developed. Appropriate use criteria have been proposed for persons with persistent or unexplained mild cognitive impairment, for those with atypical AD presentation or with suspected mixed etiology, and for those with progressive dementia with atypical early age of onset.18
In 2013, the United States Centers for Medicare & Medicaid Services (CMS) released a statement that there is insufficient evidence that amyloid PET imaging improves patient outcomes and declined to provide reimbursement.19 However, CMS did opt to provide coverage with evidence development (CED), meaning that the procedure is only covered in the context of an approved clinical study.19 This mechanism allows investigation into the utility of amyloid PET for diagnostically challenging clinical scenarios and to assist with clinical trials for treatment and prevention of AD. To date, several small single-center studies have suggested that amyloid imaging can affect diagnostic and treatment decisions.20–26 A large, multi-center CMS funded study to examine the diagnostic and therapeutic benefits of amyloid imaging, its cost effectiveness, and its impact on patient outcomes is presently ongoing (http://www.ideas-study.org/).
While many studies have evaluated the diagnostic or prognostic implications associated with amyloid PET, few have explored its effects on the patient or caregiver. Not only may amyloid imaging help clinicians with their diagnosis and management, but it may also affect patient and caregiver decisions related to lifestyle and financial planning, long-term care, and employment.18 Diagnostic uncertainty can lead to anxiety and depression among patients, which have been associated with negative quality of life outcomes for both patients and caregivers.27 Receiving a diagnosis of AD and disease education has been shown to decrease such anxiety in patients28 and to have positive effects on caregiver burden and depression.21,29 A few recent studies have qualitatively explored patient and caregiver views toward AD and mild cognitive impairment.28,30–32 So far, these studies have been small and none have directly explored patient and caregiver views toward amyloid PET imaging. A single small study involving 28 patients and 23 caregivers, which explored the impact of amyloid PET on patients and caregivers, demonstrated that caregivers appreciated the results of imaging and had an impact on their future plans.21 Here, we report the largest sample analysis of patient and caregiver views toward amyloid PET imaging and its potential use in routine clinical practice.
2. Methods
2.1 Study Design
Our dataset consisted of 510 participants who answered 7 questions provided through an online questionnaire designed to obtain the thoughts and feelings of patients and caregivers. The questionnaire can be seen in Figure 1. The vast majority of these participants (N=487) were invited through the Alzheimer’s Association TrialMatch mailing list, while others were directed to the questionnaire by the Indiana Alzheimer Disease Center website (N=8), the 2015 FTD Caregiver Conference (N=5), a family member (N=3), or an unknown source (N=7). Participants were informed that they are eligible for the study only if they or the person they provide care for had memory loss or dementia.
Figure 1.
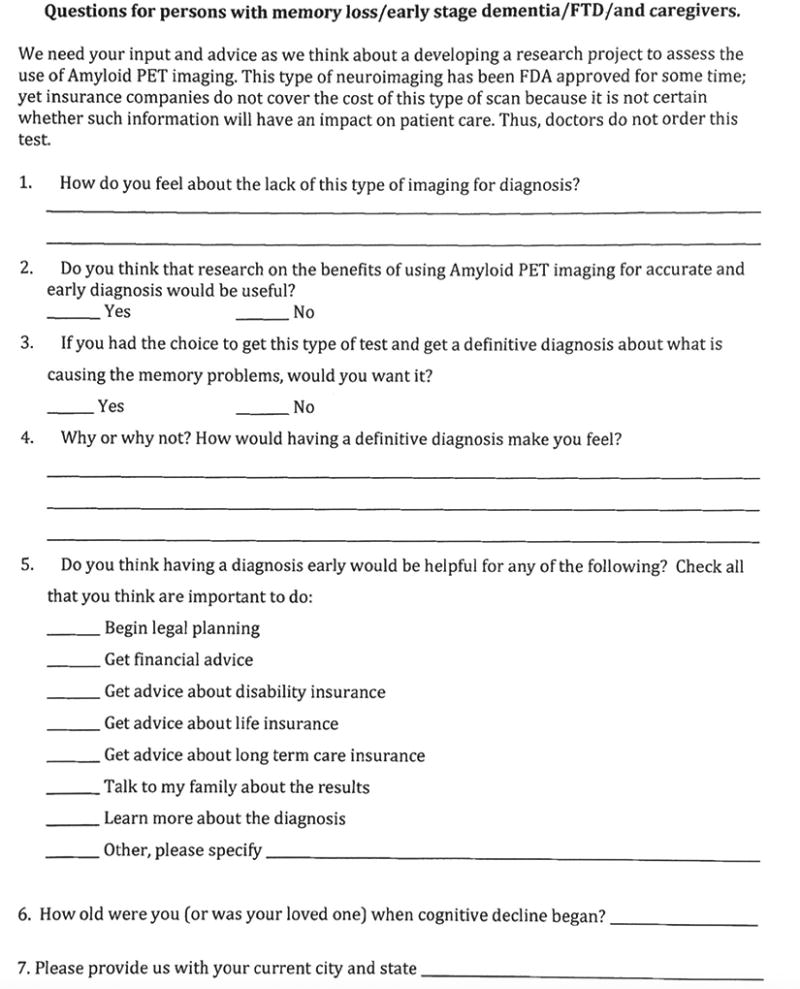
Amyloid PET questionnaire
All participants were given a brief introduction about amyloid PET with an explanation that this type of imaging is currently FDA approved, yet does not have insurance coverage, and is not part of routine clinical care (see Figure 1). Participants were given a one page questionnaire asking open-ended questions of their feelings about the lack of amyloid PET imaging in routine clinical diagnosis, whether they believed additional research on amyloid PET would be beneficial, and whether they would choose to pursue amyloid PET if offered the opportunity (Figure 1). Additionally, participants were able to report whether they thought receiving a diagnosis early on through amyloid imaging would be beneficial for legal planning, financial advice, disability insurance, life insurance, long-term care insurance, communicating with family members, learning more about their diagnosis, or “other” scenarios. Finally, participants were asked to report how old they or the person they care for were when cognitive decline began and to provide their current city and state. Additional demographic information was not acquired in order to maintain confidentiality and anonymity (see Figure 1).
