Abstract
Background
The primary objective of the study was to evaluate the efficacy of a community-based participatory intervention program in improving Hepatitis B (HBV) screening and vaccination among Korean Americans were not previously screened.
Methods
A cluster-randomized trial involving 32 Korean church-based community organizations (n = 1,834) was conducted. Sixteen churches were randomly assigned to HBV screening and vaccination multicomponent intervention condition (n=972) and 16 to general cancer education control condition (n = 862). Main components of the intervention program included interactive group education, patient navigation, and the engagement of health care providers, church leadership and church members in the medical field. Application of Community-Based Participatory Research (CBPR) principles were monitored and evaluated. HBV screening and vaccination rates (self-reported and medical record verification) were assessed at 6-month and 12-month follow-ups respectively.
Results
The study showed significant efficacy in HBV screening rate (92.5% in intervention vs 5.5% in control), 3-series HBV vaccination completion rate (84% in intervention vs 17.6% in control), and overall screening and vaccination compliance rate (87% in intervention vs 3.8% in control). Participants in the intervention group were significantly more likely to receive HBV screening (92.5%) as compared with those in the control group (5.5%). In multivariate mixed-effect logistic regression analysis, odds ratio for intervention effect on HBV screening was 512.3 (95% CI) after adjusting for cluster effect and other demographic variables. Regarding vaccination rates, of 332 participants who were screened with no immunity in the intervention group, 308 (92.8%) received at least one HBV vaccination, 300 (90.4%) received at least two shots, and 279 (84%) received all three shots.
Conclusions
A combination of CBPR and multilevel approach may produce the most optimal results and be essential in producing considerable effect in enhancing HBV screening and vaccination, particularly for Korean American populations with limited language proficiency and insurance coverage.
Keywords: HBV screening and vaccination, community-based participatory research, intervention, Korean Americans, Korean churches
INTRODUCTION
Hepatitis B virus infection (HBV) is a strong risk predictor of Hepatocellular carcinoma, the major form of primary liver cancer. The risk of liver cancer in persons with chronic HBV infection is 200 times greater than for those not infected and one of every four people with chronic HBV infection eventually dies of cirrhosis or liver cancer.1,2 In the US, approximately 2.2 million people are living with chronic hepatitis B and Asians/Pacific Islanders account for 58% of the chronic cases,3,4 with the highest prevalence among foreign-born Asian immigrants.5,6 This high incidence of chronic HBV infection contributes to incidence and mortality rates approximately two times greater in Asian Americans than in general population.7,8
Hepatitis B is a preventable disease, and HBV screening and vaccination are the most effective means to reduce morbidity and mortality rates of Hepatocellular carcinoma. Current guidelines recommend that Hepatitis B serologic testing should be conducted for adolescents and adults who were born in highly endemic areas, including Asia and the Pacific Islands and US-born persons not vaccinated as infants whose parents were immigrants from Asia.9 Despite their elevated disease vulnerability, HBV screening and vaccination rates among Asian Americans are not optimal, with estimated screening rates below 30–50% and vaccination rates below 30–40%.10,11
Korean Americans, a rapidly growing ethnic community and the fifth largest among Asian American groups in the US, report the second highest incidence rates of liver cancer and the highest liver cancer-related mortality rates.12 The prevalence of hepatitis B (Hep B) surface antigen positivity is also high among US Korean adults, particularly among Korean men, ranging from 4.9% to 7.5%13–15, comparing to 0.3 – 0.5% in general population.5 However, estimated rates of Korean Americans who had ever been screened for HBV are 32% – 56%, and of those who remain susceptible to future infection, only 38% have ever been vaccinated.11,16,17 The factors contributing to poor screening and vaccination in Korean Americans are complex, including lack of knowledge and misinformation about Hep B and liver cancer (e.g., transmission channel and cause of Hepatitis B and liver cancer), psychosocial beliefs and emotion (e.g., fear of being diagnosed with Hep B, concerns about burdening one’s family), and structural barriers to health care access (e.g., cost, unfamiliarity with health care system).16–19 Considering the high HBV-induced liver cancer burden and low rates of screening uptake due to multilevel barriers, Korean Americans are an important target group for implementation of innovative programs designed to increase screening and vaccination by tailoring programs to their needs.
Implementing intervention programs to reduce the liver cancer and Hepatitis B disparities in this population requires a long-term partnership among the medically underserved health disparity communities, clinical providers, and research institutions. Community-based participatory research (CBPR) has a promising potential to generate partnership collaborative processes in planning, implementing, evaluating and disseminating a culturally and linguistically appropriate and effective Hep B intervention.20 As one of the community-based organizations, Korean churches represent an important resource to increase HBV screening and vaccination among Korean Americans. Approximately three out of four Korean Americans attend a church on a regular basis.21,22 For many Korean Americans, a church is a place for fellowship, maintenance of cultural tradition, social services, and social status.23 Therefore, Korean churches are hospitable partners that facilitate the delivery of culturally and linguistically appropriate intervention.
The present study is one of the first large-scale cluster randomized church-based intervention trials to improve HBV screening among Korean Americans. To the best of our knowledge, only one study has evaluated the efficacy of a church-based intervention to enhance liver cancer- related HBV testing among Koreans in Los Angeles.24 Although the intervention was significantly effective compared to the control condition, the rate of HBV testing at the 6-month follow-up was only 19%, leaving room for improvement. The authors of the study indicated that the focus of their intervention on individual level factors might have contributed to the modest screening uptake rate, suggesting more intensive community interventions which include patient navigation, free or low cost testing, and/or multiple contacts/reminders for future studies.
