Abstract
Background
A novel approach for improving community case-detection of acute malnutrition involves mothers/caregivers screening their children for acute malnutrition using a mid-upper arm circumference (MUAC) insertion tape. The objective of this study was to test three simple MUAC classification devices to determine whether they improved the sensitivity of mothers/caregivers at detecting acute malnutrition.
Methods
Prospective, non-randomised, partially-blinded, clinical diagnostic trial describing and comparing the performance of three “Click-MUAC” devices and a MUAC insertion tape. The study took place in twenty-one health facilities providing integrated management of acute malnutrition (IMAM) services in Isiolo County, Kenya. Mothers/caregivers classified their child (n=1040), aged 6–59 months, using the “Click-MUAC” devices and a MUAC insertion tape. These classifications were compared to a “gold standard” classification (the mean of three measurements taken by a research assistant using the MUAC insertion tape).
Results
The sensitivity of mother/caregiver classifications was high for all devices (>93% for severe acute malnutrition (SAM), defined by MUAC < 115 mm, and > 90% for global acute malnutrition (GAM), defined by MUAC < 125 mm). Mother/caregiver sensitivity for SAM and GAM classification was higher using the MUAC insertion tape (100% sensitivity for SAM and 99% sensitivity for GAM) than using “Click-MUAC” devices. Younden’s J for SAM classification, and sensitivity for GAM classification, were significantly higher for the MUAC insertion tape (99% and 99% respectively). Specificity was high for all devices (>96%) with no significant difference between the “Click-MUAC” devices and the MUAC insertion tape.
Conclusions
The results of this study indicate that, although the “Click-MUAC” devices performed well, the MUAC insertion tape performed best. The results for sensitivity are higher than found in previous studies. The high sensitivity for both SAM and GAM classification by mothers/caregivers with the MUAC insertion tape could be due to the use of an improved MUAC tape design which has a number of new design features. The one-on-one demonstration provided to mothers/caregivers on the use of the devices may also have helped improve sensitivity. The results of this study provide evidence that mothers/caregivers can perform sensitive and specific classifications of their child’s nutritional status using MUAC.
Trial registrations
Clinical trials registration number: NCT02833740
Keywords: Screening by mothers, Severe acute malnutrition, Community management of acute malnutrition, Mid-upper arm circumference
Background
It is currently estimated that, at any one time, over 17 million children under the age of five years suffer from severe acute malnutrition (SAM) [1], possibly translating to more than 100 million global incident cases each year [2]. Over the past two decades there has been a shift from an in-patient, hospital-based treatment approach for SAM to a decentralised model combining both out-patient care for uncomplicated cases of SAM and in-patient care for SAM children with medical complications or those not responding to treatment [3]. Uncomplicated cases of SAM are treated in an out-patient therapeutic programme (OTP) while complicated cases of SAM are medically stabilised in a nutrition stabilisation centre before being referred for out-patient care in the OTP. This model, known as community management of acute malnutrition (CMAM), or integrated management of acute malnutrition (IMAM) in some contexts, has significantly increased the number of SAM cases receiving treatment in recent years. However, despite these gains, it has been estimated that less than 20% of SAM children are currently accessing treatment globally [4].
A key component of CMAM is ensuring regular screening and case-finding at community level. Since the scaling up of CMAM, mid-upper arm circumference (MUAC) measurement has become the most common form of anthropometric measurement used at community and primary health centre level for the case-finding and admission of cases of acute malnutrition. Most acute malnutrition case-finding is carried out by community health workers (CHW) or community health volunteers (CHV) who measure MUAC and refer children with a MUAC of less than 115 mm for therapeutic feeding and medical care [5–7]. Children with a MUAC of less than 125 mm are referred for supplementary feeding support if this is available. MUAC has been shown to be the best prognostic indicator for mortality in children aged 6–59 months [8–13], especially when repeated over time [14] and has been demonstrated to be a safe and effective anthropometric criterion for diagnosis of acute malnutrition and admission for acute malnutrition treatment [15–19]. If a SAM case is detected and acted upon early in the disease episode this can decrease mortality and morbidity related to malnutrition, reduce per-case treatment costs thanks to shorter treatment times and lower the numbers of children requiring expensive in-patient care for SAM with medical complications [20, 21]. A combination of high cure rates and short treatment lengths often acts to increase SAM treatment programme coverage [8].
A novel community screening approach involves mothers and caregivers using MUAC to detect acute malnutrition in their own children [22]. This may enable mothers and caregivers to develop a better understanding of the signs of malnutrition, be engaged in monitoring their children’s nutrition status and increase the frequency of child screening at community level.
A study conducted in Niger in 2013–2014 [23] demonstrated a significantly higher median MUAC at admission to OTP and better OTP Sphere standards performance indicators [24] in areas where mothers were screening their own children compared to areas where CHWs were responsible for screening children. The study also showed lower proportions of children needing in-patient care at admission or during treatment and reduced numbers of rejected referrals (i.e. children who did not fulfil OTP entry criteria of MUAC < 115mm - an important barrier to coverage [25]) in areas where mothers did the MUAC screening. The coverage of the OTP in the areas where the mothers did the screening was comparable to coverage of the OTP in the areas where the CHWs did the screening.