2.2 Data Analyses
Answers to the questionnaire were recorded verbatim. We reviewed each participant’s responses fully, then categorized the data for analyses. The question “How do you feel about the lack of amyloid PET imaging for diagnosis?” elicited a variety of responses, which were categorized as follows: 1) positive responses - responses stating amyloid imaging would be beneficial in patient care such as “If the PET scan is an effective tool…, then it should be covered by insurance and available to those effected by memory loss and other symptoms.”; 2) emotionally charged positive responses – positive responses containing the words “alarming”, “appalling”, “angry”, “cheated”, “criminal” or “it's a crime”, “disappointing”, “discouraged”, “disheartened”, “feel bad”, “feel sorry”, “frustrated”, “hate”, “indignant”, “not happy”, “outraged”, “petrified”, “pitiful”, “sad”, “scary”, “terrible”, “travesty”, “unfortunate”, “upset”; 3) neutral responses - responses that were neither positive nor negative as in “I don't know enough about it to have an opinion.”; and 4) negative responses - responses that were not supportive of this type of imaging such as “I understand why insurance doesn't feel it would be helpful”. Questions about participants’ beliefs on whether further research into amyloid imaging would be beneficial, whether participants would choose to pursue amyloid imaging if offered the opportunity, and whether receiving an early diagnosis would be beneficial for the various scenarios were not further categorized.
While we did not specifically ask whether the respondent was a patient or a caregiver, 63.3% of the respondents provided that information in their answers (i.e., “I was 54 when my doctor broke the news…” vs. “my mother was diagnosed with Alzheimer’s…”). This allowed for the dichotomization of patient vs. caregiver status in 323 of our 510 cases.
Responses were also divided by self-reported age of onset of cognitive decline as early-onset (less than age 65) or late-onset (65 and older).
Geographically we divided responses as coming from urban vs. rural area based on the U.S. Department of Health and Human Services, 2013 National Center for Health Statistics Urban-Rural Classification Scheme33,34 and by U.S. regions (i.e., Northeast, Midwest, South, and West) based on the U.S. Census Bureau region classification.35
2.3 Statistical Methods
We used Pearson’s chi-squared tests to compare response data between 1) patients and caregivers, 2) early onset and late onset cases, 3) urban and rural residents, and 4) US geographic regions. When analyzing data by U.S. regions, in order to determine which particular regions were driving the statistical significance in various scenarios, standardized Pearson residuals were determined.36 All statistical analyses were done with IBM SPSS Statistics 24. Analyses of the study responses among the different groups were performed on the data that could be assigned to the specific divisions, leaving unknown data out of the analysis.
3. Results
3.1 Sample Characteristics
Our dataset consisted of 510 total participants. The responses were categorized as 87 (17.1%) patients and 236 (46.2%) caregivers. We were unable to assign 187 (36.7%) of the responses to a participant category due to missing information. Based on age when cognitive decline began, 215 (42.2%) were categorized as early-onset and 270 (52.9%) were categorized as late-onset. Twenty-five (4.9%) were unassigned as these participants did not provide an answer for the age on onset. Geographically, 446 (87.4%) of responses were from urban areas while 59 (11.6%) of responses were from rural areas. Divided by U.S. region, the responses were categorized as 83 (16.2%) Northeast, 114 (22.4%) Midwest, 182 (35.7%) South, and 119 (23.3%) West. Five (1.0%) participants did not provide their current city and state, and so these responses were not assigned to the urban vs. rural division of responses. An additional seven participants were from locations in Canada, Greece, and the Dominican Republic and so a total of 12 (2.4%) of responses were unassigned when dividing responses by U.S. regions. Forty-eight U.S. states (not included: Rhode Island and Wyoming), two Canadian provinces (British Columbia and Ontario), and cities in the Dominican Republic (Santiago) and Greece (Athens) were represented among the responses provided.
Additional analysis of the data showed that there were significantly more patients vs. caregivers among early-onset (44.2% patients vs. 55.8% caregivers) than late-onset cognitive decline (12.6% patients vs. 87.4% caregivers), p <0.0001. There were no significant differences between the number of patients vs. caregivers or early-onset vs. late-onset participants when analyzed by urban vs. rural or U.S. regional distributions.