The intervention trial of the present study addressed the gap by focusing on both individual and health care system barriers through multifaceted, culturally appropriate innovative program elements. In addition, we included 12-month follow-up for HBV vaccination with those susceptible to future infection based on the 6-month screening results. The purpose of the study is to use a CBPR approach that engages Korean church leaders in developing and conducting a culturally and linguistically appropriate intervention to evaluate its efficacy 1) in increasing HBV screening for never screened Koreans at 6-month follow up, and 2) in increasing HBV vaccination for Koreans with no immunity at 12-month follow-up.
METHODS
Participants
Korean American participants (n = 1,834) from 32 churches in Pennsylvania and New Jersey enrolled in the study. Participants were eligible to attend this study if they: 1) self-identified their ethnic ancestry as Korean Americans; 2) were age 18 or older; 3) have never enrolled in any HBV intervention program; 4) have never had HBV screening; 5) were not aware of HBV infection status; 6) had a telephone access (for scheduling and contact purposes only). Forty-Six Korean churches were initially reached and 32 were enrolled in this study. We paired the 32 churches by size and geographic region and then randomized each church of 16 pairs into either intervention or control group. Among the 14 churches excluded in this study, 2 chose not to participate and the remaining 12 did not have enough membership size for recruitment. A total of 2,439 participants were contacted among these 32 churches, and 2,212 were recruited and screened for eligibility, leaving 1,982 eligible. The final number of participants who consented and completed the baseline data collection was 1,834, with 972 in intervention group and 862 in the control group using a matched-pair design. The retention rate of 6-month follow-up was 94.2% for intervention group and 83% for control group (Figure 1).
Figure 1.
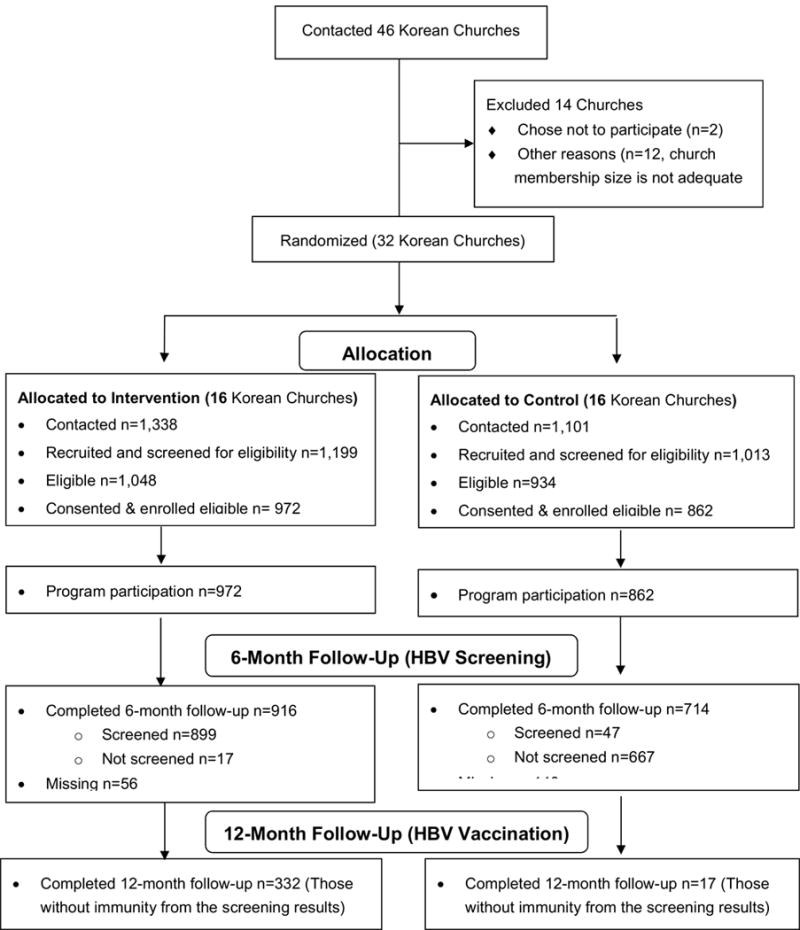
Korean CBPR HBV Intervention Study Flow Diagram
Procedures
The study was approved by the Institutional Review Board. The study was designed as a collaborative partnership between the Center for Asian Health (CAH) at Temple University and Korean community-based organizations. The Korean community-based organizations are members of the Asian Community Health Coalition (ACHC) which consists of 390 partner organizations. The CAH and the ACHC have collaborated since 2000, guided by CBPR principles. The CBPR framework was used to guide the present study and partner churches were directly involved in developing, implementing, and evaluating the protocols for the study.
In the planning phase, the Community Advisory Board (three members from community-based organizations, six from Korean churches, two health care providers, and one from an academic institution) was established to guide all aspects of the partnership serving as the liaison between CAH and the community study sites to ensure the application of CBPR approach to the intervention program activities. To strengthen the academic-community collaboration, one of the church leaders was appointed as the community co-principal investigator of the program. In addition, a full-time bilingual community coordinator was hired at CAH to work closely with the church leaders and church-designated staff in the process of project implementation and providing technical assistance to participating churches.