The work carried out to date on supporting mothers to measure MUAC is based on the utilisation of conventional MUAC tapes. These tapes are colour-coded and/or graduated. They are made of flexible material (e.g. polypropylene or plasticised paper) about 1 cm wide. As per international guidelines [26] the MUAC tape is placed on the middle of the left upper arm of the child. The tension of the band is adjusted by the person undertaking the measurement. Errors with too tight or too loose tape measurements can be observed. Measurement error may decrease the sensitivity of the diagnosis. A previous study conducted in rural Niger [27] found that mothers could use colour-banded MUAC tapes to identify cases of SAM (defined by MUAC < 115 mm) with 73% sensitivity and 98% specificity. It was therefore proposed to develop three simplified and standardised (either 115 mm circumference or including both 115 mm and 125 mm circumferences) MUAC bracelets (“Click-MUAC” devices) to support the mother-led MUAC screening approach and to test these prototypes in an operational setting. The prototypes would be compared to a universal design (i.e. for use with adults, children, and neonates for chest and head circumference), colour-banded MUAC insertion tape (“uniMUAC”). The uniMUAC tape is a modified design (i.e. to improve accuracy) compared to existing models such as the UNICEF MUAC tape [28]. The uniMUAC tape has shown increased accuracy and similar precision, when compared to conventional design MUAC tapes, in tests using soft plastic tubes of known circumference (between 100 mm and 160 mm) [29].
The primary aim of the study was to describe and compare the performance of a set of prototype “Click-MUAC” devices against a “gold standard” of classification, in terms of five measures (sensitivity, specificity, agreement, Fleiss’ Kappa and Youden’s J), for the classification (diagnosis) of nutritional status (SAM, moderate acute malnutrition, normal).
The secondary aim of the study was to determine the difference in agreement with the “gold standard” classification amongst mothers/caregivers using “Click-MUAC” devices versus mothers/caregivers using a MUAC insertion tape.
Methods
Three “Click-MUAC” devices and one MUAC insertion tape were used in the study. The “Click-MUAC” devices were developed with the support of nutrition specialists, plastics specialists and 3D-printing experts in France, the United Kingdom, the United States and Kenya. Brainstorming around product design was initially supported with 3D-printed prototypes, one of which was subsequently pursued by a separate research team [30]. However 3-D printing was not retained as the final prototype manufacturing process for the study, as the designs chosen required a level of detail, functionality and robustness that necessitated a more complex production process. Eighteen prototypes (six specimens of each of the three “Click-MUAC” designs) were produced by a plastics manufacturing company using a plastic printing injection process [31]. This process involved the injection of polypropylene into a resin mould to create functional semi-rigid prototypes. The tolerance and repeatability of the final prototypes were assessed and deemed by the manufacturer and the study team to be similar across the eighteen specimens. The “Click-MUAC” prototypes had a standard measurement of 115 mm (prototypes 1 and 2 – see Fig. 1) and 115 mm and 125 mm (prototype 3 – see Fig. 1).
Fig. 1.
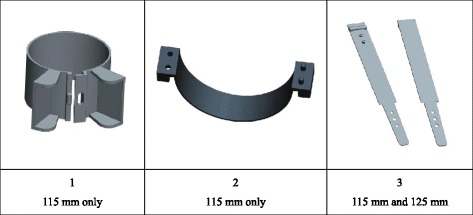
The three “Click-MUAC” prototypes used in the study. Devices 1 and 2 have an internal circumference of 115 mm. Device 3 has an internal circumference of either 115 mm or 125 mm depending on how the device is latched
The study also used a universal design, colour-banded MUAC insertion tape (“uniMUAC”), with 1 mm graduation, designed and produced by a consortium of Non-Governmental Organisations and academics led by Médecins Sans Frontières. The universal MUAC tape was designed to minimise measurement error by having a large tab to enable controlled tensioning of the tape; a three slot "buckle" to hold the tape straight while measurements are taken; a broad tape to reduce the effect of over-tensioning and to increase the probability that the tape covers the mid-point of the upper arm; measuring points that extend to the edge of the tape; and a corrected measurement scale to remove a systematic error of at least +1.8 mm in MUAC measurements found in other conventional design MUAC tapes, which is due to a failure to account for the thickness of the tape material when positioning the scale and/or measurement point. These design elements are shown in Fig. 2.
Fig. 2.
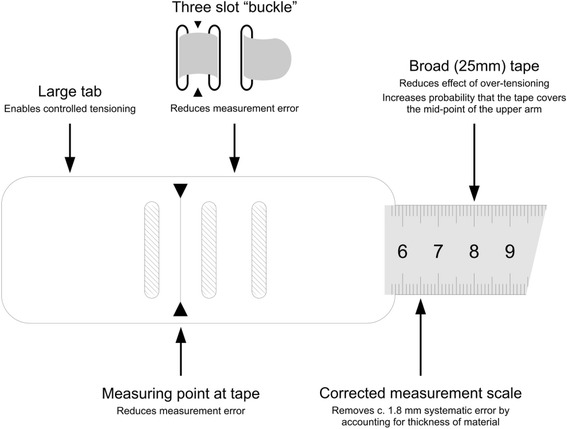
Features of the universal design MUAC insertion tape used in the study
The study was conducted according to the Declaration of Helsinki guidelines and is registered at clinicaltrials.gov (Trial number: NCT02833740). The study protocol was granted ethical approval by the African Medical and Research Foundation (AMREF) Ethics and Scientific Review Committee, Kenya (ESRC number P249/2016) in July 2016.