3.2 Questionnaire Results
Table 1 details the overall responses obtained from participants (N=510) who answered the questionnaire. Of the responses regarding the lack of amyloid PET imaging in routine clinical diagnosis, 325 (63.7%) of the responses were categorized as positive (in favor of amyloid imaging), 125 (24.5%) as positive and emotionally charged, 51 (10.0%) as neutral, and 9 (1.8%) as negative.
Table 1.
Response frequencies in the pooled sample (% represents positive responses unless otherwise noted)
| N (%) | |
|---|---|
| TOTAL RESPONSES | 510 (100) |
| REACTION TO THE UNAVAILABILITY OF AMYLOID IMAGING IN THE CLINIC: | |
| POSITIVE (IN FAVOR OF AMYLOID IMAGING) | 325 (63.7) |
| POSITIVE (EMOTIONALLY CHARGED) | 125 (24.5) |
| NEUTRAL | 51 (10.0) |
| NEGATIVE (NOT IN FAVOR OF AMYLOID IMAGING) | 9 (1.8) |
| ADDITIONAL RESEARCH WILL BE BENEFICIAL | 507 (99.4) |
| WILLINGNESS TO SUBJECT ONESELF TO AMYLOID IMAGING IF OFFERED | 508 (99.6) |
| BENEFITS OF EARLY DEFINITIVE DIAGNOSIS: | |
| LEGAL PLANNING | 446 (87.5) |
| FINANCIAL ADVICE | 392 (76.9) |
| DISABILITY INSURANCE | 306 (60.0) |
| LIFE INSURANCE | 250 (49.0) |
| LONG-TERM CARE INSURANCE | 345 (67.6) |
| COMMUNICATING WITH FAMILY | 467 (91.6) |
| LEARNING MORE ABOUT DIAGNOSIS | 474 (92.9) |
| OTHER | 123 (24.1) |
When participants were asked whether they believed additional research on amyloid PET would be beneficial, 507 (99.4%) responded yes. A large number of responders, 508 (99.6%), also stated they would choose to pursue amyloid PET if offered the opportunity. The majority cited the benefit of having definitive diagnosis as the reason for pursuing amyloid imaging. Interestingly, all 9 responders who felt the absence of insurance coverage for amyloid PET is justifiable stated that they would pursue an amyloid PET scan if recommended by their doctor.
Early diagnosis obtained through amyloid imaging was thought to be beneficial for legal planning by 446 (87.5%), for financial advice by 392 (76.9%), for disability insurance by 306 (60.0%), for life insurance by 250 (49.0%), for long-term care insurance by 345 (67.6%), for communicating with family members by 467 (91.6%), for learning more about their diagnosis by 474 (92.9%), and for “other” scenarios by 123 (24.1%) participants. 76 of the 123 “other” responses simply restated one or more of the options that were already listed. 46 were new items. Another 12 subjects made comments in this field that listed other benefits without checking the box “other”. The additional benefits among these 58 new responses consisted of eligibility for participation in clinical trials (26%), starting early treatment (21%), focusing on “enjoying life” (17%), adjusting/adapting to diagnosis (12%), participation in support groups (7%), decreased anxiety and stress (5%), engaging in spiritual pursuits (3%), increasing one’s awareness of his/her cognitive problems (3%), participation in brain donation program (2%), modifying home to meet one’s needs (2%) and aggressively addressing any other health issues (2%). Additional 16 participants voiced concerns with amyloid PET affecting their ability to sign up for long-term care and life insurance.
Table 2–5 describe the distribution of responses in our subgroup analyses. No significant differences were present among patients vs. caregivers, early-onset vs. late-onset cognitive decline, urban vs. rural locations, or among U.S. regions regarding their reaction to the unavailability of amyloid imaging in clinic (Table 2), their perceived need for additional research on amyloid PET (Table 3) and their willingness to subject themselves to amyloid imaging if recommended by their doctor (Table 4). There were no significant differences between patients vs. caregivers or urban vs. rural subgroups in terms of their intent to pursue more information about the disease, legal and financial planning, to explore their options for disability, long-term care and life insurance, and to communicate their diagnosis and prognosis with their families (Table 5). Those with early-onset cognitive decline were more likely to utilize information from amyloid imaging to explore their options for disability insurance than those with late-onset cognitive decline (66.0% early-onset vs. 54.8% late-onset, p = 0.03), however both groups did not differ in terms of the other long-term planning scenarios (Table 5).
Table 2.