For the development of intervention, in-person interviews with church pastors (n=30) and needs assessment with community members (n = 384) were conducted in a semi-structured way to gain in-depth knowledge about the needs of Korean American community and the characteristics of Korean churches. The results of the interviews and needs assessment were used to develop a culturally and linguistically appropriate HBV intervention program. Community advisory board members and church leaders were actively involved in the intervention development by providing input through regular planning meetings. Their views on cultural elements, as well as the program settings, were well incorporated into the program curriculum and intervention.
For the implementation of the intervention program, participant recruitment strategies and tools were co-developed with community leaders and the community coordinator. Recruitment procedures included church pastors’ announcements about the study after mass services, community coordinator’s task assignment to church staff, and trained church health workers’ assistance with registration for education session. Church leaders and staff used an HBV fact sheet, program recruitment flyer, and registration sheet to facilitate participants’ recruitment. Research staff performed the eligibility screening and obtained consent among the eligible individuals who expressed interest in participating in the study. Research team members and trained church health workers co-delivered educational sessions. Before the program implementation, research team members, the community coordinator, and designated church staff received intensive training regarding a study protocol, facilitation guidelines, and participants’ rights by the study PI and co-Investigators.
To ensure that the collaborative relationship between research team and community organizations followed main principles of CBPR, we asked church leaders/representatives to complete a partnership assessment after implementation of intervention. In addition, we used other channels and methods to monitor the process and extent of CBPR application. More detailed information about the CBPR approach we used for this study is described in another published study.17
Study design
The study was a two-arm cluster randomized trial with churches as the unit of randomization. Based on organization profile information provided by collaborating church leaders, we developed an algorithm to match each pair on the basis of education, age, and geographic location. Then, each member of the pair was randomly assigned to the intervention or control group. We collected assessment data at baseline, 6-month follow-up, and 12-month follow-up.
Intervention and control conditions
The intervention was designed to improve HBV screening among previously unscreened individuals and guided by the Health Belief Model and Social Cognitive Theory to address multilevel barriers.25, 26 Main intervention components included interactive group education, navigation services, and the engagement of health care providers and church leadership and church members in the medical field in advocacy, referrals and linkage to care. The interactive group education was delivered by bilingual community health educators (CHEs) for about two hours to 15 to 20 participants. The education session consisted of the following components: 1) HBV prevalence and risk factors; 2) information about HBV transmission; 3) HBV infection process to cause liver cancer; 4) HBV and liver cancer prevention strategies (e.g., screening and vaccination); 5) factors associated with HBV screening and vaccination (e.g., barriers, facilitators, strategies to communicate with health providers regarding different options for prevention and treatment of HBV). Patient navigation assistance was offered to all participants in the intervention group and provided to those who requested it by trained bilingual patient navigators upon request. The patient navigation assistance included language translation, appointment scheduling, transportation, provision of information related to the health care system, low-cost health services, and free HBV screening events provided by community health providers. Bilingual physicians provided clinical support and ensured successful vaccination follow-ups by offering more flexible open hours of clinic operation with bilingual medical staff on site.
Participants in the control condition were provided a group education session in a similar format of that for the intervention group. However, the content was different, focusing on general cancer and health issues including information about HBV-related liver cancer prevention and various types of cancer screening. Printed education materials available from federal agencies translated in Korean were provided to control group participants. Participants in control group were also encouraged to undergo routine medical check-ups with a healthcare provider.
Measures
The assessments of the study were originally developed in English, translated into Korean, and back-translated to English by bilingual translators to ensure equivalence.
Demographic variables
Information on gender, education, marital status, household income, employment, health insurance and regular physician status, ability to speak English, and cultural engagement was collected at baseline.
Screening status
The primary outcome was HBV screening at the 6 months after the intervention. Bilingual interviewers contacted participants at the 6-month follow-up and asked participants whether they received HBV screening with the response options “yes” or “no.” Participant’s self-report was confirmed by health provider. For the validation process, participants who reported receiving a screening test were asked to provide consent to allow research staff to contact their health providers to validate screening status.
Vaccination status
Vaccination status among the participants who were screened for having no HBV immunity was also measured. Participants were asked to report whether and how many times they received vaccination against HBV infection at the 12-month follow-up post intervention. Validation of the participant’s report was confirmed by his or her health providers with the participant’s permission.
CBPR Partnership Evaluation
As a process outcome, a Bell-Elkins questionnaire25 was used to evaluate the level of adherence to each CBPR principle in various stages of the research project, organizational partnerships, and resources. The assessment covered 10 principles of CBPR application described in Table 1, which together evaluated the strength of the partnership. Participants were asked to answer “yes” or “no” or rate on a scale of 1 to 5 (1 “never true” to 5 “always true”) on questions designed to cover each of the 10 principles.
Table 1.