Superiority was defined as an increase in case-finding sensitivity of 15% or more accompanied by little or no change in specificity. It was calculated that a sample size of n = 115 for each of the three groups (i.e. SAM, moderate acute malnutrition and normal) would be sufficient to determine superiority with better than 95% power, with one-sided p = 0.05, and was feasible to collect in the study programme.
The study took place in Isiolo County, Kenya. Action Against Hunger has been active in Isiolo County since 2009, supporting nutrition-specific and nutrition-sensitive programming in collaboration with the Isiolo County Management Team. The county offered IMAM services, supported by Action Against Hunger, where the devices could be tested.
The study was carried out by the Isiolo County Health Management Team (CHMT), with support from Action Against Hunger. Eight research assistants were trained by the CHMT and Action Against Hunger on the study protocol, interview techniques, obtaining informed consent and detection of acute malnutrition through the measurement of MUAC and testing for oedema. Two measurement standardization tests were conducted and analysed using Emergency Nutrition Assessment software (July 9, 2015 version) in order to verify the accuracy and precision of the measurements taken by the research assistants, following the Habicht method [32]. The questionnaire was pre-tested by the study team on patients at Isiolo County Hospital, prior to starting data collection. Sensitisation on the study, its protocol and its objectives, was also provided to participating health facility staff by the CHMT prior to starting data collection. This helped to facilitate the integration of the study into the routine screening activities conducted within the Isiolo County IMAM programme.
Data collection took place in 7 health facilities offering IMAM services. The selected sites were high-caseload facilities and were chosen in order to be able to test the prototypes on a large number of children with SAM or moderate acute malnutrition (MAM). The selection of the health facilities was done by the CHMT, based on county health records. Data collection took place from the 26th of September 2016 to the 26th of January 2017.
During data collection the health facility staff described the study and presented the prototypes to mothers and caregivers during health sensitisation sessions, which took place early in the morning, before the start of clinic appointments. Thereafter, the data collection team discussed the study individually with mothers and caregivers of children aged 6–59 months (the standard age range for IMAM services) who were entering triage at the health facility. The data collection team provided mothers and caregivers with information on the study, what participation entailed, the risks and benefits of participation and how data confidentiality would be maintained. The mothers/caregivers who agreed to participate, and whose children met the inclusion criteria, were asked to provide consent. Consent was obtained by the data collection team in either written or verbal form and was recorded through signature or thumb prints on individual consent forms. The consent forms that recorded consent through thumb prints were signed by a literate witness with no connection to the study team. The witness was often a community health volunteer (CHV) known to the mother/caregiver. Those not known to the CHV had their thumb prints witnessed by a literate mother who happened to be at the same health facility that day. Children enrolled in the study were mainly children starting or already receiving IMAM treatment services, children visiting the paediatric outpatient department, children attending the child welfare clinic or children whose mothers were involved in mother-to-mother support group meetings for infant and young child feeding at the health facility.
Once a child was enrolled, the data collection team collected identifying and demographic data and then demonstrated the use of the 3 “Click-MUAC” devices and the colour-banded MUAC insertion tape to the mother/caregiver. The mother/caregiver then classified her child’s nutrition status with the 3 “Click-MUAC” devices and the colour-banded MUAC insertion tape. These 4 classifications were recorded by the data collection team. The recorded data was then obscured (by means of a folding data collection form) allowing for partial blinding of the results. The series of MUAC classifications was then repeated by the health facility staff. These 4 health facility staff classifications were also recorded by the data collection team and obscured by folding the data collection form a second time. Mothers/caregivers and health facility staff were also asked to identify their preferred device.
The data collection team then took 3 measurements of the child’s MUAC with the colour-banded MUAC insertion tape at the measured mid-point of the left arm of each study subject. Classifications were made by comparing the arithmetic mean of the three measurements (i.e. the “gold standard” measurement) against case-defining thresholds for global acute malnutrition (i.e. MUAC < 125 mm) and severe acute malnutrition (i.e. MUAC < 115 mm). Any child identified as SAM or MAM, who was not already enrolled in the IMAM programme, was referred for IMAM services.
A mid-term review of the data collection process in December 2016 highlighted that the SAM case numbers were lower than had been expected. To ensure that the SAM sample size (n = 115) was reached, data collection was expanded to an additional 14 facilities and community-based case-finding was strengthened.
Collected data were entered into a purpose-designed EpiData v3.1 database [33]. Data were checked for range and legal values during data-entry. Data were double-entered and validated with discrepancies resolved by reference to data collection forms.
Five measures (sensitivity, specificity, agreement, Fleiss’ Kappa, and Youden’s J) for the different measurer groups (i.e. study staff, clinic staff, and mothers/caregivers) with regard to MUAC classification were calculated from two-by-two contingency tables. Sensitivity was defined as the ability of a device to correctly detect patients with the condition (SAM or MAM), specificity was defined as the ability of a device to correctly detect patients without the condition (SAM or MAM) and agreement was defined as the proportion of cases where the classification was the same as that of the “gold standard”. Fleiss’ Kappa [34] and Younden’s J [35] are both chance-corrected measures of agreement.
