Abstract
Cervical corpectomy is a viable technique for the treatment of multilevel cervical spine pathology. Despite multiple advances in both surgical technique and implant technology, the rate of construct subsidence can range from 6% for single-level procedures to 71% for multilevel procedures. In this technical note, we describe a novel technique, the bump-stop technique, for cervical corpectomy. The technique positions the superior and inferior screw holes such that the vertebral bodies bisect them. This allows for fixation in the dense cortical bone of the endplate while providing a buttress to corpectomy cage subsidence. We then discuss a retrospective case review of 24 consecutive patients, who were treated using this approach, demonstrating a lower than previously reported cage subsidence rate.
Keywords: Cervical corpectomy subsidence, Expandable corpectomy cage, Bump-stop technique
Introduction
Cervical corpectomy is a technique available for the treatment of multilevel cervical spine pathology. By allowing direct decompression of the spinal cord from anterior pathology, correcting sagittal plane deformity, and increasing fusion rates, the utility of corpectomies has expanded since its introduction by Salcman [1,2]. Initial reconstruction utilizing grafts (autograft and allograft) was abandoned because of high pseudoarthrosis rates and graft complications ranging from collapse to extrusion [3,4,5]. As such, the technical performance of the reconstruction has developed over the years to include fixed anterior plating, titanium mesh cages, and now expandable titanium cages.
Despite advances in reconstructive technique, this procedure continues to have a high complication profile, particularly relating to construct subsidence and failure, ranging from 6% to 9% for single-level procedures to as high as 71% for three-level procedures [6]. Numerous authors have sought to investigate the mechanisms of construct subsidence/failure to identify the risk factors for early failures, and provide strategies to intervene, and thereby minimize, the complication profile [7,8,9]. Daubs [6] identified the cage height as an important variable in early failure rates when reconstructed with the use of titanium mesh cages, with taller cages increasing the failure rate. Hasegawa et al. [10] found that by increasing the diameter of the cage and surface area in contact with the end plate, significant improvement in the interface strength between the cage and vertebra can be achieved.
In this study, we introduce a novel technique for screw fixation of fixed anterior cervical plating following corpectomy and placement of an expandable titanium cage to reduce cage subsidence. We then report the clinical outcomes in 24 consecutive patients treated with this technique.
Technical Notes
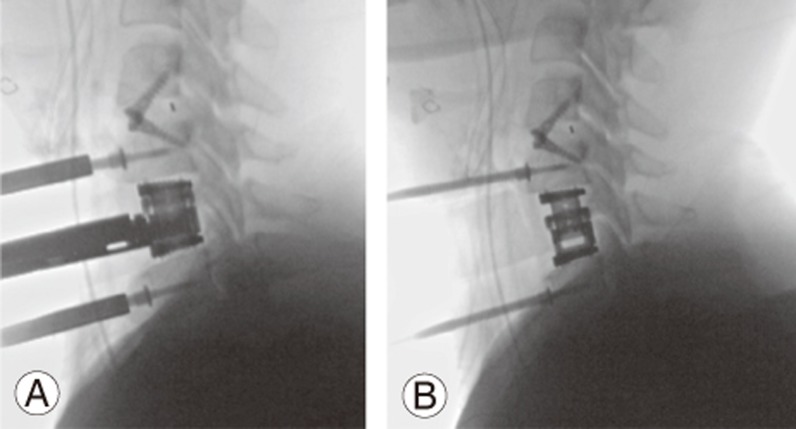
Corpectomy was performed according to the surgeon's preferred technique. Once the corpectomy was completed and the vertebral body removed, the excised bone was placed into a bone mill for use as local bone graft. An expandable titanium interbody cage was then placed and expanded to restore the vertebral height. We used the lateral radiograph during cage expansion to monitor the facet joint height to prevent over-distraction (Fig. 1).
Fig. 1. Intraoperative radiograms of a patient undergoing C4–5 anterior cervical discectomy and fusion with C5 corpectomy after expandable cage placement (A) and following cage expansion (B).