Ten CBPR principles applied to this study
| Principle 1 | Partners have agreed upon mission, values, goals, and measurable outcomes for the partnership. |
| Principle 2 | The relationship between partners is characterized by mutual trust, respect, genuineness, and commitment. |
| Principle 3 | The partnership builds upon identified strengths and assets, but also addresses areas that need improvement and address areas that need improvement. |
| Principle 4 | The partnership balances power among partners and enables resources among partners to be shared. |
| Principle 5 | There is clear, open and accessible communication between partners. Members make it an ongoing priority to listen to each other. The group has developed a common language that clarifies the meaning of terms, events, or incidents. |
| Principle 6 | Roles, norms, and processes for the partnership are established with the input and agreement of all partners. |
| Principle 7 | There is feedback to, among, and from all stakeholders in the partnership, with the goal of continuously improving the partnership and its outcomes. |
| Principle 8 | Partners share the credit for the partnership’s accomplishments. |
| Principle 9 | Partnerships take time to develop and evolve over time. |
| Principle 10 | The partnership is a community-campus partnership. |
Data Analysis
Demographic variables of interest were described using frequency and percent within each of the treatment groups (intervention versus control). The Rao-Scott chi-square test, which accounts for the design effects of clustering at the church level, was used for categorical variables to assess whether the distributions differed between the treatment and control groups. For continuous variables, t-test was used.
The primary aim of the study was to determine whether HBV screening at 6 months post intervention varied between the intervention and control groups. To compare the proportion of participants in the intervention and control groups who completed HBV screening at 6-month post the intervention, the Rao-Scott chi-square test was used. In the analysis, those who did not complete the 6-month follow-up were treated as non-screeners using intent-to-treat approach. A multiple logistic regression model was estimated to determine the strength of the treatment group associations with adjustment for significant demographic and/or clinical variables. In all models, the covariance matrix was adjusted to account for clustering of individuals at the church level. Variables included in the multiple logistic regression models were specified a priori on the basis of previous research as potential confounders.
Correlations between covariates were assessed to identify potential multicollinearity. Since insurance status and regular primary physician had a tetrachoric correlation of .88, only one of the variables was selected for the model. Regular physician status was selected over health insurance status because having health insurance does not guarantee that a participant has a regular physician. This is particularly true in the Korean culture when participants have varying English speaking abilities, and thus a limited number of physicians to choose from.
Among the screened participants who had no HBV immunity, the proportion of individuals in the intervention and control groups who received one shot, two shots, and three shots of the HBV vaccination series was summarized. In addition to the HBV vaccine completion rates based on the participants with no HBV immunity, we used intent to treat analysis to calculate the overall screening and vaccination compliance rate (OCR) based on the total participants enrolled. For the partnership evaluation as a process outcome, descriptive analysis was conducted to describe frequency and percentile of those who endorsed each principle of CBPR. All analyses were performed in SAS version 9.3 (SAS Institute Inc., Cary, NC).
RESULTS
Participant Characteristics
The mean age of participants was 51.6. There were slightly more females (58.0%) than males enrolled in the study. A majority was foreign born (93.4%) and married (79.3%). More than half had some college education or higher (58.0%), earned $40,000 or less annual income (66.5%), were employed (55.9%), did not speak English well (59.0%), and sometimes participated in social gatherings (66.5%). Approximately half of participants had health insurance (50.3%) and a regular physician (49.7%). Table 2 describes and compares sociodemographic characteristics for the intervention and control groups. No statistical differences between the groups were observed by gender, marital status, education, employment, and cultural engagement (all p-values > 0.05). Statistically significant differences in age, annual household income, health insurance status, regular physician status, and ability to speak English were observed between the two groups. Compared to the control group, the intervention group has a higher percentage of participants that are younger, had a household income less than $40,000, were uninsured or underinsured, did not have a regular physician, and did not speak English well (all p-values < .001).
TABLE 2.
Characteristics of Intervention and Control Group Participants: HBV Screening Program (n = 1,834)
| Intervention Group | Control Group | ||
|---|---|---|---|
| Variable | (n = 972) No. (%) |
(n = 862) No. (%) |
P1 |
| Age: Mean ± SD, median | 49.63 ± 13.3, 49 | 53.91 ± 13.4, 54 | < .0001 |
| Gender | .2277 | ||
| Male | 406 (41.8) | 343 (39.8) | |
| Female | 550 (56.6) | 514 (59.6) | |
| Marital status | .2481 | ||
| Married | 776 (79.8) | 678 (78.7) | |
| Not married | 155 (16.0) | 170 (19.7) | |
| Education | .8708 | ||
| Below high school | 89 (9.2) | 78 (9.0) | |
| High school graduate | 245 (25.2) | 245 (28.4) | |
| Some college or higher | 552 (56.8) | 511 (59.3) | |
| Annual household income | < .0001 | ||
| Less than $20,000 | 268 (34.5) | 203 (27.1) | |
| $20,000 – $40,000 | 290 (37.3) | 254 (33.9) | |
| Greater than $40,000 | 219 (28.2) | 293 (39.1) | |
| Health insurance status | < .0001 | ||
| No | 511 (52.6) | 319 (37.0) | |
| Yes | 393 (40.4) | 530 (61.5) | |
| Regular physician status | < .0001 | ||
| No | 520 (53.5) | 294 (34.1) | |
| Yes | 381 (39.2) | 531 (61.6) | |
| Employment | .2032 | ||
| Employed | 556 (57.2) | 470 (54.5) | |
| Unemployed/retired/homemaker | 357 (36.7) | 372 (43.16) | |
| Ability to speak English | < .0001 | ||
| Not at all | 140 (15.2) | 54 (6.3) | |
| Not well | 561 (61.0) | 521 (61.2) | |
| Well | 182 (19.8) | 230 (27.0) | |
| Very well | 36 (3.9) | 46 (5.4) | |
| Cultural engagement2 | .2131 | ||
| All the time | 52 (5.3) | 49 (5.7) | |
| Sometimes | 631 (64.9) | 586 (68.0) | |
| Not at all | 166 (17.1) | 209 (24.2) | |
P-values based on Rao-Scott chi-square test excluding missing values. Rao-Scott chi-square test used to account for design effects of clustering at the church level.