Data were analysed using purpose-written R language scripts managed using the R-AnalyticFlow scientific workflow system [36, 37]. Bootstrap methods were used to calculate 95% confidence intervals on summary statistics using r = 9999 replicates. Exact binomial confidence limits were calculated in two cases where 100% sensitivity was observed.
Results
Table 1 shows the description of the study sample. The total sample size for the study was 1040 children. The minimum sample (i.e. n = 115) was reached for each of three groups (i.e. MUAC ≥ 125 mm; 115 mm ≤ MUAC < 125 mm; and MUAC < 115 mm). The majority of children enrolled in the study came from the paediatric outpatient appointments (61.4%), followed by children attending the child welfare clinic or those whose caregivers were participating in infant and young child feeding support (29.3%). The distribution of the “gold standard” measure (i.e. the mean of 3 measurements of the MUAC as taken by a research assistant) ranged from 86 mm to 190 mm, with a median of 137 mm. Within-subject differences between the three MUAC measurements used to create the "gold standard" classification were investigating by comparing all possible pairs of within subject-measurements (n = 3120 measurements). It was found that 3075 (98.6%) differences were less than or equal to 2 mm. The maximum difference found was 4 mm, present in 3 (0.01%) of measurements. The mean difference was close to zero (mean = 0.0032, SD = 1.0227).
Table 1.
Description of the study sample
| Item | Group | Number | Percentage |
| Sample size | All children | 1040 | 100.0% |
| Sex of child | Females | 513 | 49.3% |
| Males | 527 | 50.7% | |
| MUAC classa | MUAC ≥ 125 mm | 698 | 67.1% |
| 115 mm ≤ MUAC < 125 mm | 217 | 20.9% | |
| MUAC < 115 mm | 125 | 12.0% | |
| Source | OTP or SFP program | 96 | 9.2% |
| Paediatric outpatients | 639 | 61.4% | |
| Other source | 305 | 29.3% | |
| Item | Summary | Value | Units |
| Age of child | Minimum | 6 | Months |
| Lower quartile | 11 | ||
| Median | 18 | ||
| Upper quartile | 29 | ||
| Maximum | 59 | ||
| Mean (SD) | 21.37 (13.0) | ||
| MUACb | Minimum | 86 | Mm |
| Lower quartile | 123 | ||
| Median | 137 | ||
| Upper quartile | 148 | ||
| Maximum | 190 | ||
| Mean (SD) | 136 (16.6) |
aCase-definitions applied to the mean of 3 measurements taken by a research assistant
bMean of 3 measurements taken by a research assistant
Figure 3 shows the age and sex distribution of the study sample. The distribution of ages was similar for males and females (Chi-square = 6.0074, df = 4, p = 0.1986).
Fig. 3.
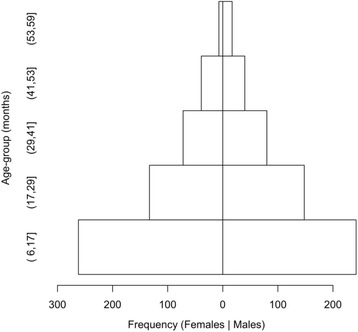
Age and sex distribution of the study sample. Ranges are expressed in ISO 31–11 form [A] The form (a,b] expresses the interval a < x ≤ b. For example, (17,29] is used to indicate the set {18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29} of ages in months. Age-heaping, the tendency of respondents to report ages round to the nearest year or six months is common in many settings. This is a major reason why data from nutritional surveys and programs are often analysed and reported using broad age-groups. The commonest age-groups used with children’s data are 6 to 17 months, 18 to 29 months, 30 to 41 months, 42 to 53 months, and 54 to 59 months. These are known as year-centred age-groups. The last age-group covers only six months but is nominally centred at five years.
Table 2 shows that for SAM classification by mothers, compared to the “gold standard” measurement, all three “Click-MUAC” devices demonstrated good sensitivity (>93%) and excellent specificity (>98%). The chance-corrected measure of agreement (Younden’s J) between mothers’ classification for SAM with the “Click-MUAC” devices and the “gold standard” was also high (>92%). Prototype 3 performed the best out of the 3 “Click-MUAC” devices with a sensitivity of 96.1% [95% CI 92.3%; 99.2%] compared to the “gold standard”. However the device that produced the most sensitive classification (100.0% [95% CI 97.1%; 100.0%]) for mothers, with the highest level of agreement (98.9% [95% CI 98.3%; 99.5%]), was the MUAC insertion tape (device 4). The difference in agreement between prototype 3 and the MUAC insertion tape is statistically significant for Younden’s J: 94.9% [95% CI 91.0%; 97.9%] versus 98.8% [95% CI 98.0%; 99.5%].
Table 2.