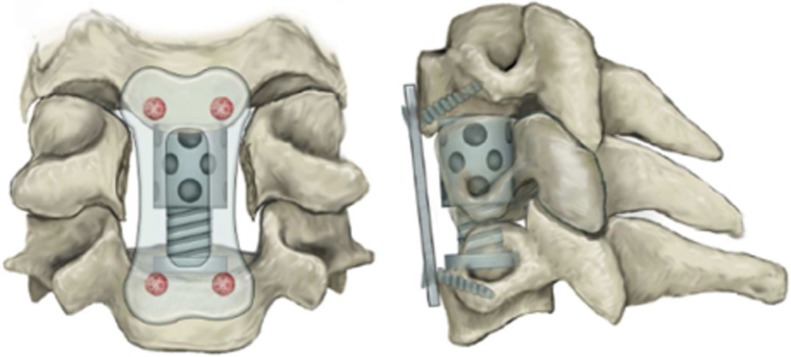
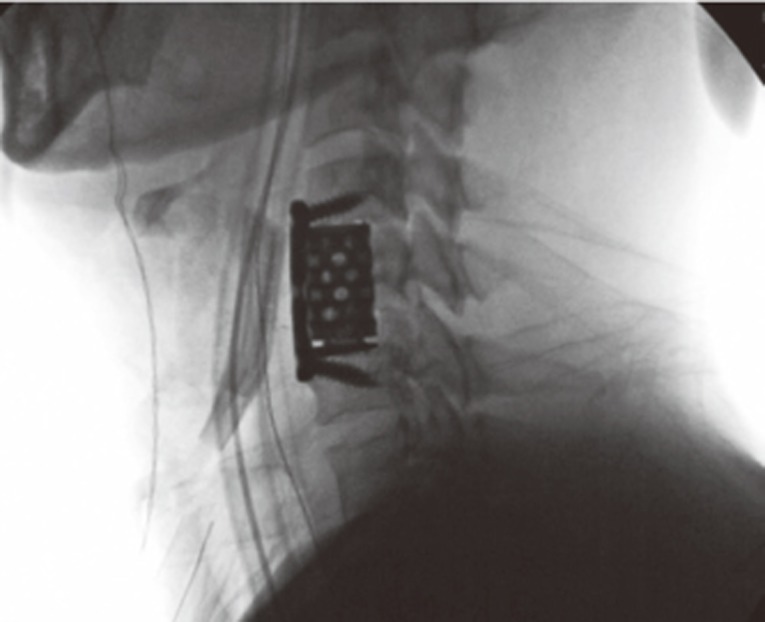
Once the desired height was established, local bone graft was then packed around the cage and a fixed angle anterior plate was used to secure the construct. The plate was sized such that the superior and inferior screw holes were bisected by the adjacent vertebral bodies (Fig. 2). An awl was then placed through the screw hole, aiming at an angle away from the corpectomy, followed by placement of an appropriately sized screw. This construct allows screw fixation into the dense bone of the endplate while simultaneously acting as a bump-stop to prevent subsidence of the cage (Fig. 3).
Fig. 2. Graphic depiction of hardware placement utilizing bump-stop technique.
Fig. 3. Postoperative fluoroscopy film showing the bump-stop technique.
Following surgery, patients were admitted for observation and pain control. We did not use cervical collars postoperatively, given the inherent stability of the instrumented constructs. Patients were discharged home and were examined during the follow-up at 2 weeks, 6 weeks, 3 months, 6 months, and 1 year, and annually if needed. Radiographs were obtained at 6 weeks, 3 months, and 6 months, and then at annual appointments as needed and assessed as indicated above.
A retrospective review of consecutive patients undergoing anterior cervical corpectomy utilizing the above technique with an expandable titanium cage, local bone graft, and fixed anterior cervical plate between January 2009 and December 2014 was performed. Procedures were performed by one of two fellowship-trained orthopedic spine surgeons. Inclusion criteria included patients treated with cervical corpectomy utilizing the described technique with a minimum of 20 months of clinical follow-up. Patients were excluded from participation if they had less than 20 months of clinical follow-up or underwent concomitant posterior cervical fusion.
Demographic and radiographic data of identified patients were recorded. Subsidence was calculated according to the method described by Lee and Sung [1]. Patients were determined to have instability or subsidence if they were found to have a greater than 10% change in either the sagittal alignment or in the settling ratio. Construct failure was defined as broken hardware or subsidence requiring revision surgery. Complications including postoperative infections, hardware complications, subsidence, and adjacent segment disease were recorded. Complications requiring revision surgery were recorded as major complications.