Reaction to lack of reimbursement for amyloid imaging in the clinic (% represents positive responses unless otherwise noted)
| PATIENTS AND CAREGIVERS: | |||
|---|---|---|---|
| % of Patients (n=87) |
% of Caregivers (n=236) |
P-value | |
| POSITIVE (IN FAVOR OF AMYLOID IMAGING) | 57.5 | 63.1 | 0.58 |
| POSITIVE (EMOTIONALLY CHARGED) | 33.3 | 25.8 | |
| NEUTRAL | 8.0 | 8.9 | |
| NEGATIVE (NOT IN FAVOR OF AMYLOID IMAGING) | 1.1 | 2.1 | |
| EARLY-ONSET AND LATE-ONSET: | |||
| % of Early-onset (n=215) | % of Late-onset (n=270) | P-value | |
| POSITIVE (IN FAVOR OF AMYLOID IMAGING) | 62.8 | 62.2 | 0.14 |
| POSITIVE (EMOTIONALLY CHARGED) | 28.4 | 23.0 | |
| NEUTRAL | 7.0 | 13.0 | |
| NEGATIVE (NOT IN FAVOR OF AMYLOID IMAGING) | 1.9 | 1.9 | |
| URBAN AND RURAL: | |||
| % of Urban (n=446) | % of Rural (n=59) | P-value | |
| POSITIVE (IN FAVOR OF AMYLOID IMAGING) | 63.5 | 64.4 | 0.41 |
| POSITIVE (EMOTIONALLY CHARGED) | 25.6 | 18.6 | |
| NEUTRAL | 9.4 | 13.6 | |
| NEGATIVE (NOT IN FAVOR OF AMYLOID IMAGING) | 1.6 | 3.4 | |
| U.S. REGIONS: | |||||
|---|---|---|---|---|---|
| % of Northeast (n=83) |
% of Midwest (n=114) |
% of South (n=182) |
% of West (n=119) |
P-value | |
| POSITIVE (IN FAVOR OF AMYLOID IMAGING) | 63.9 | 66.7 | 63.2 | 63.0 | 0.95 |
| POSITIVE (EMOTIONALLY CHARGED) | 22.9 | 23.7 | 25.8 | 23.5 | |
| NEUTRAL | 12.0 | 7.9 | 8.8 | 12.6 | |
| NEGATIVE (NOT IN FAVOR OF AMYLOID IMAGING) | 1.2 | 1.8 | 2.2 | 0.8 | |
Table 5.
Benefits of early definitive diagnosis (% represents positive responses)
| PATIENTS AND CAREGIVERS: | |||
|---|---|---|---|
| % of Patients (n=87) |
% of Caregivers (n=236) |
P-value | |
| LEGAL PLANNING | 85.1 | 89.0 | 0.56 |
| FINANCIAL ADVICE | 75.9 | 80.5 | 0.86 |
| DISABILITY INSURANCE | 64.4 | 62.3 | 0.45 |
| LIFE INSURANCE | 50.6 | 50.8 | 0.77 |
| LONG-TERM CARE INSURANCE | 70.1 | 69.9 | 0.5 |
| COMMUNICATING WITH FAMILY | 96.6 | 90.3 | 0.16 |
| LEARNING MORE ABOUT DIAGNOSIS | 95.4 | 91.9 | 0.33 |
| OTHER | 31.0 | 28.0 | 0.52 |
| EARLY-ONSET AND LATE-ONSET: | |||
| % of Early-onset (n=215) | % of Late-onset (n=270) | P-value | |
| LEGAL PLANNING | 87.0 | 87.8 | 0.61 |
| FINANCIAL ADVICE | 76.7 | 77.0 | 0.96 |
| DISABILITY INSURANCE | 66.0 | 54.8 | 0.03 |
| LIFE INSURANCE | 54.4 | 44.1 | 0.06 |
| LONG-TERM CARE INSURANCE | 70.7 | 64.8 | 0.31 |
| COMMUNICATING WITH FAMILY | 89.8 | 92.6 | 0.16 |
| LEARNING MORE ABOUT DIAGNOSIS | 93.5 | 92.6 | 0.59 |
| OTHER | 26.5 | 22.2 | 0.24 |
| URBAN AND RURAL: | |||
| % of Urban (n=446) | % of Rural (n=59) | P-value | |
| LEGAL PLANNING | 87.2 | 88.1 | 0.45 |
| FINANCIAL ADVICE | 77.6 | 69.5 | 0.09 |
| DISABILITY INSURANCE | 60.5 | 55.9 | 0.65 |
| LIFE INSURANCE | 49.8 | 42.4 | 0.38 |
| LONG-TERM CARE INSURANCE | 67.9 | 64.4 | 0.5 |
| COMMUNICATING WITH FAMILY | 91.7 | 89.8 | 0.62 |
| LEARNING MORE ABOUT DIAGNOSIS | 92.6 | 94.9 | 0.75 |
| OTHER | 24.0 | 23.7 | 0.84 |
| U.S. REGIONS: | |||||
|---|---|---|---|---|---|
| % of Northeast (n=83) |
% of Midwest (n=114) |
% of South (n=182) |
% of West (n=119) |
P-value | |
| LEGAL PLANNING | 88.0 | 93.0 | 86.3 | 84.0 | 0.02 |
| FINANCIAL ADVICE | 81.9 | 81.6 | 74.2 | 72.3 | 0.08 |
| DISABILITY INSURANCE | 67.5 | 67.5 | 55.5 | 54.6 | 0.02 |
| LIFE INSURANCE | 48.2 | 60.5 | 46.2 | 42.9 | 0.04 |
| LONG-TERM CARE INSURANCE | 71.1 | 72.8 | 67.6 | 60.5 | 0.32 |
| COMMUNICATING WITH FAMILY | 96.4 | 93.0 | 89.6 | 89.1 | 0.22 |
| LEARNING MORE ABOUT DIAGNOSIS | 92.8 | 94.7 | 92.9 | 90.8 | 0.58 |
| OTHER | 26.5 | 19.3 | 22.5 | 28.6 | 0.27 |
table 3.