Results for “Click-MUAC” devices and uniMUAC tape used by mothers/caregivers and clinic staff compared to case-definition applied to the mean of 3 MUAC measurements taken by a research assistant
| Test | Deviceb | Sensitivityc | Specificityc | Agreementc | Kappa c | Youden’s Jc | |
|---|---|---|---|---|---|---|---|
| SAMd | MSDa | 1 | 93.7% (89.0%, 97.5%) | 98.8% (98.0%, 99.5%) | 98.2% (97.3%, 98.9%) | 0.92 (0.87, 0.95) | 92.5% (87.6%, 96.4%) |
| 2 | 93.8% (89.1%, 97.5%) | 98.7% (97.9%, 99.4%) | 98.1% (97.2%, 98.9%) | 0.91 (0.87, 0.95) | 92.4% (87.7%, 96.3%) | ||
| 3 | 96.1% (92.3%, 99.2%) | 98.8% (98.0%, 99.5%) | 98.5% (97.7%, 99.1%) | 0.93 (0.89, 0.96) | 94.9% (91.0%, 97.9%) | ||
| 4 | 100.0% (97.1%, 100.0%) | 98.8% (98.0%, 99.5%) | 98.9% (98.3%, 99.5%) | 0.95 (0.92, 0.98) | 98.8% (98.0%, 99.5%) | ||
| CSDa | 1 | 92.1% (86.9%, 96.4%) | 99.1% (98.5%, 99.7%) | 98.3% (97.4%, 99.0%) | 0.92 (0.88, 0.95) | 91.3% (86.0%, 95.6%) | |
| 2 | 94.6% (90.1%, 98.2%) | 98.9% (98.2%, 99.6%) | 98.4% (97.5%, 99.1%) | 0.92 (0.88, 0.96) | 93.5% (89.0%, 97.0%) | ||
| 3 | 96.1% (92.1%, 99.2%) | 99.0% (98.3%, 99.6%) | 98.7% (97.9%, 99.3%) | 0.94 (0.90, 0.97) | 95.1% (91.1%, 98.1%) | ||
| 4 | 100.0% (97.1%, 100.0%) | 99.2% (98.7%, 99.8%) | 99.3% (98.9%, 99.8%) | 0.97 (0.94, 0.99) | 99.2% (98.7%, 99.8%) | ||
| GAMd | MSDa | 3 | 90.7% (87.4%, 93.7%) | 96.2% (94.6%, 97.5%) | 94.3% (92.9%, 95.7%) | 0.87 (0.84, 0.90) | 86.8% (83.2%, 90.1%) |
| 4 | 99.1% (98.0%, 100.0%) | 96.5% (95.0%, 97.7%) | 97.3% (96.3%, 98.3%) | 0.94 (0.92, 0.96) | 95.6% (93.7%, 97.2%) | ||
| CSD | 3 | 91.8% (88.9%, 94.6%) | 97.2% (95.8%, 98.3%) | 95.4% (94.0%, 96.6%) | 0.89 (0.86, 0.92) | 89.0% (85.6%, 92.0%) | |
| 4 | 98.0% (96.4%, 99.4%) | 97.4% (96.2%, 98.5%) | 97.6% (96.6%, 98.5%) | 0.95 (0.92, 0.97) | 95.4% (93.4%, 97.2%) |
aMSD = Classification by mother/caregiver made using the specified “Click-MUAC” device or uniMUAC tape; CSD = Classification by IMAM clinical staff using the specified “Click-MUAC” device or uniMUAC tape
bNumbers 1, 2 and 3 refer to specific “Click-MUAC” devices. Device 4 is the uniMUAC tape
cPoint estimates and associated 95% confidence intervals of summary measures are reported
dSAM is defined as MUAC < 115 mm; GAM is defined as MUAC < 125 mm. Devices 1 and 2 did not allow for GAM assessment
SAM classification by clinic staff using the three “Click-MUAC” devices, compared to the “gold standard”, was good (sensitivity > 92%, specificity > 98%, Younden’s J > 91%) however the MUAC insertion tape performed better with a sensitivity of 100.0% [95% CI 97.1%; 100.0%], a specificity of 99.2% [95% CI 98.7%; 99.8%] and a Younden’s J of 99.2% [95% CI 98.7%; 99.8%].
Table 2 also shows that for GAM classification by mothers, prototype 3 demonstrated good sensitivity (90.7% [95% CI 87.4%; 93.7%]) and specificity (96.2% [95% CI 94.6%; 97.5%]). Younden’s J for GAM classification by mothers with prototype 3 was 86.8% [95% CI 83.2%; 90.1%] compared to the “gold standard”. However the sensitivity, specificity and agreement for GAM classification by mothers with the MUAC insertion tape was better: the sensitivity was 99.1% [95% CI 98.0%; 100.0%], the specificity was 96.5% [95% CI 95.0%; 97.7%] and Younden’s J was 95.6% [95% CI 93.7%; 97.2%]. The difference in Younden’s J for GAM classification by mothers using the prototype 3 compared with using the MUAC insertion tape is statistically significant: 86.8% [95% CI 83.2%; 90.1%] versus 95.6% [95% CI 93.7%; 97.2%] respectively.
The better performance of the MUAC insertion tape for GAM classification was also reflected in the results of the clinic staff. GAM classification by clinic staff using prototype 3 demonstrated good sensitivity (91.8% [95% CI 88.9%; 94.6%]) and specificity (97.2% [95% CI 95.8%; 98.3%]). Youden’s J for GAM classification by clinic staff with prototype 3 was 89.0% [95% CI 85.6%; 92.0%]. However both sensitivity and agreement for GAM classification by clinic staff with the MUAC insertion tape was significantly better: the sensitivity was 98.0% [95% CI 96.4%; 99.4%] and Younden’s J was 95.4% [95% CI 93.4%; 97.2%].
The study also sought to gather information on preference with regards to the devices used. Table 3 demonstrates that a higher proportion of mothers (33.3%) preferred prototype 3 to the other devices. The majority of clinic staff (70.7%) preferred the MUAC insertion tape.