Thirty-one patients were identified as having undergone cervical corpectomy using the “bump-stop” technique during the specified period. Following chart review, four patients were excluded because of concomitant posterior cervical fusion and two were excluded because of inadequate follow-up, leaving a total of 24 patients for review. There were 21 males and three females with an average age of 43 years.
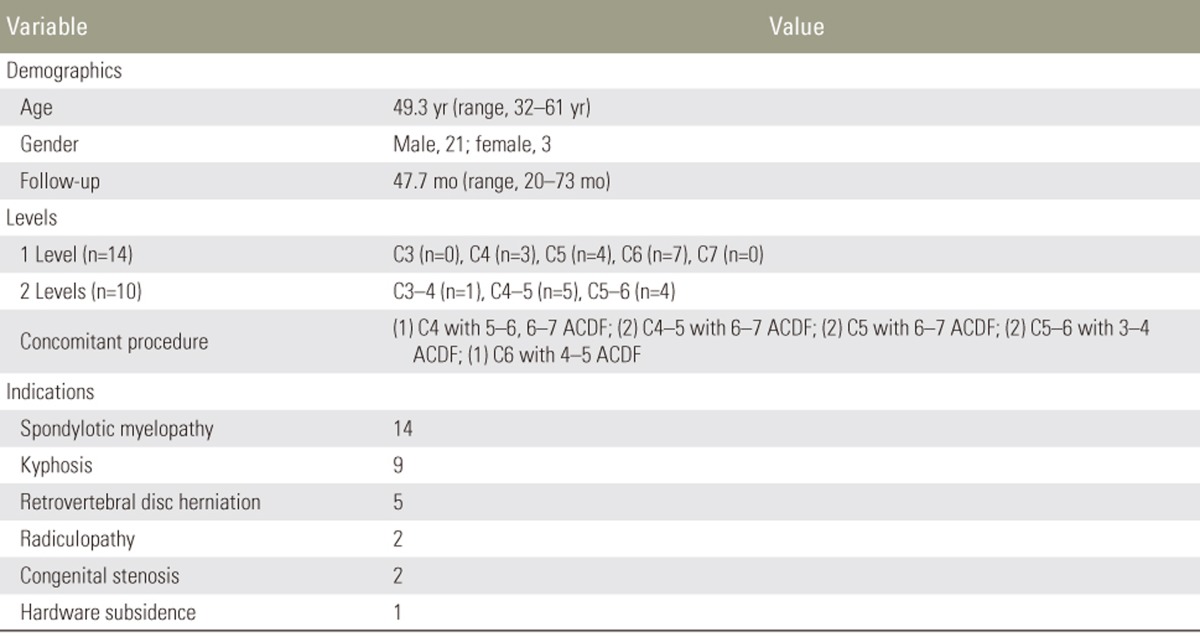
Procedures performed, including cervical levels, number of corpectomies performed, and any concomitant procedures are summarized in Table 1. Fourteen cases involved a single-level corpectomy, whereas 10 involved two levels. There were no cases of isolated three-level anterior corpectomy. Among these cases, 34% were performed on C5 and C6, with isolated C6 corpectomy being the most common procedure performed. Fifty-eight percent of these cases underwent corpectomy for the treatment of spondylotic myelopathy, with 37% involving fixed kyphosis that was not correctable with extension radiographs, and 20% having a retrovertebral disc herniation.
Table 1. Demographic information of identified patients for study inclusion.
ACDF, anterior cervical discectomy and fusion.