Beliefs on the need of additional research (% represents positive responses)
| PATIENTS AND CAREGIVERS: | |||
|---|---|---|---|
| % of Patients (n=87) |
% of Caregivers (n=236) |
P-value | |
| ADDITIONAL RESEARCH WILL BE BENEFICIAL | 97.7 | 99.6 | 0.12 |
| EARLY-ONSET AND LATE-ONSET: | |||
| % of Early-onset (n=215) | % of Late-onset (n=270) | P-value | |
| ADDITIONAL RESEARCH WILL BE BENEFICIAL | 99.1 | 99.6 | 0.44 |
| URBAN AND RURAL: | |||
| % of Urban (n=446) | % of Rural (n=59) | P-value | |
| ADDITIONAL RESEARCH WILL BE BENEFICIAL | 99.3 | 100.0 | 0.53 |
| U.S. REGIONS: | |||||
|---|---|---|---|---|---|
| % of Northeast (n=83) |
% of Midwest (n=114) |
% of South (n=182) |
% of West (n=119) |
P-value | |
| ADDITIONAL RESEARCH WILL BE BENEFICIAL | 100.0 | 99.1 | 98.9 | 100.0 | 0.55 |
Table 4.
Willingness to subject oneself to amyloid imaging if recommended by one’s doctor (% represents positive responses)
| PATIENTS AND CAREGIVERS: | |||
|---|---|---|---|
| % of Patients (n=87) |
% of Caregivers (n=236) |
P-value | |
| WILLINGNESS TO SUBJECT ONESELF TO AMYLOID IMAGING IF OFFERED | 100.0 | 99.6 | 0.54 |
| EARLY-ONSET AND LATE-ONSET: | |||
| % of Early-onset (n=215) | % of Late-onset (n=270) | P-value | |
| WILLINGNESS TO SUBJECT ONESELF TO AMYLOID IMAGING IF OFFERED | 100.0 | 99.3 | 0.21 |
| URBAN AND RURAL: | |||
| % of Urban (n=446) | % of Rural (n=59) | P-value | |
| WILLINGNESS TO SUBJECT ONESELF TO AMYLOID IMAGING IF OFFERED | 99.6 | 100.0 | 0.61 |
| U.S. REGIONS: | |||||
|---|---|---|---|---|---|
| % of Northeast (n=83) |
% of Midwest (n=114) |
% of South (n=182) |
% of West (n=119) |
P-value | |
| WILLINGNESS TO SUBJECT ONESELF TO AMYLOID IMAGING IF OFFERED | 98.8 | 100.0 | 99.5 | 100.0 | 0.50 |
Among the data divided by U.S. region, significant differences were found among participants in utilizing information from amyloid imaging for legal planning (88.0% Northeast vs. 93.0% Midwest vs. 86.3% South vs. 84.0% West, p=0.02), for disability insurance (67.5% Northeast vs. 67.5% Midwest vs. 55.5% South vs. 54.6% West, p=0.02), and for life insurance (48.2% Northeast vs. 60.5% Midwest vs. 46.2% South vs. 42.9% West, p=0.04) (Table 5). In all of these scenarios, respondents from the Midwest showed a significant positive trend indicating a greater likelihood for pursuing these actions in comparison to the other three regions (legal planning – 93.0% of Midwest, std Pearson residual = 2.8; disability insurance – 67.5% of Midwest, std Pearson residual = 2.0; life insurance – 60.5% of Midwest, std Pearson residual = 2.8). No differences were found between U.S. regions in terms of the other long-term planning scenarios (Table 5).
4. Discussion
Our data suggest that most patients and caregivers believe amyloid imaging would be beneficial in patient care. The majority of participants had positive responses for the use of amyloid imaging in clinical practice, with many reflecting strong emotional feelings such as frustration, anger, and disappointment for the lack of amyloid imaging in routine clinical practice in the absence of insurance coverage. Few participants had neutral feelings about the lack of imaging often stating they needed more information to give a thoughtful answer. Even fewer participants were comfortable with the current unavailability of amyloid PET in the clinic, frequently explaining that without any disease-modifying therapies available for AD, amyloid imaging may have no therapeutic benefit.
Nearly all participants believed additional research into amyloid PET imaging would be beneficial and would pursue amyloid imaging if recommended by their doctor, with most responders citing the benefit of having a definitive diagnosis as their reason for pursuing the test. Surprisingly, of those participants who had neutral feelings about the lack of amyloid imaging (N=51, 10.0%), 49/51 (96.1%) stated they would pursue amyloid imaging if given the opportunity. The two subjects who said that at this time they will opt out from amyloid imaging cited lack of treatment as the reason behind refusing to subject themselves to this diagnostic imaging modality. All participants who were comfortable with the lack of coverage of amyloid PET at this time (N=9, 1.8%) nonetheless stated they would pursue amyloid imaging if offered.
Receiving amyloid PET results was believed to be most beneficial for learning more about the diagnosis, communicating with family, and legal planning followed by financial planning, purchasing long-term care, disability, and life insurance, and other reasons such as finding support groups, establishing home care, and participating in clinical trials. Interestingly, no significant differences were found in responses from patients vs. caregivers or from urban vs. rural responders. However, significantly more responders with early-onset cognitive decline were likely to use information from amyloid imaging to explore options for disability insurance than responders with late-onset cognitive decline. The likely explanation for this is that younger patients and their caregivers are more likely to be still involved with their careers or are not yet eligible for Medicare or as financially established as some of their older counterparts.