Table 3.
Device preferences for mothers and IMAM clinic staff
| Device | ||||
|---|---|---|---|---|
| 1 | 2 | 3 | MUAC tape | |
| Mothers | 290 (27.9%) | 156 (15.0%) | 347 (33.3%) | 247 (23.8%) |
| IMAM clinic staff | 85 (07.9%) | 58 (05.6%) | 164 (15.8%) | 735 (70.7%) |
Discussion
The results of this study indicate that, although the “Click-MUAC” devices performed well, the improved MUAC insertion tape performed best for mothers and caregivers classifying the nutritional status of their own children. The study team reported that mothers were concerned about pinching their child’s skin with devices 1 and 2 and this may have affected the ability of mothers to latch these devices properly. This may explain why the sensitivity is more reduced and to the same degree with these two devices (93.7% for device 1 and 93.8% for device 2). Sensitivity is less reduced with device 3. Given the nature of the design (similar to that of a tape) sensitivity in this case would have been affected by under-tensioning. This may have been due to the thickness of the plastic which may have compromised the device’s flexibility and hindered the mother’s ability to tension it properly. The tail of the tape in device 3 may also have been too short or too slippery for mothers to get a good grip.
The results for sensitivity of SAM classification by mothers with the MUAC tape are higher than those previously reported in the Blackwell et al. study [14] which demonstrated that mothers had a sensitivity for the classification of their child’s nutritional status of 73% and 90% respectively for SAM and GAM. It is possible that the high sensitivity reported in this study for both SAM and GAM classification by mothers with the MUAC insertion tape is due to the use of an improved MUAC tape design which has a number of modifications as compared to the conventional MUAC tape design, as illustrated in Fig. 2. It is also possible that the method of demonstration of the use of the tape to the mothers led to improved sensitivity. In the Blackwell et al. study [14] the use of the MUAC tape was demonstrated to the whole participating village. In this study however, mothers were provided with a one-on-one demonstration on the use of the MUAC insertion tape and the “Click-MUAC” devices by a member of the study team. There are some limitations to the study which could have biased the results presented in this paper. The study was only partially blinded and there may have been potential demonstration bias. It may also have been the case that mothers got better at fitting the devices as they worked through them, which could have influenced the sensitivity of the final device (the MUAC insertion tape). It is recommended that any similar study, conducted in the future, randomised the order of use of the prototypes to avoid this. The study did not collected further qualitative information regarding the preference of mothers for each of the devices. It is possible that the mothers preferred device 3 as it had the possibility to screen for both SAM and MAM but was sturdier and simpler to use than device 4 (uniMUAC tape). Clinical staff may have preferred device 4 (uniMUAC tape) because it enabled them to quantify the MUAC, rather than have a simple binary classification. Clinical staff may also have preferred device 4 (uniMUAC tape) because it more closely resembled the tape in current use (UNICEF MUAC tape).
Conclusion
The results of this study demonstrate that although the “Click-MUAC” devices performed well, a well-designed MUAC insertion tape remains the best means to support mother-led MUAC screening. The MUAC insertion tape is also less costly to produce and may therefore be better suited to supporting larger-scale mother-led MUAC screening initiatives.
The results of this study provide strong evidence to support the ability of mothers to perform sensitive and specific measurements of their child’s MUAC. With an improved MUAC tape design and adequate minimal training, low MUAC children can be reliably identified by their mothers and caregivers. Given the potential for mother/caregiver MUAC screening to improve community case detection, early care-seeking behaviours and acute malnutrition treatment coverage, the approach should become central to efforts to scale-up acute malnutrition treatment globally.
Acknowledgments
The authors would like to thank the University of Michigan for their support in the initial 3D modelling and Alain Guelpa Concept for their support in the production of the final plastic prototypes. The authors would like to thank the mothers, children and health staff who participated in the study. The authors are grateful to the Isiolo County Health Management Team and the Action Against Hunger Isiolo programme team for their support, dedication and enthusiasm in implementing the study. The authors are also grateful to the Kenya National Emergency Nutrition Advisory Committee and the Kenya National Nutrition Information Technical Working Group for their perspectives and support in the development of the protocol, implementation of the study and review of the results.
Funding
The study was conducted with funding from the Humanitarian Innovation Fund (HIF). HIF had no role in the design of the study, the collection, analysis and interpretation of data or the drafting of the manuscript.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AMREF
African Medical and Research Foundation
- CHMT
County Health Management Team
- CHV
Community Health Volunteer
- CHW
Community Health Worker
- CMAM
Community Management of Acute Malnutrition
- ESRC
Ethics and Scientific Review Committee
- GAM
Global Acute Malnutrition
- IMAM
Integrated Management of Acute Malnutrition
- MAM
Moderate Acute Malnutrition
- MUAC
Mid-Upper Arm Circumference
- OTP
Out-patient Therapeutic Programme
- SAM
Severe Acute Malnutrition
- uniMUAC
Universal Mid-Upper Arm Circumference
Authors’ contributions
AG, MM and AB designed the prototypes and study. The study was coordinated by AG and IA. The data collection was conducted by EO, JN, SM and AS and data was analysed by MM. The manuscript was drafted by AG. It was reviewed, edited and approved by MM, AB, IA, EO, JN, SM and AS.