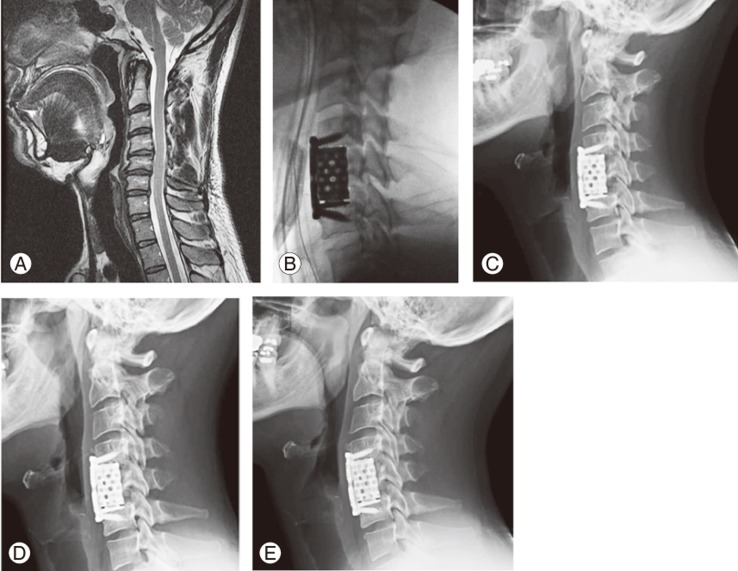
Radiographic review showed that none of the patients treated with the bump-stop technique developed construct subsidence that required revision fusion (Fig. 4). One patient demonstrated adjacent segment disease requiring adjacent-level anterior cervical discectomy and fusion one year postoperatively. Assessing the settling percentage calculation for subsidence, patients demonstrated an average of 3.2% change. Five patients demonstrated a settling percentage >5%, with two (8.3%) demonstrating a settling percentage >10% classified as clinically significant. Neither of these patients with a settling percentage >10% required revision surgery.
Fig. 4. Preoperative T2 sagittal magnetic resonance imaging (A) of a 38 years male with fixed kyphosis at C4–5 with resultant myelopathy requiring C5 corpectomy (B). Follow-up radiograms at 6 weeks (C), 6 months (D), and 18 months (E) demonstrating settling ratio of 0.52 during the last follow-up.
Discussion
The complication profile of cervical corpectomy has ranged widely in the literature, from 7% to 75% [6,11,12]. Many of these variations have been attributed to surgical approach or instrumentation [11], but techniques have since been refined to produce an effective technique for direct anterior decompression and deformity correction [11,12,13]. Despite these refinements, construct failure remains a topic of concern, given its potential catastrophic nature, potential for secondary spinal cord compression, and need for further surgery.
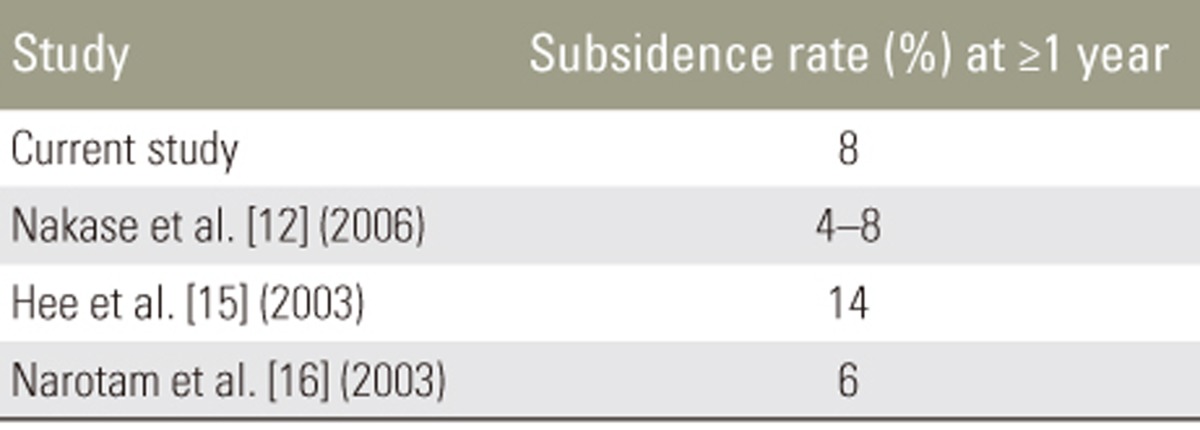
Information regarding the recognition of and efforts to minimize construct subsidence are abundant in the literature. Our technique demonstrates a mean settling of 3.2%, with a rate of clinically significant subsidence at 8%, with no patient requiring revision posterior cervical fusion. The subsidence rate is non-inferior to previous investigations [12,14,15], with the mean settling less than that reported by Narotam et al. [16] at 4.35% at 1 year of follow-up (Table 2).
Table 2. Subsidence rate comparison between the current study and historical studies, based on stated subsidence rate or settling ratio greater than or equal to 10% in the study with a minimum of 1-yea follow-up.