Variable corresponds to survey the question “Do you often participate in social cultural gatherings?”
Intervention Effect
As shown in Table 3, HBV screening rates were significantly different between intervention and control groups. A total of 899 out of 972 (92.5%) and 47 out of 862 (5.5%) participants were screened for HBV in intervention and control groups, respectively (p < .001). Among those screened, the distributions of results were similar across groups. Validation of self-reported screening status was conducted among the participants who reported receiving screening test. Screening status of the 899 intervention group participants and 30 (out of 47) control group participants who reported being screened was verified by their medical records. Verification results showed that 98.7% (887 out of 899) of medical records of intervention group participants and 76.6% (23 out of 30) of medical records of control group participants matched self-reported screening status.
TABLE 3.
HBV Screening Rates at 6 Month- Follow-up (n = 1,834)1
| Intervention (n= 972) | Control (n= 862) | ||
|---|---|---|---|
| Outcome | n (%) | n (%) | P |
| HBV screening behavior | 899 (92.5) | 47 (5.5) | < .0001 |
|
| |||
| HBV screening results | |||
| No immunity | 332 (36.93) | 17 (36.17) | |
| Currently infected | 27 (3.00) | 2 (4.26) | |
| Immune | 526 (58.51) | 26 (55.32) | |
| Not sure | 0 (.00) | 1 (2.13) | |
| Missing | 14 (1.56) | 1 (2.13) | |
P-value based on chi-square test excluding missing entries for screening behavior.
Table 4 provides the cumulative distribution for the number of shots received among the participants in the intervention group. Among the 332 participants in the intervention group with no HBV immunity, 308 (92.8%) pursued vaccination with 279 (84%) receiving all three series shots as the vaccination completion rate. In the control group, out of 17 participants with no HBV immunity, only 3 (17.6%) completed all three series shots. The overall screening and vaccination compliance rates (OCR) were calculated using the formula (N of those with immunity and no need for vaccination + N of those completed 3 series of vaccination) / N of total participants assigned to each group. OCR was 87% ((567+279)/972) for intervention group and 3.8% ((30+3)/862) for control group.
TABLE 4.
HBV Vaccination Completion Rates Among the Participants with no HBV Immunity and Overall Screening and Vaccination Compliance Rates (OCR)
| Intervention (n = 332) | Control (n=17) | ||
|---|---|---|---|
| Outcome | n (%) | n (%) | P |
| 1 shot received | 308 (92.77) | 5 (29.4%) | <0.001 |
| 2 shots received | 300 (90.36) | 4 (23.5%) | <0.001 |
| 3 shots received | 279 (84.04) | 3 (17.6%) | <0.001 |
| OCR | 87% | 3.8% | <0.001 |
P-value based on chi-square test.
Mixed effect multivariate regression analyses showed that the odds ratio for intervention effect on receiving HBV screening was significant (adjusted OR, 512.3; 95% CI, 195.2–1344.5; p < .001) controlling for significant demographic co-variates. Pseudo-R2 value of .29 suggested a good-moderate model fit. No covariates were significantly associated with screening status (Table 5).
TABLE 5.
Logistic Regression Model for Receipt of HBV Screening at 6 Months after the Program1 (n = 1,464)
| Variable | OR | 95% CI | P |
|---|---|---|---|
| Treatment group | |||
| Control | Ref | — | — |
| Intervention | 512.30 | 105.20-1,344.48 | < .0001 |
| Age, continuous | .99 | .97-1.02 | .58 |
| Annual household income | |||
| Less than $20,000 | Ref | — | — |
| $20,000 - $40,000 | .95 | .54-1.67 | .87 |
| Greater than $40,000 | .75 | .41-1.38 | .35 |
| Regular physician status | |||
| No | Ref | — | — |
| Yes | .89 | .02-0.41 | .654 |
| Ability to speak English | |||
| Not at all | Ref | — | — |
| Not well | .80 | .34-1.89 | .61 |
| Well | .53 | .20-1.43 | .21 |
| Very Well | .33 | .09-1.21 | .35 |
Abbreviations: CI, confidence interval; OR, odds ratio; Ref, referent category.
Model statistics: Pseudo R2 = .29; intraclass correlation coefficient = .24.
CBPR Partnership Evaluation
Sixty leaders and representatives from the partner churches completed the CBPR partnership evaluation. Results from the assessment showed that majority of church leaders endorsed adhering to CBPR principles. Most participants rated “yes” to Principle One (70.0%), and “always” or “usually true” to Principles Two (96.4%), Three (70.0%), Four (80.7%), Five (90.0%), Six (61.7%), Seven (86.7%), Eight (80.0%), Nine (69.5%), and Ten (95.0%).