Ethics approval and consent to participate
The study protocol was granted ethical approval by the African Medical and Research Foundation (AMREF) Ethics and Scientific Review Committee, Kenya (ESRC number P249/2016). The study is registered at clinicaltrials.gov (Trial number: NCT02833740). Consent was obtained by the data collection team in either written or verbal form and was recorded through signature or thumb prints on individual consent forms.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Angeline Grant, Email: agrant@actionagainsthunger.org.
James Njiru, Email: nutiycn.ke@acf-international.org.
Edgar Okoth, Email: hod-nut@ke-actionagainsthunger.org.
Imelda Awino, Email: iawino@actionagainsthunger.org.
André Briend, Email: andre.briend@gmail.com.
Samuel Murage, Email: matymesam@gmail.com.
Saida Abdirahman, Email: saidaabdirahman@yahoo.com.
Mark Myatt, Email: mark@brixtonhealth.com.
References
- 1.Joint Child Malnutrition Estimates. The United Nations Children’s Fund, the World Health Organisation and the World Bank Group. Levels and trends in child malnutrition - key findings of the 2016 edition. Accessed from: http://www.who.int/nutgrowthdb/jme_brochure2016.pdf?ua=1 on 4 May2017
- 2.Hure A, Oldmeadow C, Attia J. Invited Commentary: Improving Estimates of Severe Acute Malnutrition Requires More Data. Am J Epidemiol. 2016; 15;184(12):870–872 [DOI] [PubMed]
- 3.A Joint Statement by the World Health Organisation, the World Food Programme, the United Nations Standing Committee on Nutrition and the United Nations Children’s Fund. Community based management of severe acute malnutrition. Geneva: World Health Organisation; 2007.
- 4.State of Severe Malnutrition. Accessed from: http://www.severemalnutrition.org//home/Ge on 4 May 2017
- 5.A Joint Statement by the World Health Organization and the United Nations Children’s Fund. World Health Organisation, United Nations Children’s Fund. Child growth standards and the identification of severe acute malnutrition in infants and children. Geneva: World Health Organisation; 2009 [PubMed]
- 6.Updates on the management of severe acute malnutrition in infants and children. Geneva: World Health Organisation; 2013.. [PubMed]
- 7.Velzeboer MI, Selwyn BJ. Sargent 2nd F, Pollitt E. Delgado H. The use of arm circumference in simplified screening for acute malnutrition by minimally trained health workers. J Trop Pediatr. 1983;29:159–166. doi: 10.1093/tropej/29.3.159. [DOI] [PubMed] [Google Scholar]
- 8.Briend A, Dykewicz C, Graven K, Mazumder RN, Wojtyniak B, Bennish M. Usefulness of nutritional indices and classifications in predicting death of malnourished children. Br Med J (Clin Res Ed) 1986;293(6543):373–375. doi: 10.1136/bmj.293.6543.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pelletier DL. The relationship between child anthropometry and mortality in developing countries: implications for policy, programs and future research. J Nutr. 1994;124(Suppl 10):S2047–S2081. doi: 10.1093/jn/124.suppl_10.2047S. [DOI] [PubMed] [Google Scholar]
- 10.Myatt M, Khara T, Collins S. A review of methods to detect cases of severely malnourished children in the community for their admission into community based therapeutic care programs. Food Nutr Bull. 2006;27:s7–s23. doi: 10.1177/15648265060273S302. [DOI] [PubMed] [Google Scholar]
- 11.Briend A, Maire B, Fontaine O, Garenne M. Mid-upper arm circumference and weight-for-height to identify high-risk malnourished under-five children. Matern Child Nutr. 2012;8(1):130–133. doi: 10.1111/j.1740-8709.2011.00340.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grellety E, Krause LK, Shams Eldin M, Porten K, Isanaka S. Comparison of weight-for-height and mid upper arm circumference (MUAC) in a therapeutic feeding programme in South Sudan: is MUAC alone a sufficient criterion for admission of children at high risk of mortality? Public Health Nutr. 2015;18(14):2575–2581. doi: 10.1017/S1368980015000737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sachdeva S, Dewan P, Shah D, Malhotra RK, Gupta P. Mid-upper arm circumference v. weight-for-height Z-score for predicting mortality in hospitalized children under 5 years of age. Public Health Nutr. 2016;19(14):2513–2520. doi: 10.1017/S1368980016000719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Briend A, Zimicki S. Validation of arm circumference as an indicator of risk of death in one to four year old children. Nutr Res. 1986;6:249–261. doi: 10.1016/S0271-5317(86)80129-4. [DOI] [Google Scholar]
- 15.Mogendi JB, De Steur H, Gellynck X, Saeed HA, Makokha A. Efficacy of mid-upper arm circumference in identification, follow-up and discharge of malnourished children during nutrition rehabilitation. Nutr Res Pract. 2015;9(3):268–277. doi: 10.4162/nrp.2015.9.3.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Binns P, Dale N, Banda T, Banda C, Shaba B, Myatt M. Safety of using mid-upper arm circumference as a discharge criterion in community-based management of severe acute malnutrition in children aged 6–59 months. Valid International: Oxford, England; 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goossens S, Bekele Y, Yun O, Harczi G, Ouannes M, Shepherd S. Mid-upper arm circumference based nutrition programming: evidence for a new approach in regions with high burden of acute malnutrition. PLoS One. 2012;7(11):e49320. doi: 10.1371/journal.pone.0049320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Phelan KPQ, Lanusse C, van der Kam S, Delchevalerie P, Avril N, Hanson K. Simplifying the response to childhood malnutrition: MSF’s experience with MUAC-based (and oedema) programming. Field Exch. 2015;50:108–110. Accessed from: http://www.ennonline.net/fex/50/msfmuacprogramming on 11 Nov 2017.