The proposed mechanism of subsidence is known as the pistoning theory [1] that suggests that the graft or cage cavitates into the caudal vertebral endplate. This is well-supported by the higher rate of subsidence caudal to the spanning cage [12]. Tye et al. [17] retrospectively reviewed 70 patients who underwent anterior cervical fusion. In their cohort, they found significant association between construct subsidence and plate length, with longer plates favoring greater subsidence. Their recommendation was to ensure the placement of screws adjacent to the interbody graft/hardware to minimize subsidence. Despite these findings, it is important to understand that subsidence has not been shown to be associated with clinical outcomes, rather improvement of cervical lordosis has been shown to be the main determinant of clinical outcomes [18].
Extrapolating from these findings, we developed the bump-stop technique for cervical corpectomy to ensure the minimization of plate length, while strategically placing our screws to serve as a stop to further minimize the potential for hardware subsidence. Incorporating this technique with the use of an expandable titanium cage further improves the construct strength by maximizing the surface area in contact with the adjacent endplates, as shown in previous investigations [10]. Although, screw angulation has been shown in an allograft finite element analysis to increase shear stresses at the bone screw interface [19], we feel these results are not directly applicable to this construct given the biomechanical differences in the interbody device, load-sharing expandable titanium cage versus allograft strut graft. There is no biomechanical data to support our hypotheses regarding the biomechanical strength of this construct. However, previous investigations have shown that metallic implants exhibit greater resistance to axial loading when compared with osseous grafts [20].
These results must be interpreted with caution given the limitations of this study. The retrospective nature of this study and the lack of appropriate controls limit our ability to make direct observations and show that this is a superior technique for corpectomy instrumentation, than what is currently described. Despite this, our results are comparable to those reported by previous studies (Table 2). In addition, the instrumentation utilized in this technique may not be available to all surgeons.
Our results indicate that the bump-stop technique is an effective approach for instrumenting the cervical spine following one- and two-level corpectomy with a significantly lower rate of subsidence after two years of follow-up. Further prospective and biomechanical research is needed to examine the clinical and biomechanical benefits of this technique.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported. The authors of this paper have no disclosures and no affiliation with any implant manufacturers, whom implants were used during the study period.
The opinions or assertions contained herein are the private views of the authors and are not to be construed as official or reflecting the views of the Department of Defense or US Government. The authors are employees of the US government. This work was prepared as part of their official duties and, as such there is no copyright to be transferred.
References
- 1.Lee SH, Sung JK. Anterior cervical stabilization using a semi-constrained cervical plate and titanium mesh cage for single level corpectomy. J Clin Neurosci. 2008;15:1227–1234. doi: 10.1016/j.jocn.2007.09.019. [DOI] [PubMed] [Google Scholar]
- 2.Salcman M, Jamaris J, Leveque H, Ducker TB. Transoral cervical corpectomy with the aid of the microscope. Spine (Phila Pa 1976) 1979;4:209–212. doi: 10.1097/00007632-197905000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Gore DR. The arthrodesis rate in multilevel anterior cervical fusions using autogenous fibula. Spine (Phila Pa 1976) 2001;26:1259–1263. doi: 10.1097/00007632-200106010-00016. [DOI] [PubMed] [Google Scholar]