DISCUSSION
This study examined the efficacy of a culturally and linguistically appropriate multilevel intervention designed to enhance HBV screening and vaccination in a large community sample of Korean Americans. The randomized controlled trial demonstrated that the multicomponent HBV intervention program was significantly effective in increasing HBV screening at 6-month follow-up (92.5% vs. 5.5%). The odds for completing HBV screening were substantially higher for the intervention group than those for the control group after adjusting for cluster effect and other demographic variables (OR = 512.3). In addition, majority of our participants in the intervention group who were screened for no HBV immunity received HBV vaccination at 12-month follow-up. Percentage of participants receiving one to three HBV vaccination shots ranged from 92.8% to 84%. The significant intervention effect on vaccination rate in those with no HBV immunity provides a promising intervention implication for liver cancer prevention and control. Our findings in this study demonstrated the efficacy of community-based participatory and multilevel intervention in reducing liver cancer disparity in this high-risk underserved population with limited English proficiency.
Findings of the present study also demonstrated that churches are strong candidates as ideal venues for implementing health programs among other community-based organizations in Korean American community. For Korean-Americans, churches function as an important social and educational center that provides cultural ties, identity, and acceptance as part of the community and social network.26 Regular church attendance among Korean American immigrants has been consistently high,27 and church members are cooperative with the events and activities encouraged by church pastors and leaders. Indeed, over 75% of individuals who were initially contacted participated in the study and over 90% of the participants who completed baseline assessment completed 6-month follow-up. In addition, church leaders showed a strong interest in working with researchers to meet their community’s social and health needs and followed the principles of CBPR well. In sum, the present study confirmed that Korean churches are promising partners for CBPR studies to reduce health disparities.
Interestingly, however, in the previous church-based Korean HBV screening study, the screening rate at follow-up was not optimal.24 Similar to our approach, they cluster randomized Korean churches and conducted interventions at the church setting utilizing small group presentations and discussions led by bilingual facilitators. However, the study had notable differences from our study. One difference was the degree of involvement of church leaders. Although the intervention was church-based, their study was mostly conducted by research staff, including recruitment and enrollment stages. In contrast, our study church leaders played a large and significant role throughout the whole process. They were active in recruiting members to participate, implementing services, and engaging physicians and nurses amongst church members. Another important difference between the previous study and ours was the provision of direct tools to overcome access barriers. In our study, we provided participants with navigation services. These differences may help explain why our study achieved a significantly higher screening rate at 6-months follow-up than other studies with various Asian American ethnic groups, in which screening rates among intervention group participants were less than 40%.24, 28–30
There are several unique strengths of this study that led to the remarkably robust effect. First, the CBPR program was built on a well-established strong partnership between the Center for Asian Health and Korean churches of the Asian Community Health Coalition. The CBPR approach was systematically and comprehensively applied throughout the study process. The academic and community leaderships have worked together to ensure equal and complementary partnership in developing and implementing the study. The trust and credibility built by a long-term collaboration history between partners appeared to be a critical and essential element of the successful CBPR partnership. In addition, CBPR approach was strenuously applied to all aspects of research to balance the science and community needs through effective communication and equal decision-making process during the program development and implementation. Close monitoring of the application and adherence to CBPR approach was made to ensure that partners followed the main principles of CBPR. These efforts led to a high level of adherence to each CBPR principle by study partners, which might have led to community empowerment, motivation, and pride of involvement in the research study.
Second, the intervention approach used in the present study addressed both individual and system level barriers. Compared to previous studies24, 28–30 that focused primarily on individual education and motivation, our study not only included intensive community education and direct involvement with community leaders in planning and organization, but also incorporated system-based components, specifically patient navigation services (transportation assistance, appointment scheduling, language translation) and active engagement of health care providers. The substantial barriers to health care access Korean Americans face include limited English proficiency, uninsured or underinsured status, low income, and a lack of familiarity with the US health care system.31–34 To respond to the high proportion of community members who are underinsured or uninsured, we negotiated with health care providers to lower the cost of HBV test, vaccination, and clinical consultations, as well as providing patient navigation and assistance.
These findings suggest that systemic components which increase access to the health care system for Asian Americans in screening interventions are conducive to maximizing the effect. Furthermore, our findings demonstrate that a combination of CBPR method and multilevel approach would yield the most optimal results and could be essential to considerably enhancing HBV screening and vaccination, particularly for those immigrant populations with limited English proficiency and insurance coverage. Some of these intervention strategies were tested efficacious in our other cancer screening studies.35,36
Despite the large and robust intervention effect observed in this study, several limitations remain. First, majority of our study participants consisted of foreign-born Koreans residing in Pennsylvania and New Jersey. Therefore, results should be interpreted with caution when applying to general Korean American population or to Koreans in other US geographical areas. Second, we could not determine how much an individual component in the intervention program such as church leader engagement, group education, and patient navigation contributed to the final intervention effect. Although our findings exhibit that the multilevel CBPR intervention components altogether were effective in overcoming multilevel barriers, future studies about the independent effect of each intervention component would be beneficial in revealing the mechanism of the effect. Third, despite the randomization procedures, intervention and control groups were different on several sociodemographic characteristics. The participants in control group were significantly more likely to have higher income, health insurance and a regular physician (p < .001), which typically would have promoted their access to care. Even with this advantage, the control group had a drastically lower overall screening and vaccination compliance rates than the intervention group, affirming that the intervention used in the present study was truly robust.