- 19.Fernández MA, Delchevalerie P, Van Herp M. Accuracy of MUAC in the detection of severe wasting with the new WHO growth standards. Pediatrics. 2010;126(1):e195–e201. doi: 10.1542/peds.2009-2175. [DOI] [PubMed] [Google Scholar]
- 20.Sadler K, Puett C, Mothabbir G, Myatt M, 2011. Community Case Management of Severe Acute Malnutrition in Southern Bangladesh. Tufts University, 1–48. Accessed from: http://fic.tufts.edu/publication-item/community-case-management-of-severe-acute-malnutrition-in-southern-bangladesh/ on 4 May 2017
- 21.Puett C, Coates J, Alderman H, Sadler K. Quality of care for severe acute malnutrition delivered by community health workers in southern Bangladesh. Matern Child Nutr. 2013;9:130–142. doi: 10.1111/j.1740-8709.2012.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.The Alliance for International Medical Action. Mother MUAC. Teaching Mothers to Screen for Malnutrition. Guidelines for Training of Trainers. 2016
- 23.Alé F, Phelan K, Issa H, Defourny I, Le Duc G, Harczi G, Issaley K, Sayadi S, Ousmane N, Yahaya I, Myatt M, Briend A, Allafort-Duverger T, Shepherd S, Blackwell N. Mothers screening for malnutrition by mid-upper arm circumference is non-inferior to community health workers: results from a large-scale pragmatic trial in rural Niger. Arch Public Health. 2016;74(1):38. doi: 10.1186/s13690-016-0149-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.The Sphere Project. The Sphere Handbook, Humanitarian Charter and Minimum Standards in Humanitarian Response. Management of acute malnutrition and micronutrient deficiencies standard 2: Severe acute malnutrition. 2011. Accessed from: http://www.spherehandbook.org on 4 May 2017
- 25.Guerrero S, Myatt M, Collins S. Determinants of coverage in community-based therapeutic care programmes: towards a joint quantitative and qualitative analysis. Disasters. 2010;34(2):571–585. doi: 10.1111/j.1467-7717.2009.01144.x. [DOI] [PubMed] [Google Scholar]
- 26.Inter-Agency Standing Committee Global Nutrition Cluster. Harmonised Training Package: Resource Material for Training on Nutrition in Emergencies. Module 6 - Measuring Malnutrition: Individual Assessment. 2011. Accessed from: http://files.ennonline.net/attachments/1979/htp-module-6-whole-module.pdf on 4 May 2017
- 27.Blackwell N, Myatt M, Allafort-Duverger T, Balogoun A, Ibrahim A, Briend A. Mothers Understand it And Can do it (MUAC): a comparison of mothers and community health workers determining mid-upper arm circumference in 103 children aged from 6 months to 5 years. Arch of Public Health. 2015;73(1):26. doi: 10.1186/s13690-015-0074-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.MUAC, Child 11.5 Red/PAC-50. UNICEF Supply Catalogue. Accessed from: https://supply.unicef.org on 11 Nov 2017
- 29.Rao B, Roby R, LeBeau K, du Cros P, Briend A, Fritsch P, Ververs M, Myatt M. Comparing the accuracy and sensitivity of a double-sided universal MUAC strap (“uniMUAC”) with the UNICEF MUAC strap. Paper presented at Médecins Sans Frontières UK Scientific Days: Innovation 2017, London, United Kingdom, May 2017. Accessed from: https://f1000research.com/documents/6-885 on 14 Jun 2017
- 30.Michaels RE, Pearce JM. 3-D printing open-source click-MUAC bands for identification of malnutrition. Public Health Nutr. 2017;20(11):2063–2066. doi: 10.1017/S1368980017000726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Printing Injection Process. Alain Guelpa Concept and MP2i. Accessed from: http://www.pip-prototype.fr/ on 11 Nov 2017
- 32.Habicht JP. Estandardizacion de metodos epidemiologicos cuantitativos sobre el terrano. Bol Oficina Sanit Panam. 1974;76(5):375–384. [PubMed] [Google Scholar]
- 33.Lauritsen JM, Bruus M, Myatt MA. EpiData v3.10 - A tool for validated entry, documentation, and analysis of epidemiological data. County of Funen, Denmark and Brixton Health, Llanidloes, UK, 2008
- 34.Fleiss JL. Statistical methods for rates and proportions. 2. New York: John Wiley; 1980. [Google Scholar]
- 35.Youden WJ. Index for rating diagnostic tests. Cancer. 1950;3(1):32–35. doi: 10.1002/1097-0142(1950)3:1<32::AID-CNCR2820030106>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 36.R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna; 2017. Accessed from: https://cran.r-project.org on 4 May 2017
- 37.Ef-Prime. R AnalyticFlow 3.1.1. Ef-prime Inc., Tokyo; 2017. Accessed from: http://r.analyticflow.com on 4 May 2017
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.