In terms of U.S. regional differences, we found that significantly more responders from the Midwest would utilize information from amyloid imaging for legal planning, disability and life insurance than the other regions, particularly the South and the West. The U.S. Census Bureau reports that the rate of educational attainment (High School or greater education) is highest in the Midwest, followed by the Northeast, West, and then the South.37 In regards to health insurance coverage, the U.S. Census Bureau also reports that the uninsured rate is lowest in the Northeast and Midwest, followed by the West, and then the South.38 It is possible that these trends serve as an explanation for why participants from the Midwest were more likely to use information from amyloid imaging for the various life planning scenarios compared with other regions.
We observed significantly more patients vs. caregivers among those with early-onset than among those with late-onset cognitive decline. There could be several reasons for this imbalance. It is possible that persons with early-onset cognitive decline have greater emotional connection with their disease given the timing of onset and are thus more inclined to participate in studies such as ours. Among those with late-onset cognitive decline, perhaps the caregivers, heavily burdened by financial and time-intensive sacrifices, are more emotionally involved and thus more inclined to participate. It is also possible that the older patients are simply less inclined to use a computer and be digitally subscribed to TrialMatch compared with their younger counterparts. Regardless, it is important to note that were no significant differences in the responses between patients and caregivers from the early-onset vs. the late-onset groups.
Several strengths and limitations of our study are worth discussion. Patients and caregivers were invited to participate only if they or the ones they provide care for were affected by memory loss or dementia. No further participation restrictions were used and no objective verification of a diagnosis of cognitive decline was made. Thus, responses from participants not affected by dementia and more specifically AD may have been included and could have impacted our results. In our questionnaire, the only demographic questions asked were related to current location and age of onset for cognitive decline. While we limited demographic information to lessen the burden of taking part in the study and to also maintain confidentiality and anonymity, additional participants’ characteristics such as age, sex, race, education level, socioeconomic status and patient/caregiver status may have been helpful to further understand participants’ views on amyloid imaging. We do not know how the omission of these questions may have affected trends among different groups. Additional limitations may include the pre-survey information and phrasing of the questions, which may bias towards a positive response to amyloid imaging; and response bias from those who are more in favor of the technique being more likely to respond to the survey questions.
AD has a significant impact among both patients and caregivers. Clinical diagnosis of AD shows moderate accuracy, even among experts in the field. Amyloid PET imaging has demonstrated significant promise for improving diagnostic accuracy. While the value of amyloid PET toward improving patient outcomes remains debated, ongoing research studies will likely influence payers’ coverage decisions related to this imaging modality as well as its incorporation into clinical care in the United States. It will be important to not only consider the impact of amyloid PET on diagnosis, treatment, and patient outcomes, but also on how it harmonizes with the values of patients and caregivers themselves. Our data suggest that patients and caregivers feel that amyloid PET imaging would be beneficial in clinical practice and that additional research into amyloid imaging would be useful. They would also tend to pursue amyloid imaging if presented the opportunity and believe that diagnosis assisted by such imaging would be useful for various long-term planning scenarios ranging from legal planning to participation in clinical trials. Factors such as geography, education, and health insurance coverage may also play a role with decisions for future planning. Further studies will be needed to thoroughly assess the value of amyloid imaging in the lives of patients and caregivers and to understand its impact from their perspective.
Acknowledgments
The analyses reported in this manuscript were generously funded by NIA R01 AG040770, NIA K02 AG048240, NIA P30 AG010133 and the Easton Consortium for Alzheimer Drug Discovery and Biomarker Development.
Footnotes
Disclosures:
Rafid Mustafa, BS, has nothing to disclose.
Jared R. Brosch, MD, MS, has research support from Avanir Pharmaceuticals, Axovant, AbbVie, Biogen, Eisai, Eli Lilly, Genentech, Roche, TauRx
Gil Rabinovici, MD, has received research support from Avid Radiopharmaceuticals, GE Healthcare, Piramal Imaging. He has served as a consultant and/or the Speakers Bureau for Eisai, Genentech, Lundbeck, Putnam, Roche and Merck.
Brad Dickerson, MD, has served as a consultant for Lilly, Biogen, Ionis, Piramal, Med Learning Group and Haymarket Medical Education. He serves on the Data Safety Monitoring Board for Merck and receives royalties form Oxford University Press and Cambridge University Press
Maria C. Carrillo, PhD, is a full time employee of the Alzheimer’s Association, sponsor of TrialMatch
Brad Glazier serves as Managing Editor for Brain Imaging and Behavior.
Sujuan Gao, PhD, has nothing to disclose.
Martha Tierney, LCSW, is a full time employee of the Alzheimer’s Association, sponsor of TrialMatch
Keith N. Fargo, PhD, has nothing to disclose
Mary G. Austrom, PhD, has nothing to disclose.
Susan De Santi, PhD, is a full time employee of Piramal Imaging, LLC
David G. Clark, MD, has nothing to disclose.
Liana Apostolova, MD, MS, has served on the Speaker Bureau for Piramal Imaging, Inc and Eli Lilly and as an Advisory Board Member for Eli Lilly. Dr. Apostolova has received research funding from General Electric Healthcare.