Overall, the present study is one of the first large-scale clustered randomized intervention trials that demonstrated strong evidence on the efficacy of a culturally appropriate community-based participatory intervention to increase HBV screening and vaccination among the high-risk population. This study addressed the health disparities suffered by high-risk medically underserved Korean Americans with low HBV screening and vaccination uptake rates. The successful implementation of our intervention program demonstrated the efficacy evidence of culturally appropriate church-based multilevel strategies for increasing HBV screening and vaccination behaviors among Korean Americans who are disproportionally at high risk for HBV infection. In particular, combined efforts to adhere to CBPR principles and to address both individual and system level barriers may be the integral component for a large and robust intervention effect. This multilevel CBPR intervention strategy could be extended to other similar population trials and future studies to further contribute to the elimination of health disparities in HBV-associated liver cancer and other health outcomes.
Acknowledgments
This research was supported by the National Institutes of Health (NIH), National Institute of Minority Health and Health Disparities (NIMHD; grant R24MD002756 to PI: Grace X. Ma, PhD) and the Community Cancer Health Disparities Center (grant U54 CA153513 to PI: Grace X. Ma, PhD). The authors wish to thank the Asian Community Health Coalition and its Korean member organizations for their collaboration. Note: The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the NIMHD or the NIH.
Footnotes
Author Contribution:
Grace X. Ma, PhD: principal investigator, conceptualization, methodology, supervision, original drafting and final editing
Minsun Lee, PhD: manuscript draft, literature and editing
Yin Tan, MD, MPH: project administration and supervision for implementation
Alexandra Hanlon, PhD: Data analysis
Ziding Feng, PhD: methodology and manuscript contributions
Theresa Shireman, PhD: formal analysis, concepts and manuscript contributions
Joanne Rhee, MSW: project administration, coordination, and supervision,
Zhengyu Wei, PhD: manuscript contribution
Han Seung Koh, BS: project administration and coordination
Charles Kim, BS: project administration and coordination
Frank Wong, PhD: concept and manuscript contributions
Whitney York, MS: assisted with data clean and analysis
Conflicts of Interest: None
References
- 1.Chen CJ, Yang H, Su J. Risk of hepatocellular carcinoma cross a biological gradient of serum Hepatitis B virus DNA level. JAMA. 2006;295:65–73. doi: 10.1001/jama.295.1.65. [DOI] [PubMed] [Google Scholar]
- 2.Cantarini MC, Trevisani F, Morselli-Labate A. Effect of the etiology of viral cirrhosis on the survival of patients with hepatocellular carcinoma. Am J Gastroenterol 101. 2006:91–98. doi: 10.1111/j.1572-0241.2006.00364.x. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Table 3.4: Reported cases of chronic hepatitis B, by demographic characteristics and laboratory tests. 2013:2013–801937. [Google Scholar]
- 4.Pollack H, Wan K, Ramos R. Screening for chronic hepatitis B among Asian/Pacific Islander populations - New York City, 2005. MMWR Morb Mortal Wkly Rep. 2006;55:505–509. [PubMed] [Google Scholar]
- 5.Wasley A, Kruszon-Moran D, Kuhnert W. The prevalence of hepatitis B virus infection in the United States in the era of vaccination. J Infect Dis. 2010:192–201. doi: 10.1086/653622. [DOI] [PubMed] [Google Scholar]
- 6.Hwang JP, Roundtree A, Engebretson J, Suarez-Almazor M. Medical care of hepatitis B among Asian American populations: perspectives from three provider groups. J Gen Intern Med. 2010:220–227. doi: 10.1007/s11606-009-1204-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Center Institute. Table 1.21: US and SEER death rates by primary cancer site and race/ethnicity, 2007–2010. 2014:17. [Google Scholar]
- 8.Miller BA, Chu K, Hankey B, Ries L. Cancer Incidence and Mortality Patterns among Specific Asian and Pacific Islander Population in the U.S. Cancer Causes Control. 2008 doi: 10.1007/s10552-007-9088-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chou R, Dana T, Bougatsos C, Khangura J, Zakher B. Screening for hepatitis B virus infection in adolescents and adults: a systmatic review to update the U.S. Preventive Services Task Force recommendation. Ann Intern Med. 2014;161:31–45. doi: 10.7326/M13-2837. [DOI] [PubMed] [Google Scholar]
- 10.Hu DJ, Xing J, Tohme R, Liao Y, Pollack H, Ward J. Hepatitis B testing and access to care among racial and ethnic minorities in selected communities across the United States, 2009–2010. Hepatol. 2013;58:856–62. doi: 10.1002/hep.26286. [DOI] [PubMed] [Google Scholar]
- 11.Strong C, Lee S, Tanaka M, Juon HS. Ethnic differences in prevalence and barriers of HBV screening and vaccination among Asian Americans. J Community Health. 2012:1071–80. doi: 10.1007/s10900-012-9541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huang V, Li W, Tsai J, Begier E. Cancer mortality among Asians and Pacific Islanders in New York City, 2001–2010. J Cancer Epidemiol. 2013 doi: 10.1155/2013/986408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Navarro N, Lim N, Kim J, Joo E, Che K, Runyon B. Lower than expected hepatitis B virus infection prevalence among first generation Koreans in the US: Results of HBV screening in the Southern California Inland Empire. BMC Infect Dis. 2014;14:269. doi: 10.1186/1471-2334-14-269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hann HW, Hann R, Maddrey W. Hepatitis B virus infection in 6,130 unvaccinated Korean-Americans surveyed between 1988 and 1990. Am J Gastroenterol. 2007;102(4):767–772. doi: 10.1111/j.1572-0241.2007.01060.x. [DOI] [PubMed] [Google Scholar]