- 4.Hilibrand AS, Fye MA, Emery SE, Palumbo MA, Bohlman HH. Increased rate of arthrodesis with strut grafting after multilevel anterior cervical decompression. Spine (Phila Pa 1976) 2002;27:146–151. doi: 10.1097/00007632-200201150-00005. [DOI] [PubMed] [Google Scholar]
- 5.Sasso RC, Ruggiero RA, Jr, Reilly TM, Hall PV. Early reconstruction failures after multilevel cervical corpectomy. Spine (Phila Pa 1976) 2003;28:140–142. doi: 10.1097/00007632-200301150-00009. [DOI] [PubMed] [Google Scholar]
- 6.Daubs MD. Early failures following cervical corpectomy reconstruction with titanium mesh cages and anterior plating. Spine (Phila Pa 1976) 2005;30:1402–1406. doi: 10.1097/01.brs.0000166526.78058.3c. [DOI] [PubMed] [Google Scholar]
- 7.Majd ME, Vadhva M, Holt RT. Anterior cervical reconstruction using titanium cages with anterior plating. Spine (Phila Pa 1976) 1999;24:1604–1610. doi: 10.1097/00007632-199908010-00016. [DOI] [PubMed] [Google Scholar]
- 8.Thalgott JS, Xiongsheng C, Giuffre JM. Single stage anterior cervical reconstruction with titanium mesh cages, local bone graft, and anterior plating. Spine J. 2003;3:294–300. doi: 10.1016/s1529-9430(02)00588-0. [DOI] [PubMed] [Google Scholar]
- 9.Woiciechowsky C. Distractable vertebral cages for reconstruction after cervical corpectomy. Spine (Phila Pa 1976) 2005;30:1736–1741. doi: 10.1097/01.brs.0000172158.31437.ce. [DOI] [PubMed] [Google Scholar]
- 10.Hasegawa K, Abe M, Washio T, Hara T. An experimental study on the interface strength between titanium mesh cage and vertebra in reference to vertebral bone mineral density. Spine (Phila Pa 1976) 2001;26:957–963. doi: 10.1097/00007632-200104150-00022. [DOI] [PubMed] [Google Scholar]
- 11.Kalfas IH. Role of corpectomy in cervical spondylosis. Neurosurg Focus. 2002;12:E11. doi: 10.3171/foc.2002.12.1.12. [DOI] [PubMed] [Google Scholar]
- 12.Nakase H, Park YS, Kimura H, Sakaki T, Morimoto T. Complications and long-term follow-up results in titanium mesh cage reconstruction after cervical corpectomy. J Spinal Disord Tech. 2006;19:353–357. doi: 10.1097/01.bsd.0000210113.09521.aa. [DOI] [PubMed] [Google Scholar]
- 13.Mummaneni PV, Dhall SS, Rodts GE, Haid RW. Circumferential fusion for cervical kyphotic deformity. J Neurosurg Spine. 2008;9:515–521. doi: 10.3171/SPI.2008.10.08226. [DOI] [PubMed] [Google Scholar]
- 14.Dorai Z, Morgan H, Coimbra C. Titanium cage reconstruction after cervical corpectomy. J Neurosurg. 2003;99(1 Suppl):3–7. doi: 10.3171/spi.2003.99.1.0003. [DOI] [PubMed] [Google Scholar]
- 15.Hee HT, Majd ME, Holt RT, Whitecloud TS, 3rd, Pienkowski D. Complications of multilevel cervical corpectomies and reconstruction with titanium cages and anterior plating. J Spinal Disord Tech. 2003;16:1–8. doi: 10.1097/00024720-200302000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Narotam PK, Pauley SM, McGinn GJ. Titanium mesh cages for cervical spine stabilization after corpectomy: a clinical and radiological study. J Neurosurg. 2003;99(2 Suppl):172–180. doi: 10.3171/spi.2003.99.2.0172. [DOI] [PubMed] [Google Scholar]
- 17.Tye GW, Graham RS, Broaddus WC, Young HF. Graft subsidence after instrument-assisted anterior cervical fusion. J Neurosurg. 2002;97(2 Suppl):186–192. doi: 10.3171/spi.2002.97.2.0186. [DOI] [PubMed] [Google Scholar]
- 18.Wu WJ, Jiang LS, Liang Y, Dai LY. Cage subsidence does not, but cervical lordosis improvement does affect the long-term results of anterior cervical fusion with stand-alone cage for degenerative cervical disc disease: a retrospective study. Eur Spine J. 2012;21:1374–1382. doi: 10.1007/s00586-011-2131-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hussain M, Natarajan RN, Fayyazi AH, Braaksma BR, Andersson GB, An HS. Screw angulation affects bone-screw stresses and bone graft load sharing in anterior cervical corpectomy fusion with a rigid screw-plate construct: a finite element model study. Spine J. 2009;9:1016–1023. doi: 10.1016/j.spinee.2009.08.461. [DOI] [PubMed] [Google Scholar]
- 20.Hollowell JP, Vollmer DG, Wilson CR, Pintar FA, Yoganandan N. Biomechanical analysis of thoracolumbar interbody constructs: how important is the endplate? Spine (Phila Pa 1976) 1996;21:1032–1036. doi: 10.1097/00007632-199605010-00007. [DOI] [PubMed] [Google Scholar]