References
- 1.Alzheimer’s Association. 2017 Alzheimer’s disease facts and figures. Alzheimers Dement. 2017;13:325–373. [Google Scholar]
- 2.McKhann GM, Knopman DS, Chertkow H, et al. The diagnosis of dementia due to Alzheimer’s disease: Recommendations from the National Institute on Aging and the Alzheimer’s Association workgroup. Alzheimers Dement. 2011;7(3):263–269. doi: 10.1016/j.jalz.2011.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 4.Hyman BT, Phelps CH, Beach TG, et al. National Institute on Aging-Alzheimer’s Association guidelines for the neuropathologic assessment of Alzheimer’s disease. Alzheimers Dement. 2012;8(1):1–13. doi: 10.1016/j.jalz.2011.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Montine TJ, Phelps CH, Beach TG, et al. National Institute on Aging-Alzheimer’s Association guidelines for the neuropathologic assessment of Alzheimer’s disease: a practical approach. Acta Neuropathol. 2012;123(1):1–11. doi: 10.1007/s00401-011-0910-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beach TG, Monsell SE, Phillips LE, et al. Accuracy of the clinical diagnosis of Alzheimer disease at National Institute on Aging Alzheimer Disease Centers, 2005–2010. J Neuropathol Exp Neurol. 2012;71(4):266–73. doi: 10.1097/NEN.0b013e31824b211b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jack CR, Knopman DS, Jagust WJ, et al. Hypothetical model of dynamic biomarkers of the Alzheimer’s pathological cascade. Lancet Neurol. 2010;9(1):119–28. doi: 10.1016/S1474-4422(09)70299-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barthel H, Gertz HJ, Dresel S, et al. Cerebral amyloid-beta PET with florbetaben (18F) in patients with Alzheimer's disease and healthy controls: a multicentre phase 2 diagnostic study. Lancet Neurol. 2011;10(5):424–35. doi: 10.1016/S1474-4422(11)70077-1. [DOI] [PubMed] [Google Scholar]
- 9.Sabri O, Sabbagh MN, Seibyl J, et al. Florbetaben PET imaging to detect amyloid beta plaques in Alzheimer's disease: phase 3 study. Alzheimers Dement. 2015;11(8):964–74. doi: 10.1016/j.jalz.2015.02.004. [DOI] [PubMed] [Google Scholar]
- 10.Clark CM, Pontecorvo MJ, Beach TG, et al. Cerebral PET with florbetapir compared with neuropathology at autopsy for detection of neuritic amyloid-beta plaques: a prospective cohort study. Lancet Neurol. 2012;11(8):669–78. doi: 10.1016/S1474-4422(12)70142-4. [DOI] [PubMed] [Google Scholar]
- 11.Clark CM, Schneider JA, Bedell BJ, et al. Use of Florbetapir-PET for Imaging β-Amyloid Pathology. JAMA. 2011;305(3):275–83. doi: 10.1001/jama.2010.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yang L, Rieves D, Ganley C. Brain amyloid imaging - FDA approval of Florbetapir F18 injection. N Engl J Med. 2012;367(10):885–7. doi: 10.1056/NEJMp1208061. [DOI] [PubMed] [Google Scholar]
- 13.Vandenberghe R, Van Laere K, Ivanoiu A, et al. 18F–flutemetamol amyloid imaging in Alzheimer disease and mild cognitive impairment: a phase 2 trial. Ann Neurol. 2010;68(3):319–29. doi: 10.1002/ana.22068. [DOI] [PubMed] [Google Scholar]
- 14.Curtis C, Gamez JE, Singh U, et al. Phase 3 trial of flutemetamol labeled with radioactive fluorine 18 imaging and neuritic plaque density. JAMA Neurol. 2015;72(3):287–94. doi: 10.1001/jamaneurol.2014.4144. [DOI] [PubMed] [Google Scholar]
- 15.Yeo JM, Waddell B, Khan Z, et al. A systematic review and meta-analysis of 18F–labeled amyloid imaging in Alzheimer’s disease. Alzheimer’s & Dementia: Diagnosis, Assessment & Disease Monitoring. 2015;1:5–13. doi: 10.1016/j.dadm.2014.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ma Y, Zhang S, Li J, et al. Predictive accuracy of amyloid imaging for progression from mild cognitive impairment to Alzheimer disease with different lengths of follow-up: a meta-analysis. [Corrected] Medicine (Baltimore) 2014;93(27):e150. doi: 10.1097/MD.0000000000000150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ossenkoppele R, Jansen WJ, Rabinovici GD, et al. Prevalence of amyloid PET positivity in dementia syndromes: a meta-analysis. JAMA. 2015;313(19):1939–1949. doi: 10.1001/jama.2015.4669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Johnson KA, Minoshima S, Bohnen NI, et al. Appropriate use criteria for amyloid PET: a report of the Amyloid Imaging Task Force, the Society of Nuclear Medicine and Molecular Imaging, and the Alzheimer's Association. Alzheimers Dement. 2013;9(1):e-1–16. doi: 10.1016/j.jalz.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jacques L, Jensen TS, Rollins J, et al. Decision memo for beta amyloid positron emission tomography in dementia and neurodegenerative disease. Centers for Medicare & Medicaid Services. 2013 [Google Scholar]