- 15.“Viral Hepatitis B: Fact Sheet.” n.d. National Center for Infectious Diseases, Division of Viral. Hepatitis. 2006;28 http://www.cdc.gov/ncidod/diseases/hepatitis/b/fact.htm. [Google Scholar]
- 16.Bastani R, Glenn B, Maxwell A, Jo AM. Hepatitis B testing for liver cancer control among Korean Americans. Ethn Dis. 2007;17:365–73. [PubMed] [Google Scholar]
- 17.Ma G, Gao W, Tan Y, Chae W, Rhee J. A community-based participatory approach to a hepatitis B intervention for Korean Americans. Progress in Community Health Partnership. 2012;6:7–16. doi: 10.1353/cpr.2012.0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hwang JP, Roundtree A, Suarez-Almazor M. Attitudes toward hepatitis B virus among Vietnamese, Chinese, and Korean Americans in the Houston area. Tex J Community Health. 2012;37(5):1091–100. doi: 10.1007/s10900-012-9543-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Philbin MM, Erby L, Lee S, Juon H. Heptatitis B and liver cancer among three Asian American sub-groups: A focus group inquiry. J Immigr Minor Health. 2012;14:858–68. doi: 10.1007/s10903-011-9523-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Israel B, Eng E, Schults N, Parker E. Methods for Community-Based Participatory Research for Health. San Francisco, CA: John Wiley & Sons; 2013. [Google Scholar]
- 21.Min PG. Asian Americans: Contemporary Trends and Issues. 2nd. Thousand Oaks (CA): Pine Forge. Press, an Imprint of SAGE Publications, Inc; 2006. [Google Scholar]
- 22.Hurh WM, Kim K. Religious participation of Korean immigrants in the U.S. J Sci Study Relig. 1990;29(1):19–34. [Google Scholar]
- 23.Chang ET. Korean Americans. Asian-Nation: The Landscape of Asian America; http://www.asian-nation.org/korean.shtml Published January 13, 2003. [Google Scholar]
- 24.Bastani R, Glenn B, Maxwell A, Jo AM, Herrmann A, Crespi C. Cluster-Randomized Trial to Increase Hepatitis B Testing among Koreans in Los Angeles. Cancer Epidemiol Biomarkers Prev. 2015 doi: 10.1158/1055-9965.EPI-14-1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bell-Elkins J. Assessing the CCPH principles of partnership in a community–campus partnership [Internet] Seattle WA Community–Campus Partnersh Health. 2002 [Google Scholar]
- 26.Peterson J, Atwood JR, Yates B. Key elements for church-based health promotion programs: outcome-based literature review. Public Health Nurs. 2002;19(6):401–411. doi: 10.1046/j.1525-1446.2002.19602.x. [DOI] [PubMed] [Google Scholar]
- 27.Chong KH. What it means to be Christian: The role of religion in the construction of ethnic identity and buondary among second-generation Korean Americans. Sociol Relig. 1998;59(3):259–286. [Google Scholar]
- 28.Chen MS, Jr, Yang H, Su J. Increasing hepatitis B screening for Hmong adults: results from a randomized controlled community-based study. Cancer Epidemiol Biomarkers Prev. 2013;22:782–91. doi: 10.1158/1055-9965.EPI-12-1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Taylor VM, Hislop T, Tu S, Teh C, Acorda E, Yip M. Evaluation of a hepatitis B lay health worker intervention for Chinese Americans and Canadians. J Community Health. 2009;34(3):165–172. doi: 10.1007/s10900-008-9138-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Juon HS, Lee S, Strong C, Rimal R, Kirk G, Bowie J. Effect of a liver cancer education program on hepatitis B screening among Asian Americans in the Baltimore-Washington metropolitan area, 2009–2010. Prev Chronic Dis. 2014 doi: 10.5888/pcd11.130258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jang Y, Kim G, Chiriboga DA. Health, healthcare utilization, and satisfaction with service: Barriers and facilitators for older Korean Americans. J Am Geriatr Soc. 2005;53(9):1613–1617. doi: 10.1111/j.1532-5415.2005.53518.x. [DOI] [PubMed] [Google Scholar]
- 32.Song H-J, Han H-R, Lee J-E, et al. Does access to care still affect health care utilization by immigrants? Testing of an empirical explanatory model of health care utilization by Korean American immigrants with high blood pressure. J Immigr Minor Health. 2010;12(4):513–519. doi: 10.1007/s10903-009-9276-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shive SE, Ma GX, Tan Y, et al. Racial Differences in Preventive and Complementary Health Behaviors and Attitudes. J Health Disparities Res Pract. 2007:1. [Google Scholar]
- 34.Ma GX, Shive SE, Wang MQ, Tan Y. Cancer screening behaviors and barriers in Asian Americans. Am J Health Behav. 2009;33(6):650–660. doi: 10.5993/ajhb.33.6.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ma GX, Fang CY, Seals B, et al. A Community-Based Randomized Trial of Hepatitis B Screening Among High-Risk Vietnamese Americans. Am J Public Health. 2017;107(3):433–440. doi: 10.2105/AJPH.2016.303600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fang CY, Ma G, Handorf E, Feng Z, Tan Y, Rhee J. Addressing multilevel barriers to cervical cancer screening in Korean American: A randomized trial of a community - based intervention. Cancer. 2017;123(6):1018–1026. doi: 10.1002/cncr.30391. [DOI] [PMC free article] [PubMed] [Google Scholar]