- 20.Grundman M, Johnson KA, Lu M, et al. Effect of Amyloid Imaging on the Diagnosis and Management of Patients with Cognitive Decline: Impact of Appropriate Use Criteria. Dement Geriatr Cogn Disord. 2016;41(1–2):80–92. doi: 10.1159/000441139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bensaidane MR, Beauregard JM, Poulin S, et al. Clinical utility of amyloid PET imaging in the differential diagnosis of atypical dementias and its impact on caregivers. J Alzheimers Dis. 2016;52(4):1251–62. doi: 10.3233/JAD-151180. [DOI] [PubMed] [Google Scholar]
- 22.Mitsis EM, Bender HA, Kostakoglu L, et al. A consecutive case series experience with [18 F] florbetapir PET imaging in an urban dementia center: impact on quality of life, decision making, and disposition. Mol Neurodegener. 2014;9:10. doi: 10.1186/1750-1326-9-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sanchez-Juan P, Ghosh PM, Hagen J, et al. Practical utility of amyloid and FDG-PET in an academic dementia center. Neurology. 2014;82(3):230–8. doi: 10.1212/WNL.0000000000000032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zannas AS, Doraiswamy PM, Schpanskaya KS, et al. Impact of 18F–florbetapir PET imaging of beta-amyloid neuritic plaque density on clinical decision-making. Neurocase. 2014;20(4):466–73. doi: 10.1080/13554794.2013.791867. [DOI] [PubMed] [Google Scholar]
- 25.Ossenkoppele R, Prins ND, Pijnenburg YA, et al. Impact of molecular imaging on the diagnostic process in a memory clinic. Alzheimers Dement. 2013;9(4):414–21. doi: 10.1016/j.jalz.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 26.Apostolova LG, Haider J, Goukasian N, et al. Critical review of the Appropriate Use Criteria for amyloid imaging: effect on diagnosis and patient care. Alzheimers Dement (Amst) 2016;5:15–22. doi: 10.1016/j.dadm.2016.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zucchella C, Bartolo M, Bemini S, et al. Quality of life in Alzheimer disease: a comparison of patients’ and caregivers’ points of view. Alzheimer Dis Assoc Disord. 2015;29(1):50–4. doi: 10.1097/WAD.0000000000000050. [DOI] [PubMed] [Google Scholar]
- 28.Carpenter BD, Xiong C, Porensky EK, et al. Reaction to a dementia diagnosis in individuals with Alzheimer’s disease and mild cognitive impairment. J Am Geriatr Soc. 2008;56(3):405–12. doi: 10.1111/j.1532-5415.2007.01600.x. [DOI] [PubMed] [Google Scholar]
- 29.Jensen M, Agbata IN, Canavan M, et al. Effectiveness of educational interventions for informal caregivers of individuals with dementia residing in the community: systematic review and meta-analysis of randomised controlled trials. Int J Geriatr Psychiatry. 2015;30(2):130–143. doi: 10.1002/gps.4208. [DOI] [PubMed] [Google Scholar]
- 30.Lawrence V, Pickett J, Ballard C, et al. Patient and carer views on participating in clinical trials for prodromal Alzheimer’s disease and mild cognitive impairment. Int J Geriatr Psychiatry. 2014;29(1):22–31. doi: 10.1002/gps.3958. [DOI] [PubMed] [Google Scholar]
- 31.Lingler JH, Nightingale MC, Erlen JA, et al. Making sense of mild cognitive impairment: a qualitative exploration of the patient’s experience. Gerontologist. 2006;46(6):791–800. doi: 10.1093/geront/46.6.791. [DOI] [PubMed] [Google Scholar]
- 32.Karlawash JH, Casarett D, Klocinski J, et al. How do AD patients and their caregivers decide whether to enroll in a clinical trial? Neurology. 2001;56(6):789–92. doi: 10.1212/wnl.56.6.789. [DOI] [PubMed] [Google Scholar]
- 33.Ingram DD, Franco SJ. 2013 NCHS urban-rural classification scheme for counties. National Center for Health Statistics. Vital Health Stat. 2014;2(166) [PubMed] [Google Scholar]
- 34.Hart LG, Larson EH, Lishner DM. Rural definitions for health policy and research. Am J Public Health. 2005;95(7):1149–1155. doi: 10.2105/AJPH.2004.042432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. [Accessed May 4, 2017];U.S. Census Bureau: Census regions and divisions of the United States [U.S. Department of Commerce Economics and Statistics Administration web site] 2010 Available at: https://www.census.gov/geo/reference/gtc/gtc_census_divreg.html.
- 36.Agresti A. Categorical data analysis. 3. Hoboken, NJ: John Wiley & Sons; 2013. [Google Scholar]
- 37. [Accessed May 4, 2017];U.S. Census Bureau: Educational attainment in the United States: 2009 [U.S. Department of Commerce Economics and Statistics Administration web site] 2010 Available at: http://census.gov/content/dam/Census/library/publications/2012/demo/p20-566.pdf.
- 38. [Accessed May 4, 2017];U.S. Census Bureau: Health insurance coverage in the United States: 2015 [U.S. Department of Commerce Economics and Statistics Administration web site] 2015 Available at: http://census.gov/content/dam/Census/library/publications/2016/demo/p60-257.pdf.


